Abstract
The objective of this work is to assess the nutritional status of HIV-positive patients and to correlate it to the response to treatment and to certain parameters such as age, gender, socio-economic level, etc. to validate the various tools for assessing the nutritional status of the HIV-positive population. This prospective observational study was extended over a 6-month period and included 220 HIV-positive patients. The nutritional status of each patient was evaluated according to the following tools: exploitation sheet, anthropometric analysis, food survey and calculation of dietary intake, nutritional risk index and nutritional risk stratification. The sex ratio was 52.78, where 144 (65.46%) were women, the average age was 41.60 ± 11.05 years. The evaluation of energy intake showed that 82% of patients had a deficiency in intake relative to nutritional needs. The study population presented vitamin, mineral and micronutrient deficiencies. According to the nutritional risk stratification table we designed, 53% of patients were in grade 7 and 2% were in grade 12. Undernutrition among HIV-positive people was prevalent in the study population, which had a negative impact on the health status and well-being of patients. Correcting undernutrition states would correct anthropometric parameters and biological markers, thus reducing and/or stabilizing viral load and improving CD-ratio.
The trial registration number (TRN) is 354 on February 23, 2017.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With more than 35 million deaths to date, HIV continues to be a major global public health problem. In 2016, 1 million people died from one or more HIV-related causes around the world (OMS 2018). By the end of 2016, there were around 36.7 million people living with HIV, including 1.8 million new infections (OMS 2018). In Morocco, the prevalence of HIV remains low in the general population (0.1%), the total cumulative number of people living with HIV notified since the beginning of the epidemic in 1986 to end of June 2017 amounted to 13,322, three regions concentrate more than 50% of cases (Ministère de la Santé Maroc 2017).
The human immunodeficiency virus (HIV) targets the immune system and weakens the body’s defense systems against infections and certain types of cancer, it is a risk factor for undernutrition. The HIV/AIDS epidemic has catastrophic consequences for health, nutrition, food security and overall socio-economic development in countries most affected by the disease (OMS 2008; El Alama et al. 2016a).
The HIV/AIDS epidemic is affecting populations where malnutrition is already endemic, however nutrition, immunity and inflammation are closely linked. Abnormal nutritional status interferes with the functional capabilities of the immune system. Thus, a drop in immunity is usual in malnourished patients and all the more marked since undernutrition is important. This alteration of the inflammatory and immune response accentuates morbidity (in particular infectious morbidity), delays healing and can increase the mortality rate in certain situations (Vasson and Reimund 2007; OMS 2008).
The major challenges during antiretroviral treatment are the management of nutritional and psychological disorders. Studies that support the benefit of this type of study at the start of treatment are rare. The objective of this work is to assess the nutritional status of HIV-positive patients and to correlate it to the response to treatment and to certain parameters such as age, gender, socio-economic level, etc. to validate the various tools for assessing the nutritional status of the HIV-positive population.
Patients and methods
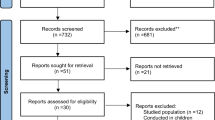
The prospective observational study was extended over a 6-month period and included 220 HIV-positive patients.
-
Ethics
-
Agreement of the ethics committee The study was conducted after obtaining the agreement of the ethics committee of the Faculty of Medicine and Pharmacy of Rabat under number 354 on February 23, 2017.
-
Informed consent and respect for anonymity We informed patients of the nature of the study, we explained the approach of each parameter studied in order to have their consent by respecting the will of each and the anonymity of the personal data which were used solely for research purposes.
-
-
Inclusion and exclusion criteria.
-
Inclusion criteria The patients who were selected for this study had to be consenting, HIV seropositive, adults over the age of 18 years with a complete clinical and biological record.
-
Exclusion criteria The patients who were excluded from this study were non-consenting, HIV negative whose age was below 18 years with an incomplete clinical and biological record.
-
The nutritional status of each patient was evaluated according to the following tools:
-
Exploitation sheet
Exploitation sheet is a file which contains the following information: diagnosis, risk factors related to the patient, risk factors related to treatment, weight, weight loss over a month, weight loss over 6 months, body mass index (BMI), albuminemia, associated infections, changes in clinical and biological parameters, etc.
-
Anthropometric analysis
It included admission weight, usual weight, height, and body mass index. The latter allowed us to classify the study population into nutritional grades (Table 1).
Table 1 Classification of nutritional status in adults by body mass index (BMI) -
Food survey and calculation of dietary intake
The food survey included daily intake of macronutrients (proteins, carbohydrates, lipids) and micronutrient (vitamins, minerals and trace elements) as well as water intake according to the nutritional value of each food product. The survey was conducted using a questionnaire using food intakes for the week, including weekends and holidays.
-
Nutritional risk index (NRI)
NRI was validated as a prognostic index in 368 patients receiving gastrointestinal, vascular, noncardiac thoracic, plastic, laparotomy and thoracotomy (minority) surgeries, by the original studies of Buzby et al. 1988a, b.
It takes into account the albumin and the ratio of the current weight to the theoretical ideal weight according to the Lorentz formula. The terminals used are specific to a geriatric population (Bach-Ngohou et al. 2004).
$${\text{NRI}} = \left[ {1.519 \times {\text{albumin}}\left( {{\text{g}}/{\text{L}}} \right)} \right] + \left[ {41.7 \times \left( {{\text{current}}\;{\text{weight}}/{\text{usual}}\;{\text{weight}}} \right)} \right]$$-
NRI > 100 No risk
-
97.5 ≤ NRI ≤ 100 Low risk
-
83.5 ≤ NRI ≤ 97.5 Moderate risk
-
NRI < 83.5 Major risk
-
-
Nutritional risk stratification
After making this nutritional assessment, each population was classified into nutritional grades based on their nutritional status and the risk of viral infection and disease stage morbidity, with a view to establishing a nutritional stratification (Table 2). The scale has been validated at the hospital.
Table 2 Stratification of nutritional risk -
Statistical analysis
The statistical analysis was done using the IBM SPSS Statistics 20.0, a p value < 0.05 was considered significant. Statistical tests were selected based on study factors (qualitative with two or more groups, matched or independent, or quantitative) and response variables (categorical qualitative with two or more groups, ordinal or quantitative qualitative).
The association of response variables (viral load and CD4 count) with quantitative study factors (weight and age) was made according to the Spearman correlation (non normal distribution or ordinal data), that with independent qualitative factors in two groups (association of undernutrition factors with gender) according to the Kruskal–Wallis test and the association with independent qualitative study factors to several groups according to the Cochran–Armitage test.
The correlation between the different scales of study was according to Pearson’s Correlation.
Results
A total of 220 patients were selected for the study, 144 (65.46%) were women (Table 3), the sex ratio was 52.78, the average age was 41.60 ± 11.05 years, 125 patients were single, 77 (35%) were illiterate, 93 (42.27%) rural, 57 (25.91%) unemployed, 39 (17.72%) without monthly income, 48 (21.82%) without medical coverage, 52 (23.63%) had family support, 118 (53.64%) were alcoholics, 94 (42.73%) were substance abusers, 202 (91.82%) had a psychiatric history.
The mode of transmission of the virus was sexual in 163 (74.09%) cases, 194 (88.18%) of patients were on antiretroviral therapy, of whom 124 (63.91%) were on triple therapy with 2INTI + 1INNTI, 171 (88.14%) patients were observant on treatment (Table 3).
The average weight of the population was 58.13 ± 13.86 kg, the average BMI value was 21.26 ± 5.85 (Tables 4 and 5).
Following a retrospective analysis of the evolution of the weight of the patients during the last 6 months, we detected a significant weight loss over one or 6 months (Table 6).
We identified 52 patients with albumin levels < 30 g/l. According to NRI values, 72% of the patients were at nutritional risk, of which 17% were at major risk (Tables 7 and 8).
The evaluation of energy intake showed that 82% of patients had a deficiency in intake relative to nutritional needs (Table 9). The study population presented vitamin, mineral and micronutrient deficiencies (Table 10a, b).
There was also a lack of total water intake (from food and beverages) (Table 11).
According to the nutritional risk stratification table we designed, 53% of patients were in grade 7 and 2% were in grade 12 (Table 12).
Biological parameters analysis identified abnormalities in total cholesterol, HDL, LDL, triglycerides, blood glucose, AST, ALT, alkaline phosphatase and hemoglobin (Table 13).
In terms of viral load, 8% of patients had a viral load ≥ 100,000 copies/mL and 81% of patients had a CD4 count > 500/mm3. The mean CD4 count was 632.93 ± 45.82, the mean viral load was 8963.15 ± 532.76 (Table 14).
Discussion
The sample was mostly composed of single women with medium or low levels of education, ranging in age from 26 to 45 years, from an urban setting. Comparing the results with African countries, a study on the assessment of the impact of HIV in the general population in Ivory Coast reported that HIV prevalence peaks at 8.7% among women aged 40 to 44 years, at 5.9% and 6.0% for men aged 55 to 59 and 60 to 64, respectively. HIV prevalence is higher among women than among men in several age groups, including 20 to 24, 25 to 29, 35 to 39, 40 to 44, and 50 to 54 years. This difference, according to the same study, is more pronounced among people aged 25 to 29 for whom HIV prevalence is about sixteen times higher for women (3.2%) than for men (0.2%) (Mbopi-Keou et al. 2013).
Social fragmentation, divorce, low socio-economic and socio-cultural levels, lack of schooling and lack of awareness are among the vulnerability factors for women, however the analysis of these factors remains complex as it is an interference and an entanglement of these and other factors (Kablan et al. 2006).
The causal link between alcohol and drug use can be direct through transmission via the instruments used or indirectly through sexual acts with multiple partners, by group sex because often drug users consume their drugs in groups or forgetting the use of condoms related to drunkenness and/or unconsciousness.
Prouvost-Keller et al. studied sex and risk factors associated with the use of psychoactive substances, found that the main sexual risks associated were: more than one partner in the month (56%), the absence of a condom (50%) or group sexuality (28%) (Prouvost-Keller et al. 2017).
HIV infection was associated in the study with a psychiatric history, according to Zoungrana et al. a personal psychiatric history was found in 38% of HIV-positive patients in Mali, including 12.9% suicidal ideation and 8, 3% had already been hospitalized in psychiatry (for depression). A family psychiatric history was noted in 1.9% of patients and this concerned the mother (Zoungrana et al. 2017).
Loss of control, envy of vengeance (of others and of oneself) and to attract the attention of others, mood disorders, indifference to the external environment, underestimation risk and disinterest in living related to depression, psychic sexual abnormalities and other mechanisms may explain this close relationship between HIV and psychiatric history.
The transmission of the virus in the patients was predominantly sexual, this mode of transmission predominates. Anogenital reports are the most effective mode of transmission: the risk for a receptive anal intercourse (penetration by an HIV-positive partner) is between 0.65% and 1.43%, depending on whether or not there is ejaculation. In an insertive anal intercourse, the risk is lower between 0.11% in circumcised men and 0.62% in others. The risk for a vaginal intercourse is 0.1% lower, depending on the sex of the HIV-positive partner, a risk of 0.15% per act in the man–woman sense and 0.09% in the sense of woman–man (Ivanovic et al. 2012).
In the present study, a total of 23 patients (11.86%) were not observant to antiretroviral therapy. Malnourished patients did not tolerate treatment and often presented with metabolic complications, which pushed them to stop treatment. Therapeutic interruption is not recommended, except in particular situations of essentially toxicity (HAS 2007).
According to a study conducted by Mbopi-Keou et al. The level of adherence reported was significantly higher than the overall level of compliance observed (80.2% vs. 51.5%, p < 10−5). The two main barriers to compliance were forgetfulness and work. Patients referred to this management unit were less observant (p < 10−4). Compliance with antiretroviral therapy was greatest when CD4 levels at baseline were high (p = 0.01) and treatment duration was prolonged (p = 0.00) (Mbopi-Kéou et al. 2012).
The main factors responsible for non-adherence in the patients were: adverse drug reactions, disease stress, lack of psychological and family support, underestimation of the risks associated with silent infection. It is obvious that the therapeutic observance is essential to transform the infection into a stable and manageable chronic disease with a well-defined viral load and without risk of passing to the AIDS stage.
Undernutrition was common in the sample with varying severity, however there is a close relationship between nutritional grade and the course of infection. In 2001, in the United States, 20% of patients living with HIV still have the wasting syndrome criteria, which is at least 80% in sub-Saharan Africa. The prevalence of malnutrition (BMI < 18.5) was 36 or 19.6%, twice as common among men as among women (p = 0.034) (Sidibé et al. 2017).
Although water is the crucial element for metabolism and life in general, the water intake of the population was insufficient, which can aggravate the adverse effects of some drugs especially renal, alter albumin levels and accelerate complications of undernutrition.
Cases of hypoalbuminemia have been identified (147 patients), lack of energy or protein intake and catabolic stress can induce hypoalbuminaemia. Its blood level is inversely proportional to the level of cytokines and reactive protein C, these elements are elevated in case of infection (Gatta et al. 2012; Kannangai et al. 2008).
Albumin is widely used as an indicator of nutritional status, however it remains a parameter that is not always reliable for assessing nutritional status, this is why we did not stop at this stage, and we used the NRI which combines albumin with other parameters for an overall and more objective evaluation (El Alama et al. 2016a).
Although metabolic disorders are due to malnutrition in the study population, antiretrovirals have also metabolic side effects and may aggravate existing metabolic disorders such as hypercholesterolemia, hypertriglyceridemia and hyperglycemia. On the other hand, the interactions between antiretrovirals and metabolism drugs or food can cause disorders on the different metabolic pathways (Theriaque 2019).
Liver enzymes (AST, ALT, alkaline phosphatase) were elevated in the study population due to antiretrovirals (Theriaque 2019), however tobacco, alcohol and drugs also have a direct impact on serum transaminase levels, ALT is more high when cigarette consumption exceeds 20 per day (Robinson and Whitehead 1989).
Some foods can also increase them such as those high in simple sugars, saturated fatty acids, sodium, vitamin C, food additives, herbs for both herbal and culinary purposes, with the exception of some that have hepatoprotective effects and detoxifiers such as milk thistle and burdock root, two medicinal plants belonging to the Asteraceae family. Other foods, however, lower the level of liver enzymes, either by a direct effect or by protecting both lesions and detoxification. People with a high level of vitamin D are less vulnerable to liver damage than those with low levels of vitamin D (Skaaby et al. 2014).
The mean hemoglobin level was 11.94 ± 1.48 g/dl, this decrease, although it has inflammatory origins linked to the infection whose mechanism is unknown but which may be due to an increase in cytokines that modify iron homeostasis and inhibit erythropoiesis, also has dietary origins due to lack of intake and/or absorption of certain nutrients such as iron, vitamin B12 and folic acid (Weiss and Goodnough 2005).
Nutritional status has an impact on the immune system, the coexistence of infection and malnutrition has serious and long-lasting consequences, especially among HIV-positive people (Cunningham-Rundles et al. 2011).
Water intake was insufficient in the population, dehydration can alter albumin levels and aggravate the adverse drug effects of antiretrovirals especially renal.
Pharmaco-economic factors related to the disease, whether for the overall cost of treatment or for the direct or indirect handicap of having a stable monthly income, influence the level of food intake.
The disease itself as well as antiretroviral therapy with its side effects (nausea, vomiting, diarrhea, hyperglycemia, etc.) is a nutritional risk factor. Antiretroviral drug-drug interactions can alter the response to treatment by physiochemical, pharmacokinetic and pharmacodynamic mechanisms, which is why the timing of medication with respect to meals must be respected (El Alama et al. 2016b). Total daily energy intakes in the patients were inadequate with an average of 19.20 ± 11.68 kcal/kg/day, WHO suggests that it is likely that energy requirements will increase by 10% to maintain weight and physical activity in HIV-infected and asymptomatic adults, these needs increase by approximately 20 to 30% in symptomatic patients to maintain weight in adults.
The average daily protein intake was 0.6 ± 0.23 g/kg/day, the recommended intakes in the normal person are of the order of 1.1 g/kg/day, these needs increase in the seropositive and typically range from 1.2 to 2.0 g/kg/day, and can reach 3.0 g/kg/day during the symptomatic phase (Nguewo and Winkler 2008). As for WHO, there is insufficient evidence to establish that protein requirements increase with HIV infection.
The mean daily carbohydrate intake in the patients was 3.78 ± 1.86 g/kg/day, the recommended intakes in a normal person are of the order of 4 g/kg/day, these intakes should cover about 60% of total energy intake.
Average daily lipid intake was 0.92 ± 0.45 g/kg/day, the recommended intakes in a normal person are of the order of 0.9 g/kg/day. In seropositive patients the daily intake of fat should be between 1.2 and 1.8 g/kg (Nguewo and Winkler 2008).
There is no argument from the WHO justifying the increase in total fat intake due to HIV infection. In contrast, specific advice on lipid intake may be required for people on antiretroviral therapy or those with persistent diarrhea (Nguewo and Winkler 2008).
In the present study, the intake of vitamins, minerals and trace elements in the patients did not meet the recommended reference values, although they are involved in the proper functioning of the immune system and therefore in the response to antiretroviral therapy. The requirements for vitamins A, B1, B2, B3, B6, B12, C, E and zinc are generally high in seropositive patients (Nguewo and Winkler 2008).
Zinc and copper are essential mineral substances in the human body, which are also necessary for many enzymes. Zinc and copper levels in the body are regulated by a protein called metallothionein. This protein acts so that zinc levels increase when copper levels drop, and vice versa. People living with HIV/AIDS who take zinc supplements are also advised to take copper supplements (Lyons 2019). Several studies have evaluated the impact of zinc supplementation on HIV-positive patients, a supplementation of 45 mg or 200 mg has increased the rate of CD4, maintain or regain weight and strengthen the immune system while decreasing the risk of infection, however, there was controversy over the significant quality of these results, Some studies were inconclusive because they used only zinc as supplement knowing that an increase in the rate of zinc lowers that of copper (Lyons 2019).
Conclusion
Undernutrition among HIV-positive people was prevalent in the study population, which had a negative impact on the health status and well-being of patients.
Correcting undernutrition states would correct anthropometric parameters and biological markers, thus reducing and/or stabilizing viral load and improving CD-ratio.
Nutritional management among HIV-positive people has become a therapeutic necessity because of the impact of the disease and treatment on the nutritional status of patients.
It is clear that pharmaconutrients play a vital role in strengthening the immune system.
The design of a clinical nutrition service specifically trained for this type of pathology, the combination of natural nutrition and supplementation with micro and macronutrients, remains the best solution for the metabolic complications caused in these patients, as well as the degree of anorexia and psychological disorder induced by the disease.
References
Bach-Ngohou K, Bettembourg A, Le Carrer D, Masson D, Denis M (2004) Évaluation clinico-biologique de la dénutrition. Ann Biol Clin 62(4):395–403
Buzby G, Knox L, Crosby L, Eisenberg J, Haakenson C, McNeal G et al (1988a) Study protocol: a randomized clinical trial of total parenteral nutrition in malnourished surgical patients. Am J Clin Nutr 47(2):366–381
Buzby G, Williford W, Peterson O, Crosby L, Page C, Reinhardt G et al (1988b) A randomized clinical trial of total parenteral nutrition in malnourished surgical patients: the rationale and impact of previous clinical trials and pilot study on protocol design. Am J Clin Nutr 47(2):357–365
Cunningham-Rundles S, Ahrné S, Johann-Liang R, Abuav R, Dunn-Navarra A-M, Grassey C et al (2011) Effect of probiotic bacteria on microbial host defense, growth, and immune function in human immunodeficiency virus type-1 infection. Nutrients 3(12):1042–1070
El Alama H, Boufettal R, Benmoussa A, Jai SR, Chehab F, Derfoufi S (2016a) Evaluation of preoperative nutritional status in visceral surgery Correlational study. J Pharm Belg 4:30–39
El Alama H, Filali H, Rahmoune I, Tazi A, Hakkou F (2016b) The drug-food interactions. J Chem Pharm Res 8(9):1–3
Gatta A, Verardo A, Bolognesi M (2012) Hypoalbuminemia. Intern Emerg Med 7(3):S193–S199
HAS (2007) Guide – Affection de longue durée. Infection par le virus de l’immunodéficience humaine (VIH). Décembre. https://www.has-sante.fr/portail/upload/docs/application/pdf/vih_guidemedecin_version_web.pdf. Accessed 20 Sept 2019
Ivanovic J, Misic D, Zizovic I, Ristic M (2012) In vitro control of multiplication of some food-associated bacteria by thyme, rosemary and sage isolates. Food Control 25(1):110–116
Kablan C, Obrist B, Cissé G, Wyss K, Touré I, Tanner M (2006) VIH/SIDA, genre et vulnérabilité. VertigO-la revue électronique en sciences de l’environnement. (Hors-série 3)
Kannangai R, Kandathil AJ, Ebenezer DL, Mathai E, Prakash AJ, Abraham OC et al (2008) Usefulness of alternate prognostic serum and plasma markers for antiretroviral therapy for human immunodeficiency virus type 1 infection. Clin Vaccine Immunol CVI 15(1):154–158
Lyons L (2019) CATIE. Canadian AIDS Treatement Information Exchange. Feuillet d’information: Le zinc et le cuivre. https://www.catie.ca/ga-pdf.php?file=pdf/Supple-f/Zinc_Copper_f.pdf. Accessed 25 Sept 2019
Mbopi-Keou F-X, Nguefack-Tsague G, Kalla GCM, Viche L, Noubom M (2013) Profil épidémiologique de l’infection à VIH au cours d’une campagne de sensibilisation à Yaoundé au Cameroun. Pan Afr Med J 15(1):119
Mbopi-Kéou F-X, Dempouo Djomassi L, Monebenimp F (2012) Etude des facteurs liés à l’observance au traitement antirétroviral chez les patients suivis à l’Unité de Prise En Charge du VIH/SIDA de l’Hôpital de District de Dschang, Cameroun. Pan Afr Med J 12:55
Ministère de la Santé Maroc (2017) Journée Mondiale de Lutte Contre le Sida: Réalisations et Perspectives. http://www.sante.gov.ma/Documents/2017/11/JMS%202017%20BROCHURE%20fr.pdf. Accessed 22 Sept 2019
Nguewo EA, Winkler G (2008) Recommandations nutritionnelles pratiques avec exemples de menus pour personnes vivant avec le VIH/SIDA en Afrique Noire. Pan Afr Med J 1:1
OMS (2008) Besoins en nutriments des personnes vivant avec le VIH/sida: Rapport d’une consultation technique. http://www.who.int/nutrition/publications/hivaids/9789242591194_fre.pdf. Accessed 20 Sept 2019
OMS (2018) VIH/sida: principaux faits. http://www.who.int/fr/news-room/fact-sheets/detail/hiv-aids. Accessed 23 Sept 2019
Prouvost-Keller B, Naqvi A, Joulié A, Cua E, Pradier C, Roger PM (2017) Characteristics and risk factors associated to the consumptions of psychoactive products during sexual intercourse of patient attending HIV and viral hepatitis screening management centers in Southern France in 2015. Bull Epidémiol Hebd 21:455–463
Robinson D, Whitehead TP (1989) Effect of body mass and other factors on serum liver enzyme levels in men attending for well population screening. Ann Clin Biochem 26:393–400
Sidibé S, Magassouba A, Delamou A, Magaboussa F, Sandouno S, Kra K et al (2017) Statut nutritionnel des personnes vivant avec le VIH/sida dans le centre médical communautaire de Ratoma (République de Guinée). Médecine et Santé Tropicales 27(1):77–81
Skaaby T, Husemoen LLN, Borglykke A, Jørgensen T, Thuesen BH, Pisinger C et al (2014) Vitamin D status, liver enzymes, and incident liver disease and mortality: a general population study. Endocrine 47(1):213–220
Thériaque (2019) Banque de donnée sur les médicaments. http://www.theriaque.org/apps/interaction/itr_ordonnance.php. Accessed 19 Sept 2019
Vasson M-P, Reimund J-M (2007) Nutrition, immunité et inflammation. In: Cano N, Barnoud D, Schneider SM, Vasson M-P, Hasselmann M, Leverve X (eds) Traité de nutrition artificielle de l’adulte. Springer, Paris, pp 455–472
Weiss G, Goodnough LT (2005) Anemia of chronic disease. N Engl J Med 352(10):1011–1023
Zoungrana J, Dembélé J, Sako F, Siranyan S, Traore J, Sawadogo A et al (2017) Dépression et VIH: aspects épidémiologiques et cliniques au centre hospitalier universitaire du Point G de Bamako (Mali). Médecine et Santé Tropicales 27(2):186–189
Acknowledgements
The authors wish to thank everyone who participated in the realization of this work. The authors received no funding for this work.
Author information
Authors and Affiliations
Contributions
All the authors participated in the development of this work.
Corresponding author
Ethics declarations
Ethical statement
The study was conducted after obtaining the agreement of the ethics committee of the Faculty of Medicine and Pharmacy of Rabat under number 354 on February 23, 2017.
Conflict of interest
Hakim El Alama has no conflict of interest. Touria Fatihi has no conflict of interest. Adnane Benmoussa has no conflict of interest. Amina Barkat has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
El Alama, H., Fatihi, T., Benmoussa, A. et al. Assessment of nutritional status in HIV-positive population. ADV TRADIT MED (ADTM) 21, 163–171 (2021). https://doi.org/10.1007/s13596-020-00444-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13596-020-00444-8