Abstract
Purpose of Review
COPD is a prevalent, highly morbid, but manageable disease. Challenges exist in diagnosis that leads to both missed and inappropriate diagnosis with apparent ethnic, sex, and socioeconomic disparities. Disease management is possible with medications and intensive efforts such as pulmonary rehabilitation, but as these interventions are become increasingly expensive, the divide in socioeconomic outcomes expands.
Recent Findings
Health systems have increasingly focused resources on COPD, but the efforts have not been equally implemented. There is increasing prevalence of COPD in women, patients with low socioeconomic status, and minorities attributable to higher burden of tobacco, occupational, and rural exposure. Recent mortality estimates suggest a growing socioeconomic divide.
Summary
As providers and healthcare systems work to improve the diagnosis and care of COPD patients, biases and disparities must be measured, appreciated, and addressed to assure just implementation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In high-income countries, the predominant cause of chronic obstructive pulmonary disease (COPD) is long-term tobacco use, but environmental and occupational factors also play a significant role. Environmental factors—poor air quality, occupational exposures, and a high burden of tobacco exposure—and socioeconomic factors—sex, race/ethnicity, income, and access to adequate healthcare—impact the development, diagnosis, and outcomes of COPD.
In this review, we will discuss the new and most impactful literature investigating the social and demographic factors that influence the development, diagnosis, and management of COPD. As disparities in health are dependent local healthcare systems, the scope of this review focuses predominantly on the USA.
Disease Burden and Prevalence
Prevalence
Estimates of COPD prevalence vary depending on how the diagnosis is made. Studies on prevalence vary in estimates based upon the method of detection, definition of COPD used, and location [1]. The 2011 Behavioral Risk Factor Surveillance System (BRFSS) used patient-reported diagnosis of COPD and showed a prevalence of 6.3% in the USA [2]. The BRFSS data also demonstrated a higher prevalence in women (7.3%) than men (5.7%), a gender disparity borne out in other studies as well [3]. A recent analysis of the burden by state found a large variance from 3.7% in Hawaii to 12% in West Virginia, with a strong association with state-wide smoking rates [4]. The National Health Interview Survey (NHIS) independently asked participants about a physician diagnosis of COPD, emphysema, and/or chronic bronchitis, and found an overall prevalence of 5.7% [5]. COPD prevalence was higher when asking about chronic bronchitis, emphysema (6.1%), and COPD as opposed to COPD alone (3.0%) [2].
Patient-reported estimates consistently underestimate prevalence when compared to measurement by spirometry. The Global Burden of Diseases, Injuries, and Risk Factors (GBD) 2015 study analyzed international data from vital registries. Using the fixed FEV1/FVC ratio of < 0.7 spirometric criteria for obstruction, the age-standardized prevalence was found to be 3.2% in men and 2.0% in women [6]. With an unbiased cross-sectional sample of patients underwent spirometry, the prevalence of moderate to severe obstruction was 10.1%, almost twice as high as reported in patient-reported and registry studies suggesting clinical under-diagnosis [1]. The large variability in prevalence between spirometric and patient-reported diagnosis highlights the need for spirometry in high-risk patients.
Tobacco Exposure
Higher rates of tobacco abuse drive the increased COPD prevalence in low socioeconomic status (SES) groups. In addition, active smokers with an annual income less than US minimum wage experience more deleterious effects of tobacco exposure when compared to higher SES groups [7]. Lowe et al. demonstrated that this population has a more rapid decline in FEV1 over 5 years, although this decline comes without a measurable increase in exacerbations or symptom burden [7]. Both people in the USA living below the poverty line and those with low education achievement have nearly twice the rates of tobacco abuse when compared to those with income more than double the poverty line and highly educated people [8]. Patients with low SES often experience higher psychological stress, potentially explaining higher rates of tobacco abuse, though the relationship is likely far more complex [9]. While cessation attempts for those below the poverty line do not significantly differ from those above it, people who live below the poverty line are substantially less likely to successfully quit [8].
Air Quality/Environmental Exposure
There is considerable data supporting the myriad factors in the physical environment—air pollution, substandard housing/indoor air pollution, rural living with exposure to pesticides, and occupational exposures (including organic and inorganic dusts, irritant gases, and chemicals)—that lead to the development and progression of COPD. Many of these environmental risks are more often experienced by people of low SES, racial/ethnic minorities, and women [10, 11].
Some data suggests that as many as 24% of US adults with a diagnosis of COPD have never smoked, and the majority of these are thought to be caused by occupational exposures [11]. While occupational exposures historically include coal mining and other industrial exposures, similar prevalence (3.1–3.3%) is seen in the information industry (including publishing, data processing workers, and telecommunication) and administrative/office support workers. In these non-smoking patients, women have a higher COPD prevalence than men [11] and there is a higher prevalence of people with low SES [12].
Geography is associated with and may in fact directly affect COPD prevalence. In a large cohort of over 300,000 UK patients, air quality was significantly associated with lung function. Higher small particulate matter (PM2.5) and nitrogen dioxide (NO2) concentrations were associated with worse FEV1 and forced vital capacity (FVC) [13]. This effect was not equally distributed among the population; the association was stronger among people of lower income. Rural patients in the USA are at high risk of COPD not only because established risk factors (i.e., lower SES, fewer insured/less access to healthcare, higher smoking rates) are more prevalent in this population, but also because of higher exposure to environmental triggers (e.g., NO2, organic dust) [14]. In fact, patients in rural settings have a higher age-adjusted prevalence of COPD, more frequent hospitalizations, and a higher mortality from COPD when compared to residents of US cities [14]. An analysis of the SPIROMX data showed that rural residence is associated with increase in moderate, but not severe, COPD exacerbations (in contrast to prior published works showing patients who live in rural areas are at higher risk for severe COPD exacerbations and subsequent in-hospital mortality) [15, 16]. Interestingly, their sub analyses did not fully explain these effects by agricultural exposure alone [16].
While causality is plausible, the association between geography and the development of COPD is unclear due to the challenges of accounting for confounders that track with poor air quality: low SES, racial disparities, access issues [17]. Regardless, it is clear that low SES individuals and communities both experience higher rates of COPD and are exposed to higher concentrations of air pollutants [18].
Diagnosis
COPD is both often missed (i.e., respiratory symptoms with spirometry never ordered or COPD never diagnosed) and mis-diagnosed (i.e., diagnosed with COPD despite no appreciable airway obstruction) [19]. Under-diagnosis is largely driven by underutilization of spirometry, despite efforts to increase use among primary care providers. Many times, spirometry is often only performed when symptoms become severe, delaying diagnosis which is associated with higher costs and higher exacerbation rates compared to patients admitted earlier in disease [20]. COPD is also often underdiagnosed, as the criteria—airflow obstruction on spirometry; exposure to known pulmonary toxins such as cigarettes or poor air quality; respiratory symptoms including cough, dyspnea, and sputum production, and radiographic evidence of airway or alveolar damage—are imprecise [21, 22]. Conversely, in an analysis of the Burden of Obstructive Lung Disease (BOLD) data, 16,177 participants were analyzed with 919 (5.7%) reporting a previous medical diagnosis of COPD. Postbronchodilator spirometry was performed and 61.9% were found to have no obstruction, leading to overdiagnosis, though it is not clear if some of these patients had radiographic evidence of COPD. Among the subjects with false-positive COPD, 45.7% reported current use of respiratory medication, likely with minimal if any clinical benefit and definite economic cost [23].
Estimates of prevalence can vary depending on the definition of COPD used, often impacting certain groups disproportionately. Most guidelines require documentation of obstruction on spirometry after bronchodilators for a diagnosis of COPD [22]. While spirometry is under-utilized in general, spirometry is less likely to be ordered in underserved populations and challenges in diagnosis persist even when spirometry is performed [24]. A cross-sectional analysis of the population—the COPD Genetic Epidemiology (COPDGene®) study—found COPD to be grossly underdiagnosed. Of those diagnosed, women were more likely than men and black patients were less likely than white patients to carry a diagnosis of COPD prior to enrollment [25]. Recently, the COPDGene consortium proposed a new diagnostic criteria where spirometry is not necessary. This approach can limit the bias in diagnosis introduced by the need for spirometry and decrease under-diagnosis [21, 22].
The choice of a spirometric threshold for airway obstruction can inherently introduce bias that may lead to disparities. The Global Burden of Obstructive Lung Disease (GOLD) and other society guidelines recommend using a fixed FEV1/FVC ratio of < 0.70 regardless of age, size, or other demographic parameters [21]. Using the fixed ratio approach, Lamprecht et al. evaluated international data from BOLD and other large, international cohorts to identify determinants of under-diagnosis. Risk factors for under-diagnosis using this approach included male sex, younger age, being an active or never smoker, and less education achievement [26]. Alternatively, the lower limit of normal (LLN) approach adjusts the FEV1/FVC threshold for various patient characteristics such as age, sex, height, and race. While seemingly the best approach for limiting disparities, LLN underdiagnoses patients who are older, non-white, and women [27,28,29]. Bhatt et al. recently compared LLN and fixed ratio of < 0.70 approaches and found no difference in identifying patients who are hospitalized for COPD or died from a COPD; therefore, the clinical importance of the difference in these approaches is not clear [27].
There are reported gender and ethnic differences in the diagnosis of asthma overlap. From a cohort of subjects with COPD, more women and African-Americans were found to have a reported history of asthma. These subjects were found to have more severe and frequent exacerbations than subjects solely with COPD and those of other gender or ethnicities [30]. Whether this is driven by a biologic or health disparity remains unclear.
Many clinical criteria require for a diagnosis of COPD appropriate exposure and duration, often defined by at least 10 pack-years in clinical trials. Recent data suggests duration of exposure, even if lower intensity, is the larger determinant of developing COPD [31]. African-Americans tend to have longer smoking duration at a lower intensity compared to whites in the USA, which could lead to less lung cancer screening and clinical trial opportunities using the traditional pack-year approach to quantifying exposure [32, 33].
Despite a higher prevalence of COPD among women, evidence supports that physicians have a bias that supports diagnosis of COPD more commonly in men [34]. Chapman et al. gave physicians clinical scenarios describing COPD. Physicians were less likely to diagnose COPD if the patient was a woman. If spirometry data was included in the stem, the bias decreased [35]. This is especially concerning given recent mortality estimates that show improvements in mortality have disproportionately occurred in men. Women have higher rates of FEV1 decline when matched for tobacco exposure and have a higher prevalence of COPD despite lower overall tobacco exposure [36]. Whether the discrepancy in prevalence of COPD between sexes is due to inherent physiologic differences (estrogen-related propensity for emphysema, susceptibility to tobacco, etc.) or disparities in diagnosis (higher reporting of symptoms in women, larger impact on health-related quality of life) remains unclear [36].
Management and Access to Care
Minimal evidence exists directly comparing COPD management between socioeconomic groups, but health disparities likely exist. Patients with low SES have numerous barriers to guideline-suggested medications. High cost, insurance companies dictating certain drugs, and lack of inhaler technique training contribute to lower adherence to respiratory medications among patients with lower SES [37, 38]. In the USA, the cost of respiratory medications with proven benefit in COPD is often prohibitively expensive for patients. Even those with health insurance often have out-of-pocket costs that patients of low SES cannot afford [39]. Completion of pulmonary rehabilitation is associated with improved symptom control and decreased exacerbations, yet suboptimal adherence is independently associated with low SES [40]. Tiotropium, a front-line therapy for COPD, is prescribed less often for black patients [41] [42].
The personal economic impact of COPD extends beyond the cost of medication. It may also include the cost of hospitalization, the cost of missed work, and loss of gainful employment related to functional limitations. Furthermore, economic reality may keep patients from seeking interventions—such as pulmonary rehabilitation or even routine appointments—that require time commitments during work hours. Patients who may derive benefit from these interventions long-term might not be able to afford the short-term sacrifice of taking time off, which in turn may harm their long-term prospects for continued employment.
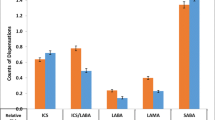
The most obvious source of personal economic burden for patients with COPD is the direct cost of medications. As discussed, patients with lower SES experience a higher symptom burden and higher rate of lung decline than similarly matched higher-income patients. Thirty-one percent of Medicare patients with COPD and asthma reported non-adherence to prescribed inhalers due to cost [43]. GoodRx (www.goodrx.com), a widely used website for comparing drug pricing in the USA, lists the direct monthly retail cost of albuterol or ipratropium near $50. Generic fluticasone/salmeterol costs about $137 directly, and brand name combination inhalers may cost between $300 and 400. Prices of inhalers (and cost directly to patients) have increased significantly since the 2006 US federal ban on chlorofluorocarbon, which was used cheaply for generic inhalers [44]. The high cost of COPD medications significantly impacts those with more limited resources.
Even patients who have health insurance, including Medicare and Medicaid, may be burdened by high levels of cost sharing through co-pays or gaps in drug coverage. Low-income persons with Medicare coverage are disproportionately more impacted by high out-of-pocket costs than their higher-income counterparts despite efforts to lower costs through Medicaid coverage, subsidies, and vouchers [45]. One study found that even a monthly out-of-pocket cost of less than 100 dollars per month resulted in substantial cost-related medication non-adherence among Medicare Beneficiaries. Unfortunately, this effort to curb personal costs can lead to higher symptom burden. Beyond inhaler costs, some COPD patients also incur the cost of chronic oxygen use, the direct cost of which can reach into the thousands of dollars.
The per-person healthcare costs including direct costs to the patient only increase with the comorbidity burden. It is well established that patients with COPD are at high risk for cardiovascular and circulatory disorders, malignancy, coagulopathy, and depression both because of epidemiological factors and because of shared pathobiology such as a chronic inflammatory state [46]. The Agency for Healthcare Research and Quality finds that for patients with no chronic healthcare conditions, out-of-pocket spending is less than $300 per year. For each additional comorbidity, the annual cost to patients increases by about $200–300 per condition such that the annual out-of-pocket healthcare spending for a person with five chronic healthcare conditions (for example, a patient with COPD along with hypertension, coronary disease, atrial fibrillation, and diabetes) is about $1600 [47]. COPD patients incur significantly more direct costs than those without COPD but with an otherwise similar comorbidity profile [48].
The personal economic burden of COPD extends beyond the direct costs of hospitalization, outpatient visits, medications, and other therapies. Patients with COPD also have more absenteeism hours and more time spent on short-term disability than those without COPD, which is especially pronounced among frequent exacerbators. The indirect costs of this missed work add up to about $7000 per patient per year [48]. These costs were studied in patients who are eligible for short-term disability, which may not be the case for workers who fall below a certain earning threshold or depend upon contracted work. For patients who work hourly jobs, who are the sole earners for their family, or who are undocumented and unprotected, the indirect costs of missing work are likely even higher relative to earnings. For women, who earn 70–80% the hourly wage of men—and for women of color for whom this discrepancy is even more pronounced [49]—the impact of these indirect costs of COPD is greater.
Since many low SES patients with COPD have a history of occupational exposures, their employment possibilities may be limited after diagnosis. For example, agricultural workers may find their COPD symptoms are exacerbated by dust or other environmental exposures, limiting their ability to work. Patients who find themselves temporarily or permanently disabled by their COPD might find that they are no longer able to work in industries that require heavy lifting or other physical labor because of dyspnea. This is especially burdensome for those patients with low educational achievement or little vocational training for whom changing fields is difficult.
While not in mainstream practice to date, new technologies to monitor patient symptoms, educate, and potentially intervene offer promise to improve outcomes. Their effects will likely not be applied equally though, as patients with low SES, more advanced age, and worse overall health are less likely to use communication technologies and performed more poorly on simulated electronic health tasks [50].
Outcomes
SES, sex, and ethnicity influence patient-focused outcomes (dyspnea, exacerbation frequency) and mortality. Low SES is associated with more exacerbations, less access to care, worse symptom burden, and lower FEV1 [36, 38, 51]. Although white patients have a higher prevalence and mortality of COPD, black patients experience higher hospitalization rates, worse COPD-related quality of life, and their mortality is not declining at the same rate as white patients [36, 38, 52, 53]. Women are more than three times as likely than men to have severe disease at time of diagnosis [54]. Women also have higher reported dyspnea when controlled for FEV1 despite less tobacco exposure and lower age [34].
Mortality
The impact of the aforementioned disparities is most clearly and poignantly seen in mortality. While age-adjusted mortality rates for men declined between 1999 and 2014, there was no change for women [5, 55]. More recent US estimates demonstrate mortality has decreased in American Indians, Asian/Pacific islanders, and Hispanics, but not in African-Americans [55]. A longitudinal, population-based study of Canadian administrative data demonstrated while overall mortality rates declined between 1996 and 2011, the difference between the lowest and highest socioeconomic quintiles increased by 28% [51]. This population of Canadians had access to universal healthcare insurance; health disparity by wealth is likely more pronounced in other health systems that do not provide robust coverage for the poor. These data illustrate the direct and quantifiable but uneven gains in COPD treatment.
Health-Related Quality of Life
It is well recognized that COPD is associated with poor health-related quality of life (HRQOL), though this is disproportionately represented in low SES groups, racial and ethnic minorities, and women [56]. HRQOL is inherently complex to define. In COPD, exacerbation frequency, depression/anxiety, symptom burden, and social isolation are considered major determinants. In a recent assessment of the COPDGene cohort, which stratified subjects by income, those with lower income were more likely to have severe exacerbations, chronic bronchitis symptoms, and lower HRQOL [7]. In a cross-sectional Spanish study of outpatients with COPD, women were more likely to have exacerbations and a higher symptom burden than men, regardless of the degree of airflow obstruction [57].
In research settings, HRQOL in COPD is usually assessed by the St. George’s Respiratory Questionnaire, though there is evidence that this metric does not adequately capture depression [58] and impaired peripheral oxygen consumption [59], two of the main drivers of poor HRQOL. Several other screening tools have variable specificity for determinants of HRQOL, and the best combination of screening tools to elicit the exact cause of poor HRQOL is not yet known [60]. There has been considerable interest in assessing genetic pathways involved in depression and anxiety in COPD, though this is not yet a viable approach [61].
There is conflicting data on the treatment effects of factors related to poor HRQOL in disadvantaged groups. As an example, pulmonary rehabilitation programs are known to help COPD patients regardless of SES status [62] or sex [63]. In fact, it is possible that women in particular may benefit from pulmonary rehabilitation more than men due to increased loss of quadriceps muscle fibers and strength given the same degree of airflow obstruction as men [64]. Counter to this, a recent randomized trial assessed the effectiveness of an intensive transition program to assist patients admitted with COPD exacerbations return home with education and nursing evaluations [65]. The study found an unexpected increase in recurrent exacerbations in the intervention arm, which was disproportionately seen in lower SES groups.
Conclusions
COPD remains a prevalent, serious disease that suffers from variable diagnostic criteria, diagnostic bias, imperfectly understood risk factors, and unevenly distributed care. Consequently, SES, ethnic minorities, rural communities, and women suffer disproportionately with this disease. The reasons for this are sometimes clear (e.g., poor access to healthcare, higher smoking rates) and sometimes less clear (e.g., women’s biologic response to smoking that leads to more airway and alveolar damage). Despite a large impact on the US population both in terms of prevalence and morbidity/mortality, research for COPD has traditionally received appreciably less funding when compared to cancer, heart disease, and other diseases [66]. More recently, there has been a concerted approach to improve research and implementing strategies to improve COPD care. Internationally (e.g., World Health Organization’s diagnosis and prevalence studies), nationally (e.g., National Institute of Health’s National Action Plan), and locally (e.g., California’s Tobacco Related Disease Research Program) have supported researchers and clinicians alike to improve the health of COPD patients. Further efforts to improve the health of patients with COPD should consider social, economic, geographic, and gender disparities and assure that interventions to be evenly applied.
Key References
-
Pivotal publication on gender bias influencing COPD diagnosis [35].
-
Superb review on the effects of gender in COPD pathogenesis, diagnosis, and treatment [34].
-
A granular epidemiologic report on COPD and socioeconomic determinants [14].
-
A recent study on the impact of socioeconomic status on COPD [7].
-
A recent epidemiologic study on air pollution and lung function/COPD [13].
-
A study demonstrating the association between rural communities and higher COPD exacerbation rates [16].
-
An argument for changing the criteria for COPD diagnosis to include imaging evidence of emphysema [22].
-
An analysis of the BOLD data showing issues with both over and under-diagnosis [23].
-
A superb review/editorial about the future challenges of clinical COPD care [36].
-
A discussion of the social factors that influence pulmonary rehabilitation completion [40].
-
Self-management and transition care for COPD exacerbations [65].
-
Analysis of the COPDGene data showing gender and race differences in COPD diagnosis [25]
-
Superb review of over and under-diagnosis of COPD [19].
-
Review of the health disparities in respiratory diseases relating to management [37]
References
Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet. 2007 Sep 1;370(9589):741–50.
Ward BW, Nugent CN, Blumberg SJ, Vahratian A. Measuring the prevalence of diagnosed chronic obstructive pulmonary disease in the United States using data from the 2012-2014 National Health Interview Survey. Public Health Rep. SAGE PublicationsSage CA: Los Angeles, CA; 2017 Mar;132(2):149–156.
Jenkins C, Chapman K, Donohue J, Roche N, Tsiligianni I, Han M. Improving the management of COPD in women. Chest. Elsevier Inc; 2017 Mar 1;151(3):686–696.
Sullivan J, Pravosud V, Mannino DM, Siegel K, Choate R, Sullivan T. National and state estimates of COPD morbidity and mortality — United States, 2014-2015. Chronic Obstructive Pulmonary Diseases: Journal of the COPD Foundation. 2018;5(4):324–33.
Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance--United States, 1999-2011. Chest. 2013 Jul;144(1):284–305.
GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017 Sep;5(9):691–706.
Lowe KE, Crapo JD, Kinney GL, Hokanson JE, Kim V, Iyer AS, et al. Association of low income with pulmonary disease progression in smokers with and without chronic obstructive pulmonary disease. 2018 Nov 7;:1–11.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014.
Reid JL, Hammond D, Boudreau C, Fong GT, Siahpush M, ITC Collaboration. Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res. 2010 Oct;12 Suppl(Supplement 1):S20–33.
Levy JI, Quirós-Alcalá L, Fabian MP, Basra K, Hansel NN. Established and emerging environmental contributors to disparities in asthma and chronic obstructive pulmonary disease. Curr Epidemiol Rep. 2018 May 25;5(2):114–24.
Syamlal G, Doney BC, Mazurek J. Chronic obstructive pulmonary disease prevalence among adults who have never smoked, by industry and occupation — United States, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019 Apr 3;:1–5.
Predictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary disease. American Thoracic SocietyNew York, NY; 1999 Jan;159(1):158–64.
Doiron D, de Hoogh K, Probst-Hensch N, Fortier I, Cai Y, De Matteis S, et al. Air pollution, lung function and COPD: results from the population-based UK Biobank study. Eur Respir J. European Respiratory Society. 2019 Jul;54(1):1802140.
Croft JB, Wheaton AG, Liu Y, Xu F, Lu H, Matthews KA, Cunningham TJ, Wang Y, Holt JB. Urban-rural county and state differences in chronic obstructive pulmonary disease - United States, 2015. MMWR Morb Mortal Wkly Rep. 2018 Feb 23;67(7):205–11.
Abrams TE, Vaughn-Sarrazin M, Fan V, Kabouli P. Geographic isolation and risk for COPD-related mortality. Ann Intern Med. 2011 Jun 29;155:80–6.
Burkes RM, Gassett AJ, Ceppe AS, Anderson W, O’Neal WK, Woodruff PG, Krishnan JA, Barr RG, Han MLK, Martinez FJ, Comellas AP, Lambert AA, Kaufman JD, Dransfield MT, Wells JM, Kanner RE, Paine R III, Bleecker ER, Paulin LM, Hansel NN, Drummond MB, Alexis NE, Anderson WH, Barr RG, Bleecker ER, Boucher RC, Bowler RP, Carretta EE, Christenson SA, Comellas AP, Cooper CB, Couper DJ, Criner GJ, Crystal RG, Curtis JL, Doerschuk CM, Dransfield MT, Freeman CM, Han MLK, Hansel NN, Hastie AT, Hoffman EA, Kaner RJ, Kanner RE, Kleerup EC, Krishnan JA, LaVange LM, Lazarus SC, Martinez FJ, Meyers DA, Moore WC, Newell JD, Paulin L, Peters S, Oelsner EC, O’Neal WK, Ortega VE, Paine R, Putcha N, Rennard SI, Tashkin DP, Scholand MB, Wells JM, Wise RA, Woodruff PG, Postow L, Croxton T. Rural residence and chronic obstructive pulmonary disease exacerbations. Analysis of the SPIROMICS cohort. Annals of the American Thoracic Society. 2018 Jul;15(7):808–16.
Schikowski T, Mills IC, Anderson HR, Cohen A, Hansell A, Kauffmann F, Kramer U, Marcon A, Perez L, Sunyer J, Probst-Hensch N, Kunzli N. Ambient air pollution: a cause of COPD? Eur Respir J. European Respiratory Society. 2014 Jan;43(1):250–63.
Hajat A, Hsia C, O’Neill MS. Socioeconomic disparities and air pollution exposure: a global review. Curr Envir Health Rpt. 2015 Sep 18;2(4):440–50.
Diab N, Gershon AS, Sin DD, Tan WC, Bourbeau J, Boulet L-P, Aaron SD. Underdiagnosis and overdiagnosis of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018 Nov;198(9):1130–9.
Larsson K, Janson C, Ställberg B, Lisspers K, Olsson P, Kostikas K, Gruenberger JB, Gutzwiller FS, Uhde M, Jorgensen L, Johansson G. Impact of COPD diagnosis timing on clinical and economic outcomes: the ARCTIC observational cohort study. Int J Chron Obstruct Pulmon Dis. Dove Press. 2019;14:995–1008.
Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2020 REPORT. 2019 Nov 14;:1–141.
Lowe KE, Regan EA, Anzueto A, Austin E, Austin JHM, Beaty TH, Benos PV, Benway CJ, Bhatt SP, Bleecker ER, Bodduluri S, Bon J, Boriek AM, Boueiz AR, Bowler RP, Budoff M, Casaburi R, Castaldi PJ, Charbonnier JP, Cho MH, Comellas A, Conrad D, Costa Davis C, Criner GJ, Curran-Everett D, Curtis JL, DeMeo D, Diaz AA, Dransfield MT, Dy JG, Fawzy A, Fleming M, Flenaugh EL, Foreman MG, Fortis S, Gebrekristos H, Grant S, Grenier PA, Gu T, Gupta A, Han MK, Hanania NA, Hansel NN, Hayden LP, Hersh CP, Hobbs BD, Hoffman EA, Hogg JC, Hokanson JE, Hoth KF, Hsiao A, Humphries S, Jacobs K, Jacobson FL, Kazerooni EA, Kim V, Kim WJ, Kinney GL, Koegler H, Lutz SM, Lynch DA, MacIntye NR Jr, Make BJ, Marchetti N, Martinez FJ, Maselli DJ, Mathews AM, McCormack M, McDonald M, McEvoy C, Moll M, Molye SS, Murray S, Nath H, Newell JD Jr, Occhipinti M, Paoletti M, Parekh T, Pistolesi M, Pratte KA, Putcha N, Ragland M, Reinhardt JM, Rennard SI, Rosiello RA, Ross JC, Rossiter HB, Ruczinski I, San Jose Estepar R, Sciurba FC, Sieren JC, Singh H, Soler X, Steiner RM, Strand MJ, Stringer WW, Tal-Singer R, Thomashow B, Vegas Sánchez-Ferrero G, Walsh JW, Wan ES, Washko GR, Michael Wells J, Wendt CH, Westney G, Wilson A, Wise RA, Yen A, Young K, Yun J, Silverman EK, Crapo JD. COPDGene® 2019: redefining the diagnosis of chronic obstructive pulmonary disease. Chronic Obstr Pulm Dis. 2019 Nov;6(5):384–99.
Sator L, Horner A, Studnicka M, Lamprecht B, Kaiser B, McBurnie MA, et al. Overdiagnosis of COPD in subjects with unobstructed spirometry: a BOLD analysis. Chest. 2019 Aug;156(2):277–88.
Ghattas C, Dai A, Gemmel DJ, Awad MH. Over diagnosis of chronic obstructive pulmonary disease in an underserved patient population. Int J Chron Obstruct Pulmon Dis. Dove Press; 2013;8:545–549.
Mamary AJ, Stewart JI, Kinney GL, Hokanson JE, Shenoy K, Dransfield MT, Foreman MG, Vance GB, Criner GJ, COPDGene® Investigators. Race and gender disparities are evident in COPD underdiagnoses across all severities of measured airflow obstruction. Chronic Obstr Pulm Dis. 2018 Jul 2;5(3):177–84.
Lamprecht B, Schirnhofer L, Kaiser B, Buist SA, Mannino DM, Studnicka M. Subjects with discordant airways obstruction: lost between spirometric definitions of COPD. Pulm Med Hindawi. 2011;2011(1):780215–6.
Bhatt SP, Balte PP, Schwartz JE, Cassano PA, Couper D, Jacobs DR, et al. Discriminative accuracy of FEV1:FVC thresholds for COPD-related hospitalization and mortality. JAMA. 2019 Jun 25;321(24):2438–47.
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, Enright PL, Hankinson JL, Ip MSM, Zheng J, Stocks J, the ERS Global Lung Function Initiative. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012 Dec 1;40(6):1324–43.
Lamprecht B, Soriano JB, Studnicka M, Kaiser B, Vanfleteren LE, Gnatiuc L, Burney P, Miravitlles M, García-Rio F, Akbari K, Ancochea J, Menezes AM, Perez-Padilla R, Montes de Oca M, Torres-Duque CA, Caballero A, González-García M, Buist S, BOLD Collaborative Research Group, the EPI-SCAN Team, the PLATINO Team, and the PREPOCOL Study Group. Determinants of underdiagnosis of COPD in national and international surveys. Chest. 2015 Oct;148(4):971–85.
Hardin M, Cho M, McDonald ML, Beaty T, Ramsdell J, Bhatt S, et al. The clinical and genetic features of COPD-asthma overlap syndrome. Eur Respir J. 2014 Jul 31;44(2):341–50.
Pleasants RA, Rivera MP, Tilley SL, Bhatt SP. Both duration and pack-years of tobacco smoking should be used for clinical practice and research. Annals of the American Thoracic Society. 2020 Jul;17(7):804–6.
Benowitz NL, Dains KM, Dempsey D, Wilson M, Jacob P. Racial differences in the relationship between number of cigarettes smoked and nicotine and carcinogen exposure. Nicotine Tob Res. 2011 Sep 7;13(9):772–83.
Gilkes A, Hull S, Durbaba S, Schofield P, Ashworth M, Mathur R, et al. Ethnic differences in smoking intensity and COPD risk: an observational study in primary care. NPJ Prim Care Respir Med. Springer US; 2017 Aug 28;:1–6.
Han MK, Postma D, Mannino DM, Giardino ND, Buist S, Curtis JL, et al. Gender and chronic obstructive pulmonary disease: why it matters. Am J Respir Crit Care Med. 2007 Dec 15;176(12):1179–84.
Chapman KR, Tashkin DP, Pye DJ. Gender bias in the diagnosis of COPD. Chest. 2001 Jun;119(6):1691–5.
Criner RN, Han MK. COPD care in the 21st century: a public health priority. Respir Care. 2018 Apr 26;63(5):591–600.
Beran D, Zar HJ, Perrin C, Menezes AM, Burney P. Forum of international respiratory societies working group collaboration. Burden of asthma and chronic obstructive pulmonary disease and access to essential medicines in low-income and middle-income countries. Lancet Respir Med. 2015 Feb;3(2):159–70.
Pleasants R, Riley I, Mannino D. Defining and targeting health disparities in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2016;11:2475–96.
Patel MR, Press VG, Gerald LB, Barnes T, Blake K, Brown LK, et al. Improving the affordability of prescription medications for people with chronic respiratory disease. An Official American Thoracic Society Policy Statement. American Thoracic Society; 2018. pp. 1367–74.
Oates GR, Hamby BW, Stepanikova I, Knight SJ, Bhatt SP, Hitchcock J, Schumann C, Dransfield MT. Social determinants of adherence to pulmonary rehabilitation for chronic obstructive pulmonary disease. COPD: J Chron Obstruct Pulmon Dis. 2017 Nov 3;14(6):610–7.
Blanc PD, Eisner MD, Yelin EH, Earnest G, Balmes JR, Gregorich SE, Katz PP. Socioeconomic gradients in tiotropium use among adults with COPD. International Journal of COPD. Dove Press. 2008;3(3):483–90.
Gerald LB, Berry CE. Health disparities. In: Gerald LB, Berry CE, editors. Respiratory medicine. Cham: Humana Press; 2015. 1 p.
Castaldi PJ, Rogers WH, Safran DG, Wilson IB. Inhaler costs and medication nonadherence among seniors with chronic pulmonary disease. Chest. 2010 Sep;138(3):614–20.
Jena AB, Ho O, Goldman DP, Karaca-Mandic P. The impact of the US Food and Drug Administration chlorofluorocarbon ban on out-of-pocket costs and use of albuterol inhalers among individuals with asthma. JAMA Intern Med. 2015 Jul 1;175(7):1171–9.
Schoen C, Davis K, Willink A. Medicare beneficiaries’ high out-of-pocket costs: cost burdens by income and health status. Issue Brief (Commonw Fund). 2017 May;11:1–14.
Tzanakis N, Hillas G, Perlikos F, Tsiligianni I. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015 Jan;:95–15.
Agency for Healthcare Research and Quality. Multiple chronic conditions chartbook. 2014 Apr 7;:1–52.
Patel JG, Coutinho AD, Lunacsek OE, Dalal AA. COPD affects worker productivity and health care costs. Int J Chron Obstruct Pulmon Dis Dove Press. 2018;13:2301–11.
STATISTICS USBOL. Highlights of women’s earnings in 2018 [Internet]. US Bureau of Labor statistics. 2018 pp. 1–142. Available from: https://www.bls.gov/opub/reports/womens-earnings/2018/home.htm
Witry M, Comellas A, Simmering J, Polgreen P. The association between technology use and health status in a chronic obstructive pulmonary disease cohort: multi-method study. J Med Internet Res. 2018;20(4):e125–8.
Gershon AS, Hwee J, Victor JC, Wilton AS, To T. Trends in socioeconomic status–related differences in mortality among people with chronic obstructive pulmonary disease. Annals of the American Thoracic Society. 2014 Oct;11(8):1195–202.
Han MK, Curran-Everett D, Dransfield MT, Criner GJ, Zhang L, Murphy JR, Hansel NN, DeMeo D, Hanania NA, Regan EA, Make BJ, Martinez FJ, Westney GE, Foreman MG, COPDGene Investigators. Racial differences in quality of life in patients with COPD. Chest. 2011 Nov;140(5):1169–76.
Ejike CO, Dransfield MT, Hansel NN, Putcha N, Raju S, Martinez CH, Han MLK. Chronic obstructive pulmonary disease in America’s black population. Am J Respir Crit Care Med. 2019 Aug 15;200(4):423–30.
Foreman MG, Zhang L, Murphy J, Hansel NN, Make B, Hokanson JE, et al. Early-onset chronic obstructive pulmonary disease is associated with female sex, maternal factors, and African American race in the COPDGene Study. Am J Respir Crit Care Med. American Thoracic Society; 2011 Aug 15;184(4):414–20.
CDC. Age-standardized death rate (Per 100,000 population) for chronic obstructive pulmonary disease (COPD) by state, United States, 2014. 2016 Aug 10;:1–1.
Kamil F, Pinzon I, Foreman MG. Sex and race factors in early-onset COPD. Curr Opin Pulm Med. 2013 Mar;19(2):140–4.
Trigueros JA, Riesco JA, Alcázar-Navarrete B, Campuzano A, Pérez J. Clinical features of women with COPD: sex differences in a cross-sectional study in Spain (“the ESPIRAL-ES study”). Int J Chron Obstruct Pulmon Dis. 2019;14:2469–78.
Orlandi L de CL, Pinho JF, Murad MGR, Rocha FL, Rodrigues-Machado MG. Depression diagnosed by the mini international neuropsychiatric interview plus (MINI) in patients with chronic obstructive pulmonary disease: relationship with functional capacity and quality of life. BMC Res Notes. BioMed Central; 2016 Feb 4;9(1):65–11.
Broxterman RM, Hoff J, Wagner PD, Richardson RS. Determinants of the diminished exercise capacity in patients with chronic obstructive pulmonary disease: looking beyond the lungs. J Physiol (Lond). 2019 Dec 19;:JP279135.
Szentes BL, Schwarzkopf L, Kirsch F, Schramm A, Leidl R. Measuring quality of life in COPD patients: comparing disease-specific supplements to the EQ-5D-5L. Expert Rev Pharmacoecon Outcomes Res. Taylor & Francis; 2019 Sep 12;10(6):1–7.
Heinzman JT, Hoth KF, Cho MH, Sakornsakolpat P, Regan EA, Make BJ, Kinney GL, Wamboldt FS, Holm KE, Bormann N, Robles J, Kim V, Iyer AS, Silverman EK, Crapo JD, Han S, Potash JB, Shinozaki G, COPDGene Investigators. GWAS and systems biology analysis of depressive symptoms among smokers from the COPDGene cohort. J Affect Disord. 2019 Jan 15;243:16–22.
Grosbois J-M, Heluain-Robiquet J, Machuron F, Terce G, Chenivesse C, Wallaert B, et al. Influence of socioeconomic deprivation on short- and long-term outcomes of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. Dove Press; 2019;14:2441–2449.
Nguyen L-P, Beck E, Cayetano K, Li C-S, Hardin K. Differential pulmonary rehabilitation outcomes in patients with and without COPD: role of gender. Journal of Cardiopulmonary Rehabilitation and Prevention. 2017 Sep;37(5):350–5.
Ausín P, Martínez-Llorens J, Sabaté-Bresco M, Casadevall C, Barreiro E, Gea J. Sex differences in function and structure of the quadriceps muscle in chronic obstructive pulmonary disease patients. Chron Respir Dis. SAGE PublicationsSage UK: London, England; 2017 May;14(2):127–139.
Aboumatar H, Naqibuddin M, Chung S, Chaudhry H, Kim SW, Saunders J, Bone L, Gurses AP, Knowlton A, Pronovost P, Putcha N, Rand C, Roter D, Sylvester C, Thompson C, Wolff JL, Hibbard J, Wise RA. Effect of a hospital-initiated program combining transitional care and long-term self-management support on outcomes of patients hospitalized with chronic obstructive pulmonary disease: a randomized clinical trial. JAMA. American Medical Association. 2019 Oct 8;322(14):1371–80.
Gillum LA, Gouveia C, Dorsey ER, Pletcher M, Mathers CD, McCulloch CE, et al. NIH disease funding levels and burden of disease. Ross J, editor. PLoS ONE. Public Library of Science; 2011 Feb 24;6(2):e16837.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on COPD and Asthma
Rights and permissions
About this article
Cite this article
Kuhn, B.T., Wick, K.D. & Schivo, M. An Update in Health Disparities in COPD in the USA. Curr Pulmonol Rep 10, 14–21 (2021). https://doi.org/10.1007/s13665-021-00268-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-021-00268-0