Abstract
Multiphase CT angiography (CTA) in collateral assessment provides time-resolved cerebral angiograms of the intracranial vasculature, requiring a high-speed multidetector CT (MDCT) scanner with ≥ 64 slices. Unfortunately, many hospitals are equipped with lower speed MDCT scanners. Herein, we present our experience performing dual-phase CTA (d-CTA) on a 16 slice MDCT with a biphasic rate injection to grade intracranial collaterals as predictor of clinical outcome. 42 patients were evaluated with both dual-phase CTA (d-CTA) and single-phase CTA (s-CTA) for occluded anterior intracranial circulation and collaterals. They were treated with endovascular reperfusion. Univariate and multivariate analyses were performed to define the independent predictors for favorable outcome at 3 months. Good collateral circulation status on d-CTA was associated with a lower median 24-h (5 vs. 7.5, p = 0.03) and discharge (2 vs. 4.6, p = 0.04) NIHSS. A logistic regression model showed that only age (OR 0.95, 95% CI 0.91–0.98, p = 0.03) and good collateral circulation status at d-CTA (OR 4.3, 95% CI 1.87–11.3, p < 0.01) were independent predictors of favorable functional outcome at 3 months, but that s-CTA was not. The collateral status on d-CTA can be a useful predictor for clinical outcome in acute stroke patients. The proposed protocol adapted to a low-speed MDCT scanner could be of particular interest in hospitals without access to the more up-to-date technology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Recent data suggest that clinical outcome of acute ischemic stroke due to large vessel anterior circulation occlusion is improved by endovascular treatment with stent retrievers [1]. The most important factors in patient selection for endovascular stroke therapy are a substantial acute neurological deficit, a treatable arterial occlusion, and a non-extensive ischemic core [2]. Although consensus does not exist on the best neuroimaging technique for the assessment of patient eligibility, CT and CT angiography are mainly used to confirm vessel occlusion, whereas different methods are used to estimate the infarct core (CT angiography, Alberta Stroke Program Early CT Score, perfusion imaging and assessment of collateral circulation) [3]. Good collateral flow is associated with better clinical outcome, less risk of hemorrhagic transformation and a greater likelihood of successful recanalization [4]. Multiphase CT Angiography (m-CTA) technique aims at assessing the grade of the intracranial collaterals and helping in decision-making on whether to proceed or not with endovascular therapy. m-CTA is a novel, but simple imaging technique where acquisitions are obtained in the late-arterial, mid-venous and late-venous phases providing time-resolved cerebral angiograms of the intracranial vasculature [5]. However, it does require a high-speed multidetector CT (MDCT) scanner with ≥ 64 slices while, unfortunately, many hospitals are equipped with lower speed MDCT scanners (< 64 detectors). The ability to obtain high-temporal-resolution images on such scanners would thus be helpful. Herein, we present our experience performing dual-phase CTA (d-CTA) on a 16 slice MDCT with a biphasic rate injection to grade intracranial collaterals as predictor of clinical outcome.
Materials and methods
We carried out a validation study in an internal cohort of acute anterior occlusion stroke patients. Stroke patients treated with endovascular reperfusion therapies were evaluated by single CTA (s-CTA) and d-CTA, to assess if d-CTA could improve the accuracy for the evaluation of the collateral circulation as a predictor of clinical outcome. Consecutive acute stroke patients, admitted to the Casualty Department of the Guglielmo da Saliceto Hospital (Piacenza, Italy) within 6 h from symptom onset, were enrolled and studied. In line with our radiological acute stroke protocol, all patients received an unenhanced CT to exclude a hemorrhagic stroke and large early ischemic changes [Alberta Stroke Program Early CT score (ASPECTS) < 6]. A s-CTA and d-CTA were then performed to evaluate intracranial occlusion and collateral circulation (CC) status. The stroke severity was evaluated by the means of the National Institute of Health stroke scale (NIHSS). A 90-day post-stroke follow-up evaluation was made on all patients using the modified Rankin scale (mRS) and they were considered functionally independent if the mRS score was ≤ 2. Patients with an NIHSS score of ≥ 10 and a proximal intracranial occlusion were given endovascular reperfusion. Any patients with an occlusion of the middle cerebral artery (M1 segment) or intracranial internal carotid artery (IICA) were included in the study.
Intracranial collaterals were not considered for clinical decision-making in the acute stroke phase but measured off-line by an expert stroke neuroradiologist blinded to the clinical data. Measurement of the CC status was visually determined by comparing backfilling arteries beyond the occluded artery to similar arteries in the opposite unaffected hemisphere. Table 1 reports the CC scores from both s-CTA and d-CTA.
Patients were dichotomized into good and poor CC status, according to both the s-CTA (poor CC: 0–1, good CC: 2–3) [6] and d-CTA scores (poor CC: 0–3, good CC: 4–5) [5]. The collateral scores on both d-CTA and s-CTA were evaluated independently by two neuroradiologists blinded to the clinical data. Disagreements were settled by consensus.
All enrolled patients were given endovascular reperfusion treatment. Proximal arterial occlusion was confirmed by digital subtraction angiography (DSA) before treatment and recanalization was determined by the modified thrombolysis in cerebral ischemia (TICI) score [7]. A final TICI score of 2b–3 was defined as complete recanalization.
The study protocol was approved by the local ethical committee and the researchers.
CT angiography protocol
CT angiograms of the intracranial vasculature were obtained in two phases after i.v. contrast medium (CM) injection using a 16 slice MDCT scanner (Siemens Somatom Emotion). For the arterial phase, obtained from skull base to vertex, bolus tracking was utilized to monitor the arrival of contrast into the pre-cavernous internal carotid artery segments. The second imaging phase was acquired in the late-venous phase from the vertex to the skull base. Each scan phase lasted ~ 8 s, with a 4-s interval (110 kV, 100 eff. mAs, a rotation time of 0.6 s, a pitch of 1.3 and a collimation of 16 × 0.6 mm, with an effective slice thickness of 0.75 mm). An additional scan was then performed on the neck vessels from the skull base to the aortic arch, with a different detector configuration to shorten acquisition time (110 kV, 100 eff. mAs, a rotation time of 0.6 s, a pitch of 1.3 and a collimation of 16 × 1.2 mm, with an effective slice thickness of 1.5 mm). A dual configuration of the detectors is essential to maximize spatial resolution in the intracranial vessels and to increase the acquisition rate at the neck (Fig. 1a). A total of 80 mL of iodinated CM (350 mg I/mL) was injected at a biphasic rate [8] (50 cc at a rate of 4.5 mL/s, subsequently 30 cc at 2.5 mL/s followed by a 50 mL normal saline chase at a rate of 2.5 mL/s) to allow for a persistent opacification of the neck vessels (Fig. 1e). Axial images were reconstructed in 1-mm overlapping sections with multiplanar reconstructions for axial, coronal, and sagittal images of the circle of Willis, performed with 3-mm thickness at 1.5-mm intervals. Thick-section axial maximum intensity projections (MIP) at 30 mm thickness and 5-mm intervals were also reconstructed. Automatic post-processing of d-CTA maps was completed in less than 2–3 min. The first phase of the d-CTA was acquired in the late-arterial phase and was defined as the s-CTA. Intracranial occlusion was determined in the first phase of d-CTA.
a d-CTA images with slow-speed 16 slice MDCT scanner; each phase is represented by an arrow. b The curve with the circle points illustrates the configuration of the geometry bolus with a biphasic rate injection (50 cc at a rate of 4.5 mL/s, subsequently 30 cc at 2.5 mL/s followed by a 50 mL normal saline chase at a rate of 2.5 mL/s; comparison bolus single rate injection is shown on the curve with triangle). c, d Divergence in CC status with s-CTA and d-CTA scores. An example of good collateral flow with d-CTA (axial MIP image; score 3: delay in the 1st phase in the filling-in of peripheral vessels, prominence and extent is the same in the 2nd phase compared to the asymptomatic contralateral hemisphere) and poor collateral flow when using s-CTA (score 1: collateral supply filling < 50% but > 0% of the occluded vascular territory). Arrow evidences occlusion of the left MCA. The late-arterial phase (1st phase) in c and the late-venous phase (2st phase), in d. Adequate persistent opacification of the carotid arteries is shown in e (arrows). est effective slice thickness, t scan time, NVs neck vessels
Statistical analysis
Continuous variables were expressed as average values with standard deviations and categorical variables as frequencies. Intergroup comparisons were performed by Student’s t test, the Mann–Whitney U test and the chi-square test when appropriate. Multivariate logistic regression analyses were performed for each group to determine factors that could be considered independent predictors of favorable outcome; variables showing a p value of < 0.1 in a univariate analysis were included in the multivariate model.
Statistical analysis was performed using a standard statistical package (SPSS version 17.0 SPSS Inc, Chicago, Ill., USA). All tests were two-tailed and conventional levels of statistical significance were used (p = 0.05). Error rate, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were also calculated for s-CTA and d-CTA as predictors of good outcome after recanalization treatment.
Results
42 patients were enrolled in the study from January 2016 to June 2017. Their mean age was 71 ± 12 years, median baseline NIHSS score was 17 and median baseline ASPECTS was 9. Patient characteristics at baseline are shown in Table 2. 30 patients (71.4%) showed an M1 occlusion and 12 (28.6%) an intracranial internal carotid artery occlusion. Intravenous rt-PA treatment was administered to 23 patients (54.7%) before endovascular reperfusion, according to the European stroke guidelines. All patients were treated with stent retrievers. Complete recanalization (TICI score 2b–3) was achieved in 76.2% (32 pts) of the patients. 20 patients (47.6%) had an early clinical improvement and 23 (54.8%) achieved functional independency (an mRS score of 0–2) at 3 months. At s-CTA, 18 patients (52.6%) had good CC compared to 57.1% (24 pts) at d-CTA.
There was no significant difference in recanalization rate (TICI score 2b–3) for patients with good or poor CC status, evaluated by both s-CTA (74.6 vs. 76.5%, p = 0.52) and d-CTA (77.2 vs. 73.5%, p = 0.35). It was observed that CC status at d-CTA was a good predictor of clinical outcomes, while s-CTA was not. Good CC on d-CTA was associated with a lower median 24-h (5 vs. 7.5, p = 0.03) and discharge (2 vs. 4.6, p = 0.04) NIHSS score. Conversely, a good CC status at s-CTA was also associated to a better tendency in early and long-term outcomes, even if statistical significance was not reached.
A logistic regression model, adjusted for baseline NIHSS score, ASPECTS and recanalization, showed that only age (OR 0.95, 95% CI 0.91–0.98, p = 0.03) and good CC status at d-CTA (OR 4.3, 95% CI 1.87–11.3, p = 0.002) were independent predictors of favorable functional outcome at 3 months (Table 3).
Six patients where s-CTA and d-CTA showed a divergence in their CC status were investigated. All of them had poor intracranial collaterals at s-CTA and good ones at d-CTA. A total of 83.3% of this population achieved good functional outcome (an mRS score of < 3 at 3 months) with no differences in baseline characteristics, which may indicate that s-CTA underestimates collateral status in some patients due to its lack of temporal resolution.
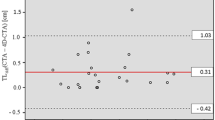
s-CTA as a predictor of good outcome after recanalization treatment showed, respectively, error rate 11.9%, sensitivity 78.3%, specificity 100%, PPV 100% and NPV 79.2%, whereas d-CTA an error rate 2.4%, sensitivity 100%, specificity 94.7%, PPV 95.8% and NPV 100%.
Discussion
A consensus on the optimal neuroimaging technique to be adopted for the determination of patient eligibility for endovascular therapy has not been reached yet. However, given the relatively easy availability of CT scanners worldwide, CT and CTA remain the standard modality for acute stroke diagnosis [9]. The collateral circulation is a physiologic pathway of specialized endogenous bypass vessels present in most tissues. It protects against ischemic injury during initial oligemic status [10]. A good collateral flow is associated with better clinical outcomes, less risk of haemorrhagic transformation and a greater likelihood of successful recanalization [11]. In the setting of acute ischemic stroke, the extent of collateral circulation influences the size of the final infarct and extension of the penumbra. Collateral blood flow is assessed by comparing the pial arterial filling in the ischaemic area of the brain at CTA with that of similar arteries in the contralateral hemisphere. The advantage of a dual-phase study is that it can detect temporal delay in the filling of vessels in addition to prominence and extent of vessels detectable with a single-phase technique. Moreover, CC status has already been used to select patients for endovascular therapy [12]. Our study shows that d-CTA is a quick, noninvasive, accurate technique to evaluate CC status in acute ischemic stroke patients in line with another study that compared m-CTA with other scales [5]. Furthermore, d-CTA was also associated with early and long-term good clinical outcomes and was an independent predictor of favorable outcome, whilst s-CTA was not. The ESCAPE trial [12] showed the utility of current endovascular reperfusion treatment in patients with good or intermediate leptomeningeal CC status at m-CTA.
It was also observed that patients with collateral assessment divergence on s-CTA and d-CTA (poor CC status on s-CTA and good CC status on d-CTA) had a high probability of good functional outcome (83.3% mRS score < 3 at 3 months). This supports the hypothesis, reported in several studies, that s-CTA may underestimate CC [13,14,15]. Caution is required if patients with ‘‘poor/absent” collaterals at s-CTA are excluded from treatment, as some of them will actually have a quite good collateral flow, which arrived after the CTA acquisition. However, multifactorial aspects may be involved in this topic and other explanations beside just temporal resolution may be hypothesized to explain our observation. Therefore, endovascular therapy decisions based on CC status measured by s-CTA may be inaccurate and can lead to the discarding of patients for reperfusion based on an incorrect evaluation of the CC status. These considerations could be extended also for the study of collaterals in the posterior circulation stroke, but at present the literature data are few or missing [16]. Furthermore, d-CTA has a low error rate and a negative result predicts a negative outcome after revascularization without any error, whereas a positive s-CTA predicts a good outcome without errors, although the model should be tested on a wider cohort.
Nevertheless, our study is not without limitations. The small sample size and the lack of a comparison with angiographic imaging (still the gold standard for vascular occlusion detection although it is invasive) are the main limitations of the present study. Furthermore, caution is required when analyzing the clinical outcome through non-randomized studies, due to the numerous biases and confounders that may render any conclusion unreliable.
Further studies are required to confirm these results, but the proposed protocol adapted to a low-speed MDCT scanner, could be of particular interest in hospitals without access to the more up-to-date technology.
References
Badhiwala JH, Nassiri F, Alhazzani W et al (2015) Endovascular thrombectomy for acute ischemic stroke: a meta-analysis. JAMA 314(17):1832–1843
Morelli N, Rota E, Michieletti E, Guidetti D (2017) Mechanical thrombectomy after intravenous thrombolysis for acute ischaemic stroke. Lancet Neurol 16(2):103–104. https://doi.org/10.1016/S1474-4422(16)30379-9
Eswaradass P, Appireddy R, Evans J, Tham C, Dey S, Najm M, Menon BK (2016) Imaging in acute stroke. Expert Rev Cardiovasc Ther 14(8):963–975. https://doi.org/10.1080/14779072.2016.1196134 (Epub 2016 Jun 16. Review)
Nordmeyer H, Webering N, Chapot R, Hadisurya J, Heddier M, Stracke P et al (2017) The association between collateral status, recanalization and long term outcome in stroke patients treated with stent retrievers—are there indications not to perform thrombectomy based on CT angiography? J Neuroradiol 44:217–222. https://doi.org/10.1016/j.neurad.2016.12.009
Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM et al (2015) Multiphase CT angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology 275:510–520. https://doi.org/10.1148/radiol.15142256.
Tan JC, Dillon WP, Liu S, Adler F, Smith WS, Wintermark M (2007) Systematic comparison of perfusion-CT and CT-angiography in acute stroke patients. Ann Neurol 61(6):533–543
Tomsick T, TIMI, TIBI, TICI (2007) I came, I saw, I got confused. AJNR Am J Neuroradiol 28(2):382–384
Bae KT (2010) Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology 256:32–61. https://doi.org/10.1148/radiol.10090908
Olivot JM (2017) Which imaging before reperfusion strategy? Rev Neurol (Paris) 173(9):584–589. https://doi.org/10.1016/j.neurol.2017.09.002 (Epub 2017 Oct 13)
Raymond SB, Schaefer PW (2017) Imaging brain collaterals: quantification, scoring, and potential significance. Top Magn Reson Imaging 26(2):67–75. https://doi.org/10.1097/RMR.0000000000000123
Ginsberg MD (2017) The cerebral collateral circulation: Relevance to pathophysiology and treatment of stroke. Neuropharmacology. https://doi.org/10.1016/j.neuropharm.2017.08.003 (Epub ahead of print)
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD (2015) ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372(11):1019–1030. https://doi.org/10.1056/NEJMoa1414905 (Epub 2015 Feb 11)
Caldwell J, Heran MKS, McGuinness B, Barber PA (2017) Imaging in acute ischaemic stroke: pearls and pitfalls. Pract Neurol 17(5):349–358. https://doi.org/10.1136/practneurol-2016-001569 (Epub 2017 Jul 25)
Campbell BC, Parsons MW (2018) Imaging selection for acute stroke intervention. Int J Stroke 1:1747493018765235. https://doi.org/10.1177/1747493018765235
Flores A, Rubiera M, Ribó M, Pagola J, Rodriguez-Luna D, Muchada M, Boned S, Seró L, Sanjuan E, Meler P, Carcámo D, Santamarina E, Tomassello A, Lemus M, Coscojuela P, Molina CA (2015) Poor collateral circulation assessed by multiphase computed tomographic angiography predicts malignant middle cerebral artery evolution after reperfusion therapies. Stroke 46(11):3149–3153. https://doi.org/10.1161/STROKEAHA.115.010608 (Epub 2015 Sep 29)
Goyal N, Tsivgoulis G, Nickele C, Doss VT, Hoit D, Alexandrov AV, Arthur A, Elijovich L (2016) Posterior circulation CT angiography collaterals predict outcome of endovascular acute ischemic stroke therapy for basilar artery occlusion. J Neurointerv Surg 8:783–786. https://doi.org/10.1136/neurintsurg-2015-011883 (Epub 2015 Aug 17)
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
This is all those who: (1) made a substantial contribution to the concept or design of the work or acquisition, analysis or interpretation of data, (2) drafted the article or revised it critically for important intellectual content, (3) approved the version to be published, (4) each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standards
The study was approved by the Guglielmo da Saliceto Hospital Ethics Committee.
Human and animal rights
Human and animal studies have been approved by local ethics committee and, therefore, have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Specific national laws have been observed, too.
Informed consent
Informed written consent of the patient has been obtained.
Data availability
All data of research materials related to my paper (for example data, samples or models) can be accessed.
Rights and permissions
About this article
Cite this article
Morelli, N., Rota, E., Immovilli, P. et al. Dual-phase 16 slice CT angiography in stroke imaging: a poor man’s multiphase study?. Acta Neurol Belg 119, 187–192 (2019). https://doi.org/10.1007/s13760-018-1019-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-018-1019-4