Abstract
Purpose of Review
While the delivery of medications through enteral tubes is common in critically ill patients, there are complications and a lack of unified practices between institutions. The purpose of this review is to evaluate current practices and literature evidence regarding this administration route. The effect of this administration on the medication’s efficacy, safety, tolerability, and pharmacokinetics was examined, as well as other considerations to ensure that this route of delivery is both safe and effective for patients.
Recent Findings
Studies have found crushed oral tablets are the most frequent cause of obstructed feeding tubes. Complications such as this are primarily due to inadequate personnel training and failure to properly access medications before enteral administration.
Summary
There are many factors that should be considered in order to effectively administer drugs via enteral tubes. Formal training and use of a multi-disciplinary approach that includes pharmacists and dieticians has been shown to reduce tube obstructions and administration errors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The administration of oral medications via enteral nutrition (EN) is common in critically ill patients. Although this method of delivery poses many challenges in practice, the enteral delivery of medications is generally preferred to intravenous (IV) administration. As the conversion from IV therapy to oral (PO) therapy is being emphasized as a clinical initiative, this method of delivery becomes increasingly necessary.
The EN delivery of medications offers many advantages over IV administration, such as reduced costs and decreased potential adverse effects, such as line-related infections [1,2,3]. In patients with chronic enteral access, need for EN is essential to avoid long-term IV medication use. Many medications are not available in IV formulations, especially outpatient medications for the management of chronic diseases. The lack of IV formulations becomes problematic not only in providing therapy for acute issues but also with continuation of home medications and management of comorbid conditions.
Administration of medications through enteral feeding tubes provides solutions to these issues, but there are potential barriers to this method of delivery. Feeding tubes are prone to clogging or obstruction and often require surgical or endoscopic tube replacement. Clogged feeding tubes usually result from improper preparation and administration of medications. Studies have found crushed oral tablets are the most frequent cause of obstructed feeding tubes [4, 5]. In addition to clogging feeding tubes, the inappropriate administration of medications through an access device can result in reduced drug efficacy and increased drug toxicity.
Guidance to avoid these issues is provided in resources such as the Institute for Safe Medication Practices (ISMP) with their “Oral Dosage Forms that Should Not be Crushed” comprehensive list and also the FDA-approved drug labeling provided by manufacturers [6•]. Unfortunately, many of the commercially available liquid formulations of medications are expensive, and compounding can be both labor-intensive and costly. Furthermore, the product information generally states “do not crush” without providing further details that would allow for clinical judgment.
While there have been various review articles over the years regarding medication delivered through the enteral route, practice heavily relies on experience, and methodology varies widely between institutions. The purpose of this review is to examine current practices and available literature regarding the enteral delivery of medications, to highlight potential barriers, and to discuss solutions to ensure this route of delivery is both safe and effective for patients.
Current Practices
Oral liquid formulations of medication are the preferred dosage form for delivery through enteral feeding tubes [7, 8]. These formulations must either be commercially available or compounded in the pharmacy. However, the commercially available oral liquid formulations can be more expensive or are pediatric formulations and thus require a large fluid volume for administration of adult doses. Compounding by pharmacy is also associated with issues such as higher costs and increased labor without the guarantee of similar efficacy. Compounded solutions or suspensions will also have shorter beyond-use dates than commercially available preparations, and stability data may be lacking. Due to these obstacles, oral tablets and capsules are commonly modified to be administered with EN.
Modifying oral tablets for enteral tube administration is generally performed by nurses. There is often a lack of formal training on this procedure causing nurses to learn administration practices from what has been passed on from other nurses [9, 10]. Methods for administering medication via feeding tubes are provided in various references [8, 11]. There are generally two approaches for administering oral tablets, either (1) crushing the tablet with instruments such as a mortar and pestle or (2) dispersion of the tablet in 10–30 mL of sterile water. Some experts recommend the latter approach in every case, whereas others claim this is only appropriate if the tablet will disperse completely within 2 min [8]. Regardless of the approach, feeding tubes should be flushed with 15–30 mL of sterile water before and after medication administration. In addition, each medication should be administered separately to avoid mixing of medication in the feeding tube [7, 8].
Similar to oral tablets, oral capsules that contain a powdered drug can be opened up and their contents mixed with 10–30 mL of sterile water. Liquid-filled capsules are more challenging to administer. Proper administration of liquid capsules requires puncturing the gelatin capsule with a needle and allowing the aspirated contents to be mixed with water. Alternatively, the capsule can be dissolved in warm water and all contents (except any undissolved gelatin portion) are administered. The first approach has the potential to acquire less than the total dose of the medication, resulting in subtherapeutic doses. The latter approach may be more accurate but is more time-consuming. If possible, switching to an alternative medication or to a different formulation that does not have a liquid-filled capsule may be a more effective strategy.
In the instances when the medication cannot be administered per the tube or by alternative routes, and there are no available compounded or commercially available products, as a last resort, the medication is discontinued or transitioned to a similar medication that can be administered via the feeding tube.
If a tube does become obstructed, there are various options to try to unclog the tube to allow for administration. The simplest, cheapest, and perhaps most effective method is to use warm water. If warm water is ineffective, carbonated beverages are often tried as a second-line therapy. For tubes that remain clogged, despite the previous therapies, a mixture of pancreatic enzymes and bicarbonate is an effective option [7]. Determining the cause of the obstruction is useful. If the obstruction is due to a medication, the American Society for Parenteral and Enteral Nutrition (ASPEN) recommends an acidic beverage, whereas protein clogs from the enteral formula will respond better to pancreatic enzymes [12].
Considerations
The pharmacokinetic and pharmacodynamics of a medication must be considered when administering a medication through feeding tubes, as well as the clinical use, tolerability, and efficacy of the medication. Feeding tube characteristics also play a role in this decision.
Feeding Tube Characteristics
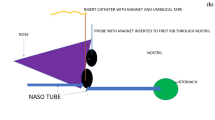
The size and placement of the feeding tube will affect the likelihood of obstruction, as well as tolerability and efficacy of the medication. Small-bore feeding tubes are generally 5–12 French units (1 French unit = 0.33 mm in diameter), whereas large-bore tubes are more than 14 French units. While small-bore tubes are more comfortable for the patient, they have an increased risk of becoming clogged. Due to the smaller diameter of jejunostomy tubes, it is recommended that medications be in liquid form rather than crushed oral tablets to avoid potential obstruction [7, 8].
The placement of the feeding tube influences many medication pharmacokinetic parameters. Some medications require the location of the stomach to exert their mechanism of action. These medications, such as antacids and sucralfate, are consequently ineffective if delivered to the small bowel [8]. In addition, medications that require gastric acidity to be activated (e.g., aspirin) are not absorbed and could result in therapeutic failure [7, 13].
A review article by McIntyre and Monk investigated the safety and efficacy of 70 medications administered via post-pyloric feeding tubes [13]. The authors determined that various medications were absorbed to a greater extent in the small bowel, such as fluconazole and ciprofloxacin. In contrast, medications such as gabapentin and lopinavir-ritonavir were absorbed when administered directly into the duodenum or jejunum. The reduced absorption of the HIV medications is clinically concerning, as incomplete absorption could result in increased resistance.
The results found by McIntyre and Monk are alarming for many reasons. The authors highlight several concerns with post-pyloric medication administration. Patients that have ventricular assist devices (VADs) who require antiplatelet therapy with aspirin may have decreased drug exposure when bypassing the acidic environment of the stomach. Post-operatively, enteral access may only be feasible through feeding tubes, and if not tolerated, generally a post-pyloric tube is placed. Thus, despite antithrombotic therapy (e.g., aspirin) being essential in these patients, it may not be effective due to decreased absorption by bypassing the stomach.
Administering medications through post-pyloric tubes also affects medications that undergo first-pass hepatic metabolism. This form of metabolism occurs after medications are absorbed in the stomach and are partly metabolized by the liver prior to reaching the systemic circulation. By avoiding this partial metabolism, these medications (e.g., morphine, midazolam, and lidocaine) will have potentially higher serum levels leading to possibly toxic effects [7, 8, 10]. Additionally, bypassing this metabolic phase could theoretically lead to therapeutic failure in medications that require hepatic metabolism to be activated.
Tolerability may also be compromised when medications are administered directly into the small bowel. Many medications with high osmolality have been shown to cause osmotic diarrhea, bloating, and cramping when administered via jejunal or duodenal tubes [7, 13, 14]. The small bowel is also less tolerant of the administration of large fluid volumes when compared with the stomach. This is a concern when using low-concentration formulations such as pediatric liquids or some IV formulations given by the enteral route.
In addition to tube placement and size, the functionality of the feeding tube must be considered. NG tubes are commonly used for suctioning contents of the stomach. Some clinicians recommend against administering any medications through this tube due to medication removal upon suctioning [13]. Other experts argue that clamping the tube for at least 30 min post-medication administration will allow for medication absorption [7, 8]. Despite the stance on this issue, it is imperative that pharmacists and other clinicians caring for the patient are aware of the indication of the NG tube.
Oral Tablets and Capsules
Many oral tablets and oral capsules can be manipulated to be administered via feeding tubes, but those that cannot be crushed will have to be transitioned to a different formulation or route of administration. Crushing oral tablets often alters the integrity and function of the medication. Additionally, crushing agents that are enteric coated (EC) or sustained release (SR) would result in the loss of gastric protection by EC formulations and potentially faster rates of distribution from SR formulations. By crushing the tablets with EC and SR, these functions are removed [6•, 7].
For SR medications, crushing tablets may result in higher peak concentrations initially and lower concentrations towards the end of the dosing interval [10]. Losing this integrity could even result in drug-free intervals, which could be unfavorable with medications that have the potential for withdrawal symptoms. This loss of drug activity would be detrimental with medications that depend on a steady state above a certain therapeutic level for efficacy, such as time-dependent antimicrobials.
Crushing EC tablets will allow liberation and absorption by the gastric acid of the stomach instead of its desired location in the small intestine. A common example of this is the proton pump inhibitors (PPIs). Omeprazole and lansoprazole are delayed-release capsules that contain enteric-coated granules, and pantoprazole is a delayed-release tablet. For this class of medications, either lansoprazole 3 mg/mL or omeprazole 2 mg/mL suspension should be utilized, or instead switched to a histamine-2 receptor antagonist (H2RA) that can be crushed [8].
In addition to SR and EC medications, hazardous medications that possess adverse effects such as teratogenic properties should not be crushed, to avoid harming the nurse or the administrator. The ISMP “do not crush” list mentioned previously identifies medications that are inappropriate to crush and provides a reason for this recommendation [6•]. This list however does not provide solutions or alternatives. Furthermore, institutions are known to stray from these instructions due to anecdotal evidence. For an example, tamsulosin is on ISMP’s “do not crush” list for its CR actions, but in practice, the capsule is often opened and beads are administered via tubes. The CR actions are thought to be preserved as long as the beads are not broken. Other previously published references have also provided a list of medications that should not be crushed [8, 11].
Liquid Formulations
Although oral liquid formulations are preferred to tablets and capsules during enteral administration, liquid formulations still have the potential to cause adverse effects. Like tablets, liquid formulations can lead to tube occlusion. Specifically, viscous syrups are the most likely to cause an obstruction when exposed to feeding formulas [7]. Furthermore, many oral liquids are created for pediatric use which involves smaller total doses. These formulations are specifically designed to have low concentrations for accuracy in measurement. Thus, the large volume requirements of pediatric formulations can lead to intolerance when given at adult doses.
Excipients (i.e., inactive ingredients) in liquid formulations are a major concern for tolerability when administered via enteral tubes. The most problematic excipient, sorbitol, is commonly used to sweeten and improve palatability of medications but is also a potent osmotic laxative [7, 10]. Diarrhea is a common symptom seen in patients receiving EN, and the cause is often incorrectly blamed on the nutrition formula. Studies have shown that diarrhea is often caused by drug excipients rather than the formula itself [15, 16•, 17].
Liquid formulations with the least amount of sorbitol are preferred. Doses of sorbitol greater than 20 g/day are thought to cause diarrhea while doses greater than 10 g/day can still cause cramping, bloating, and flatulence [7]. There are multiple previously published lists of medications and their sorbitol content [8, 13, 18]. However, these lists are not all-inclusive and manufacturers do not always disclose the amount of sorbitol in their labeling information. Suspensions often contain less sorbitol than syrups but are sometimes more hypertonic, which also may lead to GI intolerance [7].
The pH and osmolality of liquid formulations are highly influential on tolerability and compatibility with EN tube feeds. The osmolality of gastrointestinal fluids ranges from 100 to 400 mOsm/kg [8]. Hyperosmotic formulations lead to osmotic diarrhea and are most problematic when administered into the small bowel. Acidic formulations are known to bind EN formulas and lead to tube obstructions [14].
Authors Klang et al. evaluated the osmolality, pH, and physical compatibility of 62 liquid formulations with EN. The authors stated that osmolality should aim to be less than 700 mOsm for gastric administration and less than 300 mOsm for jejunal administration. Their study found 17 medications (including propranolol, sulfamethoxazole-trimethoprim) with an osmolality greater than 5000 mOsm and 3 products (potassium iodine, dexamethasone intensol, and ergocalciferol) with an osmolality greater than 10,000 mOsm. Formulations that contained a pH less than 4.5, such as carbamazepine, formed a solid clog [14].
To prevent osmotic diarrhea, gastric administration of liquids with high osmolality should be used preferentially over jejunal administration. Diluting hyperosmotic formulations in sterile water is a method to reduce the osmolality. An equation (below) will determine the amount of water required to achieve the osmolality goals that Klang and colleagues described [8, 14, 19].
The sorbitol content (% w/v) and osmolality (mOsm/kg) of various medications are described in Table 1. This list provides values for certain medications whose properties have been explored trough pharmacokinetic studies, stated by the manufacturer or by inquiry of other investigators [7, 8, 11, 14, 18, 19]. This list has some limitations in that it is not all-inclusive and varies with manufacturers. However, it still provides an estimate for volume dilution (above), and in combination with the sorbitol content, it can help delineate if excipients are the cause of adverse effects such as diarrhea.
Drug-Nutrient Interactions
There are many potential interactions between EN formulas and both the active and inactive ingredients of medications. Thus, the compatibility and the stability of the EN formula and the medication must be evaluated. The ASPEN guidelines recommend against adding medications directly to enteral formulas [20].
Management of compatibility issues may involve holding tube feeds during medication administration, changing the dose of the medication, changing the feeding formula, or changing to an alternate but similar medication. The reduced absorption of phenytoin is a common example that has been discussed in the literature for over 20 years. Management of this interaction involves both holding tube feeds and increasing the dose of phenytoin [20].
Wohlt and coauthors performed a literature review exploring the interactions of 46 medications with enteral feeding formulas. For each medication, the authors provided the mechanism for the interaction, potential management strategies, and a grade of evidence. Wohlt et al. concluded that there is a lack of evidence and consensus regarding many of the medications and emphasized the need for further pharmacokinetic studies to evaluate these interactions. In order to prevent interactions, it is imperative to have institutional policies, utilize resources (pharmacists and dieticians), and change products (medication or enteral formula) to avoid potential interactions.
Alternative Medication Formulations
Changing the medication formulation is an approach to delivering medications via the enteral route. For example, a patient with a jejunostomy tube takes a medication that is not available in an oral liquid formulation. Converting the medication to a transdermal or rectal administration may be an alternative strategy, such as use of a promethazine suppository or clonidine transdermal patch. Beckwith and colleagues provide a list of alternative routes for certain medications [8].
If the medication is not available in an alternative form, a medication within the same class or with a similar mechanism of action can be used. Paroxetine liquid is often utilized when other selective serotonin reuptake inhibitors (SSRIs) cannot be administered; an example being in patients who cannot receive crushed medications via a jejunostomy tube. Few of the SSRIs are available in a liquid formulation, and paroxetine is generally the cheapest option. Caution should be taken with this approach however, as that the patient may still experience withdrawal symptoms and there is not much guidance available on equivalent dosing [21, 22].
Opioids are a class of medications that are often administered via feeding tubes, both on an inpatient and outpatient basis. Various opioids, such as morphine, are available in liquid formulations. In patients who have high requirements and are not opioid naïve, fentanyl patches are a useful option. There is literature available to provide equivalence dosing and to guide transitioning between various opioids [23•].
Multi-disciplinary Approach
A solution to many of the possible barriers discussed above is the use of a multi-disciplinary team to manage medication administration via the enteral route. A pre- and post-intervention study by van den Bemt et al. at two Dutch hospitals demonstrated the impact of an integrated program to improve the administration of oral medications through enteral tube feeds. The project team consisted of a pharmacist, pharmacy technician, quality manager, dietician, and head nurse. The program required that the nurses receive a formal training session, which is uncommon at most institutions [9, 10].
The program also consisted of daily ward visits by pharmacy technicians, who would screen medications of patients who were on enteral tube feeds, suggest alternative medications if needed, and provide advice on appropriate administration techniques. EC and modified-release medications were flagged in the electronic health record (EHR) in order to alert a contraindication in the computer for those patients that are on enteral feeds. A “do not crush” icon was also printed on the unit dose labels for these medications. Other measures included placing a laminated card on the medication cart listing the “five golden tube rules” and creating a database of oral dosage forms [10].
The program resulted in a decrease in the number of tube obstructions and a reduction in administration errors [10]. These outcomes are important to the patient, reduce institution liability, and result in important clinical outcomes. Although mortality was not measured in this study, the decreased need for replacement of surgical tubes, less medication toxicity, and reduced medication efficacy were all seen as additional positive outcomes. Thus, a competency-based service composed of a multi-disciplinary team is suggested to manage patients receiving oral medications by enteral methods.
Conclusions
Inappropriate administration of medications can result in many detrimental issues that include compromising the efficacy and safety of medications, delaying the delivery of nutrition, and increasing the need for endoscopic or surgical interventions (such as tube replacement). Clinicians, including pharmacists, dieticians, and nurses, must be competent in administering medications by the enteral route and identifying potential problems that may arise by such strategy.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Nathwani D, Lawson W, Dryden M, Stephens J, Corman S, Solem C, et al. Implementing criteria-based early switch/early discharge programmes: a European perspective. Clin Microbiol Infect. 2015;21(Suppl 2):S47–55.
Cyriac JM, James E. Switch over from intravenous to oral therapy: a concise overview. J Pharmacol Pharmacother. 2014;5(2):83–7.
Paladino JA, Sperry HE, Backes JM, Gelber JA, Serrianne DJ, Cumbo TJ, et al. Clinical and economic evaluation of oral ciprofloxacin after an abbreviated course of intravenous antibiotics. Am J Med. 1991;91(5):462–70.
Belknap DC, Seifert CF, Petermann M. Administration of medications through enteral feeding catheters. Am J Crit Care. 1997;6(5):382–92.
Gora ML, Tschampel MM, Visconti JA. Considerations of drug therapy in patients receiving enteral nutrition. Nutr Clin Pract. 1989;4(3):105–10.
Institute for Safe Medication Practices (ISMP). Oral dosage forms that should not be crushed. Assessed at ismp.org. Updated 2019. This is an online resource provided by ISMP that lists oral medications that should not be crushed. The list also provides reasoning for the recommendations.
Williams NT. Medication administration through enteral feeding tubes. Am J Health Syst Pharm. 2008;65(24):2347–57. https://doi.org/10.2146/ajhp080155.
Beckwith MC, Feddema SS, Barton RG, Graves C. A guide to drug therapy in patients with enteral feeding tubes: dosage form selection and administration methods. Hosp Pharm. 2004;39(3):225–37.
Leff RD, Roberts RJ. Enteral drug administration practices: report of a preliminary survey. Pediatrics. 1988;81(4):549–51.
Van den bemt PM, Cusell MB, Overbeeke PW, et al. Quality improvement of oral medication administration in patients with enteral feeding tubes. Qual Saf Health Care 2006;15(1):44–47.
Sacks GS. Drug-nutrient considerations in patients receiving parenteral and enteral nutrition. Pract Gastroenterol. 2004;28(7):39–48.
Bankhead R, Boullata J, Brantley S, Corkins M, Guenter P, Krenitsky J, et al. Enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr. 2009;33(2):122–67.
Mcintyre CM, Monk HM. Medication absorption considerations in patients with postpyloric enteral feeding tubes. Am J Health Syst Pharm. 2014;71(7):549–56.
Klang M, Mclymont V, Ng N. Osmolality, pH, and compatibility of selected oral liquid medications with an enteral nutrition product. JPEN J Parenter Enteral Nutr. 2013;37(5):689–94.
Hill DB, Henderson LM, Mcclain CJ. Osmotic diarrhea induced by sugar-free theophylline solution in critically ill patients. JPEN J Parenter Enteral Nutr. 1991;15(3):332–6.
De brito-ashurst I, Preiser JC. Diarrhea in critically ill patients: the role of enteral feeding. JPEN J Parenter Enteral Nutr. 2016;40(7):913–23. This review article discusses a common issue in patients receiving enteral nutrition, diarrhea. The article highlights the potential etiologies, specifically considerations with medications that are administered via EN tubes.
Chang SJ, Huang HH. Diarrhea in enterally fed patients: blame the diet? Curr Opin Clin Nutr Metab Care. 2013;16(5):588–94.
Lutomski DM, Gora ML, Wright SM, Martin JE. Sorbitol content of selected oral liquids. Ann Pharmacother. 1993;27(3):269–74.
Estoup M. Approaches and limitations of medication delivery in patients with enteral feeding tubes. Crit Care Nurse. 1994;14(1):68–72 77-9.
Wohlt PD, Zheng L, Gunderson S, Balzar SA, Johnson BD, Fish JT. Recommendations for the use of medications with continuous enteral nutrition. Am J Health Syst Pharm. 2009;66(16):1458–67. https://doi.org/10.2146/ajhp080632.
Keks N, Hope J, Keogh S. Switching and stopping antidepressants. Aust Prescr. 2016;39(3):76–83.
American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder, Third Edition. 2010.
American Pain Society. Pain Management and Dosing Guide. 2016. Assessed from americanpainsociety.org. This includes the most recent guidelines for pain management from the American Pain Society. These guidelines discuss morphine equivalents and provide recommendations for transitioning between opioids.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kathryn S. Bandy, Stephanie Albrecht, Bhavyata Parag, and Stephen A. McClave declare they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Gastroenterology, Critical Care, and Lifestyle Medicine
Rights and permissions
About this article
Cite this article
Bandy, K.S., Albrecht, S., Parag, B. et al. Practices Involved in the Enteral Delivery of Drugs. Curr Nutr Rep 8, 356–362 (2019). https://doi.org/10.1007/s13668-019-00290-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-019-00290-4