Abstract
Although repetitive transcranial magnetic stimulation (rTMS) for upper limb motor area in stroke patients is beneficial, it has been poorly investigated in rTMS for leg motor area. Furthermore, no study has examined the usefulness of rTMS for leg motor area in patients in the early phase of stroke. Twenty-one patients with a hemispheric stroke lesion in the early phase were randomly assigned into two groups: the high-frequency (HF)-rTMS group [N = 11] and the sham stimulation group [N = 10]. Patients received rTMS for 5 consecutive days, beginning 10.9 ± 6.6 days on average after the onset. Brunnstrom Recovery Stages (BRS) for the lower limbs and the Ability for Basic Movement Scale Revised (ABMS II) were assessed before and after the intervention. The improvement in BRS for the lower limbs was significant after the intervention in the HF-rTMS group. Although both the HF-rTMS and sham stimulation groups had significant improvements in ABMS II scores, the extent of improvement in the AMBS II was significantly greater in the HF-rTMS group than in the sham stimulation group. Application of HF-rTMS over the bilateral leg motor areas has potential to be a new rehabilitation therapy for patients in the acute phase of stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Repetitive transcranial magnetic stimulation (rTMS) is a non-invasive neuromodulation technique that can produce sustained changes in local neural excitability, depending on the stimulation frequency. High-frequency rTMS (HF-rTMS ≥5 Hz) reportedly activates local neural excitability, whereas low-frequency rTMS (LF-rTMS ≤1 Hz) suppresses local neural excitability [1, 2]. Both HF-rTMS applied to the lesioned upper limb motor area and LF-rTMS applied to the non-lesioned upper limb motor area were beneficial for upper limb hemiparesis in stroke patients [3]. Although most researchers reported the efficacy of rTMS in chronic stroke patients, we previously reported that these two rTMS modalities were beneficial for motor improvement of paretic upper limb, even in the early phase of stroke [4, 5]. Studies of rTMS therapeutic use for the leg motor area are scarce. Kakuda et al. reported that HF-rTMS applied to bilateral leg motor areas using a double-cone coil could improve walking function in chronic stroke hemiparetic patients [6]. However, no information regarding the efficacy or feasibility of rTMS applied to the leg motor area for stroke patients in the early phase is available. It was hypothesized that the same approach should also be effective in the early phase. The purpose of this pilot study was to provide an initial evaluation of the safety and feasibility of therapeutic HF-rTMS, and to clarify whether HF-rTMS is beneficial in terms of motor function recovery of the paretic leg and trunk function in stroke patients in the early phase.
Materials and methods
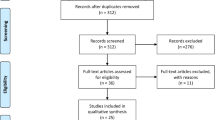
The study subjects included 21 consecutive stroke patients who met all of the following inclusion criteria: (1) emergently admitted to International University of Health and Welfare Atami Hospital within 6 h of onset between April 2014 and March 2015; (2) clinical diagnosis of supratentorial intracerebral hemorrhage (ICH) or subcortical cerebral infarction (CI) in the area of the middle cerebral artery (MCA), without invasion into the cerebral cortex, as confirmed with non-contrast brain computed tomography (CT) or magnetic resonance imaging (MRI); (3) between 25 and 85 years of age at admission; (4) no surgical management, including intravascular surgery, and no administration of tissue plasminogen activator (tPA) as an emergent treatment; (5) started the study intervention within 28 days of admission; (6) no disturbance of consciousness [an eye opening score of 4 and best verbal response of 5 on the Glasgow Coma Scale (GCS)]; (7) no active physical or mental illness requiring medical management; (8) no development of convulsion after onset; (9) no pathological conditions known to be contraindications for rTMS in the guidelines suggested by Wassermann (e.g., cardiac pacemakers, intracranial implants, implanted medication pumps, or pregnancy) [7, 8]; and (10) no prior experience with rTMS application (to confirm blindness to the intervention).
The study was a randomized controlled trial, and the study patients were randomly assigned to the HF-rTMS group (N = 11) or the sham stimulation group (N = 10) according to the date of admission. The sample size used in this study was determined based on the total number of patients enrolled in the study period mentioned above. Since this study was a pilot study intended to investigate the efficacy of HF-rTMS, we did not perform any power analyses.
All patients in the 2 groups were scheduled to receive 2 sessions (AM/PM) of HF-rTMS or sham stimulation per day for 5 consecutive days (10 sessions in total) as in-patient treatment. Motor function of the paretic leg and trunk function were evaluated serially before and after the 5-day treatment protocol, and the extent of improvement in the assessments were compared between the two groups.
Application of HF-rTMS and sham stimulation
For rTMS delivery, an 80-mm double-cone coil and a MagPro R30 stimulator (MagVenture Company, Farum, Denmark) were used. For HF-rTMS, 10-s trains of 10 Hz were applied repeatedly with 50-s inter-train intervals (ITIs) over 10 min (1000 pulses per session). The stimulation site on the skull was defined as the position on the midsagittal plane where the stimulation evoked most apparent visible dorsiflexion movement of the intact ankle. The center of contact between the two circles of the coil was placed vertically over the determined stimulation site on the midsagittal plane, so that the bilateral leg motor areas could be stimulated simultaneously and at the same intensity (Fig. 1). The resting motor threshold (RMT) was defined as the minimum output of stimulation that evoked target movement of the ankle. The HF-rTMS intensity was 90 % of the RMT at the stimulation site. Sham stimulation was performed with a pseudo-coil that was not connected to the stimulator. Patients in the sham group received only recorded sounds of 10-Hz stimulus from a speaker for 10 min. During the rTMS session, patients sat in a reclining wheelchair with their heads strapped to the headrest. In terms of safety, patients were monitored clinically through medical and neurological examination during the study period. Vital signs, including blood pressure, heart rate, and consciousness level, were assessed before and after each rTMS session. According to the hemiparesis severity, conventional rehabilitation programs, such as range-of-motion exercise, muscle exercise, sitting and/or standing training, and gait training for 40–80 min, were provided daily for all patients during the study period by therapists who were blind to the allocation of studied groups. They also received medical treatment such as anti-hypertensive agents for blood pressure control and anti-coagulant/anti-platelet therapy for secondary prevention.
Photograph of high-frequency repetitive transcranial magnetic stimulation (HF-rTMS) application using a double-cone coil. The center of the contact between the two circles of the coil was placed vertically over the determined stimulation site on the midsagittal plane so that the bilateral leg motor areas could be stimulated simultaneously and at the same intensity
Clinical measures of motor function in the paretic leg and trunk function
Motor function of the paretic leg was evaluated using the Brunnstrom Recovery Stages (BRS) for the lower limbs, and trunk function was evaluated using the Ability for Basic Movement Scale Revised (ABMS II) [9]. Immediately before the first application and immediately after the last application of HF-rTMS or sham stimulation, these evaluations were performed by a physical therapist in our department who was blind to the allocation and provided no training to the patient to ensure a bias-free outcome evaluation. The Mini-Mental State Examination (MMSE) was administered to all patients to evaluate cognitive function immediately before the first intervention by an occupational therapist in our department who was also blind to the allocation of the patients.
Statistical analyses
Data are expressed as mean ± standard deviation (SD). Clinical characteristics before the intervention and baseline motor function between the two groups were compared using unpaired t tests for parametric data (age, days between onset, and rehabilitation/rTMS), the Mann–Whitney U test for non-parametric data (BRS, ABMS II, MMSE), and the Chi-square test for categorical data (gender, subtype of stroke, and cerebral lesion side). In each patient group, significant changes in BRS and ABMS II following the intervention were analyzed using the Wilcoxon signed-rank test. Following the intervention, the Mann–Whitney U test was performed to compare the extent of improvement (100* [post-intervention – pre-intervention)/pre-intervention (%)] in ABMS II between the two groups. All statistical analyses were performed using SPSS version 19 (SPSS Inc., Chicago, IL). A p value less than 0.05 was considered to be statistically significant.
Results
Twenty-one patients were enrolled in the study during the study period; 11 and 10 stroke patients in the early phase were assigned to the HF-rTMS group and the sham stimulation group, respectively. All patients completed the study protocol. No patient experienced any pathological symptoms or deterioration of neurological symptoms. None of the patients were able to recognize the protocol they were receiving during the rTMS session, since no one had experienced rTMS before entry into the study and none had detailed knowledge of rTMS. Clinical characteristics of the study patients in both groups are presented in Table 1. For all studied patients, the age at admission was between 25 and 83 years (mean, 61.4 ± 13.7 years), and the time between admission and intervention ranged from 4 to 26 days (mean, 10.9 ± 6.6 days). The diagnosis was confirmed by a brain CT or MRI as cerebral infarction in 11 patients and intracerebral hemorrhage in 10 patients. The differences in the clinical characteristics of the two groups were insignificant. Moreover, differences in the clinical measures of motor function and cognitive function for the two groups before the intervention were insignificant.
BRS for the lower limb was significantly improved in the HF-rTMS group (from 3.3 ± 1.3 to 4.7 ± 1.3; p < 0.01), although it was not changed in the sham stimulation group (from 3.5 ± 1.6 to 3.8 ± 1.5). The ABMS II score was significantly improved in both the HF-rTMS group and the sham stimulation group (from 17.5 ± 4.5 to 25.2 ± 4.3 in the HF-rTMS group; from 18.4 ± 4.8 to 21.8 ± 5.1 in the sham stimulation group; all p < 0.01) (Table 2). However, the extent of improvement in the ABMS II was significantly greater in the HF-rTMS group than in the sham stimulation group (48.7 ± 30.0 in the HF-rTMS group; 20.2 ± 17.4 in the sham stimulation group, p < 0.05) (Fig. 2).
Discussion
Previous reports showed the positive effects of rTMS for improving upper limb hemiparesis in stroke patients [10, 11]. While the upper limb motor area is located in the dorsal cerebral cortex, the leg motor area is located deep inside the longitudinal cerebral fissure. An 8-figured coil is generally used for rTMS; however, it is difficult for the 8-figured coil magnetic field to stimulate the leg motor area, which is located 3 to 4-cm deep from the scalp surface. Even with the 8-figured coil, it is not impossible to stimulate the leg motor area when the output of the coil is set higher. However, since the magnetic field widely stimulates the scalp surface in such cases, the examinees often cannot tolerate the pain of the stimulation, and the locality of the stimulation is decreased. On the other hand, it was confirmed that the double-cone coil used in the present study has a well-balanced design that produces localized stimulation in deep areas of the brain [12]. Some previous studies showed that stimulation with a double-cone coil reached the leg motor area [13, 14], and our present study provided additional evidence; the stimulation delivered by the double-cone coil evoked visible dorsiflexion movement of the intact ankle.
The aim of therapeutic rTMS for upper limb hemiparesis is to enhance the cortical activity of the upper limb motor area on the lesioned side. Two modalities of rTMS have been devised: one directly activates the upper limb motor area on the lesioned side with HF-rTMS, and the other activates the upper limb motor area on the lesioned side indirectly via interhemispheric inhibition (IHI) by suppressing the upper limb motor area on the non-lesioned side with LF-rTMS. HF-rTMS and LF-rTMS application resulted in beneficial effects following introduction in both the chronic [3] and early phases of stroke [4]. Furthermore, simultaneous application of the two rTMS modalities resulted in greater efficacy in the chronic [15] and early phases [5]. However, unlike the upper limb motor area, the right and left leg motor areas are located in close proximity to each other on the medial side of the longitudinal cerebral fissure, and it is difficult to use these two modalities of rTMS separately.
It is known that 20–30 % of the pyramidal tract has ipsilateral control, which dominates the body trunk and proximal limbs. In stroke cases with hemiparesis, the body trunk and proximal limbs of the non-paretic side are not healthy; these muscles are bilaterally affected [16], although more strongly on the side contralateral to the brain lesion, and muscle strength recovers bilaterally during the acute phase [17]. A functional MRI study reported that increased cortical activity in the bilateral leg motor areas was involved in the improvement of voluntary movement of the paretic leg [18]. According to these reports, we hypothesized that HF-rTMS for bilateral leg motor areas would be beneficial for improving function of the body trunk and paretic leg. This method is reportedly effective for patients with hemiparesis in the chronic phase of stroke [6].
After the 5-day intervention, BRS for the lower limbs significantly improved in the HF-rTMS group. The BRS is a 6-grade non-parametric scale that tends to cause a ceiling effect. The present study was a pilot study that included a limited number of cases; therefore, hemiparesis severity was not an inclusion criteria variable. However, it was necessary to employ an additional assessment that was unlikely to be subject to the ceiling effect. For the HF-rTMS and sham stimulation groups, in which the average paresis severity was comparable before the intervention, BRS for the lower limbs was improved following intervention only in the HF-rTMS group. We therefore speculate that the results of motor recovery were attributable to the positive effects of HF-rTMS.
Bilateral leg motor areas were activated in this study, but it remains unclear if the lesioned or non-lesioned side was more influenced by this intervention. For example, some children acquired the ability to walk after resection and hemispherectomy [19]. Therefore, re-organization of the ipsilateral pyramidal tract might be greater than expected in the early phase due to high plasticity. However, compensation by the ipsilateral pyramidal tract may be limited. It is necessary to verify the changes using functional brain images to determine the paresis severity prior to intervention.
Body trunk function is a critical element of the physical outcome in stroke patients [20]. ABMS II significantly improved in both groups after the 5-day intervention, and the extent of change in the ABMS II was significantly higher in the HF-rTMS group. The ABMS II consists of 6 non-parametric grades for 5 body trunk function subtests, with a perfect score of 30 points [9]. Since the total score range is wide (i.e., 5–30 points), and only a few cases reached 30 points, we speculate that the influence of the ceiling effect was minimal.
The current study had some limitations. Firstly, this was a randomized controlled study; however, the number of patients enrolled was small. Therefore, the findings of this study should be confirmed with a larger patient sample. Secondly, we did not apply any neuroimaging techniques, such as functional (f)MRI or positron emission tomography (PET) in this study. Neuroimaging techniques should be applied to investigate the difference in functional neural reorganization with the intervention between two groups. Thirdly, the studied patients represented a heterogeneous group with regard to stroke type and baseline stroke severity. Differences in the beneficial effect of HF-rTMS should be assessed among various types of stroke and stroke severity. In addition, the final evaluation was performed immediately after the final session of rTMS. Therefore, the difference between two groups might disappear or get smaller in their chronic phase. In other words, it remains unknown whether our rTMS protocol could produce a greater functional recovery compared to sham stimulation or only accelerated the rate of such recovery. Future study with longer follow-up period is needed to clarify this issue.
Conclusion
Our proposed HF-rTMS protocol using a double-cone coil is a safe and feasible intervention for motor function recovery of the paretic leg and trunk function in patients with stroke in the early phase. Since improvements in sitting and standing are prioritized in stroke patients during the early phase, this approach is considered markedly important because improvement in the capacity of the proximal leg areas to the body trunk is expected.
References
Butler AJ, Wolf SL (2007) Putting the brain on the map: use of transcranial magnetic stimulation to assess and induce cortical plasticity of upper-extremity movement. Phys Ther 87:719–736
Lefaucheur JP (2006) Stroke recovery can be enhanced by using repetitive transcranial magnetic stimulation (rTMS). Neurophysiol Clin 36:105–115
Hsu WY, Cheng CH, Liao KK, Lee IH, Lin YY (2012) Effects of repetitive transcranial magnetic stimulation on motor functions in patients with stroke: a meta-analysis. Stroke 43:1849–1857
Sasaki N, Mizutani S, Kakuda W, Abo M (2013) Comparison of the effects of high- and low-frequency repetitive transcranial magnetic stimulation on upper limb hemiparesis in the early phase of stroke. J Stroke Cerebrovasc Dis 22:413–418
Sasaki N, Kakuda W, Abo M (2014) Bilateral high- and low-frequency rTMS in acute stroke patients with hemiparesis: a comparative study with unilateral high-frequency rTMS. Brain Inj 28:1682–1686
Kakuda W, Abo M, Nakayama Y, Kiyama A, Yoshida H (2013) High-frequency rTMS using a double cone coil for gait disturbance. Acta Neurol Scand 128:100–106
Wassermann EM (1998) Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5–7, 1996. Electroencephalogr Clin Neurophysiol 108:1–16
Rossi S, Hallett M, Rossini PM, Pascual-Leone A, Safety of TMS Consensus Group, Safety of TMS Consensus Group (2009) Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol 120:2008–2039
Tanaka T, Hashimoto K, Kobayashi K, Sugawara H, Abo M (2010) Revised version of the ability for basic movement scale (ABMS II) as an early predictor of functioning related to activities of daily living in patients after stroke. J Rehabil Med 42:179–181
Hoyer EH, Celnik PA (2011) Understanding and enhancing motor recovery after stroke using transcranial magnetic stimulation. Restor Neurol Neurosci. 29:395–409
Corti M, Patten C, Triggs W (2012) Repetitive transcranial magnetic stimulation of motor cortex after stroke: a focused review. Am J Phys Med Rehabil 91:254–270
Deng ZD, Lisanby SH, Peterchev AV (2014) Coil design considerations for deep transcranial magnetic stimulation. Clin Neurophysiol 125:1202–1212
Stokić DS, McKay WB, Scott L, Sherwood AM, Dimitrijević MR (1997) Intracortical inhibition of lower limb motor-evoked potentials after paired transcranial magnetic stimulation. Exp Brain Res 117:437–443
Terao Y, Ugawa Y, Hanajima R, Machii K, Furubayashi T, Mochizuki H, Enomoto H, Shiio Y, Uesugi H, Iwata NK, Kanazawa I (2000) Predominant activation of I1-waves from the leg motor area by transcranial magnetic stimulation. Brain Res 859:137–146
Yamada N, Kakuda W, Kondo T, Shimizu M, Mitani S, Abo M (2013) Bihemispheric repetitive transcranial magnetic stimulation combined with intensive occupational therapy for upper limb hemiparesis after stroke: a preliminary study. Int J Rehabil Res 36:323–329
Andrews AW, Bohannon RW (2000) Distribution of muscle strength impairments following stroke. Clin Rehabil. 14:79–87
Andrews AW, Bohannon RW (2003) Short-term recovery of limb muscle strength after acute stroke. Arch Phys Med Rehabil 84(1):125–130
Enzinger C, Dawes H, Johansen-Berg H, Wade D, Bogdanovic M, Collett J, Guy C, Kischka U, Ropele S, Fazekas F, Matthews PM (2009) Brain activity changes associated with treadmill training after stroke. Stroke 40:2460–2467
Wieser HG, Henke K, Zumsteg D, Taub E, Yonekawa Y, Buck A (1999) Activation of the left motor cortex during left leg movements after right central resection. J Neurol Neurosurg Psychiatry 67:487–491
Morgan P (1994) The relationship between sitting balance and mobility outcome in stroke. Aust J Physiother 40:91–96
Acknowledgments
Funding for this study was provided by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (2014).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Ethical standards
Ethics committee at International University of Health and Welfare Atami Hospital approved the study protocol.
Informed consent
Informed consent was obtained from each patient before entry into the study.
Rights and permissions
About this article
Cite this article
Sasaki, N., Abo, M., Hara, T. et al. High-frequency rTMS on leg motor area in the early phase of stroke. Acta Neurol Belg 117, 189–194 (2017). https://doi.org/10.1007/s13760-016-0687-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-016-0687-1





