Abstract
Purpose of Review
This review describes policy and regulatory strategies to prevent obesity and summarizes worldwide progress and impediments to scaling up strategies globally.
Recent Findings
While there is considerable variation in the breadth and depth of uptake of recommended strategies, the adoption of effective obesity prevention policies has been slow and inconsistent. There is broad consensus that strong government, corporate, and consumer actions, including regulatory measures, are needed to advance obesity prevention policies. Governments have lacked sufficient will to take necessary action, the food industry has actively worked to thwart policies to protect its commercial interests, and consumers have not exerted sufficient influence or demand to produce change.
Summary
Advancing obesity prevention will require the use of effective strategies to shape and influence the information environments and political environments towards messages and actions to support public health. Greater emphasis is needed on reducing the influence of commercial interests, mobilizing civil society, and targeting vulnerable populations through equity-focused frameworks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past four decades, there has been a dramatic rise in global obesity, with recent studies reporting an eight times increase in girls, to 5.6%, and a ten times increase in boys, to 7.8%, in 2016 [1, 2••]. Among adults, global estimates indicate that approximately 13% of the population (10.8% men and 14.9% of women) are obese [3, 4]. As of 2015, excess body weight was estimated to affect two billion people worldwide and accounted for approximately four million deaths and 120 million disability-adjusted life years, with associated health and economic burdens [1, 2••, 5].
Throughout human history, insufficient food was the most pressing nutritional challenge. In response, government food policies in many countries shifted to support a high volume of agricultural production of low-nutrient commodities. Despite food surpluses and an unprecedented increase in obesity and diet-related diseases, governments across much of the world have continued to support an outdated approach to food policy priorities, supporting conventional ideas regarding food security, economics, and trade [6]. While the problem of undernutrition remains a significant threat to health in some regions, it must be noted that the global food system now produces a high volume of widely marketed, palatable, energy dense, low-nutrient food that has been a significant contributor to the global obesity pandemic [2••, 7]. Changes in societal eating norms that privilege a ‘western diet’, including increased overall daily calories, increased consumption of foods high in fat and sugar, increased access to inexpensive and refined foods, increased meals consumed outside the home, and decreased consumption of fruits, vegetables, and whole grains, have been found to be associated with increased body composition and nutrition-related morbidities [8,9,10]. The burden of obesity is not isolated to developed nations. Research has demonstrated that, similar to high-income countries, low- and medium-income countries are experiencing the adverse health effects of rapidly shifting dietary patterns associated with adoption of the ‘western diet’ [9]. The last half-century has also been characterized by major structural and developmental changes in many societies, including technological changes in the workplace (decline of physically active occupations), in the home (advent of labor-saving devices), and transport systems (widespread use of automobiles) that have been linked to decreased physical activity. Community design and transportation infrastructure (i.e., land use, urban sprawl, built environment) increasingly privilege motor vehicle use and limit opportunities for active transit and recreation [11]. Several studies have demonstrated links between these factors and weight status [12]. Low and declining rates of worldwide physical activity and active transit have been repeatedly documented [13,14,15].
The global response to obesity has included extensive research, scientific recommendations, and guidance, as well as regional declarations prioritizing action [16,17,18,19,20,21]. It is widely accepted that a systems-oriented approach, targeting numerous aspects of the food system and the built environment must be the primary focal point for obesity prevention. This paper reviews worldwide progress toward adoption of the policy and regulatory strategies that are the foundation of this approach and the impediments to scaling up these strategies globally.
Global Progress on Policy and Regulatory Strategies to Prevent Obesity
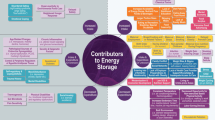
Most recommended policy and regulatory approaches to obesity prevention include five emergent areas: taxation, nutrition labeling, media and marketing, built environment, and school-based initiatives.
Taxation
The price of food is an important determinant of food choices [16, 22]. Emerging research indicates that regulatory policies, such as food and beverage taxes, can contribute to a reduction in purchases of sugar-sweetened beverages (SSBs) and energy-dense foods (EDFs). Research suggests that positive changes in purchasing behaviors (i.e., reduced purchasing of SSBs and EDFs) are likely to occur when product prices are increased by 20% or more [23,24,25]. Recent estimates suggest that even a 10% increase in SSBs may reduce consumption [26]. Studies have shown that increases in SSB and EDF prices can improve dietary choices and weight status among at-risk populations [26,27,28]. Mexico’s SSB tax led to a decrease on average consumption of 17% over the first year of implementation. Overconsumption of SSBs and EDFs is associated with lower intake of vital nutrients and an increased risk for obesity and related chronic diseases [29,30,31].
In 2016, WHO-recommended governments raise the prices of SSBs by at least 20% through use of an excise tax [32]. Numerous countries (e.g., Bahrain, Barbados, Belgium, Chile, Dominica, France, Hungary, Kiribati, Mauritius, Mexico, and Tonga) have implemented taxes on SSBs [33, 34]. For example, Mexico implemented a SSBs tax in 2013, and it resulted in a marked decrease in sales—5.5% in the first year and 9.7% in the second year [31]. France currently has an excise tax proportional to the sugar content present in a beverage. This tax was implemented in 2012 and includes all non-alcoholic beverages with added sugar. Within the first 2 years, the demand for regular cola decreased by 6.7% [35].
Taxation for EDFs has been used as a regulatory approach to discourage consumption. In 2011, Hungary introduced a 4% junk food tax on pre-packaged foods that are high in salt, caffeine, or sugar [36]. In 2013, Mexico introduced an 8% tax on non-essential foods that surpass a calorie density threshold. This policy contributed to a decline in food purchases in this category [37]. The Navajo Nation within the USA adopted the Healthy Diné Nation Act, which includes a tax on SSBs along with pre-packaged and non-prepackaged snacks stripped of essential nutrients and high in salt, saturated fat, and sugar [34]. Several cities within the USA have adopted similar policies [34]. In 2011, Denmark introduced the very first tax on foods with high saturated fats. Danish citizens avoided this tax by purchasing items across the border in countries such as Sweden and Germany [38]. This cross-border shift in purchasing behavior following an EDF or SSB tax has been observed elsewhere [39]. After 12 months, Denmark’s “fat tax” was repealed.
Taxes on SSB and EDFs have been successfully implemented in numerous countries and local jurisdictions. When implemented appropriately, such taxes serve as regulatory strategies that can impact consumers’ purchasing behaviors and result in a marked reduction in the sales of SSBs and EDFs. While taxing SSBs is a financially regressive tax, research shows that the benefits are consistent across all socioeconomic groups and can show even greater impacts for lower SES groups [40]. In some cases, regulations have led food companies to reformulate their products as to abide by the tax thresholds [41].
Still, considerable obstacles to the promotion of healthful foods and diets persist. The corporate practice of price promotions undermines taxation as a strategy to disincentivize the purchasing of less healthful foods. Price promotions temporarily reduce prices of specific goods, similar to coupon face values, and can be used to entice customers and influence their purchasing behaviors. The foods and beverages that are often price promoted are typically less healthful, and, thus, runs counter to the public health aims of taxation. Research in Australian supermarkets has demonstrated that beverage price promotions mitigated efforts to decrease SSB consumption [42]. In addition, while taxation has shown promise for positively influencing food purchasing behaviors, global uptake and reach is limited. The vast majority of retailers globally are not subject to regulatory food policies that include taxation of SSB and EDFs. Thus, consumer purchasing behaviors are not influenced, and the consumption of SSBs and EDFs remains high [40].
A further challenge, globally, is the food industry’s efforts to influence obesity science and policy. This is seen by their funding of scientists and health organizations who shift blame for obesity away from foods and sugar-sweetened beverages, through corporate political activity of the food industry, or by funding the production of potentially biased research findings [43,44,45,46,47]. In China, the soda industry has worked to influence obesity science and policy by shifting the focus from diet to physical activity [48, 49]. Beyond these efforts, the food industry has actively lobbied against legislation that seeks to reduce soda consumption or improve nutrition [43]. A relatively new strategy for the food industry in thwarting regulation are efforts to pre-empt the legal authorities of local jurisdictions to impose taxes on sugar-sweetened beverages, and their efforts include lobbying and significant financial investments to advance such approaches [50].
Nutrition Labeling
Nutrition labeling can inform consumer food choices and promote healthful eating. An emerging base of evidence suggests that nutrition labeling at the time of purchase can lead consumers to select foods with up to 150 fewer calories per order when purchasing from a menu [51,52,53]. Bleich (2014) found that calorie labeling of beverages was associated with reduced purchasing of SSBs [52]. Other research has found that when chain restaurants post calorie information on their menus, they offer items with fewer calories when compared to restaurants that did not post calorie information [54].
In 2004, WHO began promoting the use of nutrition labeling on food packages. Front of package (FOP) labeling provides simplified information on a product’s essential nutrients and has been promoted as a strategy to help consumers identify and select healthier foods, to motivate manufacturers to make healthier products, and to allow consumers to compare similar food items easily [17, 18, 55]. Kanter, Venderless, and Vandevijvere (2018) reviewed and developed a timeline of notable global policy action from 1989 to 2019, which included 37 FOP labeling initiatives worldwide [56]. Nordic and Northern European countries such as Norway, Sweden, Denmark, Iceland, and Lithuania were among the first to implement FOP labeling (in 1989) and utilize an endorsement logo to help consumers identify healthier options across different food groups [57]. Belgium, Czech Republic, Netherlands, and Poland have adopted a similar FOP labeling system [58]. Another approach to FOP labeling is the traffic light labeling system used by the United Kingdom (UK), South Korea, and Ecuador. This method uses a traffic light color beside each critical nutrient to denote prescriptive and proscriptive contents [56]. In Ecuador, the use of this labeling system led to decreased sales of certain unhealthy foods [59]. In South Korea, the traffic light labeling system is only in place for children’s snack foods [56, 58••]. Brazil, Chile, China, and Thailand have implemented mandatory labeling on packaged food or snacks [60]. Many countries (e.g., Argentina, Brazil, Canada, Chile, Hong Kong, Paraguay, South Korea, Taiwan, Uruguay, USA) have enacted policies that make it mandatory to include trans fats in nutrition labels [58••].
In 2014, Australia and New Zealand adopted a Health Star Rating system that generates a star rating from ½ to 5 stars based on the food’s nutritional content, with more stars indicating a healthier item. This rating system is based on total calories, risk nutrients (i.e., sodium, sugar, saturated fat), and positive nutrients (i.e., dietary fiber, protein, fruit and vegetable content, etc.). This system of labeling is not mandatory in Australia and New Zealand, and while the voluntary uptake is increasing, there has not been a measurable public health impact [61, 62].
The provision of purchasing guidance to consumers through use of labels or tags positioned on supermarket shelving, adjacent to food products, can be helpful in promoting healthier options. Shelf tags provide point-of-purchase health promotion messages to increase consumer knowledge and encourage healthful food selections [63]. The utilization of shelf tags to promote healthful foods purchases in supermarkets has been shown to be effective [62, 64,65,66].
While some countries have adopted strong regulations that mandate specific food labeling requirements, others have taken little to no action and are depending on voluntary self-regulation by the food industry. Thus, there is an uneven distribution of nutrition labeling regulations, and the citizens of many nations remain at-risk for poor food choices as a result of an inadequate food information environment. Even among those nations with substantial nutrition labeling requirements, data suggest a need to simplify the labels such that the vast majority of consumers find them understandable and easy to decipher. In a 2012 study conducted by Nielsen, nearly six in ten (59%) global respondents indicated they had difficulty grasping the nutritional facts included on nutrition labels, with 52% understanding the labels “in part” and 7% not understanding them at all [67]. There remains considerable work to be done in advancing food labeling regulations and improving our understanding of the impact of various food labeling schemes on consumer perceptions of food products and purchasing behaviors.
Media and Marketing
Mass media and marketing can have a profound impact on obesity-related health behaviors. Food and beverage marketing, which largely advertises and promotes low nutrient, high-calorie foods, and beverages, has been shown to have a significant influence on food preferences and eating behaviors and contributes to childhood obesity [55, 68,69,70]. The food industry implements many effective marketing and advertising techniques to influence food choices, purchasing behaviors, and consumption with limited accountability [71]. This includes strategies that use the four P’s of marketing—product, place, price, promotion—also called the marketing mix. Within this framework and the food system, product refers to the food or beverage item and is influenced by quality, variety, branding, and packaging/labeling. Place refers to both the physical location and the distribution channels in which a consumer can access a product and is influenced by distribution, market coverage, location, and inventory. Price refers to the cost of a product and the value a consumer has placed on it. Rebates or allowances for distributors, price promotions or discounts for consumers, and other price setting tactics can all influence price. Promotion refers to the marketing communications used to reach consumers and includes advertisements, public relations, media, and messaging [71,72,73]. The combination of these four elements has guided food and beverage marketing since the 1960s, with industry actively employing strategies across these domains to promote sales of their products—many of which are energy dense, low nutrient foods, and beverages [72].
The adoption of legislative measures to regulate food and beverage marketing and its influence has been challenging, though there has been some progress globally. In Europe, many countries (e.g., Belgium, Denmark, Finland, France, Germany, Greece, Iceland, Ireland, Luxembourg, Liechtenstein, the Netherlands, Portugal, Sweden, and the UK) restrict televised food advertisements targeting children [18, 74]. Australia, Canada, and South Korea ban food advertisements targeting children through any media platform [75]. France and Turkey require food advertisements to include approved health messages [75, 76]. Mandatory regulations of food marketing in schools have also been enacted in Costa Rica, Chile, Ecuador, Hungary, Lithuania, Poland, Spain, Turkey, Uruguay, and the USA [75, 77]. In Austria, Germany, and Slovenia, national legislation restricts digital food marketing to youth [78].
Many countries (e.g., Australia, Canada, CARICOM member states, France, Macedonia, Mexico, the Netherlands, New Caledonia, Norway, Peru, Singapore, Tonga, the UK, the USA, and Venezuela) have implemented public awareness, mass media, and informational campaigns focused on healthy eating [75]. For example, Argentina, Chile, Germany, Mexico, New Zealand, South Africa, Spain, and Tonga have implemented “5 per day” public awareness campaigns using a variety of media platforms to increase daily fruit and vegetable intake. Denmark introduced a campaign promoting six servings per day and found that between 1995 and 2004, children ages 4–10 years increased their fruit and vegetable intake by 58% and 29%, respectively, and individuals aged 11–75 years increased their fruit and vegetable intake by 75% and 41%, respectively [79].
Several countries have implemented mass media campaigns using imagery and health warnings to serve as counter-advertisements to poor dietary and physical activity behaviors. For example, Western Australia implemented the “LiveLighter” campaign, which uses graphic images and messaging to illustrate the unseen, adverse effects of obesity [80, 81]. New York ran ads with graphic images depicting obesity in its “Man Drinking Fat” campaign and advertisements about soda drinking and amputations as a result of diabetes [74].
The food industry has promoted voluntary self-regulation of food and beverage marketing. However, research suggests that such approaches have either yielded minimal progress or are ineffective [82,83,84]. The global effort to regulate media and marketing on food products with low nutritional value reflects action by numerous nations. However, media-related barriers to the promotion of healthful eating remain. Children continue to be a target of food marketing that promotes energy dense, low-nutrient products [85]. And although televised advertisements have been the primary medium used by food and beverage companies, evidence shows that the food and beverage industry is shifting to new mediums—digital, viral, and social media marketing—to reach younger populations [86]. Food industry marketing and advertising continue to influence their food preferences. Counter-marketing promoting healthful foods and dietary behaviors and physical activity has been widely used and has shown some positive effects. It must be noted, however, that the scale of such efforts is limited relative to those of the food industry and commercial interests.
Built Environment
The physical environment can influence physical activity, sedentary and dietary behaviors [87,88,89,90,91]. Well-designed communities with green spaces, recreational facilities, sidewalks, and bike lanes are associated with higher levels of physical activity in adults and children [92,93,94,95]. Greater density of and proximity to green spaces and neighborhood walkability are associated with a decrease in sedentary behaviors [96,97,98]. Policy recommendations to improve the built environment include policies and land use decisions that impact community design, transportation, and zoning [99]. These policies can improve connectivity, enhance safety, and improve opportunities for physical activity [100,101,102]. Research findings indicate that cities in the USA have successfully increased walking, cycling, and the use of public transportation following the adoption of Complete Streets policies [103]. Complete Streets policies can be found in cities across Northern Europe, Canada, Chile, India, and other Asian countries [104,105,106,107,108,109]. In addition, some countries have embraced open streets events where main roads are temporarily blocked off to cars for leisure-time and recreational activities. Columbia is credited with inspiring the uptake of open streets events through its weekly Ciclovía. Many countries (e.g., Australia, Argentina, Belgium, Brazil, Canada, Chile, Costa Rica, Ecuador, Guatemala, India, Mexico, New Zealand, Peru, USA) have also reported open streets initiatives [110,111,112,113].
A challenge in reviewing progress in this area is that there is a shortage of literature enumerating and reviewing policies implemented globally to improve the built environment for physical activity. It has been noted that it is difficult to monitor such policies because they are administered primarily in local (city level) jurisdictions and may vary in nature, scope, and purpose [114]. Increased standardization of measures and tracking of such policies is needed [114]
The presence of certain food retailers and access to healthy foods are a vital part of a healthy food environment [115, 116]. Studies have found a positive association between the availability of markets selling fresh produce, a quality diet, and a lower prevalence of obesity [117, 118]. Research suggests that limited access to healthy foods is associated with a higher risk for chronic diseases [117, 119, 120]. Strategies to enhance the food environment include approaches that regulate the promotion of unhealthy foods and beverages, improve access to food retailers or vendors with affordable and healthy options (e.g., grocery stores, farmers’ markets, community gardens, etc.), and limit the presence, density, and promotion of less healthy options (e.g., fast food restaurants, convenience stores etc.) [74]. Complementary strategies, such as healthy food promotion, food-benefit programs, and subsidies, can also help to build the infrastructure for and provide support necessary to create a more equitable food system [119, 121, 122]. While the presence of supermarkets or grocery stores alone has not been shown to improve dietary behaviors, research suggests that approaches, which combine procurement, promotion, and infrastructure strategies (i.e., strategies that address multiple aspects of supply and demand) and food access show promise in influencing the purchasing of healthy food by consumers and retailers [119, 123, 124]. Cameron et al. (2016) found that interventions within grocery stores, such as shelf tags and labeling, stand out as a low cost option for improving consumer purchases and promoting healthy eating [61]. The US Congress has supported the Healthy Food Financing Initiative (HFFI), which uses public and private grants, loans, training, and technical assistance, to bring grocery stores and other healthy food retailers to underserved urban and rural communities (i.e., food deserts) [125]. Between 2010 and 2018, the HHFI helped to leverage more than $220 million in grants and an estimated $1 billion in additional financing, supporting nearly 1000 grocery and other healthy food retail projects [126]. Different approaches have included policies to reduce the number of unhealthy food retailers by prohibiting the building of new fast food restaurants in Los Angeles (USA) and the enactment of restrictions for fast food and hot food takeaway retailers in close proximity to schools in the UK [34, 127, 128]. Procurement policies and subsidies have also been used to influence food supply chains and offset the cost of bringing healthy foods to vulnerable communities. In Canada, the government’s Nutrition North Canada program provided subsidies to retailers to reduce shipping rates of perishable foods for isolated communities in North Canada. The program was reported to reach 121 communities in its first year [129]. Still, there are notable challenges to improving healthy food access. In underserved areas, retailers may face increased costs to develop stores due to higher construction and operating costs, higher land prices, and challenging zoning laws, all of which can serve as barriers to retailers locating in low-income communities [130].
There has been the inadequate mobilization of public support and demand for policy and regulatory measures for health-promoting food and built environments. This has been the focus of recent commissions, with scholarly investment in rectifying this shortcoming [2, 131]. However, to date, the absence of public demand for healthier environments and public accountability for the food industry’s subversive and manipulative behaviors has left commercial interest relatively unchecked, and it has limited global progress on obesity prevention.
School-Based Initiatives
Schools influence diet and physical activity behaviors in children. Interventions focused on increasing the availability of healthy foods and beverages provided by schools combined with enhancing physical education (PE) has resulted in increased physical activity, modestly increased fruit and vegetable intake, and decreased overweight and obesity [132].
For nutrition, over 35 countries have developed mandatory standards for foods sold at school, spanning all populated continents, though there is variation in policy details across countries [58••, 133]. Romania introduced legislation in 2008 that set limits for salt, sugar, and fat for foods sold in schools and prohibited soft drinks. In 2011, Sweden implemented the Swedish Education Act, which requires school meals to be nutritious as well as free of charge [58••]. The UK, New Zealand, and the USA have government-sponsored programs to provide free fruits and vegetables to students [134,135,136]. In 2010, the USA adopted the Healthy Hunger-Free Kids Act (Healthy, Hunger-Free Kids Act of 2010), which aligned the National School Lunch Program and School Breakfast Program with the Dietary Guidelines for Americans [137, 138]. Parts of Australia adopted the Crunch&Sip program to promote fruit, vegetable, and water consumption in schools across the country [139].
For physical activity, between 2000 and 2013, the allocation of PE time within school curriculums has decreased [140,141,142]. Many countries have a legal requirement for PE in schools, but many do not adhere to their implementation regulations [143]. In the USA, some states have enacted laws requiring fitness assessments, minimum PE contact hours, and certified PE teachers to help improve the quality of physical activity offered in schools [144,145,146]. Russia, China, and the European Union have implemented similar fitness assessment requirements in primary schools [147]. Another strategy to increase opportunities for school physical activity is the promotion of active transit to school through community planning, supportive policies, and built environment improvements [148]. Such programs can be found in cities across the USA, Europe, Australia, New Zealand, and Canada [149, 150].
Many countries have implemented school-based policies and programs to promote a healthy weight. While foci and intervention approaches vary, there is evidence that some strategies have yielded positive outcomes, including positive changes in body mass index [151]. Unfortunately, there have been efforts by politicians, the food industry, and organizations receiving funding from the food industry to obstruct the development of school nutrition policy and to advocate for weakening such policies following implementation [152,153,154,155].
Impediments to Global Progress
The past 20 years of obesity prevention globally can be characterized by the development of scientific recommendations and guidance by leading health organizations and by efforts aimed at the diffusion of such strategies globally. While there is considerable variation in the breadth and depth of uptake of recommended policies, in general, the adoption of effective obesity prevention policies has been slow.
There has been an absence of institutional and political will to take needed action and a reluctance by governments to consistently impose strong regulations that promote healthier food environments and built environments [2••, 131, 156, 157]. Such political reluctance can be linked to a common narrative that has sought to shift responsibilities for obesity and health solely to the individual [131]. In many cases, a nanny-state metaphor has been deployed by politicians against government intervention, symbolically portraying an image of the Government as a coddling nanny [158]. Such efforts have been effective, at least in part, in preventing or slowing policy and regulatory actions for obesity prevention. Narratives that privilege individual responsibility at the expense of collective, systems-oriented interventions have attenuated the will to act.
The food industry has consistently impeded action on obesity prevention to promote an environment favorable to its aims. Brownell (2012) has noted a pattern in food industry behavior to make promises to improve, to highlight minor progress, and to create an impression of change, while their larger attempts actively subvert regulatory efforts that aim to improve the food environment [159]. Mialon et al. (2016) have highlighted the Corporate Political Activity (CPA) of the food industry, identifying specific strategies it uses to shape the food environment and influence public policy and illuminating the incongruence between commercial objectives in this context to maximize profits and broader aims for population health. Others have suggested that the food industry, to advance its goals, has promoted the belief that policy and regulations impose an unacceptable cost on business [47]. The Lancet Commission (2019) has noted that Big Food has used multiple strategies to obstruct obesity prevention, including adopting self-regulation to pre-empt and delay state regulation, public relations to portray industry as socially responsible, undermining and contesting the strength of existing scientific evidence, direct lobbying of politicians, and framing nutrition as a matter of individual responsibility [2••]. Thus, the food industry has aggressively, and effectively, manipulated the information environment (through marketing and advertising, mass media, sowing doubt and bias in obesity science, promoting physical activity to minimize nutrition) and political environment (through lobbying, cooptation of influencers, and preemption) to support their commercial interests.
Discussion
This review suggests that recommended policy and regulatory approaches are being implemented across countries and continents. However, the adoption of effective obesity prevention policies has been slow and inconsistent and the result of inadequate political leadership and governance, strong opposition to proposed policies by powerful commercial interests, and a lack of demand for policy action by the public. An overarching theme during the past two decades in the global politics of obesity is that efforts to control the information environment and the political environment have been a central factor in the observed outcomes of obesity prevention efforts. Advancing obesity prevention policies and regulations will require the use of effective strategies to shape and influence the information environments and political environments towards messages and actions to support public health.
Three approaches that hold promise for increasing success in the global campaign for obesity prevention require increased focus. First, there is a need to unsettle the power and influence of the food industry and other commercial interests, and to increase their accountability. This has been explicitly identified as a priority previously but warrants reiteration and ongoing attention [2••, 159]. Efforts in this area should seek to obtain consensus and adoption of standards, regulations, and accountability systems for the food industry [2••, 157, 160]. The work underway by the International Network for Food and Obesity/NCDs Research, Monitoring, and Action Support (INFORMAS) to provide data on food environments and independent assessments of government and corporate actions is an important resource [157]. The recent and growing body of work on identifying and countering the corporate and commercial determinants of health may be useful here [161, 162••, 163•]. There is also research in political science focused on advancing knowledge related to policy or issue regimes, which promote long-term stable power arrangements in a given policy system and facilitate resistance to fundamental change (e.g., food industry and politicians collaborate to maintain current food policies) [164, 165]. The idea of an issue regime emerging in obesity has been noted [166]. However, to our knowledge, there have not been any studies that aim to understand the establishment, maintenance, and disruption of policy or issue regimes. These findings might inform efforts to restructure (and reduce) the existing influence and control of commercial interests on policies and regulations for food policy and obesity prevention.
Second, there is potential in harnessing the power of media and advocacy to mobilize public support for evidence-informed obesity prevention. Despite calls for greater emphasis on advocacy and mobilization of civil society and specific guidance, the implementation of these efforts remains in an early phase [2••, 131, 167, 168]. There are frameworks and guidance for producing increased engagement by the public and civil society and stronger collective advocacy [2••, 131, 167, 168]. Key recommended strategies include engaging, educating, and collaborating with key stakeholders to establish a broad base of support; developing compelling narratives to frame the problem of obesity in terms relevant to known values and beliefs; and leveraging media to communicate and amplify persuasive messages [2••, 131, 167, 168]. Related to the effort to mobilize public support, it may also be effective to enlist alternate framing of obesity with other issues relevant to specific population groups as to increase support for proposed policies [2••, 131]. Obesity prevention efforts can benefit from greater alignment with broader social, environmental, and sustainability challenges and goals [2••]. This is an important, if not central, takeaway from the Lancet Commission’s 2019 report, that the global pandemic of obesity must be aligned with other pressing societal challenges that are the result of a shared set of human factors that are amenable to change. For example, in some countries, health-related obesity messages may motivate interest and action while in others, issues such as environmental sustainability, climate change, food security, animal rights, and national security may have greater appeal [2••, 131]. The goal of these efforts is to build public interest, mobilize citizens and decision-makers as advocates, and support the adoption of effective obesity prevention policies.
Finally, though there are well-established policy recommendations, there is a pressing need to implement these efforts through a lens that prioritizes equity in the access and opportunities that result from policy and regulatory approaches. Sub-populations who experience social disadvantage often have greater exposure to the influences that promote obesity and the resulting higher prevalence [169•, 170]. This usually includes racial minority and low-income populations, especially women and children. For example, while people of all income levels have a basic understanding of what constitutes a healthy diet, issues of affordability, accessibility, and availability of healthful foods create barriers for individuals who have low income [171]. Policy interventions that increase available resources to purchase foods and reduce the price of healthy foods are likely to help reduce inequities. There must be recognition that in order to lessen obesity disparities, interventions that work better in these populations than in white or more advantaged populations will be required [169•]. Equivalent or better impacts in advantaged compared to disadvantaged populations mean that gaps in obesity prevalence will widen rather than become smaller [114, 169•, 172]. Available frameworks and recommendations focused on equity in obesity prevention can serve as important resources [114, 169•, 172]. Failure to appropriately target vulnerable populations most affected by obesity will limit the effectiveness of the global campaign to mitigate it.
Conclusion
No country to date has significantly improved its overall food environment or reversed its obesity epidemic [173••]. This review found considerable evidence of global action on obesity prevention policies. While this represents progress, the most recent evidence suggests that the pace of implementation has been painfully slow and inadequate relative to the scale of the global pandemic. There is broad consensus that strong government and consumer actions, including regulatory measures, are needed to advance obesity prevention policies and that governments have lacked sufficient will to take necessary action, the food industry has actively worked to thwart such policies to protect its commercial interests, and consumers have not exerted sufficient influence or demand to produce change. Greater emphasis is needed on (a) reducing the power and influence of commercial interest, (b) mobilizing civil society, and (c) targeting vulnerable population through the application of equity-focused frameworks and guidance. Across the globe, strong leadership and bold action will be vital to catalyzing the changes necessary to advance obesity prevention.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet (London, England). 2017;390(10113):2627–42. https://doi.org/10.1016/S0140-6736(17)32129-3.
•• Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet (London, England). 2019;393(10173):791–846. https://doi.org/10.1016/S0140-6736(18)32822-8This paper describes the connection between obesity and climate change and provides recommendations for actions that must be taken to address obesity.
NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet (London, England). 2016;387(10026):1377–96. https://doi.org/10.1016/S0140-6736(16)30054-X.
World Health Organization. Obesity and overweight: World Health Organization. 2018. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 12 March 2019.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13–27. https://doi.org/10.1056/NEJMoa1614362.
Mozaffarian D, Angell SY, Lang T, Rivera JA. Role of government policy in nutrition—barriers to and opportunities for healthier eating. BMJ (Clinical research ed). 2018;361:k2426. https://doi.org/10.1136/bmj.k2426.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14. https://doi.org/10.1016/S0140-6736(11)60813-1.
The Nielsen Company. We Are What We Eat: Healthy Eating Trends Around The World., New York. 2015. https://www.nielsen.com/us/en/insights/report/2015/we-are-what-we-eat/.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. https://doi.org/10.1111/j.1753-4887.2011.00456.x.
O’Shaughnessy N. The Changing Face of Global Eating Patterns. Kerry Health and Nutrition Institute. 2017. https://khni.kerry.com/wp-content/uploads/2017/03/The-Changing-Face-of-Global-Eating-Patterns_FINAL.pdf.
Swinburn B, Egger G. The runaway weight gain train: too many accelerators, not enough brakes. BMJ (Clinical research ed). 2004;329(7468):736–9. https://doi.org/10.1136/bmj.329.7468.736.
Mackenbach JD, Rutter H, Compernolle S, Glonti K, Oppert J-M, Charreire H, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health. 2014;14:233. https://doi.org/10.1186/1471-2458-14-233.
Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. 2018;6(10):e1077–e86. https://doi.org/10.1016/S2214-109X(18)30357-7.
Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet (London, England). 2012;380(9838):247–57. https://doi.org/10.1016/S0140-6736(12)60646-1.
Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annu Rev Public Health. 2005;26:421–43.
World Health Organization. WHO Global Strategy on Diet, Physical Activity and Health. 2004. https://www.who.int/ncds/prevention/global-strategy-diet-physical-activity-2004-goals/en/. Accessed 12 March 2019.
World Health Organization. Global action plan for the prevention and control of NCDs 2013-2020. 2013. https://www.who.int/nmh/publications/ncd-action-plan/en/.
World Health Organization. Joint FAO/WHO workshop on Front-of-Pack Nutrition Labelling. 2013. https://www.who.int/nutrition/events/2013_FAO_WHO_workshop_frontofpack_nutritionlabelling/en/. Accessed 12 March 2019.
World Health Organization. WHO European Ministerial Conference on Counteracting Obesity Conference Report. 2007. http://www.euro.who.int/__data/assets/pdf_file/0006/96459/E90143.pdf. Accessed 12 March 2019.
Visser R, Atkinson RL. Proceedings of the Second Pan American Conference on Obesity with special attention to childhood obesity and a workshop, ‘Education for childhood obesity prevention: A life-course approach'. Int J Obes Suppl. 2013;3(Suppl 1):S1–2. https://doi.org/10.1038/ijosup.2013.1.
Pan American Health Organization. The 2007 Caribbean Community Port-of-Spain Declaration on noncommunicable diseases: an overview of a multidisciplinary evaluation. 2007. http://iris.paho.org/xmlui/handle/123456789/49692. Accessed 12 March 2019.
World Health Organization. Diet, nutrition, and the prevention of chronic diseases. [electronic resource]: report of a Joint WHO/FAO expert consultation. In: WHO technical report series: 916. World Health Organization. 2003. https://apps.who.int/iris/bitstream/handle/10665/42665/WHO_TRS_916.pdf?sequence=1.
Wright A, Smith KE, Hellowell M. Policy lessons from health taxes: a systematic review of empirical studies. BMC Public Health. 2017;17(1):583. https://doi.org/10.1186/s12889-017-4497-z.
World Health Organization. WHO calls on countries to reduce sugars intake among adults and children. 2015. https://www.who.int/mediacentre/news/releases/2015/sugar-guideline/en/. Accessed 12 March 2019.
Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka FJ, Thompson JW, et al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009;361(16):1599–605. https://doi.org/10.1056/NEJMhpr0905723.
Andreyeva T, Long MW, Brownell KD. The impact of food prices on consumption: a systematic review of research on the price elasticity of demand for food. Am J Public Health. 2010;100(2):216–22. https://doi.org/10.2105/AJPH.2008.151415.
Powell LM, Chaloupka FJ. Food prices and obesity: evidence and policy implications for taxes and subsidies. Milbank Q. 2009;87(1):229–57. https://doi.org/10.1111/j.1468-0009.2009.00554.x.
Smith C, Butterfass J, Richards R. Environment influences food access and resulting shopping and dietary behaviors among homeless Minnesotans living in food deserts. Agric Hum Values. 2010;27(2):141–61. https://doi.org/10.1007/s10460-009-9191-z.
Popkin BM, Nielsen SJ. The Sweetening of the World's Diet. Obesity Research. 2003;11(11):1325-32. https://doi.org/10.1038/oby.2003.179.
Vartanian LR, Schwartz MB, Brownell KD. Effects of Soft Drink Consumption on Nutrition and Health: A Systematic Review and Meta-Analysis. Am J Public Health. 2007;97(4):667–75. https://doi.org/10.2105/AJPH.2005.083782.
Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. In Mexico, Evidence Of Sustained Consumer Response Two Years After Implementing A Sugar-Sweetened Beverage Tax. Health Affairs (Project Hope). 2017;36(3):564–71. https://doi.org/10.1377/hlthaff.2016.1231.
World Health Organization. Fiscal policies for diet and the prevention of noncommunicable diseases. 2015. https://www.who.int/dietphysicalactivity/publications/fiscal-policies-diet-prevention/en/. Accessed 19 March 2019.
Roache SA, Gostin LO. The Untapped Power of Soda Taxes: Incentivizing Consumers, Generating Revenue, and Altering Corporate Behavior. Int J Health Policy Manag. 2017;6(9):489–93. https://doi.org/10.15171/ijhpm.2017.69.
World Cancer Research Fund International. Nourishing Framework: Use economic tools to address food affordability and purchase incentives. 2019. https://www.wcrf.org/sites/default/files/3_Use%20Economic%20Tools_May2019.pdf.
Tamir O, Cohen-Yogev T, Furman-Assaf S, Endevelt R. Taxation of sugar sweetened beverages and unhealthy foods: a qualitative study of key opinion leaders’ views. Israel Journal of Health Policy Research. 2018. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6069556/.
Bíró A. Did the junk food tax make the Hungarians eat healthier? Food Policy. 2015;54:107–15. https://doi.org/10.1016/j.foodpol.2015.05.003.
Taillie LS, Rivera JA, Popkin BM, Batis C. Do high vs. low purchasers respond differently to a nonessential energy-dense food tax? Two-year evaluation of Mexico's 8% nonessential food tax. Prev Med. 2017;105s:S37–s42. https://doi.org/10.1016/j.ypmed.2017.07.009.
The Economist. Denmark’s food taxes: A fat chance. Copenhagen, Denmark. 2012. https://www.economist.com/europe/2012/11/17/a-fat-chance.
Francis N, Marron D, Rueben K. The Pros and Cons of Taxing Sweetened Beverages Based on Sugar Content. The Urban Institute. 2016. https://www.heart.org/idc/groups/ahaecc-public/@wcm/@adv/documents/downloadable/ucm_490771.pdf.
Backholer K, Sarink D, Beauchamp A, Keating C, Loh V, Ball K, et al. The impact of a tax on sugar-sweetened beverages according to socio-economic position: a systematic review of the evidence. Public Health Nutr. 2016;19(17):3070–84. https://doi.org/10.1017/s136898001600104x.
European Competitiveness and Sustainable Industrial Policy Consortium. Food Taxes and Their Impact on Competitiveness in the Agri-Food Sector: Annexes to the Main Report. Rotterdam, The Netherlands: European Competitiveness and Sustainable Industrial Policy Consortium; 2014.
Zorbas C, Palermo C, Chung A, Iguacel I, Peeters A, Bennett R, et al. Factors perceived to influence healthy eating: a systematic review and meta-ethnographic synthesis of the literature. Nutr Rev. 2018;76(12):861–74. https://doi.org/10.1093/nutrit/nuy043.
Aaron DG, Siegel MB. Sponsorship of National Health Organizations by Two Major Soda Companies. Am J Prev Med. 2017;52(1):20–30. https://doi.org/10.1016/j.amepre.2016.08.010.
O'Connor A. Coca-Cola Funds Scientists Who Shift Blame for Obesity Away From Bad Diets. In: The New York Times. The New York Times. 2015. https://well.blogs.nytimes.com/2015/08/09/coca-cola-funds-scientists-who-shift-blame-for-obesity-away-from-bad-diets/.
Fabbri A, Holland TJ, Bero LA. Food industry sponsorship of academic research: investigating commercial bias in the research agenda. Public Health Nutr. 2018;21(18):3422–30. https://doi.org/10.1017/s1368980018002100.
Bes-Rastrollo M, Schulze MB, Ruiz-Canela M, Martinez-Gonzalez MA. Financial conflicts of interest and reporting bias regarding the association between sugar-sweetened beverages and weight gain: a systematic review of systematic reviews. PLoS Med. 2013;10(12):e1001578-e. https://doi.org/10.1371/journal.pmed.1001578.
Mialon M, Swinburn B, Wate J, Tukana I, Sacks G. Analysis of the corporate political activity of major food industry actors in Fiji. Glob Health. 2016;12(1):18–4. https://doi.org/10.1186/s12992-016-0158-8.
Greenhalgh S. Making China Safe for Coke: How Coca-Cola Shaped Obesity Science and Policy In China. In: BMJ: British Medical Journal 2019. https://www.bmj.com/content/364/bmj.k5050.abstract.
Greenhalgh S. How Coca-Cola shaped China's response to rising levels of obesity. Br Med J. 2019;364(8183):k5050.
O'connor A, Sanger-Katz M. California, of All Places, Has Banned Soda Taxes. How a New Industry Strategy Is Succeeding. In: The New York Times. The New York Times. 2018. https://www.nytimes.com/2018/06/27/upshot/california-banning-soda-taxes-a-new-industry-strategy-is-stunning-some-lawmakers.html.
Auchincloss AH, Mallya GG, Leonberg BL, Ricchezza A, Glanz K, Schwarz DF. Customer Responses to Mandatory Menu Labeling at Full-Service Restaurants. Am J Prev Med. 2013;45(6):710–9. https://doi.org/10.1016/j.amepre.2013.07.014.
Bleich SN, Barry CL, Gary-Webb TL, Herring BJ. Reducing Sugar-Sweetened Beverage Consumption by Providing Caloric Information: How Black Adolescents Alter Their Purchases and Whether the Effects Persist. Am J Public Health. 2014;104(12):2417–24. https://doi.org/10.2105/AJPH.2014.302150.
Bollinger B, Leslie P, Sorensen A. Calorie Posting in Chain Restaurants. 2011. https://doi.org/10.1257/pol.3.1.91.
Bleich SN, Wolfson JA, Jarlenski MP. Calorie Changes in Chain Restaurant Menu Items: Implications for Obesity and Evaluations of Menu Labeling. Am J Prev Med. 2015;48(1):70–5. https://doi.org/10.1016/j.amepre.2014.08.026.
World Health Organization. Report of the Commission on Ending Childhood Obesity. Geneva: WHO; 2016.
Kanter R, Vanderlee L, Vandevijvere S. Front-of-package nutrition labelling policy: global progress and future directions. Public Health Nutr. 2018;21(8):1399–408. https://doi.org/10.1017/S1368980018000010.
The Choices Programme. Positive nutrition labeling: A scientific overview. Choices International Foundation. 2019. https://www.choicesprogramme.org/uploads/Positive_Nutrition_Labeling_-_A_Scientific_Overview_2019.pdf.
•• World Cancer Research Fund International. World Cancer Research Fund International Nourishing Framework: Nutrition label standards and regulations on the use of claims and implied claims on foods. World Cancer Research Fund International. 2014. https://www.wcrf.org/sites/default/files/1%20Nutrition%20Labelling%20and%20Claims_November_2014.pdf. Provides a comprehensive review (via NOURISHING Framework) of implemented policy actions across different countries that address nutrition, the food environment, and food systems.
Díaz AA, Mariana Veliz P, Rivas-Mariño G, Vance Mafla C, María Martínez Altamirano L, Vaca Jones C. Food labeling in Ecuador: implementation, results, and pending actions. Pan-American Journal of Public Health. 2017. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6612743/.
Hawkes C, Jewell J, Allen K. A food policy package for healthy diets and the prevention of obesity and diet-related non-communicable diseases: the NOURISHING framework. Obes Rev. 2013;14:159–68. https://doi.org/10.1111/obr.12098.
Jones A, Shahid M, Neal B. Uptake of Australia’s Health Star Rating System. Nutrients. 2018;8:997. https://doi.org/10.3390/nu10080997.
Cameron AJ, Charlton E, Ngan WW, Sacks G. A Systematic Review of the Effectiveness of Supermarket-Based Interventions Involving Product, Promotion, or Place on the Healthiness of Consumer Purchases. Curr Nutr Rep. 2016;5(3):129–38. https://doi.org/10.1007/s13668-016-0172-8.
Glanz K, Yaroch AL. Strategies for increasing fruit and vegetable intake in grocery stores and communities: policy, pricing, and environmental change. Prev Med. 2004;39(Suppl 2):S75–80. https://doi.org/10.1016/j.ypmed.2004.01.004.
Sigurdsson V, Larsen NM, Gunnarsson D. Healthy food products at the point of purchase: An in-store experimental analysis. J Appl Behav Anal. 2014;47(1):151–4. https://doi.org/10.1002/jaba.91.
Foster GD, Karpyn A, Wojtanowski AC, Davis E, Weiss S, Brensinger C, et al. Placement and promotion strategies to increase sales of healthier products in supermarkets in low-income, ethnically diverse neighborhoods: a randomized controlled trial. Am J Clin Nutr. 2014;99(6):1359–68. https://doi.org/10.3945/ajcn.113.075572.
Holmes AS, Estabrooks PA, Davis GC, Serrano EL. Effect of a grocery store intervention on sales of nutritious foods to youth and their families. J Acad Nutr Diet. 2012;112(6):897–901. https://doi.org/10.1016/j.jand.2012.01.012.
The Nielsen Company. Battle of the Bulge & Nutrition Labels: Healthy Eating Trends Around the World. The Nielsen Company. 2012. http://silvergroup.asia/wp-content/uploads/2012/02/Nielsen-Global-Food-Labeling-Report-Jan2012.pdf.
Bakir A, Vitell SJ. The Ethics of Food Advertising Targeted Toward Children: Parental Viewpoint. J Bus Ethics. 2010;91(2):299–311. https://doi.org/10.1007/s10551-009-0084-2.
Hastings G, Cairns G, Angus K. The Extent, Nature And Effects Of Food Promotion To Children: A Review Of The Evidence. World Health Organization. 2006. https://www.who.int/dietphysicalactivity/publications/Hastings_paper_marketing.pdf.
McGuire S. Institute of Medicine. 2012. Accelerating progress in obesity prevention: solving the weight of the nation. Washington, DC: the National Academies Press. Adv Nutr. 2012;3(5):708–9. https://doi.org/10.3945/an.112.002733.
McGinnis JM, Gootman J, Kraak V. Food Marketing to Children and Youth: Threat or Opportunity? Washington, DC: The National Academies Press; 2006.
Bitner MJ. The Evolution Of The Services Marketing Mix And Its Relationship To Service Quality. In: Brown S, Gummesson E, Edvardsson B, Gustavsson B, editors. Service Quality: A Multidisciplinary And Multinational Perspective. New York, NY: Lexington Books; 1991.
Blythe J. Key Concepts in Marketing. In: SAGE Key Concepts series. SAGE Publications Ltd; 1 edition. 2009. https://us.sagepub.com/sites/default/files/upm-assets/24611_book_item_24611.pdf.
•• Taylor AL, Parento EW, Schmidt LA. The Increasing Weight of Regulation: Countries Combat the Global Obesity Epidemic. In: Indiana Law Journal. 2015. https://www.repository.law.indiana.edu/cgi/viewcontent.cgi?article=11138&context=ilj. Accessed Issue 1. This paper identifies recent global trends and progress around obesity prevention and describes nine key policy and regulatory trends.
World Cancer Research Fund International. NOURISHING framework: Restrict food advertising and other forms of commercial promotion. 2019. https://www.wcrf.org/sites/default/files/4_Restrict%20advertising_May2019.pdf. Accessed 19 March 2019.
CTV News. French Food Ads Carry Health Warnings: CTV News; 2007. https://www.ctvnews.ca/french-food-ads-carry-health-warnings-1.231591. Accessed 22 March 2019.
Organisation for Economic Co-operation and Development (OECD). Obesity Update. 2017. http://www.oecd.org/health/obesity-update.htm.
Lupiáñez-Villanueva F, Gaskell G, Veltri GA, Theben A, Folkvord F, Bonatti L, et al. Study on the impact of marketing through social media, online games and mobile applications on children's behaviour. Luxembourg: Publications Office of the European Union; 2016.
Rekhy R, McConchie R. Promoting consumption of fruit and vegetables for better health. Have campaigns delivered on the goals? Appetite. 2014;79:113–23. https://doi.org/10.1016/j.appet.2014.04.012.
LiveLighter. Program Background: LiveLighter; 2019. https://livelighter.com.au/About/Background. Accessed 10 April 2019.
Morley B, Niven P, Dixon H, Swanson M, Szybiak M, Shilton T, et al. Population-based evaluation of the ‘ LiveLighter’ healthy weight and lifestyle mass media campaign. Health Educ Res. 2016;31(2):121–35. https://doi.org/10.1093/her/cyw009.
Kunkel DL, Castonguay JS, Filer CR. Evaluating Industry Self-Regulation of Food Marketing to Children. Am J Prev Med. 2015;49(2):181–7. https://doi.org/10.1016/j.amepre.2015.01.027.
Ronit K, Jensen JD. Obesity and industry self-regulation of food and beverage marketing: a literature review. Eur J Clin Nutr. 2014;68(7):753–9. https://doi.org/10.1038/ejcn.2014.60.
King L, Hebden L, Grunseit A, Kelly B, Chapman K, Venugopal K. Industry self regulation of television food advertising: responsible or responsive? Int J Pediatric Obes. 2011;6(2-2):e390–8. https://doi.org/10.3109/17477166.2010.517313.
Frazier III W, Harris JL. Trends in Television Food Advertising to Young People: 2017 Update. . UConn Rudd Center for Food Policy & Obesity. 2018. http://uconnruddcenter.org/files/Pdfs/TVAdTrends2018_Final.pdf.
Powell LM, Harris JL, Fox T. Food marketing expenditures aimed at youth: putting the numbers in context. Am J Prev Med. 2013;45(4):453–61. https://doi.org/10.1016/j.amepre.2013.06.003.
Renalds A, Smith TH, Hale PJ. A systematic review of built environment and health. Family Commun Health. 2010;33(1):68–78. https://doi.org/10.1097/FCH.0b013e3181c4e2e5.
Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125(5):729–37. https://doi.org/10.1161/CIRCULATIONAHA.110.969022.
Sallis JF, Glanz K. Physical activity and food environments: solutions to the obesity epidemic. Milbank Q. 2009;87(1):123–54. https://doi.org/10.1111/j.1468-0009.2009.00550.x.
Giles-Corti B, Vernez-Moudon A, Reis R, Turrell G, Dannenberg AL, Badland H, et al. City planning and population health: a global challenge. Lancet. 2016;388(10062):2912–24. https://doi.org/10.1016/S0140-6736(16)30066-6.
Salvo G, Lashewicz MB, Doyle-Baker KP, McCormack RG. Neighbourhood Built Environment Influences on Physical Activity among Adults: A Systematized Review of Qualitative Evidence. Int J Environ Res Public Health. 2018;15(5). https://doi.org/10.3390/ijerph15050897.
Sallis JF, Glanz K. The role of built environments in physical activity, eating, and obesity in childhood. Futur Child. 2006;16(1):89–108.
Sallis JF, Saelens BE, Frank LD, Conway TL, Slymen DJ, Cain KL, et al. Neighborhood built environment and income: examining multiple health outcomes. Soc Sci Med (1982). 2009;68(7):1285–93. https://doi.org/10.1016/j.socscimed.2009.01.017.
Bauman A, Bull F. Environmental correlates of physical activity and walking in adults and children: a review of reviews. London: National Institute of Health and Clinical Excellence; 2007.
Sallis JF, Spoon C, Cavill N, Engelberg JK, Gebel K, Parker M, et al. Co-benefits of designing communities for active living: an exploration of literature. Int J Behav Nutr Phys Act. 2015;12:30. https://doi.org/10.1186/s12966-015-0188-2.
Astell-Burt T, Feng X, Kolt GS. Greener neighborhoods, slimmer people? Evidence from 246,920 Australians. Int J Obes (2005). 2014;38(1):156–9. https://doi.org/10.1038/ijo.2013.64.
O'Donoghue G, Perchoux C, Mensah K, Lakerveld J, van der Ploeg H, Bernaards C, et al. A systematic review of correlates of sedentary behaviour in adults aged 18-65 years: a socio-ecological approach. BMC Public Health. 2016;16:163. https://doi.org/10.1186/s12889-016-2841-3.
Storgaard RL, Hansen HS, Aadahl M, Glumer C. Association between neighbourhood green space and sedentary leisure time in a Danish population. Scand J Public Health. 2013;41(8):846–52. https://doi.org/10.1177/1403494813499459.
Community Preventive Services Task Force. Using Evidence to Improve Health Outcomes: Annual Report to Congress, Federal Agencies, and Prevention Stakeholders. 2016. https://www.thecommunityguide.org/sites/default/files/assets/2016-congress-report-full.pdf.
Heath GW, Brownson RC, Kruger J, Miles R, Powell KE, Ramsey LT. The Effectiveness of Urban Design and Land Use and Transport Policies and Practices to Increase Physical Activity: A Systematic Review. J Phys Act Health. 2006;3(s1):S55–76. https://doi.org/10.1123/jpah.3.s1.s55.
Brownson RC, Chriqui JF, Stamatakis KA. Understanding evidence-based public health policy. Am J Public Health. 2009;99(9):1576–83. https://doi.org/10.2105/AJPH.2008.156224.
Ferdinand AO, Sen B, Rahurkar S, Engler S, Menachemi N. The relationship between built environments and physical activity: a systematic review. Am J Public Health. 2012;102(10):e7–e13. https://doi.org/10.2105/ajph.2012.300740.
Brown BB, Smith KR, Tharp D, Werner CM, Tribby CP, Miller HJ, et al. A Complete Street Intervention for Walking to Transit, Nontransit Walking, and Bicycling: A Quasi-Experimental Demonstration of Increased Use. J Phys Act Health. 2016;13(11):1210–9. https://doi.org/10.1123/jpah.2016-0066.
Smart Growth America. Complete Streets Policies Nationwide [US]. In: Policy Inventory. 2019. https://smartgrowthamerica.org/program/national-complete-streets-coalition/publications/policy-development/policy-atlas/. Accessed 10 April 2019.
California Bicycle Coalition (CalBike). Complete streets fact sheet. 2019. https://www.calbike.org/resources/fact_sheets_and_faq_s/complete_streets_fact_sheet. Accessed 10 April 2019.
Leather J, Fabian H, Gota S, Mejia A. Walkability and Pedestrian Facilities in Asian Cities: State and Issues. In: ADB Sustainable Development Working Paper Series No.17,. Asian Development Bank 2011. https://www.adb.org/sites/default/files/publication/28679/adb-wp17-walkability-pedestrian-facilities-asian-cities.pdf.
Institute for Transportation and Development Policy (ITDP). ITDP Annual Report 2015. New York, 2015. https://itdpdotorg.wpengine.com/wp-content/uploads/2014/07/ITDP_AR_15.pdf.
Paris Process On Mobility And Climate (PPMC). Provide And Improve Walking And Cycling Infrastructure (E.G. Connected Walking Paths, Protected Cycle Lanes), Reallocating Roadspace Where Necessary. 2019. http://www.ppmc-transport.org/provide-and-improve-walking-and-cycling-infrastructure-e-g-connected-walking-paths-protected-cycle-lanes-reallocating-roadspace-where-necessary/. Accessed 10 April 2019.
Hidalgo D. Beyond a bus system: Complete streets to revitalize Santiago, Chile. In: The City Fix. World Resources Institute Ross Center. 2013. https://thecityfix.com/blog/beyond-a-bus-system-complete-streets-to-revitalize-santiago-chile-dario-hidalgo/.
Sarmiento O, Torres A, Jacoby E, Pratt M, Schmid TL, Stierling G. The Ciclovía-Recreativa: A mass-recreational program with public health potential. J Phys Act Health. 2010;7(Suppl 2):S163–S80.
Citizen Matters. First ‘Feel Bengaluru Cycle Day’ sees participation from 1200 cyclists. 2013. http://bengaluru.citizenmatters.in/first-feel-bengaluru-cycle-day-sees-participation-from-1200-cyclists-5823. Accessed 15 April 2019.
Kohli S. Raahgiri: Less honking, more bonding — How Gurgaon showed the way. 2016. https://timesofindia.indiatimes.com/city/gurgaon/Raahgiri-Less-honking-more-bonding-How-Gurgaon-showed-the-way/articleshow/51468982.cms. Accessed 15 April 2019.
Cycling in Christchurch. It’s Back – Open Streets Ciclovía, Sun Sept 29th. 2013. http://cyclingchristchurch.co.nz/2013/09/15/its-back-open-streets-ciclovia-sun-sept-29th/. Accessed 15 April 2019.
Institute of Medicine. Measuring Progress in Obesity Prevention: Workshop Report. The National Academies Press, Washington, DC. 2012. https://www.nap.edu/catalog/13287/measuring-progress-in-obesity-prevention-workshop-report.
Grimm KA, Moore LV, Scanlon KS. Access to Healthier Food Retailers -- United States, 2011. MMWR. 2013;62:20–6.
Cooksey-Stowers K, Schwartz MB, Brownell KD. Food Swamps Predict Obesity Rates Better Than Food Deserts in the United States. Int J Environ Res Public Health. 2017;14(11). https://doi.org/10.3390/ijerph14111366.
Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR Jr. Associations of the Local Food Environment with Diet Quality—A Comparison of Assessments based on Surveys and Geographic Information Systems: The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167(8):917–24. https://doi.org/10.1093/aje/kwm394.
Morland K, Diez Roux AV, Wing S. Supermarkets, Other Food Stores, and Obesity: The Atherosclerosis Risk in Communities Study. Am J Prev Med. 2006;30(4):333–9. https://doi.org/10.1016/j.amepre.2005.11.003.
Evans A, Banks K, Jennings R, Nehme E, Nemec C, Sharma S, et al. Increasing access to healthful foods: a qualitative study with residents of low-income communities. Int J Behav Nutr Phys Act. 2015;12(Suppl 1):S5. https://doi.org/10.1186/1479-5868-12-s1-s5.
Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15(2):491–5. https://doi.org/10.1016/j.healthplace.2008.09.004.
An R. Effectiveness of subsidies in promoting healthy food purchases and consumption: a review of field experiments. Public Health Nutr. 2013;16(7):1215–28. https://doi.org/10.1017/s1368980012004715.
Story M, Kaphingst KM, Robinson-O'Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–72. https://doi.org/10.1146/annurev.publhealth.29.020907.090926.
Escaron AL, Meinen AM, Nitzke SA, Martinez-Donate AP. Supermarket and Grocery Store-Based Interventions to Promote Healthful Food Choices and Eating Practices: A Systematic Review. Prev Chronic Dis. 2013;10:E50. https://doi.org/10.5888/pcd10.120156.
Gittelsohn J, Rowan M, Gadhoke P. Interventions in small food stores to change the food environment, improve diet, and reduce risk of chronic disease. Prev Chronic Dis. 2012;9:E59.
US Department of Health and Human Services. Healthy Food Financing Initiative. 2019. https://www.acf.hhs.gov/ocs/programs/community-economic-development/healthy-food-financing. Accessed 10 April 2019.
Reinvestment Fund. Healthy Food Financing Initiative. 2019. https://www.reinvestment.com/initiatives/hffi/. Accessed 15 April 2019.
Thornton LE, Kavanagh AM. Association Between Fast Food Purchasing and The Local Food Environment. In: Nutrition & Diabetes. Nature Research. 2012. https://doi.org/10.1038/nutd.2012.27.
Spacht AC. The Zoning Diet: Using Restrictive Zoning to Shrink American Waistlines. Notre Dame Law Review. 2009; (1):391. https://pdfs.semanticscholar.org/10ed/b48e67266d659d3588587b078460a99fa443.pdf. Accessed Issue 1.
Indigenous and Northern Affairs Canada. Performance Measurement Strategy - 4.1.2 Nutrition North Canada. 2016. https://www.aadnc-aandc.gc.ca/eng/1490794132119/1490794299502. Accessed 10 April 2019.
United States Department of Agriculture (USDA). Access to affordable and nutritious food: measuring and understanding food deserts and their consequences. Washington, D.C: United States Department of Agriculture; 2009.
Huang T, Wu F, Yu J, Zhang B. International political risk and government bond pricing. J Bank Financ. 2015;55:393–405. https://doi.org/10.1016/j.jbankfin.2014.08.003.
The Community Guide. Obesity Prevention and Control: Meal or Fruit and Vegetable Snack Interventions Combined with Physical Activity Interventions in Schools. 2018. https://www.thecommunityguide.org/findings/obesity-prevention-control-meal-fruit-vegetable-snack-interventions-combined-physical-activity-interventions-schools. Accessed 10 April 2019.
Hunter D, Giyose B, PoloGalante A, Tartanac F, Bundy D, Mitchell A et al. Schools as a System to Improve Nutrition: A new statement for school-based food and nutrition interventions. United Nations System Standing Committee On Nutrition. 2017. https://www.unscn.org/uploads/web/news/document/School-Paper-EN-WEB.pdf.
Boyd S, Dingle R, Campbell R, King J, Corter A. Taking a bite of the apple: The implementation of Fruit in Schools (Healthy Futures evaluation report to the Ministry of Health). New Zealand Council for Educational Research, Wellington, New Zealand. 2007. https://www.nzcer.org.nz/system/files/healthy-futures-report-june07_0.pdf. Accessed 15 April 2019.
United Fresh Produce Association. Healthy School Meals. 2019. https://www.unitedfresh.org/nutrition/healthy-school-meals/. Accessed 15 April 2019.
USDA Food and Nutrition Service. Evaluation of the Fresh Fruit and Vegetable Program (FFVP). US Department of Agriculture, Alexandria, VA. 2013. https://fns-prod.azureedge.net/sites/default/files/FFVP.pdf.
United States Department of Agriculture (USDA). National School Lunch Program. 2019. https://www.ers.usda.gov/topics/food-nutrition-assistance/child-nutrition-programs/national-school-lunch-program.aspx. Accessed 15 April 2019.
USDA Food and Nutrition Service. Healthy Hunger-Free Kids Act. 2013. https://www.fns.usda.gov/school-meals/healthy-hunger-free-kids-act. Accessed 15 April 2019.
Nathan N, Wolfenden L, Butler M, Bell AC, Wyse R, Campbell E, et al. Vegetable and fruit breaks in Australian primary schools: prevalence, attitudes, barriers and implementation strategies. Health Educ Res. 2011;26(4):722–31. https://doi.org/10.1093/her/cyr033.
Hardman CA, Horne PJ, Fergus LC. Effects of rewards, peer-modelling and pedometer targets on children's physical activity: a school-based intervention study. Psychol Health. 2011;26(1):3–21. https://doi.org/10.1080/08870440903318119.
Hardman K, Marshall J. International Council of Sport Science and Physical Education. Second world-wide survey of school physical education : final report. Berlin: ICSSPE/CIEPSS, International Council of Sport Science and Physical Education; 2009.
Marshall J, Hardman K. The State and Status of Physical Education in Schools in International Context. Eur Phys Educ Rev. 2000;6(3):203–29. https://doi.org/10.1177/1356336X000063001.
Hardman K. Physical education in schools: A global perspective. Kinesiology. 2008;40(1):5–28.
Silverman S, Keating XD, Phillips S. A Lasting Impression: A Pedagogical Perspective on Youth Fitness Testing. Meas Phys Educ Exerc Sci. 2008;12(3):146–66.
Bevans K, Fitzpatrick L-A, Sanchez B, Forrest CB. Individual and Instructional Determinants of Student Engagement in Physical Education. J Teach Phys Educ. 2010;29(4):399–416.
Action for Healthy Kids. Fitness Testing. 2015. http://www.actionforhealthykids.org/game-on/find-challenges/gymnasium-challenges/1512-fitness-testing. Accessed 17 April 2019.
Keating XD, Smolianov P, Liu X, Castro-Piñero J, Smith J. Youth Fitness Testing Practices: Global Trends and New Development. The Sport Journal. 2018. https://thesportjournal.org/article/youth-fitness-testing-practices-global-trends-and-new-development/.
Safe Routes Partnership. Strategic Plan 2016-2021. Safe Routes to School National Partnership. 2019. http://saferoutespartnership.org/sites/default/files/pdf/03-25-16_stratplan.pdf.
Larouche R, Mammen G, Rowe DA, Faulkner G. Effectiveness of active school transport interventions: a systematic review and update. BMC Public Health. 2018;18(1):206. https://doi.org/10.1186/s12889-017-5005-1.
Safe Routes To School Guide. History of Safe Routes to School. 2019. http://guide.saferoutesinfo.org/introduction/history_of_srts.cfm. Accessed 15 April 2019.
Ickes MJ, McMullen J, Haider T, Sharma M. Global school-based childhood obesity interventions: a review. Int J Environ Res Public Health. 2014;11(9):8940–61. https://doi.org/10.3390/ijerph110908940.
Reeve E, Thow AM, Bell C, Engelhardt K, Gamolo-Naliponguit EC, Go JJ, et al. Implementation lessons for school food policies and marketing restrictions in the Philippines: a qualitative policy analysis. Glob Health. 2018;1:1–14. https://doi.org/10.1186/s12992-017-0320-y.
Food and Nutrition Service. Child Nutrition Programs: Flexibilities for Milk, Whole Grains, and Sodium Requirements. United States Department of Agriculture (USDA). 2018. https://www.federalregister.gov/documents/2018/12/12/2018-26762/child-nutrition-programs-flexibilities-for-milk-whole-grains-and-sodium-requirements.
Del Valle G. Federally funded school lunches are about to get a lot less healthy. Vox. 2019. https://www.vox.com/the-goods/2019/1/10/18177099/school-lunch-sonny-perdue-healthy-hunger-free-kids.
Evich H. Behind the school lunch fight. Politico. 2014. https://www.politico.com/story/2014/06/michelle-obama-public-school-lunch-school-nutrition-association-lets-move-107390.
Gortmaker SL, Swinburn BA, Levy D, Carter R, Mabry PL, Finegood DT, et al. Changing the future of obesity: science, policy, and action. Lancet (London, England). 2011;378(9793):838–47. https://doi.org/10.1016/S0140-6736(11)60815-5.
Swinburn B, Kraak V, Rutter H, Vandevijvere S, Lobstein T, Sacks G, et al. Strengthening of accountability systems to create healthy food environments and reduce global obesity. Lancet. 2015;385(9986):2534–45. https://doi.org/10.1016/S0140-6736(14)61747-5.
Baker P, Gill T, Friel S, Carey G, Kay A. Generating political priority for regulatory interventions targeting obesity prevention: an Australian case study. Soc Sci Med. 2017;177:141–9. https://doi.org/10.1016/j.socscimed.2017.01.047.
Brownell KD. Thinking forward: the quicksand of appeasing the food industry. PLoS Med. 2012;9(7):e1001254-e. https://doi.org/10.1371/journal.pmed.1001254.
Sharma LL, Teret SP, Brownell KD. The Food Industry and Self-Regulation: Standards to Promote Success and to Avoid Public Health Failures. Am J Public Health. 2010;100(2):240–6.
Freudenberg N, Galea S. The impact of corporate practices on health: implications for health policy. J Public Health Policy. 2008;29(1):86–104; discussion 5. https://doi.org/10.1057/palgrave.jphp.3200158.
•• Kickbusch I, Allen L, Franz C. The commercial determinants of health. Lancet Glob Health. 2016;4(12):e895–e6. https://doi.org/10.1016/S2214-109X(16)30217-0The commercial determinants of health are the “strategies and approaches used by the private sector to promote products and choices that are detrimental to health." This concept combines a number of different concepts, including: consumer and health behaviors, individualization, personal choice, the global risk society, the global consumer society, and the political economy of globalization.
• McKee M, Stuckler D. Revisiting the Corporate and Commercial Determinants of Health. Am J Public Health. 2018;108(9):1167–70. https://doi.org/10.2105/AJPH.2018.304510This paper reviews the concept of commercial dterminants of health, identifies the ways in which commercial interests influence health, and provides recommendations for addressing these influences.
Jochim AE, May PJ. Beyond Subsystems: Policy Regimes and Governance. Policy Stud J. 2010;38(2):303–27. https://doi.org/10.1111/j.1541-0072.2010.00363.x.
Wilson CA. Policy Regimes and Policy Change. J Public Policy. 2000;20(3):247–74.
Kersh R. The politics of obesity: a current assessment and look ahead. Milbank Q. 2009;87(1):295–316. https://doi.org/10.1111/j.1468-0009.2009.00556.x.
Cullerton K, Donnet T, Lee A, Gallegos D. Effective advocacy strategies for influencing government nutrition policy: a conceptual model. Int J Behav Nutr Phys Act. 2018;15(1):83–11. https://doi.org/10.1186/s12966-018-0716-y.
Lyn R, Aytur S, Davis TA, Eyler AA, Evenson KR, Chriqui JF, et al. Policy, systems, and environmental approaches for obesity prevention: a framework to inform local and state action. J Public Health Manag Pract. 2013;19(3 Suppl 1):S23–33. https://doi.org/10.1097/PHH.0b013e3182841709.
• Kumanyika S. Getting to Equity in Obesity Prevention: A New Framework. The National Academy of Medicine. 2017. https://nam.edu/getting-to-equity-in-obesity-prevention-a-new-framework/. Obesity is an issue of health equity. This paper identifies and describes the drivers of obesity that could be modified through a health-equity lens.
Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(Suppl 3):S163–75. https://doi.org/10.1542/peds.2009-1100D.
Loring B, Robertson A. Obesity and Inequities: Guidance for addressing inequities in overweight and obesity. World Health Organizaton, Denmark. 2014. http://www.euro.who.int/__data/assets/pdf_file/0003/247638/obesity-090514.pdf.
Chung A, Backholer K, Wong E, Palermo C, Keating C, Peeters A. Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: a systematic review. Obes Rev. 2016;17(3):276–95. https://doi.org/10.1111/obr.12360.
•• Roberto CA, Swinburn B, Hawkes C, Huang TT, Costa SA, Ashe M, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385(9985):2400–9. https://doi.org/10.1016/s0140-6736(14)61744-x The Lancet Series on Obesity sets the stage for progress worldwide and the barriers that are present. This paper identified priority actions on key obesity issues and provides recommendations for a path forward.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rodney Lyn, Erica Heath, and Janhavi Dubhashi declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on The Obesity Epidemic: Causes and Consequences
Rights and permissions
About this article
Cite this article
Lyn, R., Heath, E. & Dubhashi, J. Global Implementation of Obesity Prevention Policies: a Review of Progress, Politics, and the Path Forward. Curr Obes Rep 8, 504–516 (2019). https://doi.org/10.1007/s13679-019-00358-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-019-00358-w