Abstract
The Trypanosoma brucei is the causative agent of African trypanosomiasis, a disease that affects both humans and animals. Chemotherapy which forms the major means of control for the disease has several shortcomings such as limited efficacy and adverse side effects amongst others. Thus, motivating the search for better therapies. In this study, extracts of some tropical plants including the Acacia nilotica, Bombax buonopozense and Khaya senegalensis were evaluated for therapeutic and prophylactic potential in mouse model of experimental trypanosomiasis. Both diminazene aceturate and isometamidium chloride were included as reference drugs. Results showed that T. brucei caused an elevation in rat plasma indirect bilirubin and a reduction in rat plasma albumin and total protein which suggest mild hepatic dysfunction due to experimental infection. Data also revealed that the plant extracts significantly reduced the rat parasite burden both in the prophylaxis and therapeutic treatment groups when compared with the negative drug control. The infection and treatments had no adverse effect on the rat organ and body weights. The infection did not alter the activity of rat plasma ALT, AST and ALP compared with the administered extracts of A. nilotica and B. buonopozense. Further, the plant extracts ameliorated some trypanosomiasis-induced pathologies in treated rats compared with negative drug control. Taken together, findings do not only lend credence to the folkloric use of these plants for medicinal purposes but also suggest these plant extracts have potential to serve as alternative source of anti-parasitic agents particularly for the control of trypanosomiasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trypanosomes are causative agents for a number of human infections and veterinary diseases. The Trypanosoma brucei is the causative agent of African trypanosomiasis, a disease that affect both humans and animals. The human African trypanosomiasis (HAT) is commonly referred to as sleeping sickness. The parasite is transmitted in humans by bites from tsetse flies which are blood-sucking thereby transmitting the parasite to the blood of the host (Buscher et al. 2017). Currently, ~ 500,000 people in sub-Saharan Africa are infected with deaths between 50,000 and 70,000 annually. Prevalence is higher in adults than children and rural dwellers are more susceptible due to easy exposure to the vector especially in farms, river etc. There is no known effective vaccination against diseases caused by T. brucei as there is no successful trial yet. The HAT caused a very critical epidemic in the twentieth century. On the other hand, the animal African trypanosomiasis also known as nagana (which means weakness in Zulu) kills about 1 million cattle each year with estimated economic cost put at around $1.2 billion (Buscher et al. 2017; Ekanem et al. 2005, 2006a, b). Nagana is caused by T. congolense, T. brucei and T. vivax, these parasites have more adverse effect on domestic than on game animals thereby making it of economic importance and every domestic animal could be affected by this infection. Certain symptoms are associated with trypanosomiasis which includes, discharge from the eye, hair loss, weight loss, fever, oedema etc. (Steverding 2008). If untreated, both the human and animal trypanosomiasis could lead to fatal outcome (Adeyemi et al. 2017, 2018). Studying closely the disease over the years in African history; the progress achieved thus far is in the control and not in eradication of the disease. Current treatment options include the use of pentamidine, suramin, and melarsoprol amongst others (Steverding and Tyler 2005). But these drugs have several limitations; unwanted side effects, emergence of drug resistance strains, difficulty of administration as well as insufficient understanding of the mode of action (Adeyemi and Sulaiman 2012a, b; Sulaiman and Adeyemi 2010; Akanji et al. 2009; Perez-Morga 2007; Sulaiman et al. 2017). Therefore, the development of newer therapy for trypanosomiasis is urgently needed.
Plant materials present novel possibilities to obtain new drugs that are active against trypanosomes (Adeyemi et al. 2011). Indeed, there have been several reports of alternative anti-Trypanosoma agents obtained from screening extracts of African plants (Ekanem et al. 2006a, b; Sulaiman et al. 2017). Acacia nilotica is a significant ornamental and medicinal plant that is commonly found in the tropics and sub-tropics and it has been implicated for wide-range of biological activities such as anti-diarrhea, anti-tuberculosis and anti-leprosy as well as identified as a source of many active secondary metabolites which may serve as potential candidates for development of novel lead compounds (Rather et al. 2015). Bombax buonopozense, is commonly known as the Gold Coast Bombax. It is a wild tree commonly found in Nigeria and other West Africa countries (Ngwuluka et al. 2012). It has several medicinal uses locally (Ngwuluka 2012; Akuodor et al. 2012). For example, the dried stem is used in the treatment of malaria in Ghana (Asase and Oppong-Mensah 2009), the bark is used to treat chest pain in Gambia (Madge 1998) and the decoction of the leaves is used to manage stomach ulcers and burns in Ghana (Agyare et al. 2009). Khaya senegalensis is a specie of tree in the Meliaceae family that is native to Africa. Common name is African Mahogany. Traditionally, the plant has been used for treating jaundice, dermatoses, malaria, fever, mucous diarrhea, and venereal diseases as well as for hookworm infection (Onu et al. 2013). Extracts of this plant K. senegalensis have also been reported to exhibit anti-inflammatory effects (Lompo et al. 1998), anti-bacterial (Koné et al. 2004), antihelmintic (Ademola et al. 2004), wound healing and antiplasmodial activities (El Tahir et al. 1998). In the present study, three plants including the A. nilotica, B. buonopozense and K. senegalensis were screened for anti-Trypanosoma and toxicity potential in rats.
Materials and methods
Reagents
All chemicals and reagents were of analytical grade and were used as supplied. Commercial assay kits for Alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALT), urea, creatinine (CREA), albumin (ALB), bilirubin (BIL), were products of Randox Laboratories Limited, Crumlin, UK.
Plant sample
Fresh sample of the stem bark of A. nilotica, B. buonopozense and K. senegalensis were obtained from a forest at Ilorin, Kwara State, Nigeria. The plants were botanically authenticated by Mr Bolu of the Herbarium unit of the department of Plant Biology, University of Ilorin, Kwara State, Nigeria where voucher specimens (UIH001/852—A. nilotica, UIH003/899—B. buonopozense, and UIH002/856—K. senegalensis) were deposited. The fresh stem barks were air-dried to a constant weight in the laboratory. Dried plant materials were each pulverized using mortar and pestle into smaller pieces and then reduced to powdery form using a mill. Each of the powdery plant materials was weighed and soaked in a mixture of methanol and distilled water (7:3 v/v respectively) and allowed to macerate for 72 h (with intermittent shaking at 1-h interval). Sample solution was filtered using Whatman No 1 filter paper and concentrated under reduced pressure at 55 °C. The plant extracts were stored in a refrigerator until required for experimental use.
Parasite
A stabilate of pleomorphic T. brucei brucei was obtained from the Nigeria Institute for Trypanosomiasis and Onchocerciasis Research (NITR), Kaduna and maintained by serial passage in Wistar rats as previously described (Adeyemi et al. 2017). Infection was monitored every morning as previously described (Adeyemi et al. 2017) by light microscopic examination of the blood samples taken from the tail of the infected rats.
Experimental animals
Forty (40) apparently healthy male Wistar rats weighing between 100 and 115 g were obtained from the Animal House of the Biochemistry Department of the University of Ilorin, Ilorin, Kwara State, Nigeria. The animals were housed in plastic cages with saw dust as beddings and fed on standard rat feed and allowed access to water ad libitum. The animals were allowed to acclimate for 1 week before the commencement of experimental procedures. Handling of animals was consistent with relevant guidelines on the care and use of laboratory animals (National Research Council 2011).
Experimental infection of rats and parasite count
Blood was collected by jugular puncture with a syringe from a heavily infected rat and immediately diluted with PBS to serve as inoculums. Healthy rats were infected intraperitoneally with 1 ml of the inoculums containing about 100 trypanosome cells. The parasiteamia was monitored daily using light microscopy (Adeyemi et al. 2017).
Experimental treatments
The Wistar rats were distributed randomly into ten groups of four rats. Further details of the grouping are as given in Table 1. The extract administration was done orally through the use of oral gavage. Rat parasite burden and body weight were monitored daily. The experimental treatment lasted for 21 days.
Blood collection and isolation of tissues
All animals were fasted overnight and sacrificed under anesthesia in slight diethyl ether, 24 h after the last treatments. Blood samples were obtained by cardiac puncture into clean EDTA bottles. The blood samples were centrifuged at 1000×g for 10 min using a Uniscope Centrifuge (Model SM800B, Surgifriend Medicals, England, UK) to obtain the plasma. The brain, kidney and liver from each animal was excised into iced-cold isotonic solution (pH 7.4), weighed and homogenized immediately.
Biochemical assays
The levels of rat serum and tissue total protein (TP), albumin, aspartate aminotransferase (AST—EC: 2.6.1.1), alanine aminotransferase (ALT—EC: 2.6.1.2), alkaline phosphatase (ALP—EC: 3.1.3.1), bilirubin, urea, creatinine and glucose were determined using Randox assay kits (Crumlin, UK).
Data analysis
Data were analyzed using the analysis of variance (ANOVA) and Duncan multiple range test (GraphPad Prism version 5.0). The data were presented as mean ± standard error of mean. Group mean value at 5% level of confidence (p < 0.05) was considered significant.
Results and discussion
Results
In the present study, three African plants were screened for prophylactic and therapeutic potential against the T. brucei experimental infection in rats. The T. brucei infection as well as the various treatments did not adversely alter rat weight (Fig. 1a). The weight of vital organs such as the brain, heart, kidney and liver were not affected by T. brucei infection as well as the extract treatments (Fig. 1b–e). Likewise, the organ-to-body weight ratio revealed no significant difference among the experimental groups as well (Fig. 1f–i).
Average weights of rat following Trypanosoma infection and treatments. a Body; b brain; c liver; d kidney; e heart; f brain-to body ratio; g liver-to-body ratio; h kidney-to-body ratio; i heart-to-body ratio. Values are expressed as the mean + standard error of the mean (SEM, n = 5). NIF, not infected; NDC, negative drug control; DA, diminazene aceturate; ISC, isometamidium chloride; ANT, A. nilotica therapeutic; ANP, A. nilotica prophylactic; BBT, B. buonopozense therapeutic; BBP, B. buonopozense prophylactic; KST, K. senegalensis therapeutic; KSP, K. senegalensis prophylactic
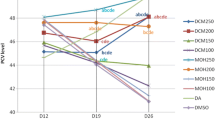
The parasite burden in the negative drug control group drastically increased as the infection progressed (Fig. 2a, b and Table 2). Also, rats in this group died 10-days post infection, while the rats treated with plant extracts both as prophylactic and therapeutic significantly decreased the parasite burden by ≥ 85% as well as extended the survival time of the infected animals until cessation of experiment.
Anti-Trypanosoma potential. a Effect of extracts of plants on parasite burden in rats; b average percentage reduction in parasite burden. Values are expressed as the mean + standard error of the mean (SEM, n = 5). NIF, not infected; NDC, negative drug control; DA, diminazene aceturate; ISC, isometamidium chloride; ANT, A. nilotica therapeutic; ANP, A. nilotica prophylactic; BBT, B. buonopozense therapeutic; BBP, B. buonopozense prophylactic; KST, K. senegalensis therapeutic; KSP, K. senegalensis prophylactic
Assay of some biochemical indices included rat plasma ALT, AST, ALP, albumin, total protein, bilirubin, urea, creatinine and glucose (Fig. 3). The T. brucei infection did not alter the activity of rat plasma ALT, AST and ALP compared with the other treatment groups. Therapeutic and prophylactic administration of B. buonopozense and A. nilotica extracts elevated the levels of rat serum ALP.
Liver function indices in rat plasma following Trypanosoma infection and treatments. a Alanine transaminase (ALT); b Aspartate transaminase (AST); c Alkaline phosphatase (ALP). Values are expressed as the mean + standard error of the mean (SEM, n = 5). NIF, not infected; NDC, negative drug control; DA, diminazene aceturate; ISC, isometamidium chloride; ANT, A. nilotica therapeutic; ANP, A. nilotica prophylactic; BBT, B. buonopozense therapeutic; BBP, B. buonopozense prophylactic; KST, K. senegalensis therapeutic; KSP, K. senegalensis prophylactic
Further, T. brucei caused reduction in rat plasma albumin and total protein level (Fig. 4) and also showed an elevation in rat plasma indirect bilirubin level (Fig. 5). The extracts of A. nilotica and B. buonopozense respectively as therapeutic and prophylactic treatments raised (p < 0.01) the plasma creatinine level when compared with the NIF group (Fig. 6).
Protein and albumin level in rat plasma following Trypanosoma infection and treatments. a Protein; b albumin. Values are expressed as the mean + standard error of the mean (SEM, n = 5). NIF, not infected; NDC, negative drug control; DA, diminazene aceturate; ISC, isometamidium chloride; ANT, A. nilotica therapeutic; ANP, A. nilotica prophylactic; BBT, B. buonopozense therapeutic; BBP, B. buonopozense prophylactic; KST, K. senegalensis therapeutic; KSP, K. senegalensis prophylactic
Bilirubin level in rat plasma following Trypanosoma infection and treatments. a Total bilirubin; b direct bilirubin; c indirect bilirubin. Values are expressed as the mean + standard error of the mean (SEM, n = 5). NIF, not infected; NDC, negative drug control; DA, diminazene aceturate; ISC, isometamidium chloride; ANT, A. nilotica therapeutic; ANP, A. nilotica prophylactic; BBT, B. buonopozense therapeutic; BBP, B. buonopozense prophylactic; KST, K. senegalensis therapeutic; KSP, K. senegalensis prophylactic
Kidney function-related indices and glucose level in rat plasma following Trypanosoma infection and treatments. a Urea; b creatinine; c glucose. Values are expressed as the mean + standard error of the mean (SEM, n = 5). NIF, not infected; NDC, negative drug control; DA, diminazene aceturate; ISC, isometamidium chloride; ANT, A. nilotica therapeutic; ANP, A. nilotica prophylactic; BBT, B. buonopozense therapeutic; BBP, B. buonopozense prophylactic; KST, K. senegalensis therapeutic; KSP, K. senegalensis prophylactic
Discussion
Chemotherapy forms the bulk of the disease-control method for trypanosomiasis. However, the available treatment options have several limitations such as limited efficacy, undesired side effects, and emergence of drug resistant parasites amongst others. These factors underscore the search for newer and better therapy for the trypanosomiasis
Increase in the parasite burden with the progression of the infection of negative drug control group correlates with severity of infection as the rats in the negative drug control group, died 10-days post infection. The extension of the survival time of infected animals treated with extracts until cessation of experiment, thus attests to the potential of natural products as likely source of alternative anti-parasitic agents. Further, analysis of the parasite counts on a weekly basis suggests a trypanostatic effect by the plant extracts for all the treatment conditions. Taken together, the data suggest that the prophylactic and therapeutic options do not have any advantage over one another. This is due to the fact that systemic parasite clearance and extension of the survival time (all plant extracts-treated animals were alive until necropsy on the 22nd day post-infection) appear not to differ appreciably among the plant extract treatments compared with the negative drug control.
Further, our finding herein is consistent with investigations demonstrating the therapeutic potential of many African plants against T. brucei experimental infection in rats (Adeyemi et al. 2017, 2011; Ekanem et al. 2006a, b). Further our findings herein are consistent with the wide-range of medicinal value such as anti-diarrhea, antimalarial and anti-microbial which had been reported for the extracts of A. nilotica (Rather et al. 2015), B. buonopozense (Ngwuluka 2012; Akuodor et al. 2012) and K. senegalensis (Onu et al. 2013).
Furthermore, in order to evaluate the pathological impact of T. brucei infection, we assayed some biochemical indices such as rat plasma ALT, AST, ALP, albumin, total protein, bilirubin, urea, creatinine and glucose. The T. brucei infection did not alter the activity of rat plasma ALT, AST and ALP compared with the other treatment groups. In contrast, extracts of B. buonopozense and A. nilotica administered as therapeutic and prophylactic did raise the rat serum ALP. The elevated level of serum ALP may reflect adaptive mechanism necessary to cope with prolonged administration of the extract. This finding is consistent with the reports of Kolawole et al. (2012) that demonstrated the increased serum ALT and AST.
Further, T. brucei caused reduction in rat plasma albumin and total protein level in manner that suggests reduced capacity of rat liver to synthesize protein. This finding agrees with our previous reports (Adeyemi and Sulaiman 2012a, b; Sulaiman and Adeyemi 2010; Adeyemi et al. 2012) in which T. brucei infection led to reduced synthetic capacity of the liver. One of the primary hepatic functions is protein synthesis. Therefore, serum/plasma protein level could be used to adjudge early compromise of the synthetic function of the liver. The elevated rat plasma indirect bilirubin level thusly indicates that the rat hepatic functions might have been mildly compromised as a result of the experimental infection. However, treatment with the plant extracts did ameliorate these biochemical indices in manners that suggest improved hepatic function.
Beyond the reduction in parasite burden, the plant extracts did not significantly impact the biochemical indices differently from the negative drug control. The elevated plasma creatinine level as a result of A. nilotica and B. buonopozense extract therapeutic and prophylactic administration respectively when compared with the NIF group suggests under-excretion as a result of kidney impairment. While the elevated creatinine level may indicate likely impairment of kidney function, the plasma urea level was not altered compared with the NIF group. Although, studies have implicated the extracts of K. senegalensis, B. buonopozense, and A. nilotica for likely toxicity in rats (Kolawole et al. 2012), nevertheless, the present study did not find any serious alteration in the rat plasma and tissue biochemical indices that may suggest serious cellular injury. Probably, the disparity in these findings may be due to the doses and/or route of administration of these plant extracts. Furthermore, the extract administration appears not to impact the blood glucose level significantly different from the negative control group or the NIF group and thus may indicate that the biochemical effect of the extracts precludes the cellular utilization of glucose.
In conclusion, the extracts of the three African plants namely A. nilotica, B. buonopozense, and K. senegalensis demonstrated promising anti-Trypanosoma activity. The plant extracts significantly reduced the rat systemic parasite burden and extended the survival time of treated animals. Furthermore, at the therapeutic doses, the plant extracts do not appear to adversely impact rat tissue functional and biochemical indices.
References
Ademola I, Fagbemi B, Idowu S (2004) Evaluation of the anthelmintic activity of Khaya senegalensis extract against gastrointestinal nematodes of sheep: in vitro and in vivo studies. Vet Parasitol 122:151–164. https://doi.org/10.1016/j.vetpar.2004.04.001
Adeyemi O, Sulaiman F (2012a) Biochemical and morphological changes in Trypanosoma brucei brucei-infected rats treated with homidium chloride and diminazene aceturate. J Basic Clin Physiol Pharmacol. https://doi.org/10.1515/jbcpp-2012-0018
Adeyemi O, Sulaiman F (2012b) Depletion of parasitaemia by halofantrine hydrochloride and artemether in rats infected with African trypanosomes. Afr J Pharm Pharmacol 3:432–438
Adeyemi O, Sykes M, Akanji M, Avery V (2011) Anti-trypanosoma and cytotoxic activity of ethanolic extracts of Psidium guajava leaves in Alamar Blue based assays. Vertin Arch 81:623–633
Adeyemi O, Akanji M, Ekanem J (2012) Ethanolic extract of Psidium guajava influences protein and bilirubin levels in Trypanosoma brucei brucei infected rats. J Biol Sci 12:111–116. https://doi.org/10.3923/jbs.2012.111.116
Adeyemi OS, Molina MT, Eseola AO, Fonseca-Berzal C, Gómez-Barrio A (2017) New imidazole compounds active against Trypanosoma cruzi. Comb Chem High Throughput Screen 20(1):20–24
Adeyemi O, Molefe N, Awakan O et al (2018) Metal nanoparticles restrict the growth of protozoan parasites. Artif Cells Nanomed Biotechnol. https://doi.org/10.1080/21691401.2018.1489267
Agyare C, Asase A, Lechtenberg M et al (2009) An ethnopharmacological survey and in vitro confirmation of ethnopharmacological use of medicinal plants used for wound healing in Bosomtwi-Atwima-Kwanwoma area, Ghana. J Ethnopharmacol 125:393–403. https://doi.org/10.1016/j.jep.2009.07.024
Akanji M, Adeyemi O, Oguntoye S, Sulyman F (2009) Psidium guajava extract reduces trypanosomosis associated lipid peroxidation and raises glutathione concentrations in infected animals. EXCLI J 8:148–154
Akuodor G, Essien A, Ibrahim J et al (2012) Phytochemical and antimicrobial properties of the methanolic extracts of Bombax buonopozense leaf and root. Asian J Med Sci 2:190–194. https://doi.org/10.3126/ajms.v2i3.4222
Asase A, Oppong-Mensah G (2009) Traditional antimalarial phytotherapy remedies in herbal markets in southern Ghana. J Ethnopharmacol 126:492–499. https://doi.org/10.1016/j.jep.2009.09.008
Buscher P, Cecchi G, Jamonneau V, Priotto G (2017) Human African trypanosomiasis. Lancet 390:2397–2409. https://doi.org/10.1016/S0140-6736(17)31510-6
Ekanem JT, Sulyman FA, Adeyemi OS (2005) Therapeutic properties and serum iron in Trypanosoma brucei brucei- infected rats treated with amodiaquine and mefloquine. Biokemistri 17(2):115–121
Ekanem J, Majolagbe O, Sulaiman F, Muhammad N (2006a) Effect of honey supplemented diet on the parasitaemia and some enzymes of Trypanosoma brucei-infected rats. Afr J Biotechnol 5:1557–1561
Ekanem J, Sulaiman F, Adeyemi O (2006b) Therapeutic properties and serum iron in T. brucei infected rats treated with amodiaquine and mefloquine. Biokemistri. https://doi.org/10.4314/biokem.v17i2.32596
Kolawole O, Wahab A, Adekanle D et al (2012) Seroprevalence of hepatitis B surface antigenemia and its effects on hematological parameters in pregnant women in Osogbo, Nigeria. Virol J. https://doi.org/10.1186/1743-422x-9-317
Koné W, Atindehou K, Terreaux C et al (2004) Traditional medicine in North Côte-d’Ivoire: screening of 50 medicinal plants for antibacterial activity. J Ethnopharmacol 93:43–49. https://doi.org/10.1016/j.jep.2004.03.006
Lompo M, Nikiéma J, Guissou I et al (1998) The topical antiinflammatory effect of chloroform extract from Khaya senegalensis stem barks. Phytother Res 12:448–450. https://doi.org/10.1002/(sici)1099-1573(199809)12:6%3c448:aid-ptr325%3e3.0.co;2-1
Madge C (1998) Therapeutic landscapes of the Jola, The Gambia, West Africa. Health Place 4:293–311. https://doi.org/10.1016/s1353-8292(98)00033-1
National Research Council (2011) Guide for the care and use of laboratory animals, 8th edn. The National Academies Press, Washington, DC. https://doi.org/10.17226/12910
Ngwuluka N (2012) Are Bombax buonopozense and Bombax malabaricum possible nutraceuticals for age management? Prev Med 54:S64–S70. https://doi.org/10.1016/j.ypmed.2011.12.027
Ngwuluka N, Kyari J, Taplong J, Uwaezuoke O (2012) Application and characterization of Gum from Bombax buonopozense calyxes as an excipient in tablet formulation. Pharmaceutics 4:354–365. https://doi.org/10.3390/pharmaceutics4030354
Onu A, Saidu Y, Ladan M et al (2013) Effect of aqueous stem bark extract of Khaya senegalensis on some biochemical, haematological, and histopathological parameters of rats. J Toxicol 2013:1–9. https://doi.org/10.1155/2013/803835
Perez-Morga D (2007) Human resistance to African trypanosoma infections. Bull Mem Acad R Med Belg 162(7–9):381–386
Rather L, Shahid-ul-Islam, Mohammad F (2015) Acacia nilotica (L.): a review of its traditional uses, phytochemistry, and pharmacology. Sustain Chem Pharm 2:12–30. https://doi.org/10.1016/j.scp.2015.08.002
Steverding D (2008) The history of African trypanomiasis. Parasites Vectors 1:3. https://doi.org/10.11866/1756-3305-1-3
Steverding D, Tyler K (2005) Novel antitrypanosomal agents. Expert Opin Investig Drugs 14:939–955. https://doi.org/10.1517/13543784.14.8.939
Sulaiman F, Adeyemi O (2010) GC-MS analysis of bioactive fractions of Terminalia avicennoides and Bombax buopodezense bark and lipid profile of Trypanosoma brucei infected wistar rats. EXCLIJ 9:39–45
Sulaiman A, Oloyede H, Akanji M et al (2017) GC-MS analysis of bioactive fractions of Terminalia avicennoides and Bombax buopodezense bark and lipid profile of Trypanosoma brucei infected wistar rats. Afr Sci 17:4
Tahir A, Ibrahim A, Satti G et al (1998) The potential antileishmanial activity of some Sudanese medicinal plants. Phytother Res 12:576–579. https://doi.org/10.1002/(sici)1099-1573(199812)12:8%3c576:aid-ptr354%3e3.0.co;2-%23
Acknowledgements
N/A
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical statement
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. The ethical reference number is 030517/BCH.
Conflict of interest
F. A. Sulaiman has no conflict of interest. O. A. Iyiola has no conflict of interest. T. A. Anifowoshe has no conflict of interest. A. A. Sulaiman has no conflict of interest. O. K. Bello has no conflict of interest. T. J. Akinyele has no conflict of interest. A. M. Jimoh has no conflict of interest. R. F. Maimako has no conflict of interest. D. A. Otohinoyi has no conflict of interest. O. O. Osemwegie has no conflict of interest. O. S. Adeyemi has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sulaiman, F.A., Iyiola, O.A., Anifowoshe, T.A. et al. Anti-Trypanosoma and toxicity potential of the extracts of Acacia nilotica, Bombax buonopozense and Khaya senegalensis. ADV TRADIT MED (ADTM) 21, 143–150 (2021). https://doi.org/10.1007/s13596-020-00438-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13596-020-00438-6