Abstract
Purpose of Review
This review will examine the use of uterine artery embolization (UAE) for the management of adenomyosis (AUB-A) and evaluate its advantages and disadvantages.
Recent Findings
In the last 5 years, 8 articles have described UAE for the management of AUB-A. These include 2 prospective and 5 retrospective studies and 1 systematic review and meta-analysis. There are no randomised controlled trials for UAE as a treatment of adenomyosis. Recent data report a reduction in heavy menstrual bleeding (HMB) in 80–88% of patients and a reduction in dysmenorrhoea in 76–80% of those undergoing UAE. Quality of life is reported to be significantly improved and uterine volumes reduced following treatment. Disadvantages of UAE include post-procedural pain, adenomyoma extrusion, pyomyoma, Asherman syndrome, and requirement for further intervention including subsequent hysterectomy for management of pain or bleeding.
Summary
Initial non-randomised data support uterine artery embolization as an effective modality for the conservative management of AUB-A. The advantages of UAE include avoidance of abdominal surgery, significant improvement in symptoms, and quality of life scores and preservation of reproductive potential. To date, most data are retrospective with no randomised controlled studies and a few prospective analyses. Randomised controlled data are needed to comprehensively evaluate UAE as conservative treatment for AUB-A and to compare efficacy, cost, and durability of both medical and surgical treatments.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adenomyosis is a condition in which endometrial glands and stroma are found in the myometrium with subsequent inflammation and myometrial hypertrophy [1]. The condition was first described in the early twentieth century. It is a recognised structural cause of abnormal uterine bleeding in the current FIGO classification system (the ‘A’ in the PALM-COIEN classification system) [2, 3]. Women with adenomyosis usually present with heavy menstrual bleeding, dysmenorrhoea, and mass-related symptoms. Other symptoms may include non-menstrual pelvic pain and subfertility [4, 5]. The exact prevalence of adenomyosis is difficult to determine, as histological confirmation is considered the gold standard [6]. Histological findings of specimen after hysterectomy for benign indications reveal adenomyosis in 10 to 25% of uteri. Yet, in selected populations, the prevalence could be up to 80% [7,8,9,10]. Advancements in imaging modalities have improved non-invasive diagnosis of adenomyosis with sensitivities and specificities of 65.0% and 97.5% and 77.5% and 92.5% for ultrasound and MRI, respectively [11].
Management of adenomyosis can be defined as medical, surgical, and radiological with the specific treatment modality, or combination treatment depending on symptom profile and patient preference. Hormonal and non-hormonal medical therapy is most often considered the first-line treatment. The most studied method is the use of LNG-IUS for symptomatic adenomyosis [6]. Surgical intervention in the form of hysterectomy has traditionally been reserved for those who are refractory to medical therapy, have completed their families, or who suffer from predominantly mass-related symptoms. An alternative method is uterine artery embolization for women who desire uterine preservation or wish to avoid surgery.
Methodology
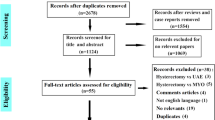
We performed a literature search in the PubMed and Cochrane databases between 2016 and 2021. Search terms included “adenomyosis” and “uterine artery embolization” in sequence and in combination. The search was limited to studies published in English language. A total of 118 articles were identified and screened for inclusion based on publication title and abstract. The bibliographies of relevant studies were screened for additional publications. A total of 8 studies were identified including 2 prospective, 5 retrospective, and a systematic review and meta-analysis. These studies are summarised in Table 1.
What Is Uterine Artery Embolization?
UAE for the management of benign leiomyoma (AUB-L) was first described by Ravina et al. in the mid-1990s [12]. Our knowledge of this application has expanded markedly with the findings of long-term reductions in symptom severity scores and improvement in quality-of-life scores of up to 64% and 23%, respectively [13]. Randomised controlled studies comparing UAE to other procedures for management of AUB-L continue to demonstrate treatment superiority with low rates of subsequent hysterectomy [14].
The procedure involves occlusion of subsidiaries of the uterine vessels using digital subtraction angiography (DSA) [15]. The embolization particles used are usually tris-acryl gelatin microspheres (TAGM) or non-spherical polyvinyl alcohol particles (PVA). The latter is associated with lower procedural radiation with comparable symptom response [15, 16]. Transfemoral access has been traditionally used. However, recent data shows that radial artery access results in less pain, shorter procedure times, and reduced length of stay following UAE [17, 18]. Occlusion of the blood supply to the uterus and the target lesion/s leads to hypoxia, ischaemia, and necrosis of the proliferative ectopic glandular tissue with minimal disruption to the surrounding normal tissue [19]. Subsequent resorption and remodelling results in decreased AUB-A-associated symptoms.
AUB-A Symptom Control Following UAE
Table 2 summarises the data on clinical response following UAE for AUB-A. Dysmenorrhoea is the hallmark symptom of adenomyosis and is reported in up to 90% of symptomatic patients [20•]. In a prospective evaluation of 115 women with dysmenorrhoea who underwent UAE, moderate improvement in symptoms was observed in 64 (55.7%) and a marked improvement in 31 (27.0%) cases 12 months following UAE [21]. A systematic review and meta-analysis in 2007 supports those findings. The authors reviewed 30 studies including 1049 patients with adenomyosis (pure AUB-A and mixed AUB-A/L) between 1999 and 2016. They found improvement in up to 93.9% of patients at 12-month follow-up [22]. Long-term data from this study showed that although initial response rates were similar, patients who had combined AUB-A and AUB-L had a sustained response to treatment compared with those who had AUB-A alone [22]. It might be due to the more diffuse infiltration of AUB-A compared to AUB-L and could explain the greater likelihood of symptom deterioration in the longer term. There are many different methods to quantify reductions in dysmenorrhoea following UAE and this heterogeneity clouds data interpretation and perhaps overestimates treatment response. A retrospective study that employed visual analogue scales (VAS) with clearly defined “improvement” parameters to assess post-procedural dysmenorrhoea demonstrated a reduction in dysmenorrhoea in 80.4% of people at 12-month follow-up (n = 56) [23]. This is supported by a retrospective analysis of 115 people who underwent UAE for the management of AUB-A. The authors reported a reduction in VAS pain scores from 7.45 to 1.32 (mean reduction 6.13, p < 0.001) at extended follow-up (mean follow-up 22.5 months, range 6–84 months) [20•].
UAE is also associated with significant improvement and reduction in HMB. Retrospective studies revealed improvement in abnormal bleeding in 70.9% (n = 227) of women 12 months after UAE, an effect that is sustained for 5 years [19]. These promising data have been reproduced in multiple studies with improvements in HMB between 70.9 and 88.0% of cases (Table 2) [20•, 23, 24, 25••]. This is further supported by a meta-analysis of data from 4 studies involving 111 participants that shows improved bleeding profiles in 81.3% of patients after a mean follow-up of 32 months [22].
Of the studies we reviewed, 4 specifically examined the effect of UAE on uterine volume, as a marker of mass-related symptoms, determined by MRI. A prospective study involving 115 patients demonstrated a progressive mean reduction in uterine volume of 28.0% (p = 0.02), 37.0% (p = 0.02) and 51.0% (p = 0.005) at 3, 6, and 12 months, respectively [21]. In this cohort, the median baseline uterine volume was 790 cm3 and the most significant reduction in the uterine size observed in the first 3 months follow embolization. The remaining retrospective studies showed similar rates of volume reduction of 33–37% at 12 to 15 months, respectively (Table 2) [20•, 25••]. A systematic review and meta-analysis show improvement in mass-related symptoms (81.3%) with an overall reduction in uterine volume approaching 50% at 24-month follow-up [22]. An example of post-UAE mass reduction is seen in Fig. 1 which demonstrates a marked reduction in adenomyoma volume 6 months after UAE.
Forty-five-year-old bank officer G0P0 suffered from severe HMB and dysmenorrhea for many years. Tranexamic acid and norethisterone were not effective. She expelled 2 Mirenas and failed endometrial ablation. MRI showed large focal adenomyosis in the posterior wall; 6 months post-embolisation MRI showed infarction of focal adenoyosis (arrows) and shrinkage from 272 to 115 ml. Note the normal enhancing and viable myometrium (M). Her periods are now lighter than normal and no longer painful
Although UAE is a uterine-sparing method, pregnancy following UAE remains controversial with documented complications including intrauterine growth restriction, preterm birth, and increased rates of caesarean [26,27,28]. Of the studies included in this review, 2 examined pregnancy outcomes with a total of 8 conceptions reported. Of these, 3 underwent elective termination of pregnancy and 2 were complicated by placental insufficiency and preterm birth. The remaining 3 had uncomplicated pregnancies that delivered at term by elective caesarean [20•, 22]. Although we did not encounter studies addressing ongoing fertility following UAE for AUB-A, a systematic review and meta-analysis (n = 353) suggests that UAE does not permanently impact ovarian reserve with no difference in AMH levels detected at 3, 6, and 12 months following UAE for AUB-L [29]. This should be carefully balanced against the documented risk of amenorrhoea, whether secondary to endometrial or ovarian failure.
Predictors of UAE Success
Table 1 shows predictors of AUB-A responsiveness to UAE. In one study, the authors evaluated the impact of UAE on lesion vascularity among 252 patients. Lesion vascularity was classified as hypervascular (abundant vessels centrally and peripherally), isovascular (abundant peripheral vessels and less internal vessels), and hypovascular (a lack of vessels both centrally and peripherally). The vascular supply to the uterus was also assessed and categorised into equal supply (left and right uterine arteries contributing 40–60% of total vascular supply) and unequal supply (one artery dominating with more than 60% of total vascular supply). Patient symptoms including menstrual loss and dysmenorrhoea were evaluated using standardised grading systems with pre-defined markers for improvement. The rates of improvement in dysmenorrhoea and menstrual loss were greater in the hypervascular group when compared to the isovascular and hypovascular groups at 12-month follow-up (Table 2) (86.5% vs. 71.6% and 58.8%, p = 0.002 and 81.0% vs. 68.3% and 60.7%, p = 0.024 respectively). These significant differences were not maintained at 5 years with overall improvements in dysmenorrhoea and HMB in 70.4% and 68.8% of cases, respectively [19].
Lesion vascularity has also been identified as a predictor of complications as demonstrated in a retrospective analysis of UAE for AUB-A [25••]. The authors evaluated 195 patients and found a 12.8% risk of Asherman syndrome following UAE. Univariate and multivariate logistic regression showed that those with hypovascular lesions, when accompanied by increased uterine size, had increased rates of post-procedural uterine synechiae (p = 0.019, OR 0.495, CI 0.275–0.891). The authors postulated that poor vascularity increased the risk of embolic agent reflux into surrounding uterine vasculature with increased global myometrial and endometrial basal layer infarction [25••].
The presence of endometriosis has also been suggested as a predictor of UAE success in the management of AUB-A. In a retrospective study involving 76 patients, the authors examined the impact of ovarian endometriosis on symptom reduction following UAE. They showed that patients without endometriosis had statistically significant improvements in dysmenorrhoea (86.0% vs. 47.1%, p = 0.001) when compared to those with no imaging evidence of endometriosis. Differences in reduction of heavy menstrual loss was also observed, but did not reach significance (84.0% vs. 63.6%, p = 0.263).
Another proposed predictor of treatment outcome following UAE can be found in differentiating between pure adenomyosis and mixed adenomyosis with accompanying leiomyomas (AUB-A/L). In a prospective study (2017), Health-Related Quality of Life (HRQOL) and Symptoms Severity (SSS) were evaluated among 29 patients with pure AUB-A (n = 14) and mixed AUB-A/L (n = 15) at 7-year follow-up [30]. In this small study, high patient satisfaction ratings of 72% were recorded with no statistically significant differences in HRQOL scores. Symptom Severity Scores, however, were superior in the mixed AUB-A/L groups. Hysterectomy was avoided by 82.0% of women and 74% of cases remained asymptomatic at extended follow-up [30]. These findings were supported by a meta-analysis involving 601 patients that demonstrated a greater improvement in patients with combined disease at long-term follow-up (85.4% vs. 74.0%, p = 0.003) [22].
Disadvantages of UAE
Uterine artery embolization, although considered a minimally invasive procedure, is not without risks. A 2017 systematic review found 20 publications involving 615 patients that reported complications. The most common post-procedural symptom was abdominal pain in 67.2% of patients. The pain lasted 2 weeks in 87.4% of cases [22]. Studies looking at varying pain management strategies have failed to identify a superior post-procedural pain protocol and pain should be managed with standard non-steroidal anti-inflammatory drugs, paracetamol, and breakthrough opioid medications [31]. A single randomised controlled trial, however, supports the use of pre-procedural dexamethasone for inflammation suppression and improved pain scores in the first 24 h [32]. Actual complications, including spontaneous expulsion of leiomyomata and endometritis, were reported in 1.6% and 0.7% of cases respectively with a single case of pseudoaneurysm [22].
Persistent amenorrhoea was reported in 13 studies and comprised 6.3% of the total population, all of whom were over 40 years of age. Others reported amenorrhoea rate between 1.7 and 21% with the patient age above 45 in all cases [20•, 25••, 30]. This complication could be due to infarction of the basal endometrium with or without Asherman syndrome as reported rates of proven ovarian failure are lower [19, 25••, 33]. A single-centre study evaluating data from 264 patients reported a peri-procedural death secondary to pulmonary embolism [19]. It is unclear if this was either directly or indirectly associated with the procedure. In general, the absolute risk-related death due to UAE appears low.
Beyond post-procedural complications, another disadvantage of UAE is an ongoing possibility of intervention subsequent to treatment failure. Repeat intervention procedures post-UAE are rare and were reported as 3.0% in only one study [20•]. Hysterectomy rates in the reviewed studies varied between 2.6 and 17.9% at extended follow-up [20•, 22, 30]. Data from the included meta-analysis reports subsequent hysterectomy rates of 2.6% [22].
Conclusion
While UAE remains an accepted conservative treatment option for the management of AUB-L, its application in the management of adenomyosis remains unclear. This is reflected by the relatively small number of publications that have examined the topic in the previous 5 years. Despite limitations in the data available, UAE is a promising conservative treatment modality for women suffering from adenomyosis with HMB, dysmenorrhoea, or mass symptoms. Significant reductions in mass-related symptoms are described in up to 81.3% of patients following UAE for AUB-A [20•, 21, 22, 25••]. This is accompanied by a reduction in HMB and dysmenorrhoea in up to 79.4% and 88.7%, respectively [19, 22].
The advantages of an effective, minimally invasive procedure are centred around avoidance of a major abdominal procedure; particularly for obese or comorbid patients. UAE is also an alternative option for women who wish to preserve their uterus for personal or reproductive reasons. As demonstrated in this review, there is limited data on pregnancy following UAE for AUB-A and those wishing to pursue pregnancy should be advised of its association with growth restriction and preterm birth. This is reflected in the cautious statements on reproduction following UAE issued by both the American and Australian colleges for Obstetrics and Gynaecology.
Risks of post-procedural pain, Asherman syndrome, amenorrhoea, early menopause, pyomyoma, pseudoaneurysm, and treatment failure have been well documented. There is significant variation in the rates of hysterectomy following UAE for management of AUB-A; however, the most reliable data indicates a rate of 2.6% [22]. UAE remains a safe and effective management strategy for adenomyosis refractory to medical management in appropriately counselled patients.
Advantages
-
Minimally invasive
-
Uterine preservation
-
Alternative option in patients with surgical comorbidities
-
Improves dysmenorrhoea, heavy menstrual bleeding, and mass symptoms
Disadvantages
-
Risk of treatment failure and subsequent hysterectomy
-
Limited data on pregnancy following UAE
-
Risk of complications
-
Not a definitive procedure
Conclusion
Uterine artery embolization offers a safe and effective conservative treatment modality for the management of adenomyosis.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Bird CC, McElin TW, Manalo-Estrella P. The elusive adenomyosis of the uterus–revisited. Am J Obstet Gynecol. 1972;112(5):583–93.
Stratopoulou CA, Donnez J, Dolmans MM. Origin and pathogenic mechanisms of uterine adenomyosis: what is known so far. Reprod Sci. 2021;28(8):2087–97.
Munro MG, Critchley HOD, Fraser IS. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet. 2018;143(3):393–408.
Lohle PNM, Higué D, Herbreteau D. Uterine artery embolisation in women with symptomatic adenomyosis. Presse Med. 2019;48(4):435–9.
Donnez J, Donnez O, Dolmans MM. Introduction: uterine adenomyosis another enigmatic disease of our time. Fertil Steril. 2018;109(3):369–70.
Abbott JA. Adenomyosis and abnormal uterine bleeding (AUB-A)-pathogenesis diagnosis and management. Best Pract Res Clin Obstet Gynaecol. 2017;40:68–81.
Vercellini P, Parazzini F, Oldani S, Panazza S, Bramante T, Crosignani PG. Adenomyosis at hysterectomy: a study on frequency distribution and patient characteristics. Hum Reprod. 1995;10(5):1160–2.
Di Donato N, Montanari G, Benfenati A, Leonardi D, Bertoldo V, Monti G, et al. Prevalence of adenomyosis in women undergoing surgery for endometriosis. Eur J Obstet Gynecol Reprod Biol. 2014;181:289–93.
Vannuccini S, Petraglia F. Recent advances in understanding and managing adenomyosis. F1000Res. 2019;8.
Bergholt T, Eriksen L, Berendt N, Jacobsen M, Hertz JB. Prevalence and risk factors of adenomyosis at hysterectomy. Hum Reprod. 2001;16(11):2418–21.
Bazot M, Cortez A, Darai E, Rouger J, Chopier J, Antoine J-M, et al. Ultrasonography compared with magnetic resonance imaging for the diagnosis of adenomyosis: correlation with histopathology. Hum Reprod. 2001;16(11):2427–33.
Ravina JH, Herbreteau D, Ciraru-Vigneron N, Bouret JM, Houdart E, Aymard A, et al. Arterial embolisation to treat uterine myomata. Lancet. 1995;346(8976):671–2.
D’Hoore T, Timmerman D, Laenen A, Maleux G. Long-term outcome and pre-interventional predictors for late intervention after uterine fibroid embolization. Eur J Obstet Gynecol Reprod Biol. 2020;247:149–55.
Laughlin-Tommaso S, Barnard EP, AbdElmagied AM, Vaughan LE, Weaver AL, Hesley GK, et al. FIRSTT study: randomized controlled trial of uterine artery embolization vs focused ultrasound surgery. Am J Obstet Gynecol. 2019;220(2):174.e1-174.e13.
Lacayo EA, Khera SS, Spies JB. Impact of patient and procedure-related factors on radiation exposure from uterine artery embolization. Cardiovasc Intervent Radiol. 2020;43(1):120–6.
Han K, Kim SY, Kim HJ, Kwon JH, Kim GM, Lee J, et al. Nonspherical polyvinyl alcohol particles versus tris-acryl microspheres: randomized controlled trial comparing pain after uterine artery embolization for symptomatic fibroids. Radiology. 2021;298(2):458–65.
Khayrutdinov E, Vorontsov I, Arablinskiy A, Shcherbakov D, Gromov D. A randomized comparison of transradial and transfemoral access in uterine artery embolization. Diagn Interv Radiol. 2021;27(1):59–64.
Himiniuc LMM, Murarasu M, Toma B, Popovici R, Grigore AM, Scripcariu IS, et al. Transradial embolization, an underused type of uterine artery embolization approach: a systematic review. Medicina. 2021;57(2):83.
Zhou J, He L, Liu P, Duan H, Zhang H, Li W, et al. Outcomes in adenomyosis treated with uterine artery embolization are associated with lesion vascularity: a long-term follow-up study of 252 cases. PLoS One. 2016;11(11):e0165610.
• Liang E, Brown B, Rachinsky M. A clinical audit on the efficacy and safety of uterine artery embolisation for symptomatic adenomyosis: Results in 117 women. Aust N Z J Obstet Gynaecol. 2018;58(4):454–9. Findings in this study demonstrate symptom reduction and improved QoL scores at long-term follow-up.
Wang S, Meng X, Dong Y. The evaluation of uterine artery embolization as a nonsurgical treatment option for adenomyosis. Int J Gynaecol Obstet. 2016;133(2):202–5.
de Bruijn AM, Smink M, Lohle PNM, Huirne JAF, Twisk JWR, Wong C, et al. Uterine artery embolization for the treatment of adenomyosis: a systematic review and meta-analysis. J Vasc Interv Radiol. 2017;28(12):1629–42.
Zheng R, Zeng D, Wan TT, Guo WB, Guo Y, Liu MJ. Predisposing factors for predicting the therapeutic response of adenomyosis after uterine artery embolization: serum CA125 levels and accompanying endometriosis. Diagn Interv Radiol. 2018;24(6):364–71.
Guo W, Hu S, Zeng D, Yan C, Zheng R, Gao J, et al. The prognostic role of ovarian endometriosis in symptomatic adenomyosis patients underwent uterine artery embolization. Ann Palliat Med. 2021;10(3):2577–83.
•• Wang Y, Lyu W, Xu W, Yu Y. Asherman syndrome in adenomyosis treated with uterine artery embolization: incidence predictive factors. Radiol Med. 2020;125(5):437–43. Findings in this study suggest that decreased lesion vascularity at the time of embolization increases the risk of subsequent intrauterine synechiae formation.
Gynaecologists TRAaNZCoOa. Uterine artery embolisation for the treatment of uterine fibroids. C-Gyn 23. 2020.
ACOG Committee Opinion. Uterine artery embolization. Obstet Gynecol. 2004;103(2):403–4.
Dessouky R, Gamil SA, Nada MG, Mousa R, Libda Y. Management of uterine adenomyosis: current trends and uterine artery embolization as a potential alternative to hysterectomy. Insights Imaging. 2019;10(1):48.
El Shamy T, Amer SAK, Mohamed AA, James C, Jayaprakasan K. The impact of uterine artery embolization on ovarian reserve: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2020;99(1):16–23.
de Bruijn AM, Smink M, Hehenkamp WJK, Nijenhuis RJ, Smeets AJ, Boekkooi F, et al. Uterine artery embolization for symptomatic adenomyosis: 7-year clinical follow-up using UFS-Qol questionnaire. Cardiovasc Intervent Radiol. 2017;40(9):1344–50.
Saibudeen A, Makris GC, Elzein A, Wigham A, Patel R, Husainy MA, et al. Pain management protocols during uterine fibroid embolisation: a systematic review of the evidence. Cardiovasc Intervent Radiol. 2019;42(12):1663–77.
Kim SY, Koo BN, Shin CS, Ban M, Han K, Kim MD. The effects of single-dose dexamethasone on inflammatory response and pain after uterine artery embolisation for symptomatic fibroids or adenomyosis: a randomised controlled study. BJOG. 2016;123(4):580–7.
Kim MD. Uterine artery embolization for leiomyomas and adenomyosis: a pictorial essay based on our experience from 1300 cases. Korean J Radiol. 2019;20(10):1462–73.
Acknowledgements
Thanks are given to Dr. Eisen Liang, Interventional Radiologist, Sydney Adventist Hospital, for the images presented in Fig. 1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Uterine Fibroids and Endometrial Lesions
Rights and permissions
About this article
Cite this article
Knapman, B.L., Abbott, J. & Vyas, M.A. The Advantages and Disadvantages of Uterine Artery Embolization in Women with Adenomyosis: What’s New?. Curr Obstet Gynecol Rep 10, 92–100 (2021). https://doi.org/10.1007/s13669-021-00309-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-021-00309-0