Abstract
Purpose of Review
This article will discuss new advances in cryoprobe technology and procedural utilization for the diagnosis of lung cancer and parenchymal lung diseases.
Recent Findings
Newly developed smaller cryoprobes can offer similar diagnostic advantages of standard cryoprobes when used as a diagnostic modality in a variety of lung conditions.
Summary
Bronchoscopic lung cryobiopsy is an innovative diagnostic technique for intraparenchymal lung diseases. Over the past decade, research has been dedicated to evaluating the safety profile of this technique, developing a standard procedural approach, and exploring the utility of this approach for a variety of indications. In this article, we will review recent developments for the diagnostic utility of cryobiopsy in interstitial lung diseases, lung cancer, and lung transplant. We will also describe a technical approach for the procedure and evaluate complications and areas of ongoing research. With a similar safety profile and superior diagnostic yield compared to transbronchial forceps biopsy, ongoing research and development may pave the way for transbronchial lung cryobiopsy to become a first-line, minimally invasive diagnostic approach for many intraparenchymal lung diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A common dilemma for chest physicians is deciding the most appropriate diagnostic modality for patients with intraparenchymal lung diseases. Surgical lung biopsy (SLB) is considered the gold standard for many diseases, but it is expensive; invasive, requires hospitalization; and is associated with significant morbidity and mortality in patients with interstitial lung disease [1,2,3,4]. Bronchoscopy with transbronchial forceps biopsy (TFBx) is a less costly, minimally invasive technique that does not require hospitalization and offers a much lower risk profile for patients [5,6,7,8,9]. But it comes with the significant trade-off a small tissue sample that has architectural distortion due to crush artifact [1, 10]. In 2009, a cryoprobe, which had previously been used for therapeutic endobronchial ablation and tumor debulking, was successfully trialed in 41 patients as a minimally invasive, tissue-preserving diagnostic technique for intraparenchymal lung diseases [11]. Since its inception as a viable diagnostic modality, transbronchial lung cryobiopsy (TCBx) has undergone significant development and innovation in both technique and application [12,13,14,15,16]. Here, we will review the latest innovation in transbronchial lung cryobiopsy during the past few years.
Transbronchial Lung Cryobiopsy
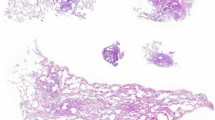
The science behind the cryoprobe is based on the Joule–Thomson effect, which is a thermodynamic principle that describes the cooling phenomenon of most compressed gases when they are released through a valve at high velocity [17, 18]. There are operator-dependent variations in TCBx technique, but the general approach is that a cryoprobe, generally a 1.7-mm probe, is introduced via flexible bronchoscope to a fluoroscopically guided target area not within 1 cm from pleura [19]. A cooling cycle is initiated for 2–8 s, freezing the tumor or lung parenchyma, which results in cryoadhesion of the tissue to the end of the cryoprobe. Freezing time recommendations vary depending on the cryoprobe used and operator preference [14, 20, 21]. In general, a longer freezing cycle will result in a larger amount of tissue adhesion to the probe. The frozen tissue section and cryoprobe are removed simultaneously from the lung and detached from the cryoprobe tip in formalin [17, 20, 22, 23]. The benefit of this procedural approach is that it yields larger, architecturally preserved tissue samples compared to TFBx, and its minimally invasive nature dramatically reduces the morbidity, mortality, and cost associated with SLB [7, 12, 21, 24,25,26,27,28,29]. However, the procedure is not without risk, and it has been associated with slightly higher complication rates of airway bleeding and pneumothorax compared to forceps biopsy, and even rare cases of mortality (see Fig. 1) [5, 6, 17, 30, 31]. It is this risk/benefit ratio that has generated so much interest in cyrobiopsy over the past decade. However, due to its development as an emerging technique, the lack of a standard technical method to perform the procedure has been a major impediment to the widespread implementation of TCBx [1, 32]. Here, we will describe the technical aspects and most common approach for TCBx.
In TFBx, the forceps are designed to pass through the bronchoscope, with the biopsied specimen enclosed within the forceps and withdrawn through the instrument channel (IC). The bronchoscope should remain in the airway of interest throughout the procedure, allowing the operator to evaluate for and control any bleeding complications. Due to the compression of the biopsied specimen, forceps biopsy comes at the cost of “crushing” the tissue during the enclosure and removal process [7, 11, 17]. In TCBx, the cryoprobe and bronchoscope must be removed from the airway simultaneously due to the large frozen specimen attached to the cryoprobe, as the larger tissue specimen typically cannot pass through the IC [17, 26]. Standard bronchoscopes generally have a 2.0-mm IC, and larger “therapeutic” bronchoscopes can have up to a 3.2-mm IC [33], but cryobiopsy obtained specimens are frequently 2–4 times larger than that. Because the bronchoscope is removed from the airway, a secure airway should be obtained for TCBx, as bleeding is a known complication and the operator must have the ability to rapidly reinsert the bronchoscope [29]. To better control potential bleeding complications, it is recommended that a fogarty balloon or bronchial blocker be placed parallel to the bronchoscope in the airway and inflated right as the scope is removed until the bronchoscope can reintroduced, allowing for control of any bleeding and prevention of spillover to adjacent segments and lobes with resultant hypoxia and difficulty with ventilation [19, 20]. Once the scope is reintroduced, the balloon can be deflated under direct visualization, with rapid reinflation if bleeding is seen distal to the balloon.
Due to the concern of removing the bronchoscope from a potentially bleeding airway, mini-cryoprobes of 1.1 mm have been developed and can be introduced to the airway of interest via guide sheath and retracted through the IC, allowing the bronchoscope to remain in the airway throughout the procedure (Table 1). A concern with sheath retraction through working channel is crush artifact seen in TFBx and sheath shearing, though sample quality in porcine models was similar to that of specimens obtained by standard TCBx [14, 16].
Interstitial Lung Disease
Interstitial lung diseases (ILD) make up a group of diagnostically challenging conditions that often require a multidisciplinary discussion (MDD) between a team of specialists, including pulmonologists, radiologists, and pathologists, to make a diagnosis [2, 36]. The final diagnosis frequently depends on the pathological evaluation of an adequate tissue sample, though obtaining this tissue via SLB gives clinicians pause, as it is associated with a mortality rate quoted between 3–4% in patients with ILD [3]. TFBx is associated with substantially less morbidity and mortality compared to SLB, but it offers a diagnostic yield in only one-third of cases in patients with ILD [2]. The common diagnostic dilemma for a clinician involves a patient with poor cardiopulmonary reserve and an unclear diagnosis based on imaging studies. The decision to proceed with a diagnostic surgical lung biopsy is based on the physician’s clinical experience, potential to discover a treatable condition, and weighing the risk/benefit ratio with the patient. In this already frail patient population, there is a definite need for a less-invasive diagnostic approach that would provide adequate tissue specimen, which is why TCBx has generated so much interest over the past several years. Indeed, three recently published major clinical practice guidelines make mention of cryobiopsy and have specific questions dedicated to its utility in the diagnosis of ILD [1, 2, 19].
Two-thirds of cases of idiopathic pulmonary fibrosis (IPF) can be diagnosed based on radiographic and clinical information alone, and do not require surgical lung biopsy. SLB is recommended in cases of diagnostic uncertainty, though data demonstrates mortality is exceptionally high in patients found to have IPF who undergo SLB [1, 4]. The most recent consensus guidelines on the diagnosis of IPF published in 2018 make mention of TCBx but make no recommendation for or against this diagnostic approach. Though the panel was “enthusiastic” about development of this minimally invasive diagnostic approach, and recognized the diagnostic yield to be 80% with low associated morbidity and mortality, the lack of comparison to SLB and no defined standard approach to the procedure led to the panel to make no formal recommendation with regard to TCBx in the diagnosis of IPF [1]. Importantly, just 1 year after this consensus guideline was released, the results of the COLDICE study were published.
The COLDICE study evaluated the diagnostic accuracy of TCBx compared to the gold standard SLB in patients with ILD. In this prospective, multicenter study, 65 patients requiring biopsy to aid in the diagnosis of ILD underwent sequential TCBx and SLB. Tissue samples were de-identified for pathologists and multidisciplinary discussants. From this study, two main points can be derived: first, there is substantial agreement in histopathological patterns between TCBx and SLB at ~ 70% agreement, with improvement to 77% diagnostic agreement after MDD, and second, the study described a standard technical procedural approach for the use of TCBx in the diagnosis of ILD [21]. The data from COLDICE produced data that conflicted with results from a study published by Romagnali et al. the year prior, which showed poor concordance between TCBx and SLB in 21 patients with ILD [37]. In fact, the results from Romagnoli discouraged practitioners from considering TCBx as a viable diagnostic technique in ILD [38]. But with the data from the larger COLDICE study, and two meta-analyses on cryobiopsy in ILD among other studies, in 2020 the American College of Chest Physicians (ACCP) released six official statements regarding the use of TCBx for the diagnosis of ILD [19, 21, 27, 39]. The ACCP panel concluded that based on local expertise and individualized risk/benefit discussion with patients, that TCBx can be used to obtain tissue specimen for MDD in patients with ILD [19]. The five other statements detail a recommended technical approach for TCBx, largely in line with the approach described in the COLDICE study: 1.9 mm cryoprobe with endobronchial blocker, biopsies taken under fluoroscopy 1 cm from pleura from 2 separate segments or lobes [19, 21]. COLDICE also detailed an average freeze time of 4.6 s and a total of 4 biopsies [21].
In August 2020, 4 months after the ACCP published their expert panel report, the American Thoracic Society released an official practice guideline on the diagnosis of hypersensitivity pneumonitis (HP). The panel separated HP into two distinct phenotypes and made different recommendations for each phenotype. The panel suggested cryobiopsy in cases of ILD with suspected fibrotic HP, mainly in order to reduce SLB in this population. They made no recommendation regarding TCBx in suspected non-fibrotic HP, as TFBx can be used to rule out other diffuse lung diseases such as infection and malignancy, where the diagnostic yield for TFBx is 68% [2]. The diagnostic yield for TCBx in patients with HP is 91%, which can be interpreted as patients with HP suspected ILD, SLB can be avoided in 80–90% of these cases if TCBx is used [2]. With the data derived from these studies and recommendations from the latest practice guidelines from major medical societies, TCBx should be considered as a reasonable diagnostic approach in conjunction with multidisciplinary discussions for higher risk patients with ILD in centers with an established cryobiopsy program [1, 2, 25, 40].
Lung Cancer
Lung cancer is often silent in the early stages and is consistently the leading cause of cancer related death in males and females in developed countries worldwide [41,42,43]. Early diagnosis is paramount to mortality reduction, and the widespread implementation of low-dose CT (LDCT) imaging in high-risk patients along with the development of precision therapeutic medical options in lung cancer has led to an explosion of interest in minimally invasive advanced diagnostic methods [44,45,46,47]. The use of a cryoprobe for endobronchial tumor debulking, “cryorecannulation” has been a safe and successful treatment modality for over 10 years [48,49,50].
Malignant central airway obstruction is a common finding in patients with lung cancer or metastatic spread of non-thoracic cancer to the central airways and its associated symptoms may be the first physical manifestation of a patients disease [51]. Cryoprobes have been in use for the emergent treatment of malignant airway obstructions for over 15 years, and have demonstrated effective tissue death and airway clearance with an acceptable safety profile [50, 52, 53]. Five years after the initial publication describing the technique of cryoprobe tumor debulking, the same group of authors published a report utilizing the cryoprobe, rather than forceps, as a diagnostic tool for endobronchial lesions [7]. Results from that report demonstrated the technique was safe, and more effective than forceps, with a diagnostic yield of 89%, compared to 66% from forceps. Forceps have long been utilized as the most common diagnostic tool for endobronchial tumors. In large, central tumors that can be directly visualized with a bronchoscope, forceps biopsy has a diagnostic accuracy of 65–88%, though samples are small and suffer from significant architectural distortion due to crush artifact [54,55,56,57]. Metanalysis studies and a follow-up, larger prospective comparative trial of forceps vs. cryoprobe for endobronchial tumors demonstrated TCBx resulted in larger, architecturally preserved tissue sample with increased diagnostic yield, 95% vs. 85%, compared to forceps [17, 29].
Innovation to aid in the early diagnosis of peripheral lung tumors has come in the form of advanced bronchoscopy techniques and tumor retrieval devices, such as larger forceps and adjunctive bronchial brushes and needle devices [10, 46, 58]. Despite these advances, forceps biopsies are still associated with small sample size and architectural distortion [17]. TCBx can be used for the diagnosis of peripheral lung tumors, and studies have described different technical approaches with and without a guide sheath, and results have indicated a superior diagnostic yield for the cryoprobe versus forceps [5, 59]. TCBx can be used in conjunction with endobronchial ultrasound (EBUS) or radial EBUS (r-EBUS), and can yield a histological diagnosis in 86–91% of patients [5, 59]. For peripheral nodules eccentrically located or adjacent to airways, the addition of r-EBUS to TCBx can result in higher tissue yield compared to TFBx, 75% compared to 49% [12].
Advances in precision medicine have led to individualized targeted therapies based on the molecular and immunohistochemical characteristics of the tumor [45]. The detection of genetic mutations such as EGFR and PD-L1 in lung cancer may be increased in specimens obtained via cryobiopsy vs. forceps, though technical ability in procedural performance plays a role in obtaining an adequate specimen [15, 60, 61]. In a prospective trial, 16 patients underwent both TCBx and TFBx to compare PD-L1 detection rate. The trial demonstrated a higher 1% PD-L1 detection rate in the cryobiopsy group at 56%, compared to that of 38% in the TFBx group [61]. Genetic analysis and the detection of PD-L1 has serious therapeutic implications, as it changes the recommended first-line therapy. In a retrospective study published last year, cryobiopsy increased the EGFR mutation detection rate compared to forceps and needle techniques by a rate of 22% vs. 14% [60]. A recent pathological feasibility study demonstrated strong histochemical concordance in 43 resected primary lung tumors comparing scalpel vs. cryoprobe [62]. Given the superior diagnostic yield, architectural preservation and immunohistochemical capabilities of cryobiopsy samples compared to forceps, this diagnostic modality should continue to emerge as a promising minimally invasive approach for the diagnosis of lung cancer.
Lung Transplant
Lung allograft recipients make up a rare patient demographic that must undergo frequent lung biopsies to evaluate for transplant-related complications such as allograft rejection, bronchiolitis obliterans syndrome (BOS), and infection [63]. Currently, the standard of care for obtaining biopsy specimens in this population is bronchoscopically guided forceps, though small sample size and crush artifact dictate ten specimens should be obtained for evaluation [63,64,65,66]. In 2013, a group of researchers already familiar with TCBx performed a safety and efficacy study on 17 lung transplant recipients and found superior tissue yield with fewer biopsies compared to TFBx, without additional risk of bleeding and pneumothorax [65]. A larger study compared 81 histopathological specimens in transplant patients and demonstrated TCBx biopsies were larger, did not contain crush artifact, and improved the diagnostic yield of acute and chronic cellular rejection compared to TFBx [67]. The importance of these findings taken together cannot be understated, as these studies demonstrate that TCBx has a similar safety profile to the current standard of care, but it significantly improves biopsy quality, which can change the clinical management of these highly complex patients. To better explore the safety profile and risk factors for complication, a large, prospective trial evaluated 321 cryoprobe specimens and found that adequate tissue was obtained in 97% of patients with yield improving when 4 biopsies were obtained, moderate-to-severe bleeding was found in 7% of patients and pneumothorax occurred in 8% of patients, 4% requiring tube thoracostomy. High blood pressure and single lung transplant recipients were found to be at higher risk for bleeding [68]. A large comparative study of 362 transplant recipients demonstrated high-quality tissue yield using TCBx and no significant difference in bleeding or pneumothorax compared to TFBx [69]. The utility of cryobiopsy in this patient population is to obtain higher quality biopsy specimens that would allow for earlier detection of critical diagnosis, such as cellular rejection and BOS, while exposing patients to no additional risk than the current standard of care.
Challenges and Future Direction
There are several limitations in TCBx involving cryobiopsy technique, specimen analysis, and complication rate. Currently, few expert centers regularly perform the technique, and there is a substantial learning curve that can affect diagnostic yield [15, 70]. The ACCP has outlined some basic technical guidance for TCBx in ILD, but there is a need for standardization for different disease indications, including in lung transplant recipients and malignancy [19, 32]. Studies have demonstrated similar good agreement on biopsied specimens from SLB and TCBx, but lower confidence from pathologists in the cryobiopsy specimens [21]. Cryobiopsy specimens are intralobar and do not contain pleura like SLB, and new guidelines would be beneficial for pathologists to evaluate ILD from this new diagnostic approach. Although complications in TCBx are substantially reduced compared to SLB, the en bloc removal of the bronchoscope and secure airway requirement may deter physicians from this procedure. Smaller cryoprobes that can be withdrawn through the IC of the bronchoscope would remove the need for in-line fogarty balloon and simplify the technique, making it accessible to more proceduralists. Animal studies have been published and human studies are ongoing to evaluate methods for the bronchoscope to remain in the airway throughout the entire procedure. The development of a novel sheath with a small, 1.1 mm cryoprobe provided similar tissue yield compared to standard cryobiopsy and allowed for the bronchoscope to remain in the airway [14, 16]. Bleeding complications, pneumothorax, and mortality have all been observed in TCBx, though the severity of these complications seems to have been increased during the early development phase of this technique. Large, prospective comparative trials are still needed to evaluate different cryoprobe sizes and freezing times for specific diseases in order to create more uniformity in the practice of this emerging diagnostic modality.
Conclusion
Transbronchial cryobiopsy is an emerging diagnostic technique that could play an important role as a preferred, minimally invasive first approach for the diagnosis of intraparenchymal lung diseases. Although more data is needed for standardization of the procedure and appropriate pathological analysis, this approach has already demonstrated a safety profile similar to TFBx, but with superior diagnostic yield. With further research, it may replace the need for SLB for many lung diseases. TCBx has proven in these early trials to be a safe, effective diagnostic option for interstitial lung diseases and lung cancer. There are several novel studies evaluating diagnostic applications and equipment innovation for this new diagnostic tool.
References
Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, Behr J, Cottin V, Danoff SK, Morell F, Flaherty KR, Wells A, Martinez FJ, Azuma A, Bice TJ, Bouros D, Brown KK, Collard HR, Duggal A, Galvin L, Inoue Y, Jenkins RG, Johkoh T, Kazerooni EA, Kitaichi M, Knight SL, Mansour G, Nicholson AG, Pipavath SNJ, et al. Diagnosis of idiopathic pulmonary fibrosis. an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44–e68.
Raghu G, Remy-Jardin M, Ryerson CJ, Myers JL, Kreuter M, Vasakova M, Bargagli E, Chung JH, Collins BF, Bendstrup E, Chami HA, Chua AT, Corte TJ, Dalphin J-C, Danoff SK, Diaz-Mendoza J, Duggal A, Egashira R, Ewing T, Gulati M, Inoue Y, Jenkins AR, Johannson KA, Johkoh T, Tamae-Kakazu M, Kitaichi M, Knight SL, Koschel D, Lederer DJ, et al. Diagnosis of hypersensitivity pneumonitis in adults: an official ATS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2020;202:e36–69.
Kaarteenaho R. The current position of surgical lung biopsy in the diagnosis of idiopathic pulmonary fibrosis. Respir Res. 2013;14:43.
Utz JP, Ryu JH, Douglas WW, Hartman TE, Tazelaar HD, Myers JL, Allen MS, Schroeder DR. High short-term mortality following lung biopsy for usual interstitial pneumonia. Eur Respir J. 2001;17:175–9.
Nasu S, Okamoto N, Suzuki H, Shiroyama T, Tanaka A, Samejima Y, Kanai T, Noda Y, Morita S, Morishita N, Ueda K, Kawahara K, Hirashima T. Comparison of the utilities of cryobiopsy and forceps biopsy for peripheral lung cancer. Anticancer Res. 2019;39:5683–8.
Koslow M, Edell ES, Midthun DE, Mullon JJ, Kern RM, Nelson DR, Sakata KK, Moua T, Roden AC, Yi ES, Reisenauer JS, Decker PA, Ryu JH. Bronchoscopic cryobiopsy and forceps biopsy for the diagnostic evaluation of diffuse parenchymal lung disease in clinical practice. Mayo Clin Proc Innov Qual Outcomes. 2020;4:565–74.
Schumann C, Hetzel J, Babiak AJ, Merk T, Wibmer T, Möller P, Lepper PM, Hetzel M. Cryoprobe biopsy increases the diagnostic yield in endobronchial tumor lesions. J Thorac Cardiovasc Surg. 2010;140:417–21.
Pourabdollah M, Shamaei M, Karimi S, Karimi M, Kiani A, Jabbari HR. Transbronchial lung biopsy: the pathologist’s point of view. Clin Respir J. 2016;10:211–6.
Huang Y, Huang H, Li Q, Browning RF, Parrish S, Turner JF, Zarogoulidis K, Kougioumtzi I, Dryllis G, Kioumis I, Pitsiou G, Papaiwannou A, Lampaki S, Machairiotis N, Katsikogiannis N, Madesis A, Karaiskos T, Li Z, Zarogoulidis P. Transbronchial lung biopsy and pneumothorax. J Thorac Dis. 2014;6:S443–7.
Arya R, Boujaoude Z, Rafferty WJ, Abouzgheib W. Usefulness and safety of transbronchial biopsy with large forceps during flexible bronchoscopy. Proc (Bayl Univ Med Cent). 2020;34:232–6.
Babiak A, Hetzel J, Krishna G, Fritz P, Moeller P, Balli T, Hetzel M. Transbronchial cryobiopsy: a new tool for lung biopsies. Respiration. 2009;78:203–8.
Kho SS, Chan SK, Yong MC, Tie ST. Performance of transbronchial cryobiopsy in eccentrically and adjacently orientated radial endobronchial ultrasound lesions. ERJ Open Research. 2019;5.
Mehrad M, Colby TV, Rossi G, Cavazza A. Transbronchial cryobiopsy in the diagnosis of fibrotic interstitial lung disease. Arch Pathol Lab Med. 2020;144:1501–8.
Yarmus LB, Semaan RW, Arias SA, Feller-Kopman D, Ortiz R, Bösmüller H, Illei PB, Frimpong BO, Oakjones-Burgess K, Lee HJ. A randomized controlled trial of a novel sheath cryoprobe for bronchoscopic lung biopsy in a porcine model. Chest. 2016;150:329–36.
Udagawa H, Kirita K, Naito T, Nomura S, Ishibashi M, Matsuzawa R, Hisakane K, Usui Y, Matsumoto S, Yoh K, Niho S, Ishii G, Goto K. Feasibility and utility of transbronchial cryobiopsy in precision medicine for lung cancer: prospective single-arm study. Cancer Sci. 2020;111:2488–98.
Hetzel J, Linzenbold W, Boesmueller H, Enderle M, Poletti V. Evaluation of Efficacy of a new cryoprobe for transbronchial cryobiopsy: a randomized, controlled in vivo animal study. Respiration. 2020;99:248–56.
Ganganah O, Guo SL, Chiniah M, Li YS. Efficacy and safety of cryobiopsy versus forceps biopsy for interstitial lung diseases and lung tumours: a systematic review and meta-analysis. Respirology. 2016;21:834–41.
Horbaniuc BD. Refrigeration and Air-Conditioning. Encyclopedia of Energy. Elsevier; 2004. p. 261–89. https://www.sciencedirect.com/topics/earth-and-planetary-sciences/joule-thomson-effect.
Maldonado F, Danoff SK, Wells AU, Colby TV, Ryu JH, Liberman M, Wahidi MM, Frazer L, Hetzel J, Rickman OB, Herth FJF, Poletti V, Yarmus LB. Transbronchial cryobiopsy for the diagnosis of interstitial lung diseases: CHEST guideline and expert panel report. Chest. 2020;157:1030–42.
Ravaglia C, Wells AU, Tomassetti S, Gurioli C, Gurioli C, Dubini A, Cavazza A, Colby TV, Piciucchi S, Puglisi S, Bosi M, Poletti V. Diagnostic yield and risk/benefit analysis of trans-bronchial lung cryobiopsy in diffuse parenchymal lung diseases: a large cohort of 699 patients. BMC Pulm Med. 2019;19:16.
Troy LK, Grainge C, Corte TJ, Williamson JP, Vallely MP, Cooper WA, Mahar A, Myers JL, Lai S, Mulyadi E, Torzillo PJ, Phillips MJ, Jo HE, Webster SE, Lin QT, Rhodes JE, Salamonsen M, Wrobel JP, Harris B, Don G, Wu PJC, Ng BJ, Oldmeadow C, Raghu G, Lau EMT. Cryobiopsy versus open lung biopsy in the diagnosis of interstitial lung disease alliance (COLDICE) investigators. Diagnostic accuracy of transbronchial lung cryobiopsy for interstitial lung disease diagnosis (COLDICE): a prospective, comparative study. Lancet Respir Med. 2020;8:171–181.
Lentz RJ, Argento AC, Colby TV, Rickman OB, Maldonado F. Transbronchial cryobiopsy for diffuse parenchymal lung disease: a state-of-the-art review of procedural techniques, current evidence, and future challenges. J Thorac Dis. 2017;9:2186–203.
DiBardino DM, Lanfranco AR, Haas AR. Bronchoscopic cryotherapy. clinical applications of the cryoprobe, cryospray, and cryoadhesion. Ann American Thorac Soc. 2016;13:1405–1415.
Pajares V, Puzo C, Castillo D, Lerma E, Montero MA, Ramos-Barbón D, Amor-Carro O, Gil de Bernabé A, Franquet T, Plaza V, Hetzel J, Sanchis J, Torrego A. Diagnostic yield of transbronchial cryobiopsy in interstitial lung disease: a randomized trial. Respirology. 2014;19:900–906.
Tomassetti S, Ravaglia C, Wells AU, Cavazza A, Colby TV, Rossi G, Ley B, Ryu JH, Puglisi S, Arcadu A, Marchi M, Sultani F, Martinello S, Donati L, Gurioli C, Gurioli C, Tantalocco P, Hetzel J, Dubini A, Piciucchi S, Klersy C, Lavorini F, Poletti V. Prognostic value of transbronchial lung cryobiopsy for the multidisciplinary diagnosis of idiopathic pulmonary fibrosis: a retrospective validation study. Lancet Respir Med. 2020;8:786–94.
Dhooria S, Sehgal IS, Aggarwal AN, Behera D, Agarwal R. Diagnostic yield and safety of cryoprobe transbronchial lung biopsy in diffuse parenchymal lung diseases: systematic review and meta-analysis. Respir Care. 2016;61:700–12.
Iftikhar IH, Alghothani L, Sardi A, Berkowitz D, Musani AI. Transbronchial lung cryobiopsy and video-assisted thoracoscopic lung biopsy in the diagnosis of diffuse parenchymal lung disease. a meta-analysis of diagnostic test accuracy. Ann Am Thorac Soc. 2017;14:1197–1211.
Unterman A, Wand O, Fridel L, Edelstein E, Pertzov B, Kramer MR. High diagnostic accuracy of transbronchial cryobiopsy in fibrotic interstitial lung diseases compared to final explant diagnosis. Respiration. 2019;98:421–7.
Hetzel J, Eberhardt R, Herth FJF, Petermann C, Reichle G, Freitag L, Dobbertin I, Franke KJ, Stanzel F, Beyer T, Möller P, Fritz P, Ott G, Schnabel PA, Kastendieck H, Lang W, Morresi-Hauf AT, Szyrach MN, Muche R, Shah PL, Babiak A, Hetzel M. Cryobiopsy increases the diagnostic yield of endobronchial biopsy: a multicentre trial. Eur Respir J. 2012;39:685–90.
Hetzel J, Eberhardt R, Petermann C, Gesierich W, Darwiche K, Hagmeyer L, Muche R, Kreuter M, Lewis R, Ehab A, Boeckeler M, Haentschel M. Bleeding risk of transbronchial cryobiopsy compared to transbronchial forceps biopsy in interstitial lung disease - a prospective, randomized, multicentre cross-over trial. Respir Res. 2019;20:140.
Pajares V, Núñez-Delgado M, Bonet G, Pérez-Pallarés J, Martínez R, Cubero N, Zabala T, Cordovilla R, Flandes J, Disdier C, Torrego A. MULTICRIO Group researchers. Transbronchial biopsy results according to diffuse interstitial lung disease classification. Cryobiopsy versus forceps: MULTICRIO study. PLoS One. 2020;15:e0239114.
Hetzel J, Maldonado F, Ravaglia C, Wells AU, Colby TV, Tomassetti S, Ryu JH, Fruchter O, Piciucchi S, Dubini A, Cavazza A, Chilosi M, Sverzellati N, Valeyre D, Leduc D, Walsh SLF, Gasparini S, Hetzel M, Hagmeyer L, Haentschel M, Eberhardt R, Darwiche K, Yarmus LB, Torrego A, Krishna G, Shah PL, Annema JT, Herth FJF, Poletti V. Transbronchial cryobiopsies for the diagnosis of diffuse parenchymal lung diseases: expert statement from the cryobiopsy working group on safety and utility and a call for standardization of the procedure. Respiration. 2018;95:188–200.
Bronchoscopes - Pulmonology - Olympus Medical Systems. at https://www.olympus-europa.com/medical/en/Products-and-Solutions/Products/Pulmonology/Bronchoscopes.html.
Wall CP, Gaensler EA, Carrington CB, Hayes JA. Comparison of transbronchial and open biopsies in chronic infiltrative lung diseases. Am Rev Respir Dis. 1981;123:280–5.
Han Q, Luo Q, Xie J-X, Wu L-L, Liao L-Y, Zhang X-X, Chen R-C. Diagnostic yield and postoperative mortality associated with surgical lung biopsy for evaluation of interstitial lung diseases: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2015;149:1394-401.e1.
Tomassetti S, Piciucchi S, Tantalocco P, Dubini A, Poletti V. The multidisciplinary approach in the diagnosis of idiopathic pulmonary fibrosis: a patient case-based review. Eur Respir Rev. 2015;24:69–77.
Romagnoli M, Colby TV, Berthet J-P, Gamez AS, Mallet J-P, Serre I, Cancellieri A, Cavazza A, Solovei L, Dell’Amore A, Dolci G, Guerrieri A, Reynaud P, Bommart S, Zompatori M, Dalpiaz G, Nava S, Trisolini R, Suehs CM, Vachier I, Molinari N, Bourdin A. Poor concordance between sequential transbronchial lung cryobiopsy and surgical lung biopsy in the diagnosis of diffuse interstitial lung diseases. Am J Respir Crit Care Med. 2019;199:1249–56.
Raghu G, Lederer DJ, Rabe KF. Cryobiopsy for interstitial lung disease: the heat is on. Am J Respir Crit Care Med. 2019;199:1183–4.
Sharp C, McCabe M, Adamali H, Medford AR. Use of transbronchial cryobiopsy in the diagnosis of interstitial lung disease-a systematic review and cost analysis. QJM. 2017;110:207–14.
Dhooria S, Agarwal R, Sehgal IS, Aggarwal AN, Goyal R, Guleria R, Singhal P, Shah SP, Gupta KB, Koolwal S, Akkaraju J, Annapoorni S, Bal A, Bansal A, Behera D, Chhajed PN, Dhamija A, Dhar R, Garg M, Gopal B, Hibare KR, James P, Jindal A, Jindal SK, Khan A, Kishore N, Koul PA, Kumar A, Kumar R, et al. Bronchoscopic lung cryobiopsy: an Indian association for bronchology position statement. Lung India. 2019;36:48–59.
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108.
Feinstein AR, Wells CK. A clinical-severity staging system for patients with lung cancer. Medicine. 1990;69:1–33.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Oudkerk M, Liu S, Heuvelmans MA, Walter JE, Field JK. Lung cancer LDCT screening and mortality reduction - evidence, pitfalls and future perspectives. Nat Rev Clin Oncol. 2021;18:135–51.
Liu X, Wang P, Zhang C, Ma Z. Epidermal growth factor receptor (EGFR): A rising star in the era of precision medicine of lung cancer. Oncotarget. 2017;8:50209–20.
Chen AC, Pastis NJ, Mahajan AK, Khandhar SJ, Simoff MJ, Machuzak MS, Cicenia J, Gildea TR, Silvestri GA. Robotic bronchoscopy for peripheral pulmonary lesions: a multicenter pilot and feasibility study (BENEFIT). Chest. 2021;159:845–52.
Ost DE, Yeung S-CJ, Tanoue LT, Gould MK. Clinical and organizational factors in the initial evaluation of patients with lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e121S–41S.
Schumann C, Hetzel M, Babiak AJ, Hetzel J, Merk T, Wibmer T, Lepper PM, Krüger S. Endobronchial tumor debulking with a flexible cryoprobe for immediate treatment of malignant stenosis. J Thorac Cardiovasc Surg. 2010;139:997–1000.
Shepherd RW, Radchenko C. Bronchoscopic ablation techniques in the management of lung cancer. Ann Transl Med. 2019;7:362.
Saka H, Oki M, Kada A, Saito AM. An open-label, single-arm study of CRYO2 for debulking at the site of central airway obstruction or stenosis. In Vivo. 2019;33:1641–4.
Oberg C, Folch E, Santacruz JF. Management of malignant airway obstruction. AME Med J. 2018;3:115–115.
Chaddha U, Hogarth DK, Murgu S. Bronchoscopic ablative therapies for malignant central airway obstruction and peripheral lung tumors. Ann Am Thorac Soc. 2019;16:1220–9.
Hetzel M, Hetzel J, Schumann C, Marx N, Babiak A. Cryorecanalization: a new approach for the immediate management of acute airway obstruction. J Thorac Cardiovasc Surg. 2004;127:1427–31.
Rivera MP, Mehta AC, Wahidi MM. Establishing the diagnosis of lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e142S – e165.
Schreiber G, McCrory DC. Performance characteristics of different modalities for diagnosis of suspected lung cancer: summary of published evidence. Chest. 2003;123:115S-128S.
Hetzel J, Hetzel M, Hasel C, Moeller P, Babiak A. Old meets modern: the use of traditional cryoprobes in the age of molecular biology. Respiration. 2008;76:193–7.
Kendall DM, Gal AA. Interpretation of tissue artifacts in transbronchial lung biopsy specimens. Ann Diagn Pathol. 2003;7:20–4.
Simon M, Simon I, Tent PA, Todea DA, Haranguș A. Cryobiopsy in lung cancer diagnosis-a literature review. Medicina (Kaunas) 2021;57.
Imabayashi T, Uchino J, Yoshimura A, Chihara Y, Tamiya N, Kaneko Y, Yamada T, Takayama K. Safety and usefulness of cryobiopsy and stamp cytology for the diagnosis of peripheral pulmonary lesions. Cancers (Basel). 2019;11.
Haentschel M, Boeckeler M, Ehab A, Wagner R, Spengler W, Steger V, Boesmueller H, Horger M, Lewis RA, Fend F, Kanz L, Bonzheim I, Hetzel J. Cryobiopsy increases the EGFR detection rate in non-small cell lung cancer. Lung Cancer. 2020;141:56–63.
Arimura K, Kondo M, Nagashima Y, Kanzaki M, Kobayashi F, Takeyama K, Tamaoki J, Tagaya E. Comparison of tumor cell numbers and 22C3 PD-L1 expression between cryobiopsy and transbronchial biopsy with endobronchial ultrasonography-guide sheath for lung cancer. Respir Res. 2019;20:185.
Nishida T, Matsumoto Y, Sasada S, Tanaka M, Nakai T, Fukai R, Ohe Y, Watanabe S-I, Motoi N. Feasibility study of cryobiopsy for practical pathological diagnosis of primary lung cancer including immunohistochemical assessment. Jpn J Clin Oncol. 2021;51:271–8.
Hopkins PM, Aboyoun CL, Chhajed PN, Malouf MA, Plit ML, Rainer SP, Glanville AR. Prospective analysis of 1,235 transbronchial lung biopsies in lung transplant recipients. J Heart Lung Transplant. 2002;21:1062–7.
Aboyoun CL, Tamm M, Chhajed PN, Hopkins P, Malouf MA, Rainer S, Glanville AR. Diagnostic value of follow-up transbronchial lung biopsy after lung rejection. Am J Respir Crit Care Med. 2001;164:460–3.
Yarmus L, Akulian J, Gilbert C, Illei P, Shah P, Merlo C, Orens J, Feller-Kopman D. Cryoprobe transbronchial lung biopsy in patients after lung transplantation: a pilot safety study. Chest. 2013;143:621–6.
Tomic R, Podgaetz E, Andrade RS, Dincer HE. Cryotechnology in diagnosing and treating lung diseases. J Bronchology Interv Pulmonol. 2015;22:76–84.
Montero MA, de Gracia J, Culebras Amigo M, Mugnier J, Álvarez A, Berastegui C, Ortiz-Villalón C. The role of transbronchial cryobiopsy in lung transplantation. Histopathology. 2018;73:593–600.
Loor K, Culebras M, Sansano I, Álvarez A, Berastegui C, de Gracia J. Optimization of transbronchial cryobiopsy in lung transplant recipients. Ann Thorac Surg. 2019;108:1052–8.
Gershman E, Ridman E, Fridel L, Shtraichman O, Pertzov B, Rosengarten D, Rahman NA, Shitenberg D, Kramer MR. Efficacy and safety of trans-bronchial cryo in comparison with forceps biopsy in lung allograft recipients: analysis of 402 procedures. Clin Transplant. 2018;32:e13221.
Almeida LM, Lima B, Mota PC, Melo N, Magalhães A, Pereira JM, Moura CS, Guimarães S, Morais A. Learning curve for transbronchial lung cryobiopsy in diffuse lung disease. Rev Port Pneumol. 2017. https://doi.org/10.1016/j.rppnen.2017.09.005.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Interventional Pulmonology
Rights and permissions
About this article
Cite this article
Green, J., Nath, S. & Semaan, R. Recent Advances in Transbronchial Lung Cryobiopsy. Curr Pulmonol Rep 11, 48–55 (2022). https://doi.org/10.1007/s13665-022-00288-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-022-00288-4