Abstract
Many studies worldwide confirm that antibiotic use is common in long-term care facilities (LTCFs). Some of that antibiotic use is inappropriate and may contribute to the emergence of antibiotic resistance. Inappropriate use may be characterized as antibiotic treatment of clinical syndromes that are not infectious, infectious conditions that do not respond to antibiotics, and prolonged duration. Additionally, better antibiotic choices should have been made or insufficient clinical evidence was present to start an antibiotic. National and international action plans are under development to curtail unnecessary antibiotic use throughout the healthcare continuum including LTCF. While the optimal strategies to curtail antibiotic use in LTCF have not been defined, there are a number of approaches that can help nursing homes monitor their antibiotic usage, recognize problem areas, and develop and implement quality improvement initiatives.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Antibiotic Use in LTCF
Antibiotic use is common in facilities that provide chronic or long-term care for older adults. While appropriate antibiotic use can be beneficial and cure or control infection, unnecessary antibiotic use may lead to adverse drug events and the emergence of antibiotic resistance. While the nomenclature may vary from country to country, this paper reviews the state of antibiotic use in long-term care facilities (LTCFs), e.g., skilled nursing homes or residential facilities that provide its residents onsite evaluation and treatment for infection.
The significance of antibiotic use in LTCF has been under discussion for almost three decades; it has been stated that 40 % of all systemic drugs used in nursing homes are antibiotics [1–5]. In addition, it has been estimated that 6–10 % of LTCF residents or in the USA and Canada and 11–13 % of residents in Europe will receive an antibiotic accounting for four to seven courses per 1000-resident-days, and 2–4 million antibiotic courses per year [5–16]. Of the 47–79 % of residents who receive at least one antibiotic during a 1-year stay, one third to one half of those residents will end up receiving additional courses [5, 6, 8, 14–17].
While complexity of care, e.g., post-acute care, rehabilitation, and spinal cord injury, correlates with increased antibiotic use when compared with behavioral and functional treatment categories, variability in infection rates and case-mix in LTCF only account for 50 and 66 % of respective differences in antibiotic use [7, 18]. Prescriber preferences may be more important predictors of antibiotic use than patient care characteristics. In one study, 20 % of high-use prescribers accounted for 80 % of antibiotic use. When adjusted for patient characteristics, residents were fourfold more likely to get an antibiotic if a high-use prescriber was caring for them when compared with a low-use prescriber [17].
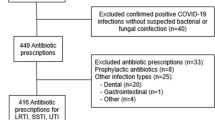
Infections of the urinary tract (UTI), respiratory tract (RTI), and skin and soft tissues (SSTI) are primarily cited as the most common reasons that antibiotics are prescribed in LTCF and residential homes [8, 15, 19]. However, not all prescribers document a rationale for antibiotic use, nor do billing codes reflect a diagnosis of infection [1, 17]. It has been estimated that 25–75 % of antibiotics are used inappropriately in LTCF [1–3, 5, 6, 20].
What Is Unnecessary or Inappropriate Antibiotic Use in LTCF?
While there is little doubt that nursing home residents receive too many antibiotics, the definition of what constitutes “unnecessary or inappropriate” antibiotic use varies from study to study. Unjustified antibiotics have been classified as prescribed for a condition that was not infectious, for which the drugs would not be of benefit, e.g., asymptomatic bacteriuria, urine prophylaxis, viral upper respiratory infection, and advanced dementia-end of life care, or continuation of treatment for an organism to which the antibiotic was not susceptible [2, 3, 6, 14, 21–24, 25]. Others found that antibiotic use was inappropriate as better drug choices, e.g., less expensive, toxic, and more efficacious, could have been made, the duration of treatment was too long, antibiotic dosing was too high or too low, or more antibiotics were prescribed than were required to treat an organism identified by culture [2, 10, 13, 23].
Still, others have defined inappropriate antibiotic use as failure to document minimum criteria for the diagnosis of infection such as symptoms, vital signs, and focal physical findings that were obtained prior to, or shortly after, the decision to initiate antibiotic treatment [1, 6, 20, 25]. Inappropriate antibiotic use has also been characterized as failure to obtain laboratory testing to help verify or exclude the diagnosis of UTI (urinalysis/leukocyte esterase and culture of urine and antibiotic susceptibilities) or pneumonia (chest radiograph) [1, 6, 20, 25]. Meeting minimum criteria for the initiation of an antibiotic varies widely for the most common diagnoses, e.g., UTI (30 %), RTI (33–80 %), and SSTI (70 %) [7, 26, 27]. Treatment of asymptomatic bacteriuria has frequently led to the prescription of nitrofurantoin, a drug that is not recommended per the Beers Criteria, and urine antiseptics [9, 14, 15, 28].
Initiatives to Improve Antibiotic Use
Over the past 30 years, the Infectious Diseases Society of America (IDSA) has provided guidelines to improve the use, selection, dosing, route, and duration of antibiotics [29]. Only recently have national and world leaders recognized the impact that inappropriate antibiotic use and antibiotic resistance has had on our society [30]. Antibiotic side effects and superinfections with resistant bacteria and Clostridium difficile result in significant mortality for patients and costs to the healthcare system. Many antibiotic-resistant infections cannot be treated with the antibiotics that are currently available, and too few new drugs are being developed that fight these infections.
Formal programs, termed antimicrobial stewardship (AS) programs, have been developed to improve infection outcomes while minimizing antibiotic use, the emergence of resistance, and costs and preventing adverse drug events. Antimicrobial stewardship is defined as “coordinated interventions designed to improve and measure the appropriate use of antimicrobial agents by promoting the selection of the optimal drug regimen including dosing, duration of therapy, and route of administration” [31]. Guidelines for the development of AS programs have been developed primarily based on experiences in hospitals and evidence obtained in intensive care units [29].
In 2007, the IDSA guidelines acknowledged that these recommendations were based on experience in adults in acute care hospitals, and evidence for the utility in LTCF was limited (29). Five years later, the IDSA, Society for Healthcare Epidemiology (SHEA), and Pediatric Infectious Diseases Society (PIDS) recommended that all healthcare institutions across the continuum of care provide resources for AS programs [31]. Each healthcare facility would be required to have a multidisciplinary AS program team, antimicrobial formulary, processes to measure and monitor antimicrobial use, distribution of a facility-specific antibiogram, and report to the National Healthcare Safety Network; national benchmarks would be developed. In response, the Centers for Medicare and Medicaid Services (CMS) has recently submitted a major rewrite of long-term care conditions of participation for public comment that includes a requirement for an AS program, antibiotic use protocols, and a system to monitor antibiotic use [32]. Similarly, national performance indicators for the implementation of antimicrobial stewardship have been developed for 32 countries in Europe, e.g., Healthcare-Associated infections in Long-Term care facilities (HALT) Project [33].
ASP in Hospitals: What Is Has Been Done?
The IDSA 2007 Guidelines recommended a prospective or “front end” AS program approach that was evidence-based and resource intensive, supported by the hospital administration, and that included an infectious diseases physician or pharmacist with infectious diseases training, and input by a clinical microbiologist [29]. The two core strategies of this front-end approach included (1) formulary restriction and antibiotic preauthorization by infectious diseases physicians and/or pharmacists and (2) prospective interventions and immediate feedback to prescribers [25, 29]. These approaches have shown significant impact on reducing antibiotic use, costs, and potentially antibiotic resistance in hospitals. Supplemental approaches include education, use of guidelines and clinical pathways in addition to de-escalation of antibiotics based on culture results, dosage adjustment, and transition from intravenous to oral therapy. Electronic health records and computer surveillance/microbiology input to support antimicrobial decision-making are viewed as potentially important.
AS Programs in LTCF: Current Status and What Is Proposed?
In 2015, the Centers for Disease Control and Prevention (CDC) made recommendations about how AS programs could be developed for LTCF [34••] (Table 1). The core elements are the same as for the 2014 CDC recommendations for AS programs in hospitals [35]. There has been limited feedback obtained from LTCF about their ability to implement AS programs in the near future [25, 36–42]. In Nebraska, 37 of 230 (16.1 %) facilities completed a survey about AS programs; 22 of 37 (59.5 %) reported having a formal program [37]. In Ireland, 11 of 69 (16 %) LTCF surveyed had an AS committee, and 19/69 (28 %) had AS guidelines [38]. In Europe, 50 % of LTCF have not had access to nursing home-specific guidelines for antimicrobial use [16].
Some LTCF have indicated that they have an antibiotic use monitor (59–81 %) as part of their infection control program, although the definition of AS program was not clear [36, 37, 39]. Most facilities (89 %) have viewed an antibiotic use program as beneficial; 54 % reported antibiotic overuse, but 64 % have noted that their current program was somewhat or not effective [36, 37]. Barriers to improving antibiotic use have included prescriber preference and autonomy (69 %) and family/patient expectations (15 %) [37, 38, 42, 43•, 44]. From the prescriber perspective, there has been a great deal of pressure from the institution from a medicolegal perspective, nursing staff, and families to prescribe antibiotics and order urine specimens [39, 41, 44]. From both the nursing and physician perspective, early ordering of antibiotic was preferred because the prescribers and sometimes the pharmacy are offsite and not necessarily available at all hours [39, 41, 44].
Few facilities have required antibiotic preauthorization by infectious diseases-trained physicians or pharmacists (11–12 %), had ready access to a pharmacist for advice (36–50 %), monitored antibiotic use practices by prescribers (7–11 %), or have given feedback to staff physicians (10–33 %) [36–38]. While some homes have had access to an antibiogram (76 %), few have had an antibiotic formulary (19–23 %) [16, 37]. Most facilities have identified a single individual, typically the infection preventionist, as their antibiotic “champion” rather than having the recommended multidisciplinary team approach [37]; this individual has had fewer than 5 h per week to devote to the activity, and many (72–84 %) have not had an electronic method to collect antibiotic data [36, 45].
Most healthcare providers have agreed that more education regarding treatment of infection would be helpful. Assessment of the appropriate evaluation and treatment of common infections has shown that LTCF staff knowledge needs to be improved [42, 44, 46]. Provision of guidelines or diagnostic algorithms for common infectious conditions in LTCF and their treatments have been viewed as valuable by prescribers, but only 28 % of facilities provide this guidance (27–28 %) [37–39, 42]. Provision of education to nursing regarding the appropriate and inappropriate use of antibiotics has been recommended to help physicians identify conditions that need treatment, versus those that do not, and to help counsel families and patients about reducing unnecessary antibiotic use [39, 42, 44]. Some potential targets for education include areas where antibiotic use should be discouraged such as prophylaxis for UTIs, asymptomatic bacteriuria, upper RTI that is commonly viral, prolonged antibiotic treatment greater than 7 days, and use of intravenous antibiotics in patients with advanced dementia [40, 43•].
AS Programs in LTCF: What Approaches Have Been Studied?
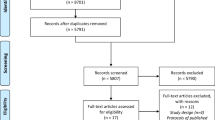
There have been approximately a dozen published trials of AS interventions in LTCF published to date, and four were historical-controlled single center studies [47–52]. Of seven multicenter trials, five were cluster-randomized [53–57] and 2 were quasi-experimental study designs [58, 59]. There are several recent reviews that analyze the strengths and weaknesses of these interventions that have been implemented to reduce unnecessary antibiotic use in long-term care [60–64].
Few AS interventions have focused on front-end approaches that have been cited as the primary reason for success in hospitals. Jump et al. initiated an Infectious Diseases Consultation Service at a single Veterans Affairs LTCF. Significant reductions in systemic antibiotic use (30 %), including oral (32 %) and intravenous (25 %) therapies, were seen over an 18-month intervention period in addition to significant reductions in positive testing for C. difficile [48, 49].
Back-end approaches to reduce overall antibiotic use in LTCF have been studied more often [47, 50, 51, 54, 57]. Most interventions involved various educational modalities with the provision of algorithms and guidelines followed by retrospective audits for appropriate antibiotic use [47, 54, 58]. Schwartz studied infection management at a single LTCF versus published guidelines [47]. Expert consultants provided interactive case discussions, algorithms, and guidelines. Empiric quinolone use and inappropriate antibiotic use directed against asymptomatic bacteriuria and treatment of isolated production of respiratory secretions were targeted by retrospective audit. A significant increase in adherence with guideline diagnostic criteria and therapy was seen as well as sustained reduction in antibiotic-use days was seen during the post intervention period [47]. In six LTCFs, an intervention by Zimmerman et al. consisted of interactive sessions and training for prescribers and nurses regarding antibiotic guidelines and when antibiotics should not be used versus usual care. Feedback was provided monthly to LTCF staff [58]. A statistically non-significant reduction in antibiotic use was seen for the intervention homes, but they estimate that 1.8 antibiotic prescriptions were avoided per 1000-resident-days. In an intervention by Monette et al., intervention physicians received their antibiotic prescribing profile along with antibiotic guidance on two occasions over 4 months versus physicians who provided usual care. Non-adherence with the guide declined in the intervention group (20.5 %) versus the control group (5.1 %) [54].
Other studies have used various tools to help reinforce appropriate use of antibiotics. Fleet et al. developed a checklist that was implemented by nurses that detailed patient signs/symptoms, physician examination, suspected site of infection, diagnostic evaluation, with clinical response, and antibiotic initiation and stop dates. These checklists were compared with the revised McGeer Criteria to see of infection was present and Loeb Minimum Criteria for the initiation of antibiotics. Retrospective audit of treatment decisions was performed within 48–72 h. A significant reduction in overall antibiotic consumption was seen during the pilot study period [27, 57, 65].
Similarly, Pate et al. used retrospective chart audit in combination with leaving non-binding recommendations as part of the patient medical record at a single long-term acute care hospital (LTACH) [50]. Recommendations included stopping one or more antibiotics (25 %), modify the agent or duration (30 %), or obtain consultation with infectious diseases about those issues (21 %). Choice of antibiotic, duration, allergies, potential drug interactions, and diagnostic testing were audited. Recommendations were followed-up with prescribers 72 h later. Most recommendations were accepted (80 %) with a significant reduction in monthly antibiotic use (21 %) and 28 % in monthly cost during the 15-month study period. Significant reductions in antibiotic use were seen following the intervention.
Furuno et al. developed algorithms for empiric antibiotic choices for each clinical syndrome along with dosage adjustments and duration. Antibiograms based on 6 months of culture data were developed for three LTCFs, in-services were given, and a pocket-sized copy was given to each prescriber. Prior to implementation, only 15 % of antibiotic choices were based on culture data [51]. After implementation in one nursing home, a non-significant increase in the appropriate use of antibiotics changed from a baseline of 35 to 45 % [51].
Some intervention studies have specifically focused on one clinical syndrome such as nursing home-acquired pneumonia (NHAP) and UTI. Studies of the improvement of NHAP treatment have focused upon multi-modal interventions to improve immunization rates [59, 66], education of nursing leadership and nurse champions about NHAP guidelines for diagnosis and treatment [66], preprinted order [59, 66], interactive prescriber education [53, 59, 66], and the use of reference cards [53, 59, 66]. Education led to improved immunization rates [66], recognition and more rapid initiation of antibiotics in intervention homes [59, 66], increased chest radiograph use [59, 66], and more appropriate antibiotic use [66] in intervention versus control LTCF. Nursing leaders and champions were educated about the recognition of pneumonia to help remind prescribers about immunizations and diagnostic and treatment guidelines. No significant impact on route of administration [53], and hospitalization [53, 66] and mortality [53, 59, 66] rates was seen.
Other interventions have focused on antibiotic use initiated in response to positive urine cultures. Presence of symptoms and signs that are not specific for UTI appears to be a major driver to obtain urinalyses and urine cultures and to order antibiotics in the absence of evidence to support these practices [67]. In one retrospective study, 41 % of patients with bacteriuria did not meet McGeer Criteria for UTI; 72 % of antibiotics chosen were inappropriate, and those patients were 8.5-fold more likely to develop C. difficile infection [68]. Similarly, 74 % of patients with advanced dementia who did not meet Loeb Minimum Criteria for the initiation of an antibiotic received treatment [69].
For antibiotic use for presumed UTI, similar interventions using education and retrospective feedback have been employed. Zabarsky et al. recognized that 61 % of antibiotic use was for asymptomatic bacteriuria [52]. Initial and semi-annual follow-up educational interventions were focused on prescribers and nursing staff, and reference cards were provided. Significant and sustained reductions in urine culture requests, particularly for cloudy and smelly urine, and treatment were seen over the 30-month study. Petterson et al. used an educational intervention to reduce quinolone usage for presumed UTI [56]. Focus groups, guidelines for prescribing, and handouts were provided to prescribers, nurses, and nurses aides. Feedback on baseline results, local patterns of resistance, and discussion of barriers to change were given. No significant difference in quinolone use was seen between intervention and control LTCF. However, physicians who received the intervention were significantly less likely to prescribe antibiotics over all and adopt a wait-and-see approach. No significant differences in hospitalizations were seen.
Other interventions for antibiotic use and UTI have focused on the use of algorithms. Rummukainen et al. developed a diagnostic algorithm based on the recognition that most antibiotics were used for UTI and 13 % for prophylaxis. Urine odor was a significant driver of urine dipstick acquisition [70]. Antibiotic use was reported on an annual basis with significant reduction in prophylactic antibiotic use. In a cluster randomized control trial, an algorithm for diagnosis and treatment of suspected UTI was based on the Loeb Minimum Criteria to initiate antibiotics. Significantly, fewer antibiotics were started for suspected UTI in intervention versus usual care LTCF without significant differences in hospitalizations for infection and mortality rates. However, overall antibiotic use did not decrease suggesting that the treatment was deferred to other suspected diagnoses [27, 55].
AS Programs in LTCF: Potential Barriers to Implementation?
The CDC recommends a number of elements to be included in a LTCF AS program (Table 1). Of the six elements of the AS program, there is some evidence based on the previously mentioned studies that some aspects of Leadership Commitment [56, 66], Accountability [50, 51, 54], Drug Expertise [49, 50, 70], Policy Practice Change [47, 50, 51, 56–59, 66, 69, 70], Tracking/Reporting [47, 49, 51–54, 56–59, 69, 70], and Education [47, 52–54, 56, 58, 59, 66, 70] can be accomplished, yield useful information, and potentially improve outcomes in the long-term care setting. Whether these interventions are feasible and sustainable in the typically LTCF that does not have access to research expertise and its resources remains to be seen [61]. Based on the current evidence, no specific intervention strategy can be recommended at this time [64]. No estimates have been provided regarding the cost effectiveness of these strategies or their impact on antibiotic resistance [60, 63].
There are several of other important barriers to the implementation of an AS program in LTCF going forward. Tracking and reporting of antibiotic use is limited by the lack of electronic medical records in many LTCFs [34••]. Per the CDC, only 19 % of residential care communities had access to an electronic medical record as of 2014 [45]. The SHEA 2012 Policy Statement specifically called for the expanded utilization of electronic medical records in ambulatory care settings, but no mention was made of nursing homes [31].
Infection preventionists in LTCF most typically have a nursing degree, but medical technicians and social workers may also be trained to perform infection surveillance. The infection preventionist does record signs and symptoms of possible infection as part of normal surveillance activities that could be used to discern whether there was sufficient evidence to initiate an antibiotic and meet the Loeb Minimum Criteria [27]. However, the final decision whether the choice or duration of an antibiotic was appropriate or not is beyond the scope of practice of the infection preventionist; this function would be more appropriately performed by someone trained in the diagnosis and treatment of infection [34••]. In addition, the Loeb Minimum Criteria can only be helpful if resident signs and symptoms are accurately and completely recorded in the medical record [27]. Ultimately, it is likely that this task will fall to the medical director or their designee and the facility pharmacist to determine whether antibiotic use criteria are met or not.
Finally, drug expertise remains a major barrier for meeting criteria for an AS program in LTCF [34••]. Drug expertise implies that all LTCF will have ready access to consultants, either physicians or pharmacists, with very specific training in infectious diseases and AS. In 2016, the proactive front-end AS approach used in hospitals where infectious diseases physicians or pharmacists would be available to provide immediate feedback about the appropriate use of an antibiotic on a case-by-case basis remains an unlikely approach in the LTCF [25]. As of 2013, there were 15,000 nursing homes in the USA encompassing 1.7 million beds [71]. In the USA, there are ~7000 active infectious diseases physicians; many are not involved in ASPs, and the vast majority have not worked in long-term care settings [72]. Similarly, all pharmacists are not necessarily trained in issues related to AS or infectious diseases. The American College of Clinical Pharmacy and the Society of Infectious Diseases Pharmacists have recommended that pharmacists should complete a 2-year residency in Infectious Diseases and become board certified in pharmacotherapy; a certification examination in infectious diseases should be developed [73]. So, it is not clear that all LTCF will have access to AS expertise if it is required in its current form.
Conclusions
Inappropriate antibiotic use in healthcare settings is all too frequent, and LTCFs are no exception. Governmental programs mandating quality improvement initiatives in the LTCF are coming. LTCF can begin to prepare for these changes by beginning to develop a process to record and track antibiotic use and the indications for that use at regular intervals. Education of leadership about appropriate versus antibiotic indications, choices, and duration will be critical to understand where improvements in antibiotic use could be made.
LTCF can begin to develop a credible AS program as part of their existing Infection Control Committee structure by assembling a multidisciplinary team including the medical and nursing directors, infection preventionist, facility pharmacist, and with input from the clinical microbiology laboratory. AS program quality improvement projects do not have to be complicated. The AS Committee should define one or two areas where inappropriate antibiotic use is a problem; failure to de-escalate antibiotic use based on culture results, prolonged antibiotic duration, or elimination of antibiotic use for UTI prophylaxis, URI, and asymptomatic bacteriuria are common targets to consider. Ultimately, we will have a better idea of what interventions are effective and what are not. Tracking antibiotic use and other outcomes of interest before and after will be important to assess the impact of an intervention. In addition, having reliable methods to provide feedback to staff, residents, and families on a regular basis will be needed.
There are a number of algorithms, guidelines, checklists, pre-printed order forms, antibiograms, and other tools that may be useful and modifiable to the situation in each LTCF.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Zimmer JG, Bentley DW, Valenti WM, Watson NM. Systemic antibiotic use in nursing homes: a quality assessment. J Am Geriatr Soc. 1986;34(10):703–10.
Jones SR, Parker DF, Liebow ES, Kimbrough RC, Frear RS. Appropriateness of antibiotic therapy in long-term care facilities. Am J Med. 1987;83(9):499–502.
Katz PR, Beam TR, Brand F, Boyce K. Antibiotic use in the nursing home: physician practice patterns. Arch Intern Med. 1990;150(7):1465–8.
Mylotte JM. Measuring antibiotic use in a long-term care facility. Am J Infect Control. 1996;24(3):174–9.
Nicolle LE, Bentley DW, Garibaldi R, Neuhaus EG, Smith PW, Society for Healthcare Epidemiology of America Long Term-Care Committee. Antimicrobial use in long-term–care facilities. Infect Control Hosp Epidemiol 2000;21(8):537-545.
Warren JW, Palumbo FB, Fitterman L, Speedie SM. Incidence and characteristics of antibiotic use in aged nursing home patients. J Am Geriatr Soc. 1991;39(10):963–72.
Benoit SR, Nsa W, Richards CL, Bratzler DW, Shefer AM, Steele LM, et al. Factors associated with antimicrobial use in nursing homes: a multilevel model. J Am Geriatr Soc. 2008;56(11):2039–44.
Loeb M, Simor AE, Landry L, Walter S, McArthur M, Duffy J, et al. Antibiotic use in Ontario facilities that provide chronic care. J Gen Intern Med. 2001;16(6):376–83.
Blix HS, Roed J, Sti MO. Large variation in antibacterial use among Norwegian nursing homes. Scand J Infect Dis. 2007;39(6-7):536–41.
Boivin Y, Talon D, Leroy J, Floret N, Gbaguidi-Haore H, Bertrand X. Antibiotic prescription in nursing homes for dependent elderly people: a cross-sectional study in Franche-Comté. Med Mal Infect. 2013;43(4):163–9.
Heudorf U, Boehicke K, Schade M. Healthcare-associated infections in long-term care facilities (HALT) in Frankfurt am Main, Germany, January to March 2011. Euro Surveill. 2012;17(35).
McClean P, Hughes C, Tunney M, Goossens H, Jans B. Antimicrobial prescribing in European nursing homes. J Antimicrob Chemother. 2011;66(7):1609–16.
Daneman N, Gruneir A, Newman A, Fischer HD, Bronskill SE, Rochon PA, et al. Antibiotic use in long-term care facilities. J Antimicrob Chemother. 2011;66(7):2856–63.
Rummukainen ML, Karki T, Kanerva M, Haappasaari M, Ollgren J, Lyytikainen O. Antimicrobial prescribing in nursing homes in Finland: results of three point prevalence surveys. Infection. 2013;41(2):355–60.
Pakyz AL, Dwyer LL. Prevalence of antimicrobial use among United States nursing home residents: results from a national survey. Infect Control Hosp Epidemiol. 2010;31(6):661–2.
van Buul LW, van der Steen Jenny T, Veenhuizen RB, Achterberg WP, Schellvis FG, Essink RTGM, et al. Antibiotic use and resistance in long term-care facilities. J Am Med Dir Assoc. 2012;13(6):568e1–568e13. Recent overview of the state of antibiotic use and antibiotic resistance in LTCF.
Mylotte JM. Trends in antibiotic use and cost and influence of case-mix and infection rate on antibiotic-prescribing in a long-term care facility. Am J Infect Control. 2003;31(2):18–25.
Daneman N, Gruneir A, Bronskill SE, Newman A, Fischer HD, Rochon PA, et al. Prolonged antibiotic treatment in long-term care: role of the prescriber. JAMA Intern Med. 2013;173(8):673–82.
McClean P, Tunney M, Gilpin D, Parsons C, Hughes C. Antimicrobial prescribing in residential homes. J Antimicrob Chemother. 2012;67(7):1781–90.
Loeb M. Antibiotic use in long-term-care facilities: many unanswered questions. Infect Control Hosp Epidemiol. 2000;21(10):680–3.
D’Agata E, Mitchell SL. Patterns of antimicrobial use among nursing home residents with advanced dementia. Arch Intern Med. 2008;168(4):357–62.
Stuart RL, Wilson J, Bellaard-Smith E, Brown R, Wright L, Vandergraaf S, et al. Antibiotic use and misuse in residential aged care facilities. Intern Med J. 2012;42(10):1145–9.
Peron EP, Hirsch AA, Jury LA, Jump RLP. Another setting for stewardship: high rate of unnecessary antimicrobial use in a veterans affairs long-term care facility. J Am Geriatr Soc. 2013;61(2):289–314.
Suetens C. Healthcare-associated infections in European long-term care facilities: how big is the challenge?. Euro Surveill 2012;17(35).
Smith PW, Watkins K, Miller H, VanSchooneveld T. Antibiotic stewardship programs in long-term care facilities. Ann Long-Term Care. 2011;19(4):20–5. An excellent review of the strategies that LTCF could use to develop antimicrobial stewardship programs.
Montgomery P, Semenchuk M, Nicolle LE. Antimicrobial use in nursing homes in Manitoba. J Geriatr Drug Ther. 1995;9:55–74.
Loeb M, Bentley DW, Bradley S, Crossley K, Garibaldi R, Gantz N, et al. Development of minimum criteria for the initiation of antibiotics in residents of long-term-care facilities: results of a consensus conference. Infect Control Hosp Epidemiol. 2001;22(2):120–4.
Budnitz DS, Shehab N, Kegler SR, et al. Medication use leading to emergency department visits for adverse drug events in older adults. Ann Intern Med. 2007;147:755–65.
Dellit TH, Owens RC, McGowan Jr JE, Gerding DH, Weinstein RA, Burke JP, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–77. This guideline was the genesis for the antimicrobial stewardship movement in hospitals in the United States and its national action plan.
National action plan for combatting antibiotic-resistant bacteria. https://www.whitehouse.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf.
Society for Healthcare Epidemiology of America, Infectious Diseases Society of America, Pediatric Infectious Diseases Society. Policy statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society of America (PIDS). Infect Control Hosp Epidemiol. 2012;33(4):322–7.
HHS proposes to improve care and safety for nursing home residents. http://www.hhs.gov/about/news/2015/07/13/hhs-proposes-to-improve-care-and-safety-for-nursing-home-residents.html.
Cookson B, Mackenzie D, Kafatos G, Jans B, Latour K, Moro ML, et al. Development and assessment of national performance indicators for infection prevention and control and antimicrobial stewardship in European long-term care facilities. J Hosp Infection. 2013;85(1):45–53.
Centers for Disease Control and Prevention. The core elements of antibiotic stewardship for nursing homes. Atlanta, GA: US Department of Health and Human Services, CDC, 2015. Available at: http://www.cdc.gov/longtermcare/index.html. This website outlines the core elements recommended for LTCF antimicrobial stewardship programs.
Centers for Disease Control and Prevention. Core elements of hospital antibiotic stewardship programs. Atlanta, GA: US Department of Health and Human Services, CDC, 2014. Available at: www.cdc.gov/getsmart/healthcare/implementation/core-elements.html.
O’Fallon E, Harper J, Shaw S, Lynfield R. Antibiotic and infection tracking in Minnesota long-term care facilities. J Am Geriatr Soc. 2007;55(8):1243–7.
Van Schooneveld T, Miller H, Sayles H, Watkins K, Smith PW. Survey of antimicrobial stewardship practices in Nebraska long-term care facilities. Infect Control Hosp Epidemiol. 2011;32(7):732–4.
Donlan S, Roche F, Byrne H, Dowling S, Cotter M, Fitzpatrick F. A national survey of infection control and antimicrobial stewardship structures in Irish long-term care facilities. Am J Infect Control. 2013;41(6):554–7.
Gahr P, Kieke B, Como-Sabetti K, Christianson RC, Williams D, Pederson J, et al. Healthcare professional surveys: judicious antibiotic use in Minnesota long-term care facilities. Infect Control Hosp Epidemiol. 2007;55(3):473–4.
Lim CJ, Kong DC, Stuart RL. Reducing inappropriate antibiotic prescribing in the residential care setting: current perspectives. Clin Interv Aging. 2014;9:165–77.
Lim CJ, Kwang M, Stuart RL, Buising KL, Friedman ND, Bennett N, et al. Antibiotic prescribing practice in residential aged care facilities—health care providers’ perspectives. Med J Austral. 2014;201(2):101–5.
Lim CJ, Kwang M, Stuart RL, Buising KL, Friedman ND, Bennett N, et al. Antimicrobial stewardship in residential aged care facilities: need and readiness assessment. BMC Infect Dis. 2014;14(7):410.
Dyar OJ, Pagani L, Pulcini C. Strategies and challenges of antimicrobial stewardship in long-term care facilities. Clin Microbiol Infect. 2015;21(1):10–9. An excellent review of the strengths and limitations of recent studies done related to antimicrobial stewardship in LTCF.
Fleming A, Bradley C, Cullinan S, Byrne S. Antibiotic prescribing in long-term care facilities: a qualitative, multidisciplinary investigation. BMJ Open. 2014;4(11):e006442e1–e006442e13.
Centers for Disease Control and Prevention. Percentage of residential care communities using electronic health records, by the number of beds—national study of long-term care providers, United States, 2014. MMWR. 2015;64(41):1181.
Jump RLP, Heath B, Crnich CJ, Moehring R, Schmader KE, Olds D, et al. Knowledge, beliefs, and confidence regarding infections and antimicrobial stewardship: a survey of Veterans Affairs providers who care for older adults. Am J Infect Control. 2015;43(3):298–300.
Schwartz DN, Abiad H, DeMarais PL, Armeanu E, Trick WE, Wang Y, et al. An educational intervention to improve antimicrobial use in a hospital-based long-term care facility. J Am Geriatr Soc. 2007;55(8):1236–42.
Jump RL, Olds DM, Jury LA, Sitzlar B, Saade E, Watts B, et al. Specialty care delivery: bringing infectious disease expertise to the residents of a Veterans Affairs long-term care facility. J Am Geriatr Soc. 2013;61(5):782–7.
Jump RLP, Olds DM, Seifi N, Kypriotakis G, Jury LA, Peron EP, et al. Effective antimicrobial stewardship in a long-term care facility through an infectious diseases consultation service: keeping a LID on antibiotic use. Infect Control Hosp Epidemiol. 2012;33(12):1185–92.
Pate PG, Storey DE, Baum DL. Implementation of an antimicrobial stewardship program at a 60-bed long-term acute care facility. Infect Control Hosp Epidemiol. 2012;33(4):405–8.
Furuno JP, Comer AC, Johnson JK, Rosenberg JH, Moore SL, MacKenzie TD, et al. Using antibiograms to improve antibiotic prescribing in skilled nursing facilities. Infect Control Hosp Epidemiol. 2014;35(S3):S56–61.
Zabarsky TF, Sethi AK, Donskey CJ. Sustained reduction in inappropriate treatment of asymptomatic bacteriuria in a long-term care facility through an educational intervention. Am J Infect Control. 2008;36(7):476–80.
Naughton BJ, Mylotte JM, Ramadan F, Karuza J, Priore RL. Antibiotic use, hospital admissions, and mortality before and after implementing guidelines for nursing home-acquired pneumonia. J Am Geriatr Soc. 2001;49(8):1020–4.
Monette J, Miller MA, Monette M, Laurier C, Boivin J-F, Sourial N, et al. Effect of an educational intervention on optimizing antibiotic prescribing in long-term care facilities. J Am Geriatr Soc. 2007;55(8):1231–5.
Loeb M, Brazil K, Lohfeld L, McGeer A, Simor A, Stevenson K, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomized controlled trial. BMJ. 2005;331(7518):669–72.
Pettersson E, Vernby A, Molstad S, Lundborg CS. Can a multifaceted educational intervention targeting both nurses and physicians change the prescribing of antibiotics to nursing home residents? A cluster randomized controlled trial. J Antimicrob Chemother. 2011;66(11):2659–66.
Fleet E, Rao GG, Patel B, Cookson B, Charlett A, Bowman C, et al. Impact of implementation of a novel antimicrobial stewardship tool on antibiotic use in nursing homes: a prospective cluster randomized control pilot study. J Antimicrob Chemother. 2014;69(8):2265–73.
Zimmerman S, Sloane PD, Bertrand R, Olsho LE, Beeber A, Kistler C, et al. Successfully reducing antibiotic prescribing in nursing homes. J Am Geriatr Soc. 2014;62(5):907–12.
Linnebur SA, Fish DN, Ruscin JM, Radcliff TA, Oman KS, Fink R, et al. Impact of a multidisciplinary intervention on antibiotic use for nursing home-acquired pneumonia. Am J Geriatr Pharmacother. 2011;9(6):442–50.
Nicolle LE. Antimicrobial stewardship in long term care facilities: what is effective? Antimicrob Resist Infect Control. 2014;3(6): doi:10.1186/2047-2994-3-6
Moro ML, Gagliotti C. Antimicrobial resistance and stewardship in long-term care settings. Future Microbiol. 2013;8(8):1011–25.
Rhee SM, Stone ND. Antimicrobial stewardship in long-term care facilities. Infect Dis Clin N Am. 2014;28(2):237–46.
Crnich CJ, Jump R, Trautner B, Sloane PD, Mody L. Optimizing antibiotic stewardship in nursing homes: a narrative review and recommendations for improvement. Drugs Aging. 2015;32:699–716.
Fleming A, Browne J, Byrne S. The effect of interventions to reduce potentially inappropriate antibiotic prescribing in long-term care facilities: a systematic review of randomised controlled trials. Drugs Aging. 2013;30(6):401–8.
Stone ND, Ashraf MS, Calder J, Crnich CJ, Crossley K, Drinka PJ, et al. Definitions of infection for surveillance in long-term care facilities: revisiting the McGeer criteria. Infect Control Hosp Epidemiol. 2012;33(10):965–77.
Hutt E, Ruscin J, Corbett K, Radcliff TA, Kramer AM, Williams EM, et al. A multifaceted intervention to implement guidelines improved treatment of nursing home-acquired pneumonia in a state veterans home. J Am Geriatr Soc. 2006;54(11):1694–700.
Walker S, McGeer A, Simor AE, Armstrong-Evans M, Loeb M. Why are antibiotics prescribed for asymptomatic bacteriuria in institutionalized elderly people?: a qualitative study of physicians’ and nurses’ perceptions. CMAJ. 2000;163(3):273–7.
Rotjanapan P, Dosa D, Thomas KS. Potentially inappropriate treatment of urinary tract infections in two Rhode Island nursing homes. Arch Intern Med. 2011;171(5):438–43.
D’Agata E, Loeb MB, Mitchell SL. Challenges assessing nursing home residents with advanced dementia for suspected urinary tract infections. J Am Geriatr Soc. 2013;61(11):62–6.
Rummukainen ML, Jakobsson A, Matsinen M, Jarvenpaa S, Nissinen A, Karppi P, et al. Reduction in inappropriate prevention of urinary tract infections in long-term care facilities. Am J Infect Control. 2012;40(8):711–4.
Harris-Kojetin L, Sengupta M, Park-Lee E, Valverde R. Long-term care services in the United States: 2013 overview. National Center for Health Statistics. Vital Health Stat 2013;3(37):1-107.
Association of American Medical Colleges. 2012 Physician Specialty Data Book. 2012, page 10.
Ernst EJ, Klepser ME, Bosso JA, Rybak MJ, Hermsen ED, Segarra-Newnham M, et al. Recommendations for training and certification for pharmacists practicing, mentoring, and educating in infectious diseases pharmacotherapy. Pharmacother. 2009;29(4):482–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Suzanne F. Bradley declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Infectious Diseases in the Elderly
Rights and permissions
About this article
Cite this article
Bradley, S.F. Antimicrobial Stewardship and Infection Prevention in Long-Term Care Settings: New Strategies to Prevent Resistant Organisms. Curr Geri Rep 5, 16–24 (2016). https://doi.org/10.1007/s13670-016-0158-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-016-0158-9