Abstract
Fibroadenoma is a common benign breast lesion that usually affects women in their second and third decade of life and usually present as small mobile painless lump. However, it is important to recognize that a small percentage have been shown to progress to giant fibroadenomas. Giant fibroadenomas can undergo infarction leading to significant morbidity and difficulty to distinguish from the more aggressive phyllodes tumors or carcinoma. We report an interesting case of giant fibroadenoma (17 × 11 × 7 cm) with massive infarction during lactation, further complicated by lactational mastitis with close resemblance to cystosarcoma phyllodes. Detailed clinical evaluation and proper investigation in the form of USG breast and PET–CT scan helped us to delineate the nature of pathology. Simple excision of lesion with curvilinear incision was done with excellent cosmetic outcome. Histopathologic features were consistent with fibroadenoma (giant) with large areas of infarction. Fibroadenoma breast has varied clinical presentations. The course of disease may be complicated by pregnancy, lactation and inflammatory processes. Massive infarction may make the picture more dubious and masquerade with malignant transformation altering our treatment decision. The presence of necrosis on core biopsy or intra-operative finding should be cautiously interpreted and is not itself a sign of malignancy. Detailed clinical evaluation and comprehensive workup should be done before embarking on radical treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibroadenomas are the most common benign breast tumors in young women in their 20s and 30s and have varied presentations ranging from small painless mobile breast lump (“breast mouse”) to rapidly enlarging and fungating mass replacing the entire breast parenchyma mimicking malignancy. Rapid increase in size is usually due to infarction or hemorrhage within tumor which is a rare phenomenon [1, 2]. Infarctions usually occur during pregnancy, lactation and following FNAC or trauma. The giant fibroadenoma (size > 5 cm or tumor weight > 500 g) [3, 4] and cystosarcoma phyllodes are two diseases of the breast which can be thought of as differential diagnoses for huge breast lumps. Preoperatively, it is important to differentiate between them, because of the variation in their presentation and pathology which determine their treatment modalities. We present herein an interesting report of giant fibroadenoma with massive infarction replacing the entire breast in a young woman. She was lactating and had a baby of about one and half months. Clinical and radiological features were more inclined towards a diagnosis of cystosarcoma phyllodes. She was offered total mastectomy at another cancer centre. Further detailed evaluation helped us to exclude malignancy and formulate the treatment plan saving a cosmetically acceptable breast.
Case summary
Twenty-nine year old lady with one and half month old baby presented to us with complaint of rapidly increasing left breast lump over last few months of pregnancy and postpartum period. Detailed history revealed that she had a small, mobile palpable lump in the same breast for about 18 months which was slowly increasing in size during pregnancy. She was investigated for the same at another centre and underwent one attempt of FNAC and one attempt of core biopsy with no definite opinion for tissue diagnosis. She developed lactation mastitis on the same side as the lump in postpartum period and responded to antibiotics and milk suppressive medication as for as inflammatory features were concerned but lump started growing rapidly. When she presented to us, there was no clinical evidence of active inflammatory process. Examination showed a breast lump of about 15 × 10 cm compressing the residual parenchyma to one side. The lump was well-defined, firm in consistency, non-tender, smooth surface, not adhered to chest wall or skin. Skin overlying lump was stretched, shiny and had several dilated veins (Fig. 1a). USG breast showed large heterogeneous mass (17 × 11 × 7 cm) extending from parasternal margin till the anterior axillary line. Nipple was displaced inferiorly with thickening of skin and subcutaneous tissue. Multiple intervening cystic clefts were identified in the lump. On Doppler study, few tiny vessels were noted in the solid areas. USG/Doppler appearance of mass was strongly suspicious of phyllodes tumor. USG guided core-needle biopsy from solid area revealed predominantly necrosis; no viable tissue was seen. Whole-body PET/CT scan was also performed to ascertain biological behavior of lesion. PET–CT scan unveiled lobulated cystic mass with mildly FDG-avid thin nodular septation and small enhancing solid component. Differential diagnoses suggested were ranging from benign to malignant etiology comprising of galactocele/phyllodes tumor/malignancy/antibioma (Fig. 1b).
Clinico-radiological pictures of large infarcted fibroadenoma; a huge well-defined, firm, non-tender lump with smooth surface compressing the residual parenchyma. Skin overlying the lump is stretched, shiny with several dilated veins b PET–CT scan: lobulated cystic mass with small enhancing solid component c intra-operative picture d gross specimen
Based on the clinical and radiological inputs, an impression of organized galactocele was rendered. Patient was taken up for surgery and curvilinear incision was given to deliver the lump. A large, well encapsulated solid-cystic lesion with areas of necrosis was seen. (Fig. 1c) Thick purulent material was aspirated and entire lump was excised along with intact capsule (Fig. 1d).
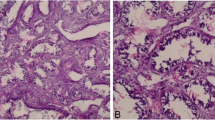
Histopathologic examination showed large area of central necrosis with few preserved areas showing a lesion comprising of epithelial elements with tubular adenosis, cystic changes and apocrine metaplasia. Surrounding stroma showed hyalinization, myxoid changes and mild increase in cellularity. Overall features were consistent with fibroadenoma (giant) with large areas of infarction (Figs. 2, 3). Excellent cosmetic result was achieved at three month postoperatively.
Discussion
Fibroadenomas are the most common benign tumors of the breast that usually affect premenopausal women but may occur at any age. Diagnosis of fibroadenoma may rarely pose a diagnostic dilemma, even on FNA, core biopsy or frozen section. Infarction within fibroadenoma is a very rare event and the frequency of infarction reported in different series varies from 0.3 to 3.6% [5,6,7,8].
The pathogenesis of this complication of fibroadenoma of the breast needs to be explored but remains obscure by now. Common inciting factors for infarction of fibroadenoma are pregnancy, lactation, thrombo-occlusive diseases, trauma and even FNAC of lesion [9,10,11,12,13].
Clinically, an infarcted fibroadenoma is likely to be mistaken for an inflammatory lesion because of rapid enlargement with pain and tenderness, or for malignancy because of fixation of the mass and lymphadenopathy [14,15,16,17]. Differential diagnosis to be considered would include mastitis, duct ectasia, and even carcinoma on aspiration cytology [17,18,19,20]. It is of utmost clinical significance to distinguish fibroadenoma with infarction from phyllodes tumor or carcinoma. It is important to recognize infarction of a fibroadenoma which is a close clinical differential with phyllodes tumor or carcinoma. In the evolution of surgical practice when most of the decisions were taken solely on clinical acumen, this close resemblance of infarcted fibroadenoma with malignancy lead to mastectomy [11]. Detailed clinical evaluation and utilization of the presently available ancillary diagnostic modalities can help us to exclude malignancy avoiding a mentally and physically devastating procedure as mastectomy. Review of literature brought into light a few case reports where avoidable mastectomies were performed for similar clinical scenario [11, 21, 22]. The clinical presentation in our case was classical for phyllodes tumor. She was offered mastectomy at another cancer centre. Pre-existent lesion, rapid increase in size during lactation and complete necrosis on core-needle biopsy raised the possibility of benign nature of this breast lump. This prompted us to evaluate further with metabolic study as PET–CT scan which helped to rule of malignancy as first differential. Definitive diagnosis was further complicated by development of lactational mastitis in this particular case which raised the possibility of organized galactocele or antibioma as clinical diagnosis.
Infarction of a fibroadenoma should be suspected if a young woman presents with a painful, rapidly enlarging breast lump during pregnancy or lactation. Because skin tethering and axillary lymphadenopathy which may be associated with this condition, can be mistaken clinically for carcinoma. However, histologically, the possibility of confusion with carcinoma is less likely, especially if the diagnosis of malignancy is made only when viable tumor tissue is identified. Treatment by local excision is adequate for this lesion and under no circumstances should mastectomy be performed without histological proof of malignancy.
Conclusion
Fibroadenoma breast has varied clinical presentations. The course of disease may be complicated by pregnancy, lactation and inflammatory processes. Massive infarction may make the picture more dubious and masquerade with malignant transformation altering our treatment decision. The presence of necrosis on core biopsy or intra-operative finding should be cautiously interpreted and is not itself a sign of malignancy. Detailed clinical evaluation and comprehensive workup should be done before embarking on radical treatment.
References
Skenderi F, Krakonja F, Vranic S (2013) Infarcted fibroadenoma of the breast: report of two new cases with review of the literature. Diagn Pathol 8:38
Ji Hoon Yu, Kim Min Jeong, Cho Hyonil et al (2013) Breast diseases during pregnancy and lactation. Obstet Gynecol Sci 56(3):143–159
Greydanus DE, Matytsina L, Gains M (2006) Breast disorder in children and adolescent. Prim Care 33(2):455–502
Raganoonan C, Fairbain JK, Williams S, Hughes LE (1987) Giant breast tumours of adolescence. Aust N Z J Surg 57:243–247
Haagensen CD (1986) Diseases of the breast. Saunders, Philadelphia
Jayasinghe Y, Simmons PS (2009) Fibroadenomas in adolescence. Curr Opin Obstet Gynecol 21:402–406
Onuigbo W (2003) Breast fibroadenoma in teenage females. Turk J Pediatr 45:326–328
Al-Atrooshi SA (2012) Fibroepithelial tumors of female breast: a review of 250 cases of fibroadenomas and phylloides tumors. Iraqi Postgrad Med J 11:140–145
Tavassoli FA (1999) Pathology of the breast, 2nd edn. McGraw Hill, New York, pp 571–579
McCutheon JM, Lipa M (1993) Infarction of a fibroadenoma of breast following fine needle aspiration. Cytopathology 4:247–250
Raju GC, Naraynsingh V (1985) Infarction of fibroadenoma of the breast. J Royal Coll Surg Edinb 30:162–163
Pinto RG, Couto F, Mandreker S (1996) Infarction after fine needle aspiration. A report of four cases. Acta Cytol 40:739–741
Vargas MP, Merino MJ (1996) Infarcted myxoid fibroadenoma following fine-needle aspiration. Arch Pathol Lab Med 120:1069–1071
Wilkinson L et al (1964) Infarction of breast lesions during pregnancy and lactation. Cancer 17:1567–1572
Wadhwa N, Joshi R, Mangal N, Khan NP, Joshi M (2014) Cytopathologic diagnosis of spontaneous infarction of fibroadenoma of the breast. Turk J Pathol 30(3):237–240
Sabate JM, Clotet M, Torrubia S, Gomez A, Guerrero R, de lasHeras P, Lerma E (2007) Radiologic evaluation of breast disorders related to pregnancy and lactation. Radiographics 27(Suppl. 1):S101–S124
Salih Abdulwahid M, Kakamad FH (2016) Spontaneous infarction of fibroadenoma of breast—a case report with literature review. Int J Surg Case Rep. 24:1–3
Laishram R (2010) Spontaneous infarction of fibroadenoma of the breast in a young girl mimicking carcinoma. Iran J Pathol 5:212–215
Kumar S, Iyengar KR, Rajagopal S, Roy SK (2005) A case of fibroadenoma with spontaneous infarction. J Cytol 22:42–43
Deshpande KM, Deshpande AH, Raut WK, Lele VR, Bobhate SK (2002) Diagnostic difficulties in spontaneous infarction of a fibroadenoma in an adolescent: case report. Diagn Cytopathol 26:26–28
Magnoni P, Nardi F (1996) Giant fibroadenoma of the breast. Its clinical picture and differential diagnosis. A report of a clinical case. Minerva Chir 51(1–2):71–75
Dolmans GH, Hoogbergen MM, van Rappard JH (2007) Giant fibroadenoma of one breast: immediate bilateral reconstruction. J Plast Reconstr Aesthet Surg 60(10):1156–1157
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Singh, S.K., Gupta, P., Arora, R. et al. Giant fibroadenoma with massive infarction masquerading as malignancy: a case report. Int Canc Conf J 6, 167–170 (2017). https://doi.org/10.1007/s13691-017-0299-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-017-0299-5