Abstract
Purpose of Review
This review investigates how exposure to palatable food and its associated cues alters appetite regulation and feeding behaviour to drive overeating and weight gain.
Recent Findings
Both supraphysiological and physiological feeding systems are affected by exposure to palatable foods and its associated cues. Preclinical research, largely using rodents, has demonstrated that palatable food modulates feeding-related neural systems and food-seeking behaviour by recruiting the mesolimbic reward pathway. This is supported by studies in adolescents which have shown that mesolimbic activity in response to palatable food cues and consumption predicts future weight gain. Additionally, stress exposure, environmental factors and individual susceptibility have been shown to modulate the effects of highly palatable foods on behaviour.
Summary
Further preclinical research using free-choice diets modelling the modern obesogenic environment is needed to identify how palatable foods drive overeating. Moreover, future clinical research would benefit from more appropriate quantification of palatability, making use of rating systems and surveys.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
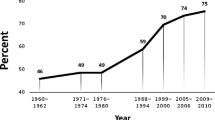
Obesity, the excessive accumulation of white adipose tissue commonly measured using body mass index (BMI), is well-known to induce or exacerbate a wide range of diseases, increasing both morbidity and mortality. The global obesity prevalence has almost tripled between 1975 and 2016 [1] and the primary cause posited for the rapid escalation in obesity prevalence is increased availability and affordability of a wide variety of energy-dense, highly palatable foods. Palatability is conferred primarily by high simple carbohydrate and fat content, although individual differences in preference and responding indicate that palatability is also determined by subjective factors. Palatable foods are attention-grabbing and cause at least transient increases in consumption due to their high hedonic value [2, 3]. Many studies in this area have confounded palatability with perceived healthiness of foods; this may not always be appropriate as relatively ‘healthy’ foods are not always relatively unpalatable and vice versa.
One of the most effective ways of inducing sustained hyperphagia (increased food intake) in both human and animal experiments is through variety or choice paradigms, where two or more foods are provided. Indeed, the importance of variety is highlighted by the failure of some preclinical obesogenic diets based on a single food choice (e.g. high-fat (HF) pellets) to successfully induce obesity despite the diet being both high in energy and palatable [4]. The hyperphagic effects of variety are further exacerbated when one or more food choices are highly palatable, and some of the most efficacious animal models of diet-induced obesity consist of free-choice diets, such as the cafeteria diet. However, it should be noted that greater variety in energy-restricted diets improved both compliance and weight loss among obese adults [5•].
The dramatic shift in the global food environment, namely an increase in energy-dense, varied and highly palatable foods, has been associated with increased incidence of overweight and obesity. This review aims to investigate recent evidence (2014 onwards) on how access to palatable food changes neural feeding systems and subsequently feeding behaviour to drive overeating and weight gain, with a focus on environment, individual susceptibilities and stress.
Pavlovian Conditioning and Palatable Food
Feeding is necessary for survival; however, it can also be induced in response to environmental cues that signal imminent reward, rather than physiological hunger, which can subsequently drive overeating. This is achieved through Pavlovian conditioning, whereby associations are formed between a neutral environmental cue (conditioned stimulus) and a reinforcer (unconditioned stimulus)–palatable food [6]. These food-paired cues can evoke a conditioned food-seeking response during exposure to the cue, which is elicited by the expectation of imminent reward. Palatability is a strong reinforcer, amplifying the effects of Pavlovian conditioning and overriding homeostatic signals [3]. This is particularly detrimental when considering the modern food environment, in which energy-dense palatable foods are often paired with salient environmental stimuli. Overfeeding can consequently occur, even in the absence of physiological hunger [7,8,9]. Other aspects of palatable food (i.e. taste and smell) play a role, as they chemically interact with sensory organs and can alter food perception, but this aspect is beyond the scope of this review.
Effects of Palatability on Cue-Induced Overeating
In rodents, ad libitum exposure to palatable foods has been shown to induce overeating [9]. When the diet is provided intermittently, hyperphagia can be further exacerbated [10, 11]. The process whereby repeated exposure to a specific food reduces motivation to consume that substance is described as sensory-specific satiety. However, in a free-choice paradigm, new foods can reinstate hyperphagia [7, 8, 12] and induce habitual overconsumption [13], and rats on a free-choice high-fat, high-sugar (HFHS) diet do not exhibit sensory-specific satiety [14].
In humans, cues associated with palatable food can induce cravings for those and other palatable foods, leading to dysregulated eating [15]. These cravings interact with both feeding and decision-making systems to bias behaviour towards food consumption. A strong habitual feeding response may lead to increased attentional/approach bias for food cues, while poor inhibitory control may cause decreased ability to resist palatable foods [16, 17]. Salient cues are thought to modulate attention [18], although there is also evidence that the effects of Pavlovian associations on food-seeking are dependent on internal motivational state. A recent study showed that in non-satiated individuals motivated to eat, food cues had no effect on responding or consumption. However, in satiated individuals, food cues evoked new food-seeking motivation and increased consumption [7]. Furthermore, it has been demonstrated that Pavlovian cues are able to overcome sensory-specific satiety in humans, driving consumption of foods on which the participants are already satiated [8].
Environmental Cues
Food Availability
Energy-dense foods are readily perceived as widely available in today’s modern environment because of their greater convenience and accessibility. Epidemiological studies have observed positive correlations between the perceived availability of palatable foods and intake/purchase [19, 20]. A large cross-European study reported that ‘lack of willpower’, ‘busy lifestyle’ and ‘price of healthy foods’ were the most frequently perceived barriers to healthy eating. Interestingly, these factors did not correlate with the intake of sweet-tasting foods [21]. Blechert et al. (2016) demonstrated stronger activation of neural regions associated with appetitive motivation and cognitive control in healthy-weight participants shown images of food available to consume (foods that participants were told were available to consume following the brain scan) compared to unavailable foods [22]. While high-energy foods were rated higher in palatability, available foods were reportedly more well-liked, independent of energy content.
Affordability
Affordability is an important determinant of food choice. Whereas minimally processed foods are generally perceived to be costly, palatable energy-dense food items are seen as cheap and convenient [23]. Amongst lower socioeconomic groups, greater rates of fast food intake and higher BMIs have been observed [24, 25]. Perceived food cost [23, 26, 27] and food insecurity (a form of psychosocial stress associated with low socioeconomic status that may bias consumption towards cheap energy-dense foods [28]) are thought to influence the motivation to purchase palatable items. However, a more positive attitude towards healthy eating [29] and higher education attainment [30, 31] may somewhat mediate the impact of low socioeconomic status and exposure to poorer food environments. Hill et al. (2016) proposed a different view by suggesting that non-restricting individuals may more readily endorse the notion that palatable foods are inexpensive, in order to justify their food choices [32].
Advertising
Humans are constantly exposed to an abundance of sensory stimuli (i.e. visual, auditory) in advertising, which can reinforce the value of food and eating. With repeated exposure, these cues may become increasingly associated with the rewarding properties of the advertised food, increasing motivation to consume it [33, 34]. Food advertising may be predictive of weight gain in children (Table 1), but such associations remain relatively unexplored in adults. A recent study found that exposure of adult participants to ‘health-evoking posters’ led to increased healthier snack purchasing, while no posters or posters with a ‘hedonic-evoking motif’ led to unhealthier purchases [40]. This study, like others [33, 34], is subjective in its definitions of what is un/healthy and un/palatable. Dovey et al. (2017) found that most non-restrained participants (Based on the Dutch Eating Behaviour Questionnaire) chose an energy-dense palatable snack regardless of the type of advertising they were exposed to, whereas restrained participants refused snacks when shown unhealthy advertising and chose the more nutritious option when a healthy message was promoted [41]. Taken together, it seems possible that advertising can manipulate an individual’s food choices but the direction and/or extent to which this occurs may depend on the individual’s food-related restraint.
Social Norms
Humans often eat in a social context, such that our eating patterns may be implicitly guided by the expectations of those around us [42]. Most relevant studies using energy-dense palatable foods, such as cookies [43] and pizza [44], have found that participants modify the amount and types of food they consume to reflect those of their eating companions. A small study showed that participants altered their preference ratings for both healthy and unhealthy foods in accordance to the presented social norms [45]. Interestingly following manipulation of social norm, neural mechanisms initially activated by the presence of unhealthy foods became more strongly engaged by group norm rather than food healthfulness. Even so, presentation of unhealthy foods evoked greater BOLD signal (blood-oxygen-level-dependent signalling; a functional MRI measure of activity-dependent regional changes in cerebral blood flow) changes than "healthy" foods despite similarities in initial ratings of liking [45]. Another study similarly demonstrated that while participants exposed to healthy messages reported lower preferences for "unhealthy" foods, the amount of chocolate sweets taken post-study was unaffected [46]. This dissociation may suggest an internal preference for energy-dense foods that could potentially override the influence of social norms in certain individuals.
Physiological Feeding and Palatable Food Exposure
Comprehensive work has been undertaken to determine how feeding and body weight are regulated by the brain. The physiological homeostatic feeding system is often conceptualised as independent of the supraphysiological reward system, however, both systems are extensively integrated and all eating is intrinsically rewarding (illustrated in Fig. 1). Unlike other homeostatic systems, feeding is slightly biased towards a positive energy balance, thought to be due to routine food scarcity throughout evolution. Both the physiological and supraphysiological systems are affected by exposure to palatable food, further biasing behaviour towards a positive energy balance, and subsequent weight gain and obesity.
Neural feeding regions associated with changed feeding in response to palatable food exposure. Several brain regions are involved in responding to highly palatable foods, leading to increases in palatable food seeking and consumption. Sensory inputs (visual, auditory, olfactory, gustatory etc.) associated with palatable food (lower light grey arrow) are integrated in the insula and then reward value is determined by the orbitofrontal cortex (OFC). In combination with inputs from anterior cingulate cortex (ACC) and amygdala (Amyg), these regions can drive feeding dependent on food salience and palatability, and independent of energy balance, via their connections with the mesolimbic reward system—consisting of the ventral tegmental area (VTA), nucleus accumbens (NAc) and the fibres connecting these regions. The NAc modulates motor outputs (upper light grey arrow) to bias behaviour towards food seeking and consumption. The dorsolateral prefrontal cortex (PFC) is often implicated in decision making and cognitive control, and is thought to inhibit supraphysiological feeding by connections to the NAc. However, in the presence of palatable foods, this inhibitory control may be insufficient to limit hyperphagia. Key regions involved in physiological food intake, such as the arcuate nucleus of the hypothalamus (ARC) and the lateral hypothalamic area (LHA), are primary sites for the processing of internal metabolic cues and neural information. The LHA integrates this physiological information and signals to the mesolimbic reward system to drive feeding behaviour in response to energy deficit. More recent work, however, indicates that these regions may be sensitive to differences in palatability and may also drive hyperphagia in the presence of palatable foods. Brain regions are shaded according to level of involvement in palatable food overconsumption, with black representing the highest involvement and light grey indicating lower involvement. Unbroken grey and black arrows represent white matter tracts
The Arcuate Nucleus of the Hypothalamus and Responses to Palatable Food
The orexigenic neuropeptide Y/Agouti-related peptide (NPY/AgRP) and anorexigenic alpha-melanocyte stimulating hormone/cocaine-and-amphetamine related transcript (αMSH/CART) neurons of the arcuate nucleus of the hypothalamus (ARC) are the primary neurons that respond to metabolic and neural signals of changes in energy balance. They act in concert to regulate long-term feeding behaviour and metabolism. Food presentation alone can reverse the effects of ghrelin (an orexigenic peptide secreted by the gut) or fasting on these neurons’ signalling patterns. However, these changes are transient unless followed by food consumption [47••, 48]. Neural response to the presentation of palatable food (peanut butter or chocolate) was exaggerated by fasting and still present following satiety. Peanut butter presentation attenuated subsequent neural responses to chow, but not vice versa [47••]. Even brief exposure (2–6 days) to a HF diet resulted in persistent NPY/AgRP neuronal activation in mice, independent of weight gain or caloric intake [49••]. Rats provided a free-choice HFHS diet are more sensitive to centrally administered NPY, and increased their consumption of a HF diet and chow relative to rats on free-choice HF or HS diets [50]. However, targeted ablation of NPY/AgRP neurons in mice did not impact HFHS diet consumption, despite reducing chow consumption [51]. Therefore, while NPY/AgRP neurons clearly modulate response to palatable foods and show differential neural activity for these foods relative to regular chow, other neuronal populations may be contributing to feeding behaviours involving palatable foods.
The Lateral Hypothalamic Area, Orexin and Palatable Food Seeking
The lateral hypothalamic area (LHA) is considered a crucial integration site of metabolic information driving motivated behavioural responses, such as food-seeking behaviour. Orexin, a key neuropeptide involved, is able to independently promote food seeking and consumption when administered centrally, via receptors in the ventral tegmental area (VTA) [52]. Reward regions also feed back onto the LHA, and stimulation of the nucleus accumbens (NAc) shell region can suppress HF feeding by gamma-aminobutyric acid (GABA) release in the LHA [53].
The Mesolimbic Reward Pathway, Supraphysiological Feeding and Palatable Food Exposure
Increasing focus has been placed on the influence of palatable foods on reward regions as a driver of hyperphagia and obesity. The mesolimbic reward pathway is highly integral to feeding behaviour, appearing to function independently of energy status although these regions are able to sense and respond to changes in feeding-related metabolites and neuropeptides to drive feeding in times of energy deficit [54]. Human and animal literature indicates that obesity is associated with both an increased striatal response to food cues and a blunted striatal response to food consumption [55, 56]. It is posited that this altered reward responsivity observed in obese individuals may be the result of neural plastic changes resulting from prolonged overexposure to highly palatable foods [57], although there is some evidence that these differences may be inherent to obesity-prone individuals rather than an acquired characteristic.
There is limited research on the effects of short-term exposure to palatable foods on the mesolimbic system, although the animal research available suggests that even single exposures to palatable foods can increase subsequent food intake and food-seeking behaviours. This is mediated by a strengthening of excitatory synaptic transmission onto VTA dopaminergic neurons for several days following initial exposure [58], increasing dopaminergic signalling. Knockdown of VTA dopamine 2 receptors led to increased motivation for sucrose on a progressive ratio (PR) schedule, where rodents are required to perform progressively more lever presses for the same reward to measure motivation to expend effort for food. The progressive ratio breakpoint is the maximum number of responses an animal will perform for a reward before ceasing the behaviour, and is regularly used as a measure of motivation to obtain that reward. The knockdown did not impact fixed ratio responding [59], indicating that VTA dopamine 2 receptors are involved in motivation to expend effort for palatable food but do not impact feeding when a fixed amount of effort is required. In humans, BOLD signalling in the striatum in response to palatable food intake has been shown to be inversely associated with BMI but not increased palatability [60, 61].
Opioidergic signalling in the mesolimbic pathway is involved in hedonic reward, or “liking”. Delta opioid receptor knockout has been shown to reduce intake of highly palatable food, and a lower breakpoint on a PR schedule [62]. Naltrexone, an opioid receptor antagonist, has been used to treat alcohol and opioid dependence and has recently been trialled for the treatment of obesity and hyperphagia. In animal models, naltrexone infusions into either the NAc core or shell can block consumption of preferred sucrose concentrations [63]. In combination with intraperitoneal baclofen (a GABA-B receptor agonist currently being trialled as a treatment for drug dependence), intraperitoneal naltrexone can reduce intake of HF, HFHS and high-sugar (HS) diets without affecting healthy chow consumption when each palatable diet is presented alongside chow [64]. In humans, naltrexone reduces BOLD signalling response to palatable food taste and images throughout the brain [65], specifically the cingulate cortex [61, 65]. Further research is needed in humans to determine whether naltrexone can sustainably reduce hyperphagia to promote weight loss.
Endocannabinoid System
Endocannabinoid receptors are expressed throughout regions involved in both physiological and supraphysiological feeding, as well as metabolically relevant peripheral organs such as adipose tissue and liver, and increased both motivation and hedonic responding to food. Recent work has shown that blocking endocannabinoid 1 receptors (CB1R) decreases intake of a HS chow when presented alongside regular chow [66, 67]. Interestingly, Radziszewska and colleagues [66] showed that both CB1R agonists and antagonists reduced intake of a HS chow. In summary, while CB1R activation is involved in palatable food consumption, further work is required to determine whether these effects are observed across different highly palatable diets.
Feeding Peptides and the Reward System
There is substantial evidence that hypothalamic neurons project to the mesolimbic system to modulate hedonic hunger and motivation to eat. NPY infusions into both the VTA and NAc increase breakpoint in a PR paradigm, whereas NAc and LHA NPY increase free sucrose intake [68]. Similarly, intra-cerebroventricular administration of AgRP and αMSH increased and decreased PR breakpoint, respectively, which can be blocked with pre-treatment of a dopamine antagonist [69]. This indicates that these behavioural changes are dependent on the mesolimbic dopaminergic system. Infusions of orexin into the VTA did not affect motivation to acquire HF food, as tested using PR, but did increase free HF feeding and increased consumption of sucrose [70]. Therefore, a number of hypothalamic neuropeptides involved in physiological feeding can act in the mesolimbic system to modulate both free and effort-dependent consumption of palatable foods.
Recent work tying feeding peptides, reward circuitry and palatable food consumption has focused on glucagon-like peptide (GLP-1) and oxytocin as they appear to reduce consumption of highly palatable foods without affecting healthy food intake, indicating potential clinical relevance.
Glucagon-Like Peptide
First recognised as a blood glucose-regulating peptide produced in the small intestine, GLP-1 also functions as an endogenous anorexigenic neuropeptide in the nucleus of the solitary tract (NTS) and liraglutide, a long-acting GLP-1 receptor agonist, is currently used as a weight loss treatment in obesity. Although there is some evidence that these anorexigenic effects may be specific to HF diets, the results are mixed. GLP-1 administration into the VTA [71] and exendin-4, a GLP-1 receptor agonist, intraperitoneally [72], reduce HF diet consumption in rodents, while exendin-4 administration into the cerebral aqueduct and parabrachial nucleus had no effect on HF diet consumption. In contrast, administration into the lateral parabrachial nucleus [73], medial NTS [74] or ventral hippocampus [75] reduced both regular and HF diet intake. Hsu et al. showed that in a choice paradigm, intake of western diet was reduced while chow consumption remained unaffected [75].
Interestingly, intraperitoneal exendin-4 can be used to reduce HF diet intake in the long-term to promote weight loss in rats. While rats initially also reduced chow consumption with exendin-4 treatment, this effect was transient and chow consumption rapidly returned to normal [72]. Additionally, intraperitoneal exendin-4 reduced consumption of HS pellets while slightly increasing intake of healthy chow [66].
Exendin-4 administration into the medial NTS reduced breakpoint for sucrose on a PR schedule as well as reducing conditioned place preference for palatable food [74]. Administration into the ventral hippocampus reduced PR breakpoint while not impacting conditioned place preference for food [75]. Administration of exendin-4 into the lateral parabrachial nucleus reduced breakpoint on a PR schedule [73]. Therefore, while GLP-1 agonism throughout the brain appears to reduce motivation to work for palatable food, reductions in food-seeking behaviour may be regionally dependent.
In humans, intravenous exendin-4 administration has been shown to reduce food intake while also increasing BOLD responses to palatable chocolate milk intake and reducing BOLD signalling in response to anticipatory cues of chocolate milk [76]. Thylakoid supplementation, known to increase GLP-1, has been shown to reduce both cravings for unhealthy snacks [77, 78] as well as overall food and snack consumption [78]. In conclusion, GLP-1 appears to effectively reduce both free consumption and motivation to consume palatable foods, although more work is needed to elucidate whether these changes are only observed for HF diets.
Oxytocin
Well-recognised for its role in childbirth and lactation, oxytocin has more recently been shown to play a role in several motivated behaviours, including sexual intercourse, lactation, social bonding and feeding. It is released centrally in response to stomach distention, elevated plasma osmolality and toxin-tainted foods to suppress feeding. Interestingly, recent studies indicate that oxytocin may also modulate overconsumption of palatable foods. In a recent study in rodents, oxytocin was injected directly into the ventromedial nucleus of the hypothalamus, involved in anorexigenic control of feeding, reduced short-term feeding without affecting non-caloric saccharin consumption and transiently increased energy expenditure and spontaneous activity [79].
Most recent preclinical work with oxytocin has involved peripheral administration. Intraperitoneal oxytocin administration in rodents has been shown to reduce food intake transiently dose-dependently [80, 81], as has nasal oxytocin administration [82]. However, the effect of oxytocin treatment on consumption of palatable foods is currently controversial; some studies have shown that oxytocin attenuates palatable food consumption [83, 84], while others have shown no effect [81]. These differences may be due to experimental paradigm, since oxytocin appears to inhibit palatable food consumption in choice paradigms only. One recent study in obese rhesus monkeys showed that chronic subcutaneous administration of oxytocin was able to reduce body weight and prevent rebound-hyperphagia following weight loss; although interestingly, intake of a palatable fructose-sweetened beverage was unchanged [85]. In summary, while oxytocin does appear to suppress appetite in preclinical models, the evidence for specific effects of oxytocin on palatable food intake is mixed.
Nasal administration of oxytocin has been shown to reduce food craving in women in response to palatable food images when they are instructed to control the urge to eat [86], indicating that oxytocin may prove a useful adjunctive therapy to diet in weight loss regimens. A small study conducted in men using a food choice paradigm revealed that while oxytocin treatment did not impact food choice across a range of caloric densities, it did reduce total caloric intake, particularly fat [87•]. The limited work conducted suggests oxytocin may be a promising treatment to inhibit palatable food consumption to reduce obesity. However, since oxytocin has a broad range of effects centrally, long-term use in humans will need to be further researched to preclude adverse social and sexual effects.
Metabolic Signals Impacting Palatable Food Consumption—Leptin and Ghrelin
Leptin is a powerful anorexigenic adipokine released by adipose tissue that directly acts on the NPY/AgRP and POMC/CART neurons of the ARC, as well as other regions involved in feeding regulation. Leptin levels in the blood are directly associated with adipose tissue volume, and is often used as a measure of adiposity. Leptin administration both peripherally and centrally reduces food intake, although this is not observed in rats fed with a free-choice HFHS diet [50].
Leptin is a key signalling peptide linking metabolic changes to reward signalling. Leptin pre-treatment prevented increased dopaminergic signalling in the ventral tegmental area (VTA), a key reward region, in response to food cues in food-restricted rats [88]. Leptin can also modulate motivation to eat via actions at the NTS. Leptin injected into the medial NTS has been shown to reduce the PR breakpoint for sucrose in both food-restricted and non-restricted rats [89]. This indicates that leptin status may affect food-seeking behaviour.
Ghrelin, predominantly produced in the stomach, is a potent orexigenic peptide. While the physiological feeding system is highly sensitive to changes in circulating ghrelin, increasing evidence indicates that the mesolimbic system is a key target for this peptide, suggesting a role for ghrelin in hedonic feeding. In rodents, intra-VTA ghrelin has been shown to increase HF diet consumption in both sated and fasted rats [90,91,92] and increase responses to previous food cues in a reinstatement paradigm [91]. These central effects have been replicated in humans using peripheral ghrelin administration, which significantly increased ratings of high-energy food palatability and associated orbitofrontal cortex (OFC) activation, a region associated with food reward valuation [93]. Despite this evidence that ghrelin can drive consumption of high-energy foods, particularly HF diets, ablation of ghrelin secreting cells in mice has been shown to not affect HF feeding [94], indicating that ghrelin’s function driving consumption of HF food may be redundant.
Predisposition to Overeat Palatable Foods—Food Addiction and Impulsivity
While the rapid growth in obesity prevalence points to changes in environmental rather than genetic determinants, individual differences observed in the population indicate thatthese environmental effects must be at least partially moderated by individual susceptibility. Differences in reward system vulnerability, as well as trait impulsivity, may predispose individuals unduly to hyperphagia and obesity.
Whether humans are subject to food addiction, whereby some foods can induce compulsive, addiction-like overeating, and its relationship to obesity has been extensively reviewed over the last 5 years. While scoring highly on food addiction scales is positively associated with BMI, most human studies indicate that food addiction is most closely associated with binge eating disorder [56]. Additionally, there is evidence that the observed differences in reward system responsivity in obesity are unlikely to be genetic; large population-based studies have failed to show associations between dopamine and opioid receptor polymorphisms and adiposity [95]. Despite this, one genome-wide association study identified the mu-opioid receptor gene locus as most closely associated with reported fat intake [96].
Research aimed at identifying behavioural and neural differences that predispose animals to obesity has involved work with obese-prone and obese-resistant strains of rats. A recent study has indicated that obese-prone rats engage in less locomotor activity, and are more sensitive to dopamine 2 receptor stimulation [97]. This builds on earlier work suggesting that obesity-proneness may be associated with differences in dopaminergic responsivity.
While there is limited work in adults investigating inherent differences in reward circuitry functioning that lead to obesity, a number of longitudinal studies (see Table 1) have been conducted in adolescents, where BOLD signalling responses to food cues or consumption have been associated with subsequent BMI changes. These studies indicate that activation in regions involved in reward, taste perception and affective significance can predict weight gain, indicating that some of the changes observed in BOLD signalling in obese individuals may predate their obesity. However, all these studies have been conducted by one research group and independent replication would help support these findings.
Impulsivity is frequently associated with dysregulated feeding behaviour and hyperphagia. When rats were separated into high- and low-impulsive responders, impulsivity predicted excessive intake, heightened motivation and compulsive-like eating in rats exposed to highly palatable food [98]. Furthermore, in a study of over 800 undergraduate students, the only trait found to be associated with food addiction scores was negative urgency, or the tendency to act impulsively when under stress [99]. These studies indicate that impulsivity may underpin hyperphagia in some individuals.
Environmental Stress
Stress Exposure in Adulthood
When under stressful conditions, we may comfort eat, i.e. ingest palatable foods to reduce negative feelings or discomfort. However, rodents will voluntarily prioritise HF, HS or HFHS foods, whether exposed to stress [100] or not [101]. Upon palatable food withdrawal, increased anxiety- and depressive-like behaviours [102] and changes in metabolic parameters associated with elevated stress levels [101] have been observed. However, despite extensive research, the relationship between exposure to palatable foods and stress responsivity remains unclear. In rodent models, factors such as feeding schedules and sex of the rat may contribute to the observed variability in results. In male rats, providing palatable diet ad libitum has been shown to have both anxiolytic [103] and anxiety- and anhedonia-inducing [104] effects, and palatable food intake was reduced with daily exposure to variable stressors [100]. Conversely, in female rats, a similar protocol evoked hyperphagia and anxiety- and depressive-like behaviours [105]. Intermittent feeding may further impair responding for palatable food rewards, by causing compulsive feeding that is resistant to aversive cues such as foot-shock in rodents [106, 107••], and is thought to similarly drive compulsive overeating in humans [108].
In human research, there is consensus that dysregulations in eating behaviour can occur following stress exposure, but variable results have been reported. Chronic exposure to stress and hyperphagia are positively associated [109, 110]. A longitudinal study of young adults observed significant positive associations between BMI and coping and reward [111]. However, stress-induced reductions in food intake have also been reported [112]. Pool et al. (2014) found greater ‘wanting’ in response to food cues following stress in participants, but no increased ‘liking’ [18]. Therefore, stress may evoke increased food-seeking independent of its hedonic pleasure. Outside of the laboratory, reductions in hedonic/taste-driven eating [112] and increased ‘emotional’ eating [113] following stress exposure have similarly been reported. However, additional factors, including BMI [110] and emotional eating style [112], may modify how and what an individual chooses to eat when stressed. Some studies have suggested that high emotional eaters experience higher levels of stress [113], and respond preferentially to hedonic rather than physiological cues [112]. Given the extensive variations in stress responding, tailoring clinical weight loss treatments to individual emotional eating styles may be beneficial and should be further investigated.
Childhood Exposure to Stress
Maladaptive coping strategies that lead to stress-induced eating during adulthood may subsequently develop as a consequence of childhood exposure to stress. Studies have demonstrated both increases [114•, 115] and marginal reductions [117] in the amount of high-energy palatable food consumed by adult rodents exposed to early life stressors (i.e. restraint, tail pinch). But whether the provision of palatable diet ameliorates or worsens, anxiety-like behaviours remain contentious. Juvenile exposure to stress is thought to alter central and metabolic parameters that may predispose rodents to the development of obesity when exposed to high-energy diets in adulthood [116]. In humans, particularly females, positive correlations between childhood trauma and comfort eating in adulthood have been demonstrated [118, 119]. The limited work conducted suggests that childhood stress may contribute to the programming of individual eating patterns and preferences for palatable energy-dense foods, predisposing people to weight gain later in life. As most animal models of juvenile stress focus on the effects of palatable diet exposure in adulthood, it would be interesting for future research to investigate the long-term impact of childhood stress on feeding patterns and anxiety when concomitantly exposed to palatable foods during childhood.
Conclusions and Future Research Questions
Highly palatable food and associated cues can trigger hyperphagia by modulating both physiological and supraphysiological feeding. However, individual differences in sensitivity to palatable foods result in variable responses, and not all individuals will overeat. Further research is required to identify what aspects of palatable food (macronutrient content, variety etc.) are more likely to drive overeating, and more animal work into the specific effects of variety should assist in better modelling the obesogenic environment created by modern human living. Much of the human literature published to date does not adequately assess differences in palatability, often assuming “healthy” and “unhealthy” foods are unpalatable and palatable respectively. Future research would benefit from appropriate quantification of palatability, making use of rating systems and surveys.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. Obesity and overweight: fact sheet. www.who.int. 2017. Accessed November 2017.
Berthoud H-R, Lenard NR, Shin AC. Food reward, hyperphagia, and obesity. Am J Physiol Regul Integr Comp Physiol. 2011;300(6):R1266–R77. https://doi.org/10.1152/ajpregu.00028.2011.
Morris MJ, Beilharz JE, Maniam J, Reichelt AC, Westbrook RF. Why is obesity such a problem in the 21st century? The intersection of palatable food, cues and reward pathways, stress, and cognition. Neurosci Biobehav Rev. 2015;58:36–45. https://doi.org/10.1016/j.neubiorev.2014.12.002.
Barrett P, Mercer JG, Morgan PJ. Preclinical models for obesity research. Dis Model Mech. 2016;9(11):1245–55. https://doi.org/10.1242/dmm.026443.
• Vadiveloo M, Sacks FM, Champagne CM, Bray GA, Mattei J. Greater healthful dietary variety is associated with greater 2-year changes in weight and adiposity in the preventing overweight using novel dietary strategies (POUNDS lost) trial. J Nutr. 2016;146(8):1552–9. https://doi.org/10.3945/jn.115.224683. This reference is interesting; it shows, somewhat unintuitively, that food variety in dieting humans can improve compliance and weight loss.
Havermans RC. Pavlovian craving and overeating: a conditioned incentive model. Curr Obes Rep. 2013;2(2):165–70. https://doi.org/10.1007/s13679-013-0053-z.
Colagiuri B, Lovibond PF. How food cues can enhance and inhibit motivation to obtain and consume food. Appetite. 2015;84:79–87. https://doi.org/10.1016/j.appet.2014.09.023.
Watson P, Wiers RW, Hommel B, de Wit S. Working for food you don’t desire. Cues interfere with goal-directed food-seeking. Appetite. 2014;79:139–48. https://doi.org/10.1016/j.appet.2014.04.005.
Reichelt AC, Morris MJ, Westbrook RF. Cafeteria diet impairs expression of sensory-specific satiety and stimulus-outcome learning. Front Psychol. 2014;5(852) https://doi.org/10.3389/fpsyg.2014.00852.
Furlong TM, Jayaweera HK, Balleine BW, Corbit LH. Binge-like consumption of a palatable food accelerates habitual control of behavior and is dependent on activation of the dorsolateral striatum. J Neurosci. 2014;34(14):5012–22. https://doi.org/10.1523/jneurosci.3707-13.2014.
Kendig MD, Cheung AMK, Raymond JS, Corbit LH. Contexts paired with junk food impair goal-directed behavior in rats: implications for decision making in obesogenic environments. Front Behav Neurosci. 2016;10:216. https://doi.org/10.3389/fnbeh.2016.00216.
Parkes SL, Furlong TM, Black AD, Balleine BW. Intermittent feeding alters sensitivity to changes in reward value. Appetite. 2017;113:1–6. https://doi.org/10.1016/j.appet.2017.02.009.
Corbit LH. Effects of obesogenic diets on learning and habitual responding. Curr Opin Behav Sci. 2016;9:84–90. https://doi.org/10.1016/j.cobeha.2016.02.010.
Myers KP. Sensory-specific satiety is intact in rats made obese on a high-fat high-sugar choice diet. Appetite. 2017;112:196–200. https://doi.org/10.1016/j.appet.2017.01.013.
Potenza MN, Grilo CM. How relevant is food craving to obesity and its treatment? Front Psychiatry. 2014;5:164. https://doi.org/10.3389/fpsyt.2014.00164.
Kakoschke N, Kemps E, Tiggemann M. Combined effects of cognitive bias for food cues and poor inhibitory control on unhealthy food intake. Appetite. 2015;87:358–64. https://doi.org/10.1016/j.appet.2015.01.004.
Meule A, Lutz APC, Vögele C, Kübler A. Impulsive reactions to food-cues predict subsequent food craving. Eat Behav. 2014;15(1):99–105. https://doi.org/10.1016/j.eatbeh.2013.10.023.
Pool E, Brosch T, Delplanque S, Sander D. Where is the chocolate? Rapid spatial orienting toward stimuli associated with primary rewards. Cognition. 2014;130(3):348–59. https://doi.org/10.1016/j.cognition.2013.12.002.
Gordon-Larsen P. Food availability/convenience and obesity. Adv Nutr. 2014;5(6):809–17. https://doi.org/10.3945/an.114.007070.
Vedovato GM, Trude ACB, Kharmats AY, Martins PA. Degree of food processing of household acquisition patterns in a Brazilian urban area is related to food buying preferences and perceived food environment. Appetite. 2015;87:296–302. https://doi.org/10.1016/j.appet.2014.12.229.
Pinho MGM, Mackenbach JD, Charreire H, Oppert JM, Bárdos H, Glonti K, et al. Exploring the relationship between perceived barriers to healthy eating and dietary behaviours in European adults. Eur J Nutr. 2017; https://doi.org/10.1007/s00394-017-1458-3.
Blechert J, Klackl J, Miedl SF, Wilhelm FH. To eat or not to eat: effects of food availability on reward system activity during food picture viewing. Appetite. 2016;99:254–61. https://doi.org/10.1016/j.appet.2016.01.006.
Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643–60. https://doi.org/10.1093/nutrit/nuv027.
Watts AW, Mason SM, Loth K, Larson N, Neumark-Sztainer D. Socioeconomic differences in overweight and weight-related behaviors across adolescence and young adulthood: 10-year longitudinal findings from Project EAT. Prev Med. 2016;87:194–9. https://doi.org/10.1016/j.ypmed.2016.03.007.
Miura K, Turrell G. Reported consumption of takeaway food and its contribution to socioeconomic inequalities in body mass index. Appetite. 2014;74:116–24. https://doi.org/10.1016/j.appet.2013.12.007.
Rummo PE, Meyer KA, Green Howard A, Shikany JM, Guilkey DK, Gordon-Larsen P. Fast food price, diet behavior, and cardiometabolic health: differential associations by neighborhood SES and neighborhood fast food restaurant availability in the CARDIA study. Health Place. 2015;35:128–35. https://doi.org/10.1016/j.healthplace.2015.06.010.
Meyer KA, Guilkey DK, Ng SW, Duffey KJ, Popkin BM, Kiefe CI, et al. Sociodemographic differences in fast food price sensitivity. JAMA Intern Med. 2014;174(3):434–42. https://doi.org/10.1001/jamainternmed.2013.13922.
Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114(12):1943–53.e2. https://doi.org/10.1016/j.jand.2014.06.353.
Aggarwal A, Monsivais P, Cook AJ, Drewnowski A. Positive attitude toward healthy eating predicts higher diet quality at all cost levels of supermarkets. J Acad Nutr Diet. 2014;114(2):266–72. https://doi.org/10.1016/j.jand.2013.06.006.
Vogel C, Lewis D, Ntani G, Cummins S, Cooper C, Moon G, et al. The relationship between dietary quality and the local food environment differs according to level of educational attainment: a cross-sectional study. PLoS One. 2017;12(8):e0183700. https://doi.org/10.1371/journal.pone.0183700.
Burgoine TH, Forouhi NG, Griffin SJ, Brage S, Wareham NJ, Monsivais P. Does neighborhood fast-food outlet exposure amplify inequalities in diet and obesity? A cross-sectional study. Am J Clin Nutr. 2016;103(6):1540–7. https://doi.org/10.3945/ajcn.115.128132.
Hill SE, Baskett K, Bradshaw HK, Prokosch ML, DelPriore DJ, Rodeheffer CD. Tempting foods and the affordability axiom: food cues change beliefs about the costs of healthy eating. Appetite. 2016;107:274–9. https://doi.org/10.1016/j.appet.2016.08.014.
Kemps E, Tiggemann M, Hollitt S. Exposure to television food advertising primes food-related cognitions and triggers motivation to eat. Health Psychol. 2014;29(10):1192–205. https://doi.org/10.1080/08870446.2014.918267.
Bailey RL. Modern foraging: presence of food and energy density influence motivational processing of food advertisements. Appetite. 2016;107:568–74. https://doi.org/10.1016/j.appet.2016.09.001.
Burger KS, Stice E. Greater striatopallidal adaptive coding during cue-reward learning and food reward habituation predict future weight gain. NeuroImage. 2014;99:122–8. https://doi.org/10.1016/j.neuroimage.2014.05.066.
Yokum S, Gearhardt AN, Harris JL, Brownell KD, Stice E. Individual differences in striatum activity to food commercials predict weight gain in adolescents. Obesity. 2014;22(12):2544–51. https://doi.org/10.1002/oby.20882.
Stice E, Burger KS, Yokum S. Reward region responsivity predicts future weight gain and moderating effects of the TaqIA allele. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2015;35(28):10316–24. https://doi.org/10.1523/jneurosci.3607-14.2015.
Stice E, Yokum S. Gain in body fat is associated with increased striatal response to palatable food cues, whereas body fat stability is associated with decreased striatal response. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience. 2016;36(26):6949–56. https://doi.org/10.1523/jneurosci.4365-15.2016.
Winter SR, Yokum S, Stice E, Osipowicz K, Lowe MR. Elevated reward response to receipt of palatable food predicts future weight variability in healthy-weight adolescents. Am J Clin Nutr. 2017;105(4):781–9. https://doi.org/10.3945/ajcn.116.141143.
Stöckli S, Stämpfli AE, Messner C, Brunner TA. An (un)healthy poster: when environmental cues affect consumers’ food choices at vending machines. Appetite. 2016;96:368–74. https://doi.org/10.1016/j.appet.2015.09.034.
Dovey TM, Torab T, Yen D, Boyland EJ, Halford JCG. Responsiveness to healthy advertisements in adults: an experiment assessing beyond brand snack selection and the impact of restrained eating. Appetite. 2017;112:102–6. https://doi.org/10.1016/j.appet.2017.01.015.
Higgs S. Social norms and their influence on eating behaviours. Appetite. 2015;86:38–44. https://doi.org/10.1016/j.appet.2014.10.021.
Robinson E, Fleming A, Higgs S. Prompting healthier eating: testing the use of health and social norm based messages. Health Psychol. 2014;33(9):1057–64. https://doi.org/10.1037/a0034213.
Feeney JR, Pliner P, Polivy J, Herman CP. The persistence of and resistance to social norms regarding the appropriate amount to eat: a preliminary investigation. Appetite. 2017;109:93–9. https://doi.org/10.1016/j.appet.2016.11.031.
Nook EC, Zaki J. Social norms shift behavioral and neural responses to foods. J Cogn Neurosci. 2015;27(7):1412–26. https://doi.org/10.1162/jocn_a_00795.
Templeton EM, Stanton MV, Zaki J. Social norms shift preferences for healthy and unhealthy foods. PLoS One. 2016;11(11):e0166286. https://doi.org/10.1371/journal.pone.0166286.
•• Chen Y, Lin Y-C, Kuo T-W, Knight ZA. Sensory detection of food rapidly modulates arcuate feeding circuits. Cell. 2015;160(5):829–41. https://doi.org/10.1016/j.cell.2015.01.033. This paper demonstrates that arcuate feeding circuits respond differentially to palatable foods when compared to regular foods.
Beutler LR, Chen Y, Ahn JS, Lin Y-C, Essner RA, Knight ZA. Dynamics of gut-brain communication underlying hunger. Neuron. 2017;96(2):461–75.e5. https://doi.org/10.1016/j.neuron.2017.09.043.
•• Wei W, Pham K, Gammons JW, Sutherland D, Liu Y, Smith A, et al. Diet composition, not calorie intake, rapidly alters intrinsic excitability of hypothalamic AgRP/NPY neurons in mice. Sci Rep. 2015;5(1):16810. https://doi.org/10.1038/srep16810. The authors demonstrate that short exposures to diet can induce similar arcuate signalling changes as observed in long-term diet, and are independent of energy intake and adiposity.
van den Heuvel JK, Eggels L, van Rozen AJ, Luijendijk MCM, Fliers E, Kalsbeek A, et al. Neuropeptide Y and leptin sensitivity is dependent on diet composition. J Neuroendocrinol. 2014;26(6):377–85. https://doi.org/10.1111/jne.12155.
Denis RG, Joly-Amado A, Webber E, Langlet F, Schaeffer M, Padilla SL, et al. Palatability can drive feeding independent of AgRP neurons. Cell Metab. 2015;22(4):646–57. https://doi.org/10.1016/j.cmet.2015.07.011.
Valdivia S, Patrone A, Reynaldo M, Perello M. Acute high fat diet consumption activates the mesolimbic circuit and requires orexin signaling in a mouse model. PLoS One. 2014;9(1):e87478. https://doi.org/10.1371/journal.pone.0087478.
Wei N, Wang Y, Wang X, He Z, Zhang M, Zhang X, et al. The different effects of high-frequency stimulation of the nucleus accumbens shell and core on food consumption are possibly associated with different neural responses in the lateral hypothalamic area. Neuroscience. 2015;301:312–22. https://doi.org/10.1016/j.neuroscience.2015.06.006.
Liu S, Borgland SL. Regulation of the mesolimbic dopamine circuit by feeding peptides. Neuroscience. 2015;289:19–42. https://doi.org/10.1016/j.neuroscience.2014.12.046.
Gilbert JR, Burger KS. Neuroadaptive processes associated with palatable food intake: present data and future directions. Curr Opin Behav Sci. 2016;9:91–6. https://doi.org/10.1016/j.cobeha.2016.02.033.
Leigh S-J, Morris MJ. The role of reward circuitry and food addiction in the obesity epidemic: an update. Biol Psychol. 2016;131:31–42. https://doi.org/10.1016/j.biopsycho.2016.12.013.
de Macedo IC, de Freitas JS, da Silva Torres IL. The influence of palatable diets in reward system activation: a mini review. Adv Pharmacol Sci. 2016;2016:7238679–7. https://doi.org/10.1155/2016/7238679.
Liu S, Globa AK, Mills F, Naef L, Qiao M, Bamji SX, et al. Consumption of palatable food primes food approach behavior by rapidly increasing synaptic density in the VTA. Proc Natl Acad Sci U S A. 2016;113(9):2520–5. https://doi.org/10.1073/pnas.1515724113.
de Jong JW, Roelofs TJ, Mol FM, Hillen AE, Meijboom KE, Luijendijk MC, et al. Reducing ventral tegmental dopamine D2 receptor expression selectively boosts incentive motivation. Neuropsychopharmacology. 2015;40(9):2085–95. https://doi.org/10.1038/npp.2015.60.
Cosgrove KP, Veldhuizen MG, Sandiego CM, Morris ED, Small DM. Opposing relationships of BMI with BOLD and dopamine D2/3 receptor binding potential in the dorsal striatum. Synapse. 2015;69(4):195–202. https://doi.org/10.1002/syn.21809.
Wang GJ, Tomasi D, Volkow ND, Wang R, Telang F, Caparelli EC, et al. Effect of combined naltrexone and bupropion therapy on the brain’s reactivity to food cues. Int J Obes. 2014;38(5):682–8. https://doi.org/10.1038/ijo.2013.145.
Mancino S, Mendonca-Netto S, Martin-Garcia E, Maldonado R. Role of DOR in neuronal plasticity changes promoted by food-seeking behaviour. Addict Biol. 2017;22(5):1179–90. https://doi.org/10.1111/adb.12401.
Katsuura Y, Taha SA. Mu opioid receptor antagonism in the nucleus accumbens shell blocks consumption of a preferred sucrose solution in an anticipatory contrast paradigm. Neuroscience. 2014;261:144–52. https://doi.org/10.1016/j.neuroscience.2013.12.004.
Avena NM, Bocarsly ME, Murray S, Gold MS. Effects of baclofen and naltrexone, alone and in combination, on the consumption of palatable food in male rats. Exp Clin Psychopharmacol. 2014;22(5):460–7. https://doi.org/10.1037/a0037223.
Murray E, Brouwer S, McCutcheon R, Harmer CJ, Cowen PJ, McCabe C. Opposing neural effects of naltrexone on food reward and aversion: implications for the treatment of obesity. Psychopharmacology. 2014;231(22):4323–35. https://doi.org/10.1007/s00213-014-3573-7.
Radziszewska E, Wolak M, Bojanowska E. Concurrent pharmacological modification of cannabinoid-1 and glucagon-like peptide-1 receptor activity affects feeding behavior and body weight in rats fed a free-choice, high-carbohydrate diet. Behav Pharmacol. 2014;25(1):53–60. https://doi.org/10.1097/fbp.0000000000000018.
Wierucka-Rybak M, Wolak M, Bojanowska E. The effects of leptin in combination with a cannabinoid receptor 1 antagonist, AM 251, or cannabidiol on food intake and body weight in rats fed a high-fat or a free-choice high sugar diet. J Physiol Pharmacol. 2014;65(4):487–96.
Pandit R, Luijendijk MC, Vanderschuren LJ, la Fleur SE, Adan RA. Limbic substrates of the effects of neuropeptide Y on intake of and motivation for palatable food. Obesity. 2014;22(5):1216–9. https://doi.org/10.1002/oby.20718.
Pandit R, van der Zwaal EM, Luijendijk MC, Brans MA, van Rozen AJ, Oude Ophuis RJ, et al. Central melanocortins regulate the motivation for sucrose reward. PLoS One. 2015;10(3):e0121768. https://doi.org/10.1371/journal.pone.0121768.
Terrill SJ, Hyde KM, Kay KE, Greene HE, Maske CB, Knierim AE, et al. Ventral tegmental area orexin 1 receptors promote palatable food intake and oppose postingestive negative feedback. Am J Physiol Regul Integr Comp Physiol. 2016;311(3):R592–9. https://doi.org/10.1152/ajpregu.00097.2016.
Wang XF, Liu JJ, Xia J, Liu J, Mirabella V, Pang ZP. Endogenous glucagon-like peptide-1 suppresses high-fat food intake by reducing synaptic drive onto mesolimbic dopamine neurons. Cell Rep. 2015;12(5):726–33. https://doi.org/10.1016/j.celrep.2015.06.062.
Yang Y, Moghadam AA, Cordner ZA, Liang N-C, Moran TH. Long term exendin-4 treatment reduces food intake and body weight and alters expression of brain homeostatic and reward markers. Endocrinology. 2014;155(9):3473–83. https://doi.org/10.1210/en.2014-1052.
Alhadeff AL, Baird J-P, Swick JC, Hayes MR, Grill HJ. Glucagon-like peptide-1 receptor signaling in the lateral parabrachial nucleus contributes to the control of food intake and motivation to feed. Neuropsychopharmacology. 2014;39(9):2233–43. https://doi.org/10.1038/npp.2014.74.
Alhadeff AL, Grill HJ. Hindbrain nucleus tractus solitarius glucagon-like peptide-1 receptor signaling reduces appetitive and motivational aspects of feeding. Am J Physiol Regul Integr Comp Physiol. 2014;307(4):R465–70. https://doi.org/10.1152/ajpregu.00179.2014.
Hsu TM, Hahn JD, Konanur VR, Lam A, Kanoski SE. Hippocampal GLP-1 receptors influence food intake, meal size, and effort-based responding for food through volume transmission. Neuropsychopharmacology. 2015;40(2):327–37. https://doi.org/10.1038/npp.2014.175.
van Bloemendaal L, Veltman DJ, Ten Kulve JS, Groot PF, Ruhe HG, Barkhof F, et al. Brain reward-system activation in response to anticipation and consumption of palatable food is altered by glucagon-like peptide-1 receptor activation in humans. Diabetes Obes Metab. 2015;17(9):878–86. https://doi.org/10.1111/dom.12506.
Montelius C, Erlandsson D, Vitija E, Stenblom E-L, Egecioglu E, Erlanson-Albertsson C. Body weight loss, reduced urge for palatable food and increased release of GLP-1 through daily supplementation with green-plant membranes for three months in overweight women. Appetite. 2014;81:295–304. https://doi.org/10.1016/j.appet.2014.06.101.
Stenblom E-L, Egecioglu E, Landin-Olsson M, Erlanson-Albertsson C. Consumption of thylakoid-rich spinach extract reduces hunger, increases satiety and reduces cravings for palatable food in overweight women. Appetite. 2015;91:209–19. https://doi.org/10.1016/j.appet.2015.04.051.
Noble EE, Billington CJ, Kotz CM, Wang C. Oxytocin in the ventromedial hypothalamic nucleus reduces feeding and acutely increases energy expenditure. Am J Phys. 2014;307(6):R737–R45. https://doi.org/10.1152/ajpregu.00118.2014.
Iwasaki Y, Maejima Y, Suyama S, Yoshida M, Arai T, Katsurada K, et al. Peripheral oxytocin activates vagal afferent neurons to suppress feeding in normal and leptin-resistant mice: a route for ameliorating hyperphagia and obesity. Am J Phys. 2015;308(5):R360–R9. https://doi.org/10.1152/ajpregu.00344.2014.
Klockars A, Brunton C, Li L, Levine AS, Olszewski PK. Intravenous administration of oxytocin in rats acutely decreases deprivation-induced chow intake, but it fails to affect consumption of palatable solutions. Peptides. 2017;93:13–9. https://doi.org/10.1016/j.peptides.2017.04.010.
Maejima Y, Rita RS, Santoso P, Aoyama M, Hiraoka Y, Nishimori K, et al. Nasal oxytocin administration reduces food intake without affecting locomotor activity and glycemia with c-Fos induction in limited brain areas. Neuroendocrinology. 2015;101(1):35–44. https://doi.org/10.1159/000371636.
Herisson FM, Brooks LL, Waas JR, Levine AS, Olszewski PK. Functional relationship between oxytocin and appetite for carbohydrates versus saccharin. Neuroreport. 2014;25(12):909–14. https://doi.org/10.1097/wnr.0000000000000201.
Sinclair MS, Perea-Martinez I, Abouyared M, St. John SJ, Chaudhari N. Oxytocin decreases sweet taste sensitivity in mice. Physiol Behav. 2015;141:103–10. https://doi.org/10.1016/j.physbeh.2014.12.048.
Blevins JE, Graham JL, Morton GJ, Bales KL, Schwartz MW, Baskin DG, et al. Chronic oxytocin administration inhibits food intake, increases energy expenditure, and produces weight loss in fructose-fed obese rhesus monkeys. Am J Phys. 2015;308(5):R431–R8. https://doi.org/10.1152/ajpregu.00441.2014.
Striepens N, Schroter F, Stoffel-Wagner B, Maier W, Hurlemann R, Scheele D. Oxytocin enhances cognitive control of food craving in women. Hum Brain Mapp. 2016;37(12):4276–85. https://doi.org/10.1002/hbm.23308.
• Lawson EA, Marengi DA, DeSanti RL, Holmes TM, Schoenfeld DA, Tolley CJ. Oxytocin reduces caloric intake in men. Obesity. 2015;23(5):950–6. https://doi.org/10.1002/oby.21069. This paper showed that despite no changes in food choice, men consumed less energy and fat in a buffet when treated with oxytocin.
van der Plasse G, van Zessen R, Luijendijk MC, Erkan H, Stuber GD, Ramakers GM, et al. Modulation of cue-induced firing of ventral tegmental area dopamine neurons by leptin and ghrelin. Int J Obes. 2015;39(12):1742–9. https://doi.org/10.1038/ijo.2015.131.
Kanoski SE, Alhadeff AL, Fortin SM, Gilbert JR, Grill HJ. Leptin signaling in the medial nucleus tractus solitarius reduces food seeking and willingness to work for food. Neuropsychopharmacology. 2014;39(3):605–13. https://doi.org/10.1038/npp.2013.235.
Wei XJ, Sun B, Chen K, Lv B, Luo X, Yan JQ. Ghrelin signaling in the ventral tegmental area mediates both reward-based feeding and fasting-induced hyperphagia on high-fat diet. Neuroscience. 2015;300:53–62. https://doi.org/10.1016/j.neuroscience.2015.05.001.
St-Onge V, Watts A, Abizaid A. Ghrelin enhances cue-induced bar pressing for high fat food. Horm Behav. 2016;78:141–9. https://doi.org/10.1016/j.yhbeh.2015.11.005.
Schele E, Bake T, Rabasa C, Dickson SL. Centrally administered ghrelin acutely influences food choice in rodents. PLoS One. 2016;11(2):e0149456. https://doi.org/10.1371/journal.pone.0149456.
Goldstone AP, Prechtl CG, Scholtz S, Miras AD, Chhina N, Durighel G, et al. Ghrelin mimics fasting to enhance human hedonic, orbitofrontal cortex, and hippocampal responses to food. Am J Clin Nutr. 2014;99(6):1319–30. https://doi.org/10.3945/ajcn.113.075291.
McFarlane MR, Brown MS, Goldstein JL, Zhao T-J. Induced ablation of ghrelin cells in adult mice does not decrease food intake, body weight, or response to high fat diet. Cell Metab. 2014;20(1):54–60. https://doi.org/10.1016/j.cmet.2014.04.007.
Hardman CA, Rogers PJ, Timpson NJ, Munafò MR. Lack of association between DRD2 and OPRM1 genotypes and adiposity. Int J Obes. 2014;38(5):730–6. https://doi.org/10.1038/ijo.2013.144.
Haghighi A, Melka MG, Bernard M, Abrahamowicz M, Leonard GT, Richer L, et al. Opioid receptor mu 1 gene, fat intake and obesity in adolescence. Mol Psychiatry. 2014;19(1):63–8. https://doi.org/10.1038/mp.2012.179.
Vogel H, Kraemer M, Rabasa C, Askevik K, Adan RAH, Dickson SL. Genetic predisposition to obesity affects behavioural traits including food reward and anxiety-like behaviour in rats. Behav Brain Res. 2017;328:95–104. https://doi.org/10.1016/j.bbr.2017.02.037.
Velazquez-Sanchez C, Ferragud A, Moore CF, Everitt BJ, Sabino V, Cottone P. High trait impulsivity predicts food addiction-like behavior in the rat. Neuropsychopharmacology. 2014;39(10):2463–72. https://doi.org/10.1038/npp.2014.98.
Pivarunas B, Conner BT. Impulsivity and emotion dysregulation as predictors of food addiction. Eat Behav. 2015;19:9–14. https://doi.org/10.1016/j.eatbeh.2015.06.007.
Zeeni N, Bassil M, Fromentin G, Chaumontet C, Darcel N, Tome D, et al. Environmental enrichment and cafeteria diet attenuate the response to chronic variable stress in rats. Physiol Behav. 2015;139:41–9. https://doi.org/10.1016/j.physbeh.2014.11.003.
Martire SI, Westbrook RF, Morris MJ. Effects of long-term cycling between palatable cafeteria diet and regular chow on intake, eating patterns, and response to saccharin and sucrose. Physiol Behav. 2015;139:80–8. https://doi.org/10.1016/j.physbeh.2014.11.006.
Baker KD, Reichelt AC. Impaired fear extinction retention and increased anxiety-like behaviours induced by limited daily access to a high-fat/high-sugar diet in male rats: implications for diet-induced prefrontal cortex dysregulation. Neurobiol Learn Mem. 2016;136:127–38. https://doi.org/10.1016/j.nlm.2016.10.002.
McNeilly AD, Stewart CA, Sutherland C, Balfour DJK. High fat feeding is associated with stimulation of the hypothalamic-pituitary-adrenal axis and reduced anxiety in the rat. Psychoneuroendocrinology. 2015;52:272–80. https://doi.org/10.1016/j.psyneuen.2014.12.002.
Dutheil S, Ota KT, Wohleb ES, Rasmussen K, Duman RS. High-fat diet induced anxiety and anhedonia: impact on brain homeostasis and inflammation. Neuropsychopharmacology. 2016;41(7):1874–87. https://doi.org/10.1038/npp.2015.357.
da Costa ED, da Silva WAM, Guimarães ATB, de Oliveira MB, da Silva Castro AL, da Silva Torres IL, et al. Predictive behaviors for anxiety and depression in female Wistar rats subjected to cafeteria diet and stress. Physiol Behav. 2015;151:252–63. https://doi.org/10.1016/j.physbeh.2015.07.016.
Velázquez-Sánchez C, Santos JW, Smith KL, Ferragud A, Sabino V, Cottone P. Seeking behavior, place conditioning and resistance to conditioned suppression of feeding in rats intermittently exposed to palatable food. Behav Neurosci. 2015;129(2):219–24. https://doi.org/10.1037/bne0000042.
•• Sirohi S, Van Cleef A, Davis JF. Patterned feeding induces neuroendocrine, behavioral and genetic changes that promote palatable food intake. Int J Obes. 2017;41(3):412–9. https://doi.org/10.1038/ijo.2016.235. This paper models human patterns of dieting in rodents, showing that patterned feeding results in neuroendocrine, behavioural and genetic changes that may promote subsequent hyperphagia.
Pool E, Brosch T, Delplanque S, Sander D. Stress increases cue-triggered “wanting” for sweet reward in humans. J Exp Psychol Anim Learn Cogn. 2015;41(2):128–36. https://doi.org/10.1037/xan0000052.
Richardson AS, Arsenault JE, Cates SC, Muth MK. Perceived stress, unhealthy eating behaviors, and severe obesity in low-income women. Nutr J. 2015;14(1):122. https://doi.org/10.1186/s12937-015-0110-4.
Järvelä-Reijonen E, Karhunen L, Sairanen E, Rantala S, Laitinen J, Puttonen S, et al. High perceived stress is associated with unfavorable eating behavior in overweight and obese Finns of working age. Appetite. 2016;103:249–58. https://doi.org/10.1016/j.appet.2016.04.023.
Boggiano MM, Wenger LE, Turan B, Tatum MM, Morgan PR, Sylvester MD. Eating tasty food to cope. Longitudinal association with BMI. Appetite. 2015;87:365–70. https://doi.org/10.1016/j.appet.2015.01.008.
Reichenberger J, Kuppens P, Liedlgruber M, Wilhelm FH, Tiefengrabner M, Ginzinger S, et al. No haste, more taste: an EMA study of the effects of stress, negative and positive emotions on eating behavior. Biol Psychol. 2016;131:54–62. https://doi.org/10.1016/j.biopsycho.2016.09.002.
Tan CC, Chow CM. Stress and emotional eating: the mediating role of eating dysregulation. Personal Individ Differ. 2014;66:1–4. https://doi.org/10.1016/j.paid.2014.02.033.
• MacKay JC, Kent P, James JS, Cayer C, Merali Z. Ability of palatable food consumption to buffer against the short- and long-term behavioral consequences of social defeat exposure during juvenility in rats. Physiol Behav. 2017;177:113–21. https://doi.org/10.1016/j.physbeh.2017.04.002. This paper explores the concept of ‘comfort eating’ as a buffer against stress. Exposure to palatable food attenuates stress responding in adult rats exposed to juvenile social defeat.
Handy C, Yanaga S, Reiss A, Zona N, Robinson E, Saxton KB. Stress during adolescence alters palatable food consumption in a context-dependent manner. PLoS One. 2016;11(2):e0148261. https://doi.org/10.1371/journal.pone.0148261.
Maniam J, Antoniadis CP, Le V, Morris MJ. A diet high in fat and sugar reverses anxiety-like behaviour induced by limited nesting in male rats: impacts on hippocampal markers. Psychoneuroendocrinology. 2016;68:202–9. https://doi.org/10.1016/j.psyneuen.2016.03.007.
Yam KY, Naninck EFG, Abbink MR, la Fleur SE, Schipper L, van den Beukel JC, et al. Exposure to chronic early-life stress lastingly alters the adipose tissue, the leptin system and changes the vulnerability to western-style diet later in life in mice. Psychoneuroendocrinology. 2017;77:186–95. https://doi.org/10.1016/j.psyneuen.2016.12.012.
Finch LE, Tomiyama AJ. Comfort eating, psychological stress, and depressive symptoms in young adult women. Appetite. 2015;95:239–44. https://doi.org/10.1016/j.appet.2015.07.017.
Michopoulos V, Powers A, Moore C, Villarreal S, Ressler KJ, Bradley B. The mediating role of emotion dysregulation and depression on the relationship between childhood trauma exposure and emotional eating. Appetite. 2015;91:129–36. https://doi.org/10.1016/j.appet.2015.03.036.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sarah-Jane Leigh, Frances Lee and Margaret J. Morris declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
Where studies performed by the authors are included, appropriate institutional animal ethics approval was obtained and details are provided in the cited source.
Additional information
This article is part of the Topical Collection on Etiology of Obesity
Rights and permissions
About this article
Cite this article
Leigh, SJ., Lee, F. & Morris, M.J. Hyperpalatability and the Generation of Obesity: Roles of Environment, Stress Exposure and Individual Difference. Curr Obes Rep 7, 6–18 (2018). https://doi.org/10.1007/s13679-018-0292-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13679-018-0292-0