Abstract
Little has been reported regarding aortic–enteric fistula (AEF) as a complication of gynecologic cancers because of its rarity. However, since it is lethal if left untreated, medical practitioners involved with gynecologic diseases should be aware of this deadly condition. In our hospital, we encountered two cases of cervical cancer complicated by AEF. In both cases, contrast computed tomography (CT) revealed leakage of the contrast material from an artery into the small intestine, indicating AEF. Endovascular procedures with complete embolization of the affected arteries and femoro-femoral artery bypass (f-f bypass) were performed in the hybrid operation room. The activities of daily living improved dramatically for both patients, and they survived for 3 months before dying from cervical cancer. While embolization by endovascular methods and f-f bypass performed in a hybrid operation room is, therefore, an available option for treating AEF, literature is lacking and more research is required to improve long-term outcomes for this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arterio-enteric fistula (AEF) leads to death by hemorrhage if left untreated [1]. Little has been reported regarding AEF in gynecologic cancer patients because of its rarity [2]. Although AEF is traditionally managed by graft explantation, aortic stump closure, and revascularization, less invasive treatments are desirable (Kakkos 2016). Recently, endovascular methods have been attempted for embolization of the artery. Femoro-femoral artery bypass (f-f bypass) is performed to allow blood flow to the affected areas and to prevent ischemia. Because AEF requires immediate treatment, embolization and f-f bypass should be performed in the hybrid operation room, which is equipped with imaging devices such as X-ray and CT, allowing surgeons to quickly assess blood flow. We report two AEF cases that occurred in cervical cancer patients, and we argue that embolization and f-f bypass in the hybrid operation room can help prolong survival.
Cases presentation
Case 1
A 28-year-old female, gravida 0, was diagnosed with stage IB1 cervical cancer, adenosquamous carcinoma. Chemotherapy, radical hysterectomy and pelvic lymph node dissection, and adjuvant concurrent chemoradiotherapy (CCRT) were conducted. One month later, SCC level in the blood was high, and fluorine-18 deoxyglucose (FDG) accumulated at right obturator lymph nodes and para-aortic lymph nodes, suggesting recurrence. The patient visited our department. Because metastases in the right external iliac lymph nodes, the right obturator lymph nodes, and the liver were identified, chemotherapy was performed.
Four months later, bloody stool and loss of consciousness occurred. Blood pressure was immeasurable. Pulse rate was 140 beats per minute (bpm). Blood hemoglobin level was 2.9 mg/dL. Contrast computed tomography (CT) revealed leakage from the right external iliac artery to the ileocecal region of the small intestine (Fig. 1a). It was thought that metastasis at the right obturator lymph nodes led to perforation of the right external iliac artery and the small intestine. Interventional radiology was conducted to place a stent in the right external iliac artery to close the fistula (Fig. 1b, c). 20 units of red blood cells, 14 units of fresh frozen plasma and 20 units of platelets were administered. Three weeks later, bloody excrement reappeared. Systolic blood pressure was 100 mmHg, pulse rate 170 bpm. Blood hemoglobin level was 5.0 mg/dL. Contrast CT showed leakage of contrast material from the location of the stent (Fig. 1d). We suspected that infection caused the right external iliac artery’s wall to become fragile and the stent expanded, putting pressure on the fistula, causing hemorrhage. We performed coil embolization of the right common, external and internal iliac arteries, and femoro-femoral artery bypass (f-f bypass) in a hybrid operation room (Fig. 1e, f). Angiography revealed that the right external iliac artery, at the site of the stent, had expanded and led to hemorrhage (Fig. 1e). A stent graft was placed inside the arteries, from aorta to left common iliac artery, to block blood flow into right common iliac artery (Fig. 1f). F-f bypass was created between the left and the right external iliac arteries. 14 units of red blood cells, eight units of fresh frozen plasma, and 30 units of platelets were administered.
Contrast CT images and angiographies of Case 1. a Contrast CT showed that contrast material was leaking from the right external iliac artery to the ileocecal region of the small intestine. b Before the stent was placed, angiography showed the leakage of contrast material from the right external iliac artery to the surrounding region (arrow heads). c After the stent was placed, the leakage stopped (arrows and red meshing pattern). d Three weeks after the first treatment, contrast CT revealed the leakage of the contrast material from the part of the right iliac artery where the stent was placed. e Angiography revealed that the blood vessel surrounding the stent has expanded, presumably because infection made the wall fragile and the pressure of the stent pushed the walls outward (arrow heads). e Coil embolization (arrow heads), placement of a stent graft inside the artery from aorta to left common iliac artery (arrows), and f-f bypass (empty arrows) were performed
Following the surgery, the patient managed to walk and eat, and was discharged from our hospital. She died 3 months later because of the cervical cancer.
Case 2
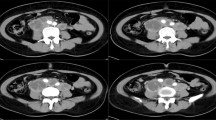
A 37-year-old female, gravida 3, para 2, presented with pain during sexual intercourse and lower abdominal pain, at a gynecology clinic. Cytology and biopsy of the uterine cervix indicated squamous-cell carcinoma (SCC). She visited our department for detailed examinations. Internal examination revealed cancer in the uterine cervix and its invasion into the left parametrium. CT revealed left hydronephrosis and lymphadenopathy in the left obturator and bilateral internal iliac regions. Cystoscopy revealed invasion of the cancer into the urinary bladder. The diagnosis was cervical cancer, SCC, stage IVA. CCRT, abdominal total hysterectomy and bilateral salpingo-oophorectomy were performed. From 7 months after the surgery, for 3 years and 9 months, chemotherapy, radiotherapy, and tumor resection were repeatedly performed. Six years after the initial surgery, the patient presented with lower abdominal pain, bloody stool, and dizziness. Blood pressure was 83/51 mmHg. Pulse rate was 100 bpm. Blood hemoglobin level was 7.9 mg/dL. Contrast CT revealed leakage into the small intestine (Fig. 2a). She was diagnosed with intestinal vascular fistula and was moved into the hybrid operation room. Angiography revealed leakage of the contrast material from the right external iliac artery to the small intestine (Fig. 2b). Embolization of the right common, external and internal iliac arteries and f-f bypass were conducted. A stent graft was placed inside the arteries, from aorta to left common iliac artery, to block blood flow into the right common iliac artery (Fig. 2c). Ligation of the right external iliac artery at the distal region of embolization was performed to prevent backflow of blood through the f-f bypass to the right external iliac artery (Fig. 2c); 14 units of red blood cells and 10 units of fresh frozen plasma were administered.
Contrast CT images and angiographies of Case 2. a Contrast CT revealed the presence of the contrast material in the small intestine, suggesting leakage from the nearby artery. b Before embolization was performed, angiography revealed the leakage of the contrast material from the right external iliac artery to the small intestine (arrow heads). c Embolization of the right common, external, and internal iliac arteries were performed (arrow heads) together with f-f bypass, and a stent graft was placed in the aorta and left common iliac artery (arrows). Ligation of the right external iliac artery at the distal region of embolization was also performed (circle)
Nineteen days after the surgery, she was discharged from our hospital. She managed to spend time at home with her family and died from cervical cancer 3 months after the surgery.
Discussion
AEF is a condition in which an artery and a part of the digestive tract are in contact with each other and perforation occurs between them, leading to hemorrhage [3]. If left untreated, its mortality rate is 100% [1]. AEF is classified as primary or secondary: primary AEF is caused by an underlying disease, usually at the intestine or a blood vessel; secondary AEF is caused by complications involving artificial blood vessels [3]. The annual incidences of primary and secondary AEF are estimated to be 0.004–0.007 and 0.69–2.36% respectively [3]. Few papers have been published about AEF: the number of patients known to have been afflicted with secondary abdominal AEF between 1999 and 2015 is only 823 [2]. Common symptoms of AEF include abdominal pain, fever, bleeding, and shock [4]. When AEF is suspected, CT scan may be useful for diagnosis [4]. Extravasation of contrast material into the bowel is suggestive of AEF, as in the two cases mentioned above [1].
Our two patients underwent CCRT before developing AEF. It is known that radiation treatment leads to endoarteritis, which may then lead to hypoxia, fibrosis, and necrosis, thus increasing the risk of fistula formation [5]. According to a study, of the 23 stage IVA cervical cancer patients who received either CCRT or radiation therapy alone, five were subsequently diagnosed with vesicovaginal or rectovaginal fistula [6]. Literature regarding AEF and CCRT appears to be lacking, but such occurrence of fistula within an irradiation area suggests that CCRT is risk for AEF on cervical cancer patients who received whole pelvic irradiation. The effect of chemotherapy on fistula formation is unclear. Moreover, there is not enough information to determine whether the AEF occurred in the two patients because of metastasis alone or because of complications caused by CCRT.
AEF is treated by closing the fistula to control hemorrhage and sepsis [2]. Embolization is useful; since it causes ischemia, blood must be supplied from other regions [2], one method being femoro-femoral (f-f) bypass.
F-f bypass involves subcutaneous or subfascial tunnel, where a graft is placed to connect the damaged vessel to a healthy vessel [7]. The patency rate for femoro-femoral grafts is estimated to be 75–86% [7, 8]. Complications following f-f bypass include hematomas, graft occlusion, and infections. Hematomas may be resolved through conservative treatment; infections are treated with partial graft excision, debridement, and antibiotics [9]. Extra-anatomic bypass graft infection is relatively uncommon 1–8.7%. However, mortality rate may be as high as 45%. Occlusions may require additional bypasses [10]. In one case, a patient was infected with methicillin-resistant Staphylococcus aureus, leading to anastomic breakdown and hemorrhage, causing the bypass graft to be removed and replaced with another one, but the patient died of sepsis [10]. Thus, while complications of f-f bypass may be treatable, death may occur.
The prevention of the complications including infection is critical after the treatments against AEF. In case 1, when graft explantation was performed, hemorrhage and infection occurred. Thus, complete occlusion was considered necessary. In both case 1 and case 2, the internal, external and common iliac arteries were embolized completely by coiling. A stent graft was then placed inside the aorta and the unaffected common iliac artery to block blood flow into the affected common iliac artery. By reviewing case 1, we decided that we should strive to relieve the fistula from the extra blood pressure caused by the blood from the f-f bypass back flowing towards the fistula after reaching the affected artery. Thus in case 2, the affected external iliac artery was ligated at the area distal to the embolization to prevent such back flow. We have seen that these procedures are effective in prolonging survival and improving activities of daily living of patients afflicted with AEF.
AEF requires immediate treatment because of its lethality. Mortality rate, even if treatment is performed, is reported to be 50–80%. 20% of the deaths occur during the operation, and 26% within 30 days after the surgery [1, 11, 12]. Although a hybrid operating room requires many medical staffs, including cardiovascular surgeons, radiologists, anesthesiologists, radiological technologists, and nurses, it allows embolization and f-f bypass to be performed simultaneously using imaging devices, thus saving time and contributing to the improvement of survival rates for AEF patients. Even if a hospital lacks a hybrid operation room, AEF may still be treated by performing embolization in a room where angiography is possible, and after the patient’s vital signs stabilize, the patient may then be taken to an operation room for f-f bypass.
In summary, complete embolization of AEF and the surrounding arteries is important in preventing repetitious hemorrhage and persistent infection. A hybrid operating room is useful for performing embolization and f-f bypass. However, literature is lacking regarding the risk factors for the long-term outcomes of treatment for AEF caused by gynecologic cancer, let alone cervical cancer. More follow-ups need to be done for this rare but life-threatening condition.
References
Mathias J, Mathias E, Jausset F et al. Aorto-enteric fistulas: a physiopathological approach and computed tomography diagnosis. Diagn Interv Imaging. 2012;93:840–51
Kakkos SK, Bicknell CD, Tsolakis IA et al. Editor’s choice—management of secondary aorto-enteric and other abdominal arterio-enteric fistulas: a review and pooled data analysis. Eur J Vasc Endovasc Surg. 2016;52:770–86
Minemura S, Matsumura T, Arai M et al. A primary arterio enteric fistula with Takayasu arteritis. Intern Med. 2013;52:359–62
Çiçek Ö, Çiçek MC, Kadiroğulları E et al (2016) Successful treatment of secondary aortoenteric fistula with a special graft. Case Rep Med 2016:9874187
Angioli R, Penalver M, Muzii L et al (2003) Guidelines of how to manage vesicovaginal fistula. Crit Rev Oncol Hematol 48:295–304
Biewenga P, Mutsaerts MA, Stalpers LJ et al (2010) Can we predict vesicovaginal or rectovaginal fistula formation in patients with stage IVA cervical cancer? Int J Gynecol Cancer 20:471–475
Blaisdell FW (2011) Development of femoro-femoral and axillo-femoral bypass procedures. J Vasc Surg 53:540–544
Fahal AH, McDonald AM, Marston A. Femorofemoral bypass in unilateral iliac artery occlusion. Br J Surg. 1989;76:22–5
de Virgilio C, Cherry KJ, Gloviczki P et al. Infected lower extremity extra-anatomic bypass grafts: management of a serious complication in high-risk patients. Ann Vasc Surg. 1995;9:459–66
Walker SR, Braithwaite B, Tennant WG et al. Early complications of femorofemoral crossover bypass grafts after aorta uni-iliac endovascular repair of abdominal aortic aneurysms. J Vasc Surg. 1998;28:647–50
Policha A, Baldwin M, Mussa F, Rockman C (2015) Iliac artery-uretero-colonic fistula presenting as severe gastrointestinal hemorrhage and hematuria: a case report and review of the literature. Ann Vasc Surg 29:1656.e1–6
Budimir I, Nikolić M, Supanc V et al (2012) Secondary arterio-enteric fistula: case report and review of the literature. Acta Clin Croat 51:79–82
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Mikami, T., Yamaguchi, K., Sawayama, S. et al. Two cases of recurrent uterine cervical cancer with arterio-enteric fistula treated by femoro-femoral artery bypass in hybrid operation room. Int Canc Conf J 7, 26–29 (2018). https://doi.org/10.1007/s13691-017-0312-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-017-0312-z