Abstract
Purpose of Review
Since the identification of multiple mutations associated with advanced non-small cell lung cancer (NSCLC), many targeted therapies have been developed for the treatment of this subgroup of lung cancers. These targeted therapies have changed the landscape of lung cancer treatment when compared to standard chemotherapy, with improved survival and quality of life. In this review article, we will review the major mutations associated with advanced NSCLC, namely EGFR, ALK, and ROS1. We will discuss their discovery, their clinical significance, and the diagnostic tests used for their detection. We will also review the respective targeted therapies developed, and the clinical trials that led to their approval.
Recent Findings
We will also review the most recent advances in targeted therapies in the treatment of advanced NSCLC, including recent data on tyrosine kinase inhibitor osimertinib showing equal effectiveness to other first-line therapy and accordingly recommended in first line for EGFR-positive advanced NSCLC. We will discuss emerging targetable mutations such as HER2, RET, and MET.
Summary
Targeted therapies will likely shape the future of NSCLC treatment. They have been shown to provide survival advantage over chemotherapy, while providing better quality of life through ease of administration (most are oral drugs), as well as tolerability and better toxicity profile. Further elucidation of these and mutations may provide for future more effective targeted therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction and Background
The incidence of lung cancer has been on the rise in the USA and worldwide. It is the second most common cancer in the USA, second only to prostate cancer in men and to breast cancer in women. It remains, however, the leading cause of mortality with an estimated 1 in 4 cancer deaths attributed to lung cancer. The mean age of lung cancer at diagnosis is 70 years with an increased prevalence an African-American males. The American Cancer Society estimates that 234,000 new cases of lung cancer will be diagnosed in 2018 (Fig. 1) constituting 14% of all new cancer diagnoses. Since the 1990s, there has been a decrease in lung cancer incidence, and that has been attributed to improving smoking habits and to smoking cessation. Multiple risk factors have been associated with lung cancer; however, smoking is by far the most implicated, with 80% of lung cancers associated with smoking. Other risk factors implicated include radon exposure, heavy metal, asbestos, and air pollution [1].
Types of Lung Cancer
There are 2 major types of lung cancer. Non-small cell lung cancer (NSCLC), the focus of this paper, makes up more than 85% of lung cancers. The other major type is small cell lung cancer (SCLC) which accounts for 15% of all cases. In the USA, the most common histology in NSCLC is adenocarcinoma followed by squamous cell carcinoma and less commonly large cell carcinoma. Historically, these different histologies have been grouped together because their staging and treatment used to be similar. However, there has been a recent change in the way we subtype, stage, prognosticate, and treat these subtypes.
The World Health Organization (WHO) reclassified lung cancer in 2015 with a new emphasis on genetic studies and the integration of molecular testing for histologic subtyping [] (Table 1). New entities were added based entirely on genetic profiling. The new classification proposed a completely different approach to lung adenocarcinoma than the 2011 International Association for the Study of Lung Cancer (ASLC), American Thoracic Society (ATS), and European Respiratory Society (ERS) Classification. Major changes in terms of pre-invasive lesions include replacing the term bronchioalveolar carcinoma (BAC) with “Adenocarcinoma in Situ”, and a new category “Minimally Invasive Adenocarcinoma” was defined. The term “predominant” was discontinued for the major adenocarcinoma subtype. As invasive lung adenocarcinomas are frequently composed of heterogeneous mixtures of patterns, a new system was introduced to allow for more comprehensive estimation of both predominant and minor components. According to the new system, tumors are classified according to the predominant subtype after evaluation of the tumor using comprehensive histologic subtyping to make a semi-quantitative estimate of all of the different histologic patterns present in 5% increments. The subtypes of clear cell and signet ring adenocarcinoma were discontinued, as was mucinous cystadenocarcinoma. The WHO classification is used for histologic subtyping of primary NSCLC in the AJCC 8th edition Staging Manual which went into effect in January 2018.
Historical Survival in Stage IV
Survival in non-small cell lung cancer has remained abysmal. For all stages, the 5-year overall survival is estimated at 15% [3]. The following is the estimated 5-year survival by stage [4]. The 5-year survival rate for people with stage IA1 NSCLC is about 92%. For people with stage IA2 NSCLC, the 5-year survival rate is about 83%. For people with stage IA3 NSCLC, the 5-year survival rate is about 77% [4]. The 5-year survival rate for people with stage IB NSCLC is about 68% [4].
For stage IIA cancer, the 5-year survival rate is about 60%. For stage IIB cancer, the survival rate is about 53% [4].
The 5-year survival rate for stage IIIA NSCLC is about 36%. For stage IIIB cancers, the survival rate is about 26%. For stage IIIC cancers, the survival rate is about 13% [4].
NSCLC that has spread to other parts of the body is often hard to treat. The 5-year survival rate for stage IVA NSCLC is about 10%, and for stage IVB, the 5-year survival rate is less than 1%. Still, there are often many treatment options available for people with these stages of cancer.
The 5-year survival for stage IV lung cancer has historically remained low. The use of palliative platinum-based chemotherapy in patients with advanced NSCLC has improved overall survival at 1 and 2 years; however, the 5-year survival has remained unaffected. With the advent of targeted therapy (including tyrosine kinase inhibitors TKI), the progression-free survival has improved when compared to chemotherapy, however, without a significant improvement in overall survival (OS). Multiple phase III clinical trials listed in Table 2 have failed to show improvement in OS. It is only with the recent advent of immunotherapy that a significant improvement in OS has been observed in patients with metastatic NSCLC, but is beyond the scope of our discussion.
The Discovery of EGFR Abnormalities and Setting Up the Stage for Other Targets
Major advances in our understanding of the pathogenesis and management of NSCLC have occurred over the last 20 years. The discovery of the biologic and therapeutic importance of alterations in 2 genes: epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK)—both pharmacologically targetable tyrosine kinases—has transformed oncologic management of pulmonary adenocarcinoma.
The epidermal growth factor receptor (EGFR) signaling pathway is an important pathway in regulating cell growth, survival, proliferation, and differentiation. Vanderbilt University Biochemist Dr. Stanley Cohen was awarded the Nobel Prize in Medicine for its discovery and characterization in 1986. Dysfunctions in its intracellular signaling pathways are implicated in carcinogenesis in a wide range of cancers including the breast, brain, gastrointestinal tract, and head and neck cancer.
The first randomized clinical trial targeting EGFR in lung cancer, the 2009 Iressa Pan-Asia Study (IPASS), showed that initial treatment with an EGFR tyrosine kinase inhibitor was superior to standard platinum-based therapy in patients with advanced NSCLC and an activating EGFR mutation [5]. In this study, patients whose tumors contained an activating EGFR mutation and who received gefitinib had a significantly longer progression-free survival than those receiving carboplatin-paclitaxel [5]. Subsequently, additional randomized controlled trials confirmed the association between activating EGFR mutations and responsiveness to gefitinib and/or erlotinib therapy.
In 2013, a molecular testing consensus statement was issued by the College of American Pathologists, International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. Their consensus paper “Molecular Testing Guideline for Selection of Lung Cancer Patients for EGFR and ALK Tyrosine Kinase Inhibitors” established the first evidence-based recommendations for molecular testing of patients with advanced-stage adenocarcinoma for EGFR and ALK and importantly addressed practical issues such as which patients, which samples, and when and how testing should be performed [6]. The most recent update to this Guideline was published in January 2018 and included endorsement from the American Society of Clinical Oncology (ASCO). The Guideline reaffirms that physicians should use molecular testing for genetic targets on either primary or metastatic lung lesions to guide initial therapy selection. ASCO additionally endorsed the recommendation that molecular biomarker testing should be performed in tumors with an adenocarcinoma component or non-squamous non-small cell histology. Priority molecular testing recommendations include EGFR mutation testing by any validated EGFR testing method with sufficient performance characteristics with the stipulation that immunohistochemistry and EGFR copy number analysis are not recommended testing methods; ALK rearrangement testing by immunohistochemistry or FISH assay; ROS1 testing by immunohistochemistry as an initial screening test to be confirmed by a molecular or cytogenetic method; and BRAF testing on all patients irrespective of clinical characteristics. Additional molecular testing as part of larger testing panels should include RET, HER2, KRAS, and MET, none of which should be performed as routine stand-alone assays. Most large medical centers perform multiplex testing using a sequencing-based system that includes EGFR, KRAS, PTEN, PIK3CA, NRAS, MEK1, AKT1, BRAF, HER2, and then separate testing for ALK, ROS1, and RET rearrangements (Table 3). As per the 2013 Molecular Testing Guideline, molecular studies can be performed on formalin-fixed, paraffin-embedded (FFPE) specimens procured by surgical resection, open biopsy, endoscopy, transthoracic needle biopsy, fine-needle aspiration, or thoracentesis [6, 7•].
Impact of TKI Therapy on Outcome
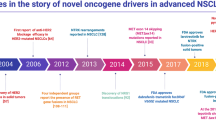
Advances in cancer research led to the identification of driver mutations in multiple cancers including non-small cell lung cancer. These are responsible for uncontrolled growth, proliferation, and acquisition of malignant characteristics of tumor cells. It is estimated that 60% of non-small cell lung cancer are a direct cause of these oncogenic driver mutations. The ongoing discovery of these complex mutations has changed our understanding of oncogenesis and accordingly led to the development of targeted therapy specific for those abnormalities. Particularly in non-small cell lung cancer, these advances have led to the identification of how heterogeneous this group of patients (previously thought to be one group) with adenocarcinoma is. Accordingly, a previously common cancer is now becoming a collection of rare cancers [8, 9] (Fig. 2).
Impact of TKI on NSCLC
The first actionable mutation discovered in NSCLC is the EGFR mutation. This mutation typically leads to the constitutive activation of the tyrosine kinase domain and has become the target of multiple tyrosine kinase inhibitors (TKIs). TKIs inhibit the intracellular domain of the EGFR TK, resulting in cell cycle arrest and inhibition of angiogenesis. One of the earliest TKIs used in the treatment of EGFR mutated NSCLC was gefitinib followed by erlotinib and afatinib.
TKIs have significantly improved the outcome in this subgroup of advanced NSCLC patients. Multiple studies have shown significantly better responses and progression-free survival (PFS) to TKIs in first line, when compared to chemotherapy [10]. Accordingly, TKIs are now recommended and approved for first-line treatment of EGFR-mutated advanced NSCLC. While TKIs offer better response and PFS, they have not been shown to offer a significant overall survival advantage; The only exception is in the subgroup of patients with EGFR Del 19, where two separate studies comparing afatinib to first-line chemotherapy did show a survival advantage [11]. However, despite the lack of a survival benefit, these agents have become the standard of care, due to their improved tolerability and superior response and PFS.
EGFR
Incidence
Epidermal growth factor receptor (EGFR) mutations are frequently found in NSCLC, especially in adenocarcinoma histologic subtype. The incidence of these EGFR mutations is widely variable along racial and gender lines. It is by far most common among Asian patients with NSCLC accounting for up to 50% of patients in this population. The incidence is even highest among the subgroup of non-smoker female Asian patients. In contrast, EGRF-sensitizing mutations are only found in 10–20% of Caucasian patients with NSCLC. Geographically, Southeast Asian countries account for the highest prevalence of EGFR mutation among NSCLC patients, while the Australian continent ranks the least. Peru stands out in South America with one of the highest incidences of these EGFR mutations [12 (Fig. 3)].
These data regarding the incidence of EGFR mutations in different population should not preclude any population from testing, even the ones with the least prevalence. All patients with advanced non-squamous NSCLC, and who are candidates for systemic therapy, must have their biopsy sample tested for EGFR mutation.
Data regarding populations EGFR mutation are lacking in many parts of the world, mostly due to the lack of testing and lack of resources. EGFR mutations’ incidence is quite underreported in areas such as the African continent, the Middle-east, and Central America.
Based on the current body of literature, four defined regions in the EGFR gene are commonly mutated in NSCLC and predict sensitivity to EGFR TKIs: exons 18–21. The most frequent mutations are exon 19 deletions and the single-point substitution L858R in exon 21, which comprise 44 and 41% of all EGFR mutations, respectively [13]. Less common mutations include G719X in exon 18 (4%), and L861Q in exon 21 (2%), which are both moderately sensitive to EGFR-TKIs. Insertions in exon 20 account for an additional 4% and are known to be less sensitive to EGFR-TKIs [14, 15, 16]. These uncommon mutations currently do not have an approved drug therapy, although the strongest data available is for the use of afatinib, which has been shown to have some activity in this subgroup of patients [59]. Alterations in exon 19 are the most numerous and complex and include multiple different deletion subtypes and insertions. Studies have shown that different subtypes are associated with distinct clinical outcomes. According to the Catalogue for Somatic Mutations in Cancer (COSMIC) database for EGFR, the most frequent exon deletions include delE746-A750 (68.9%%), followed by delL747-P753insS (6.0%), delL747-T751 (4.1%), and delL747-A750insP (3.9%) [17]. Studies have shown better TKI efficacy for delE746 than delL747 suggesting that deletion location may affect drug efficacy [18].
Treatment of EGFR-Mutated Advanced NSCLC (Adenocarcinoma)
Since the discovery of EGFR mutations in lung cancer, multiple inhibitors have been developed and are referred to as tyrosine kinase inhibitors (TKI). However, to date, only four are FDA approved and in clinical use in the USA. Historically, the first of these TKIs was gefitinib which was approved by the FDA in 2003. At that time, gefitinib had gained accelerated approval for the treatment of patients with metastatic NSCLC after progression on first-line chemotherapy. This approval was not based on EGFR mutations, and accordingly, subsequent trials failed to reveal clinical benefit leading to the withdrawal of approval by the FDA. At that time, it was not known that the effectiveness of gefitinib was limited to EGFR-mutated patients. Subsequently, and based on positive clinical trials with gefitinib, the FDA reapproved the drug for use in the USA.
Because of this prior restriction on gefitinib, erlotinib, another TKI approved shortly after gefitinib, has been the most used in patients with sensitizing EGFR mutations. Afatinib, a second-generation irreversible oral TKI with a broader receptor targets, has been later FDA approved for the first-line treatment of advanced non-squamous EGFR-mutated NSCLC. More recently, osimertinib was also approved in first line and will be discussed below in further detail (Fig. 4).
First-Generation TKIs
Gefitinib and erlotinib are first-generation TKIs and are both approved in first line for the treatment of EGFR-mutated NSCLC-AC [19]. Gefitinib and erlotinib are administered orally and their mechanism of action involves binding reversibly the aberrant EGFR tyrosine kinase and thus inhibiting its signaling activity.
The re-approval of gefitinib in 2015 was based on data from IFUM (Iressa Follow-Up Measure) clinical trial [20] which showed a 50 and 70% objective response rate (ORR) by blind independent central review (BICR) and investigators, respectively, and with a duration of response of 6 and 8.3 months. The IPASS (Iressa Pan-Asia Study) further supported the approval of gefitinib. The IPASS compared gefitinib to platinum-based chemotherapy (carboplatin/paclitaxel) in first-line treatment for metastatic NSCLC. The study showed an ORR of 67% (95% CI 56, 77) with a median duration of response of 9.6 months in the gefitinib-treated arm versus 41% (95% CI 31, 51) with median duration of response of 5.5 months for the chemotherapy arm [21].
Erlotinib was initially approved by the FDA in 2004 in second-line advanced NSCLC after progression on at least one prior chemotherapy regimen. This approval was based on one randomized trial comparing erlotinib to placebo [22]. There was a statistically significant improvement in median OS of 6.7 months in the erlotinib arm compared to 4.7 in the placebo. Only one third of the patients on the trial were tested for EGFR overexpression by staining (not molecular testing) and were labeled as high or low. Retrospective analysis revealed that patients with “high level” of EGFR had much better response to erlotinib and a greater survival when compared “low level” EGFR. At that time, the exact nature of these variations in EGFR and their clinical implications were not fully understood. Erlotinib was subsequently FDA approved in 2013 for first-line treatment of patients with metastatic NSCLC whose tumor harbors an EGFR mutation. This approval was based on the results of a multicenter open-label trial comparing erlotinib to platinum-based chemotherapy in patients with metastatic and EGFR mutated NSCLC. The median progression-free survival PFS was 10.4 months in the erlotinib arm compared to 5.2 months in the platinum-based chemotherapy arm (p < 0.001). The median overall survival was 20 months in the erlotinib arm versus 19.5 months in the platinum-based chemotherapy arm and did not reach statistical significance (p = 0.6482) [23].
Second-Generation TKIs
The second-generation TKI, afatinib, binds irreversibly to tyrosine kinase domain of EGFR (ErbB1), HER2 (ErbB2), and HER4 (ErbB4), causing inhibition of ErbB signaling pathway and decreased tumor cell proliferation. It binds to both wild-type (WT) and aberrant EGFR however with higher affinity to the aberrant EGFR. The FDA-approved afatinib based on data from the LUX–Lung 3 trial comparing afatinib to pemetrexed/cisplatin chemotherapy. This trial showed that patients taking afatinib in first line had a median progression-free survival PFS of 11.1 versus 6.9 months in the chemotherapy arm (p = 0.001) [24].
Recently, a phase 2B clinical trial compared gefitinib with afatinib in first-line therapy for metastatic NSCLC (adenocarcinoma). There was a slight difference in PFS in favor of afatinib, with patients receiving afatinib having 11.0 months PFS vs. 10.9 months in patients receiving gefitinib (p = 0.017). This difference did not however have any significant clinical implications [25].
Currently, all third-generation TKIs gefitinib, erlotinib, and afatinib are approved in first line for the treatment of metastatic NSCLC-AC with EGFR-sensitizing mutations. Chemotherapy is no longer the standard of care in first line in these patients. Aside from favorable PFS with TKIs, their toxicity profile and improved tolerability led to the recommendation of their use in first line.
Third-Generation TKI
The remarkable response in EGFR-mutated metastatic non-small cell lung cancer to first- and second-generation TKIs has been limited by the emergence of resistance to therapy. Rarely, this resistance is de novo and may be present at diagnosis. In the majority of cases, however, patient acquired resistance within the first 12 months of therapy (50–60%). The most common mechanism causing this resistance is a point mutation in exon 20 of the EGFR named T790M. Other mechanisms of resistance to first- and second-generation TKIs include activation of “bypass” pathways such as the BRAF mutation or MET amplification, or a histologic switch to small cell lung cancer.
Osimertinib is a third-generation oral TKI with significant activity against EGFR-sensitizing mutations as well as the resistance mutation EGFR T790M. It has been developed and approved for patient with metastatic NSCLC with EGFR T790M after progression on first- or second-generation TKIs (gefitinib, erlotinib, or afatinib). In a phase 2 clinical trial, osimertinib has shown a response rate of 61% and PFS of 9.6 months in patients with EGFR T790M-positive NSCLC who had progressed on sensitizing EGFR therapy (gefitinib, erlotinib, or afatinib) [26]. Osimertinib was also compared to chemotherapy in patients with EGFR T790M metastatic NSCLC. Osimertinib had a significantly higher PFS when compared to platinum/pemetrexed chemotherapy (10.1 vs. 4.4 months p = 0.001) [27].
In the recent AURA study published in the Journal of Clinical Oncology, osimertinib was used (in 2 different doses, 80 and 160 mg once daily) in first line to treat 60 patients with locally advanced or metastatic EGFR mutated NSCLC. Osimertinib demonstrated significant overall response rate of 77% (95% CI, 64 to 87%) across different doses used. PFS was also robust at 20.5 months (95% CI, 15.0 to 26.1 months) across different doses. Most noticeably, there was no evidence of acquired EGFR T790M mutation in patients who progressed on osimertinib [28].
Until recently, osimertinib was mostly recommended as second-line treatment in patients with T790M mutation and after progression on prior TKI therapy. However, based on the data from the AURA study, the National Comprehensive Cancer Network (NCCN) has moved the recommendation for osimertinib to be used as first line in patients with advanced or metastatic NSCLC with sensitizing EGFR mutations. In the recently published FLAURA study, osimertinib was compared to standard TKIs (gefitinib and erlotinib) in first-line therapy. In this double-blind phase III clinical trial, osimertinib showed a superior efficacy against standard TKI based on higher PFS (18.9 months for osmertinib vs. 10.2 months for standard TKI, p < 0.001) [60••]. Osimertinib is now FDA approved in first line for all EGFR-mutated advanced NSCLC.
Anaplastic Lymphoma Kinase (ALK) and ROS1 Rearrangements
At approximately the same time that EGFR emerged as an important therapeutic target, Soda et al. reported that an inversion on chromosome arm 2p resulted in the creation of an EML4-ALK fusion gene in lung cancer. This alteration was identified in a distinct subset of patients from those harboring mutations in EGFR and suggested an alternative pathway to carcinogenesis and a potential new therapeutic target [29]. Subsequent studies revealed the prevalence of this gene fusion to be 2–7% of all NSCLS, with enrichment in adenocarcinomas in non-and light-smokers [30, 31, 32, 33]. Shortly thereafter, another gene, ROS1, was shown to be a driver of mutations in NSCLC. Early studies showed that ROS1 rearrangement occurs in approximately 1% of NSCLC patients [34, 35]. ROS1 and ALK share a high level of similarity in their tyrosine kinase domains and therefore both rearrangements show responsiveness to critozinib. However, ROS1 rearrangements rarely occur in ALK-rearranged tumors and as such define a distinct molecular subset [36, 37].
NSCLC with ALK mutations are typically adenocarcinomas occurring in non-smokers (like EGFR mutations), but tend to occur in men at a younger age (unlike EGFR mutations). The frequency of ALK rearrangements in this group of patients is as high as 30%.
The types of rearrangements in ALK are more complex than EGFR mutations and, at this point, are not used clinically to guide the specific choice of therapy. There are currently several approved agents targeting ALK, with the later generation agents being more active against tumors that are resistant to the earlier agents (Fig. 5).
ROS1 rearrangements are also found in light and/or never-smokers and are associated with adenocarcinoma in younger patients [9]. Several rearrangements have been described and include SLC34A2-ROS1, CD74-ROS1, EZR-ROS1, TPM3-ROS1, and SDC4-ROS1 [34, 38]. ROS fusions are non-overlapping with other mutations in NSCLC and are responsive to crizotinib.
Approved TKIs for the Treatments of ALK/ROS1-Mutated NSCLC
Crizotinib was one of the first TKIs to be approved for the treatment of advanced or metastatic NSCLC-carrying ALK gene rearrangements. In the PROFILE study [39••], the efficacy of crizotinib was compared with standard first-line chemotherapy (pemetrexed and platinum) in patients with advanced ALK-positive NSCLC. Crizotinib was found to be superior to chemotherapy with significantly longer progression-free survival (PFS) of 10.9 versus 7.0 months (p < 0.001). Overall response rates were also superior in the crizotinib arm at 74 versus 45% in the chemotherapy arm (p < 0.001). However, a significant survival advantage was not observed. As far as tolerability and impact on quality of life, the authors concluded “As compared with chemotherapy, Crizotinib was associated with greater reduction in lung cancer symptoms and a greater improvement in quality of life.”
Crizotinib is also effective in the ROS1-mutated metastatic NSCLC and is FDA approved for use in these patients. The approval was based on a multicenter, single-arm phase 1 study (study 1001) that included 50 patients with ROS1-positive metastatic NSCLC treated with crizotinib. The results showed an objective response rate of 66% (95% CI 51%, 79%). The median duration of response was 18.3 months (95% CI 12.7 months, not reached) [40, 41]. The safety profile of crizotinib in ROS1-positive metastatic NSCLC was favorable and similar to its use in ALK-positive metastatic NSCLC.
Ceritinib is another oral TKI approved by the FDA for the treatment of patients with ALK-positive metastatic NSCLC who have progressed or intolerant to crizotinib. The initial approval was based on ASCEND–1 phase I study showing an overall response rate of 56% to ceritinib in patients who had previously been treated with crizotinib [42]. The effectiveness of ceritinib was further ascertained in ASCEND–2 even when used in third line and after progression on crizotinib. The overall response rate was 38% and the duration of response was 9.7 months (95% CI, 7.1–11.1 months). Noticeably, responses in patients with intracranial metastases were in favor of ceritinib use, with an intracranial overall response rate of 45% (95% CI, 23.1 to 68.5%) [43].
Ceritinib was also compared to platinum-based chemotherapy as first line in patients with ALK-positive metastatic NSCLC. In a recent phase III trial, ceritinib was superior to chemotherapy and was associated with a PFS of 16.6 months (95% CI, 12.6–27.2) vs 8.1 months (95% CI, 5.8–11.1) for the chemotherapy arm [44] (Table 3).
Alectinib an oral TKI that inhibits ALK rearrangements was initially approved by the FDA for patients with ALK-positive metastatic NSCLC who progressed on crizotinib or were intolerant to it. This approval was based on a phase II clinical trial showing close to 50% overall response rate in patients previously treated with crizotinib [45]. In a phase II global study published in the JCO 2015 by Ou et al., alectinib was shown to be “highly active and well tolerated in patients with advanced crizotinib-refractory ALK-positive NCSLC.” Alectinib was noted to have significant activity in patients with CNS metastasis, with 43% of patients with baseline CNS metastasis without prior irradiation, having complete CNS response to alectinib [46].
In the most recent ALEX trial, alectinic was compared to crizotinib in first-line treatment for ALK-positive metastatic NSCLC. Progression-free survival was significantly higher in the alectinib arm at 68.4 vs. 48.7% in the crizotinib arm. Patients receiving alectinic had less CNS progression at 12 vs. 45% with crizotinib [47]. Based on this trial, the National Comprehensive Cancer Network (NCCN) updated their recommendations for alectinib as the preferred first-line therapy for ALK-positive metastatic NSCLC. Alectinib does not have any activity against ROS1.
Brigatinib is another oral TKI that inhibits ALK rearrangements and was approved by the FDA for patients with ALK-positive metastatic NSCLC who progressed on crizotinib or were intolerant to it. The approval was based on the ALTA phase II trial in which two different doses of brigatinib were tested, 90 and 180 mg. The overall response rate was 45 vs 54%, and PFS was 9.2 vs 12.9 months respectively [48]. Brigatinib is also active in patients who have developed a resistance mutation to Alectinib. Brigatinib does not have any known activity against ROS1.
Lorlatinib is an investigational next-generation TKI effective in ALK and ROS1 mutated NSCLC that have also acquired resistance to prior TKI therapies. In a recently published phase I study in T he Lancet-Oncology (December 2017), lorlatinib has shown a considerable activity in patients with advanced ALK-positive or ROS1-positive NSCLC as well as a significant ability to cross the blood-brain barrier [49]. Lorlatinib is currently being investigated in a phase III randomized controlled trial comparing lorlatinib to crizotinib.
Although all of the currently approved ALK-TKIs inhibit tumor growth in ALK-rearranged tumors, tumors relapse because of acquired resistance: Alectinib has been shown to be active against crizotinib-resistant mutations such as L1196M or G1269A; Ceritinib has also been shown to be active against crizotinib-resistant mutations such as L1196M and G1269A; and Brigatinib has been shown to be active against most crizotinib-, alectinib- or certinib-resistant mutations. [61]
BRAF
BRAF mutations are found in 1–3% of patients with NSCLC [50, 51], more commonly in adenocarcinomas and in smokers (Fig. 5). BRAF mutations have been associated with more aggressive tumor behavior and poorer prognosis, including decreased PFS and OS. The most common BRAF mutation is the V600E point mutation occurring in approximately 50% of all BRAF mutations in NSCLC [51].
Types V600 Vs Others
In contrast to colon and melanoma in which the majority of BRAF mutations occur at valine 600 (V600) within exon 15, BRAF mutations in lung adenocarcinoma occur at multiple other positions within the kinase domain. One of the largest adenocarcinoma studies showed BRAF mutations present in 3% of patients with mutations spread across 3 domains including V600E(50%), G469A(39%), and D594G(11%) [51]. As per the 2018 Molecular Testing Guideline, BRAF molecular testing should be performed on all patients with advanced lung adenocarcinoma, irrespective of clinical characteristics [7•].
Dabrafenib is an oral TKI and an inhibitor of BRAF V600E mutations previously approved for metastatic melanoma. Trametinib is also an oral TKI that inhibits the BRAF V600E mutations as well as mutations involving MEK pathways. Both dabrafenib and trametinib are approved as monotherapy or as doublets for the treatment of metastatic melanoma. The combination of dabrafenib/trametinib was recently approved by the FDA for the treatment of patients with BRAF-V600E-positive metastatic NSCLC. This approval was based on phase II clinical trial, where 36 treatment-naïve patients and 57 previously treated patients received the combination dabrafenib/trametinib. The ORR was 61.1% (95% CI, 43.5–76.9) in the treatment-naïve group and 63% (95% CI, 49–76) in the previously treated population [52].
Doublet chemotherapy remains an effective treatment for BRAF-positive metastatic NSCLC because of the aggressive nature of the disease. Accordingly, The National Comprehensive Cancer Network (NCCN) recommends either combination of dabrafenib/trametinib or doublet chemotherapy in first line for the treatment or BRAF-positive metastatic NSCLC.
Emerging Targeted Therapies in NSCLC
HER2 overexpression is common in NSCLC and is found in up to 20% of biopsies of lung adenocarcinomas. Although in breast cancer and gastric cancer anti-HER2 drugs are effective all cancers that overexpress HER2, unfortunately, it is not as easily effective in NSCLC. In NSCLC, mutation of HER2 (rather than overexpression or HER2) is required for anti-HER2 drugs to be effective. Unfortunately, only 2% of NSCLC carry the HER2 mutation [53]. Multiple drugs are effective in these patients and have been or are being studied in patients with HER2-mutated NSCLC. These include trastuzumab, pertuzumab, lapatinib, and trastuzumab emanstine (also known as TDM-1). Trastuzumab has been studied the most, but is not approved yet in NSCLC.
The results of a phase II basket trial investigating TDM-1 (ado-trastuzumab) in the treatment of patients with HER2-mutated advanced NSCLC were published in JCO 2017. ORR was 33% (5/15 confirmed, 95% CI 12–62%). Further phase III trials are needed to further evaluate effectiveness [54].
RET arrangements are other evolving “druggable” targets in NSCLC. One to two percent of NSCLC are found to harbor RET rearrangements [55]. They are almost exclusively found in adenocarcinomas. Multiple drugs in development or in trials have shown activity against RET-positive NSCLC. Cabozantinib, vandetanib, and lenvatinib are multikinase inhibitors of RET shown to have activity in patients with RET rearranged NSCLC.
A recent phase II clinical trial results published in the Lancet oncology revealed activity of cabozantinib in patients with RET-rearranged lung cancer. In the single-arm trial, cabozantinib was given to patients with metastatic/advanced non-small cell lung cancer with RET rearrangements. There was a 28% overall response (95% CI, 12–49). The authors concluded that RET rearrangements in lung cancer are actionable drivers although better understanding of the tumor biology and number therapeutic approaches are needed to improve outcomes in these patients [56].
Vandetanib is another multi-kinase inhibitor with activity against RET rearranged non-small cell lung cancer. In a phase II clinical trial published in 2017, the efficacy and safety of vandetanib was evaluated. Eighteen percent of patients had a partial response with mild blood-related adverse events [55].
MET mutations are also evolving actionable mutations in non-small cell lung cancer. MET mutations in NSCLC are less common than other mutations and are seen in 5% of adenocarcinoma biopsies [57]. Multiple MET inhibitors have been studied including tivantinib, crizotinib, and onartuzumab. Results have been somewhat inconsistent. The most promising agent in this subgroup of non-small cell lung cancer has been crizotinib [58].
Discussion/Conclusion
Multiple trials have proven the effectiveness of targeted therapy in advanced and metastatic NSCLC. It is currently recommended that all patients with recurrent or advanced non-squamous NSCLC be tested for genetic mutations. Patients with an identifiable mutation should be offered the targeted therapy with a TKI. Although EGFR mutations were among the first to be discovered in NSCLC, many tyrosine kinase-targeted therapies have been developed and are proving to be effective in treating these cancers.
The discovery of ALK rearrangements has provided a broader range for targeting advanced/metastatic NSCLC. Crizotinib was the first TKI developed against ALK mutations and was approved by the FDA in 2011. This breakthrough came after a long period of time lacking progress in the treatment of metastatic NSCLC. Since then, other rearrangements and corresponding treatment have been developed including c-MET, BRAF, and RET mutation and others continue to evolve.
One of the major advantages of these TKI, especially when compared to standard chemotherapy, is their tolerability and safety profile. Along with that, their ease of administration (most are oral agents) has provided patients with a better quality of life while maintaining similar if not better effectiveness. These TKIs have become first-line standard of care in metastatic NSCLC carrying the appropriate targetable mutations.
Despite the immense progress in our understanding of NSCLC carcinogenesis, there remain significant challenges in the ongoing oncologic management of this group of patients. The rapidly growing number of mutations and targeted therapies discovered in NSCLC is adding significant complexity to the care of patients with metastatic NCSLC. The need for medical oncologists dedicated solely to the care of these patients is becoming increasingly evident. And the cost of diagnosing and treating these patients has significantly increased in recent years with more sophisticated and expensive genetic platforms required to perform molecular testing. How we overcome these challenges will have great impact not only on our ability to diagnose and treat patients with NSCLC, but equally importantly on our ability to continue to do the research necessary to identify new therapeutic targets.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major Importance
About Non-small cell lung cancer Am Cancer Soc 2018.
Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. WHO Classification of tumours of the lung, pleura, thymus and heart. Lyon: International Agency for Research on Cancer; 2015.
Heist RS, Engelman JA. SnapShot: non-small cell lung cancer. Cancer Cell. 2012;21(3):448–54.
Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WEE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39–51.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947–57.
Lindeman NI, Cagle PT, Beasley MB, Chitale DA, Dacic S, Giaccone G, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol. 2013;8:823–59.
•• Kalemkerian GP, Narula N, Kennedy EB, et al. Molecular testing guideline for the selection of patients with lung cancer for treatment with targeted tyrosine kinase inhibitors: American Society of Clinical Oncology endorsement of the College of American Pathologists/International Association for the Study of Lung Cancer/ Association for Molecular Pathology Clinical Practice Guideline Update. J Clin Oncol. 2018;36:1–9. The ASCO Expert Panel endorsed the CAP/IASLC/AMP molecular testing guideline with minor modifications.
Mitsudomi T, Suda K, Yatabe Y. Surgery for NSCLC in the era of personalized medicine. Nat Rev Clin Oncol. 2013;10(4):235–44.
Meador CB, Micheel CM, Levy MA, Lovly CM, Horn L, Warner JL, et al. Beyond histology: translating tumor genotypes into clinically effective targeted therapies. Clin Cancer Res. 2014;20(9):2264–75.
Shea M, Costa DB, Rangachari D. Management of advanced non-small cell lung cancers with known mutations or rearrangements: latest evidence and treatment approaches. Ther Adv Respir Dis. 2016;10(2):113–29.
Yang JC, Wu YL, Schuler M, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-lung 3 and LUX-lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16(2):141–51.
Midha A, Dearden S, Mc Cormack R. EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: a systematic review and global map by ethnicity (mutMapII). Am J Cancer Res. 2015;5(9):2892–911.
Gazdar AF. Activating and resistance mutations of EGFR in non-small-cell lung cancer: role in clinical response to EGFR tyrosine kinase inhibitors. Oncogene. 2009;28:S24–31.
Yasuda H, Kobayoshki s CDB. EGFR exon 20 insertion mutations in non-small-cell lung cancer: preclinical data and clinical implications. Lancet Oncol. 2012;13e23;13:e23–31.
Arrieta O, Cardona AF, Corrales L, Campos-Parra AD, Sánchez-Reyes R, Amieva-Rivera E, et al. The impact of common and rare EGFR mutations in response to EGFR-tyrosine kinase inhibitors and platinum-based chemotherapy in patients with non-small cell lung cancer. Lung Cancer. 2015;87:169–75.
Baek JH, Sun JM, Min YJ, et al. Efficiency of EGFR tyrosine kinase inhibitors in patients with EGFR-mutated non-small cell lung cancer expect both exon 19 deletion and exon 21 L858R: a retrospective analysis in Korea. Lung Cancer. 2015;87:148–54.
COSMIC database http://cancer.sanger.ac.uk/cosmic/search?q=egfr.
Chung KP, Wu SH, Wu JY, et al. Clinical outcomes in non-small cell lung cancers harboring different exon 19 deletions in EGFR. Clin Cancer Res. 2012;18:3470–7.
Non-small cell lung cancer. National Comprehensive Cancer Network NCCN Guidelines Version 1.2018.
Kazandjian D, Blumenthal GM, Yuan W, He K, Keegan P, Pazdur R. FDA approval of gefitinib for the treatment of patients with metastatic EGFR mutation–positive non–small cell lung Cancer. Clin Cancer Res. 2016;22(6):1307–12.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin–paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57.
Shepherd FA, Pereira J, Ciuleanu TE, Tan EH, Hirsh V, Thongprasert S, et al. A randomized placebo-controlled trial of erlotinib in patients with advanced non-small cell lung cancer (NSCLC) following failure of 1st line or 2nd line chemotherapy. A National Cancer Institute of Canada Clinical Trials Group (NCIC CTG) trial. J Clin Oncol. 2004;22(suppl):7022–8.
Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–46.
Yang JC, Schuler MH, Yamamoto N, et al. LUX-lung 3: a randomized, open-label, phase III study of afatinib versus pemetrexed and cisplatin as first-line treatment for patients with advanced adenocarcinoma of the lung harboring EGFR-activating mutations. J Clin Oncol. 2012;30(18_suppl):LBA7500.
Park K, Tan EH, O'Byrne K, Zhang L, Boyer M, Mok T, et al. Afatinib versus gefitinib as first-line treatment of patients with EGFR mutation-positive non-small-cell lung cancer (LUX-lung 7): a phase 2B, open-label, randomised controlled trial. Lancet Oncol. 2016;17(5):577–89.
Yang J, Ramalingam SS, Jänne PA, Cantarini M, Mitsudomi T. LBA2_PR: Osimertinib (AZD9291) in pre-treated pts with T790M-positive advanced NSCLC: updated phase 1 (P1) and pooled phase 2 (P2) results. J Thorac Oncol. 2016;11(4):S152–3.
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam SS, et al. Osimertinib or platinum–pemetrexed in EGFR T790M–positive lung cancer. N Eng J of Med. 2017;376(7):629–40.
Ramalingam SS, Yang JC, Lee CK, Kurata, et al. Osimertinib as first-line treatment of EGFR mutation–positive advanced non–small-cell lung cancer. J Clin Oncol. 2018;36(9):841–9.
Soda M, Young LC, Munehiro E, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448:561–6.
Koivunen JP, Mermel C, Zejnullahu K, et al. EML4-ALK fusion gene and efficacy of an ALK kinase inhibitor in lung cancer. Clin Cancer Res. 2008;14:4275–83.
Mano H. Non-solid oncogenes in solid tumors: EML4-ALK fusion genes in lung cancer. Cancer Sci. 2008;99:2349–55.
Perner S, Wagner PL, Demichelis F, Mehra R, LaFargue CJ, Moss BJ, et al. EML4-ALK fusion lung cancer: a rare acquired event. Neoplasia. 2008;10:298–302.
Wong DW, Leung EL, So KK, et al. The EML4-ALK fusion gene is involved in various histologic types of lung cancers from nonsmokers with wild-type EGFR and KRAS. Cancer. 2009;115:1723–33.
Bergethon K, Shaw AT, Sai-Hong IO, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012;30(8):863–70.
Gainor JF, Shaw AT. Novel targets in non-small cell lung cancer: ROS1 and RET fusions. Oncologist. 2013;18:865–75.
Birchmeier C, Birnbaum D, Waitches G, Fasano O, Wigler M. Characterization of an activated human ROS gene. Mol Cell Biol. 1986;6:3109–16.
Shaw AT, Sai-Hong IO, Yung-Jue B, et al. Crizotinib in ROS1-rearranged non-small cell lung Cancer. N Engl J Med. 2014;371:1963–71.
Takeuchi K, Soda M, Toqashi Y, et al. RET, ROS1 and ALK fusions in lung cancer. Nat Med. 2012;18(3):378–81.
•• Solomon BJ, Mok T, Kim DW, Wu YL, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371(23):2167–. This trial represented a breakthrough in NSCLC-targeted therapy involving ALK mutation after decades of limitation to EGFR directed therapy–77.
Ou SH, Bang YJ, Camidge DR, et al. Efficacy and safety of crizotinib in patients with advanced ROS1-rearranged non-small cell lung cancer (NSCLC). J Clin Oncol. 2013;31(15 Suppl):8032.
Shaw AT, Camidge DR, Engelman JA, et al. Clinical activity of crizotinib in advanced non-small cell lung cancer (NSCLC) harboring ROS1 gene rearrangement. J Clin Oncol. 2012;30(15 Suppl):7508.
Kim DW, Mehra R, Tan DS, Felip E, et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol. 2016;17(4):452–63.
Mok T, Spigel D, Felip E, et al. ASCEND-2: a single-arm, open-label, multicenter phase II study of ceritinib in adult patients (pts) with ALK-rearranged (ALK+) non-small cell lung cancer (NSCLC) previously treated with chemotherapy and crizotinib (CRZ). J Clin Oncol. 2015;33(15 Suppl):8059.
Soria JC, Tan DS, Chiari R, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet. 2017;389(10072):917–29.
Larkins E, Blumenthal GM, Chen H, He K, Agarwal R, Gieser G, et al. FDA approval: alectinib for the treatment of metastatic, ALK-positive non–small cell lung cancer following crizotinib. Clin Cancer Res. 2016;22(21):5171–6.
Ou SH, Ahn JS, De Petris L, et al. Alectinib in crizotinib-refractory ALK-rearranged non–small-cell lung cancer: a phase II global study. J Clin Oncol. 2015;34(7):661–8.
Peters S, Camidge DR, Shaw AT, Gadgeel S, Ahn JS, Kim DW, et al. Alectinib versus crizotinib in untreated ALK-positive non–small-cell lung cancer. N Engl J Med. 2017;377(9):829–38.
Kim DW, Tiseo M, Ahn MJ, et al. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase–positive non–small-cell lung cancer: a randomized, multicenter phase II trial. J Clin Oncol. 2017;35(22):2490–8.
Shaw AT, Felip E, Bauer TM, Besse B, Navarro A, Postel-Vinay S, et al. Lorlatinib in non-small-cell lung cancer with ALK or ROS1 rearrangement: an international, multicentre, open-label, single-arm first-in-man phase 1 trial. Lancet Oncol. 2017;18(12):1590–9.
Chen D, Zhang LQ, Huang JF, Liu K, Chuai ZR, Yang Z, et al. BRAF mutations in patients with non-small cell lung cancer: a systematic review and meta-analysis. PLoS One. 2014;9(6):e101354.
Paik PK, Arcila ME, Fara M, et al. Clinical characteristics of patients with lung adenocarcinomas harboring BRAF mutations. J Clin Oncol. 2011;15:2046–51.
Planchard D, Kim TM, Mazieres, et al. Dabrafenib in patients with BRAFV600E-positive advanced non-small-cell lung cancer: a single-arm, multicentre, open-label, phase 2 trial. Lancet Oncol. 2016;17(5):642–50.
Mazieres J, Peters S, Lepage B, et al. Lung cancer that harbors an HER2 mutation: epidemiologic characteristics and therapeutic perspectives. J Clin Oncol. 2013;31(16):1997–2003.
Li BT, Shen R, Buonocore D, et al. Ado-trastuzumab emtansine in patients with HER2 mutant lung cancers: results from a phase II basket trial. J Clin Oncol. 2017;35(15 Suppl):8510.
Lee SH, Lee JK, Ahn, et al. Vandetanib in pretreated patients with advanced non-small cell lung cancer-harboring RET rearrangement: a phase II clinical trial. Ann Oncol. 2016;28(2):292–7.
Drilon A, Rekhtman N, Arcila M, Wang L, Ni A, Albano M, et al. Cabozantinib in patients with advanced RET-rearranged non-small-cell lung cancer: an open-label, single-centre, phase 2, single-arm trial. Lancet Oncol. 2016;17(12):1653–60.
Kawakami H, Okamoto I, Okamoto W, Tanizaki J, Nakagawa K, Nishio K. Targeting MET amplification as a new oncogenic driver. Cancers (Basel). 2014;6(3):1540–52.
Camidge DR, Ou SH, Shapiro G, et al. Efficacy and safety of crizotinib in patients with advanced c-MET-amplified non-small cell lung cancer (NSCLC). J Clin Oncol. 2014;32(15):8001–9.
Yang JC, Sequist LV, Geater SL, et al. Clinical activity of afatinib in patients with advanced non-small-cell lung cancer harbouring uncommon EGFR mutations: a combined post-hoc analysis of LUX-lung 2, LUX-lung 3, and LUX-lung 6. Lancet Oncol. 2015;16(7):830–8.
•• Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non–small-cell lung cancer. N Engl J Med. 2018;378(2):113–25. This trial may be the first trial to reveal a newer TKI (Osimertinib) with statistically significant PFS and probably OS over standard TKI.
Katayama R. Drug resistance in anaplastic lymphoma kinase-rearranged lung cancer. Cancer Sci. 2018;109:572–80.
Acknowledgements
Thanks are due to Dr. Shirin Shafazand for helping to review this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Raja Mudad is on the advisory board for Novartis, Astra Zeneca, Takeda, and Guardant Health.
Mohamad Masri and Martine McManus declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Lung Cancer
Rights and permissions
About this article
Cite this article
Masri, M., McManus, M. & Mudad, R. Treatment of Advanced Non-Small Cell Lung Cancer in the Era of Targeted Therapy. Curr Pulmonol Rep 7, 79–91 (2018). https://doi.org/10.1007/s13665-018-0204-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-018-0204-5