Abstract
Objective
The objective of the study was to evaluate the benefit of adjuvant chemoradiation compared to adjuvant chemotherapy for resected pancreatic head cancer.
Methods
Three hundred thirty-nine patients (2000–2012) had pancreatoduodenectomy for pancreatic cancer. Chemotherapy was gemcitabine or 5-fluorouracil (5-FU) and radiotherapy was 45–54 Gy. Locoregional recurrences (LRR) were operative bed or regional nodal failures. Logistical regression, Kaplan-Meier estimates, and log-rank tests were used for statistics.
Results
One hundred thirty patients had resection alone (A), 84 had adjuvant chemotherapy (B), and 129 had adjuvant chemoradiation (C). Median follow-up and median survival (MS) for all patients was 17.5 and 19.5 months, respectively. MS for groups A, B, and C were 13, 23, and 26 months, respectively. Groups B and C had R1 resection rates of 37 and 39 % (p = ns). LRR was 60, 63, and 38 % and distant failure was 64, 65, and 66 % for groups A, B, and C, respectively. Group C had significantly lower LRR compared to group B (p = 0.01); however, survival between groups B and C was not statistically different (p = 0.23). On univariate analysis, LRR (p = 0.0038), N-category (p < 0.0001), perineural invasion (PNI; p = 0.007), and R1 resection (p = 0.018) were significant predictors of survival. Multivariable analysis (MVA) showed that LRR (p = 0.004) and N-category (p = 0.01) were predictors of survival. On subgroup analysis, there was improved survival in group C vs B in patients with R1 resection, MS of 27 vs 16 months, respectively (p = 0.01), and in patients with lymph node ratio (LNR) ≤0.2 who had ≥8 LN dissected, MS of 32 vs 24 months (p = 0.04).
Conclusion
Adjuvant chemoradiation significantly decreases LRR in resected pancreatic cancer patients compared to adjuvant chemotherapy. Significant predictors of survival on MVA were LRR and N-category. Additionally on subgroup analysis, chemoradiation improved survival over chemotherapy with a (1) positive surgical margin and/or (2) LNR ≤0.2 with ≥8 LNs dissected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic cancer is the fourth highest cause of cancer mortality in the USA. Surgery remains the only potentially curative treatment, and despite improvements in technique and perioperative care, survival is generally 5 % at 5 years for all stages [1]. Only 15–20 % of pancreatic cancer patients have resectable disease and both local and distant recurrences occur frequently after definitive treatment [2, 3]. Adjuvant treatment with either chemotherapy or chemoradiation has improved survival in both randomized and non-randomized studies; however, optimal adjuvant management remains controversial [1, 4–6] despite continued efforts to develop modern clinical trials.
While meta-analysis data show that adjuvant chemotherapy improves survival, inconsistent results, mixed interpretations, and different pathologic definitions (i.e., R1 definition) have not completely settled the controversy of optimal adjuvant treatment. Despite pancreatic cancer having a high proportion of distant recurrence [2, 7, 8], there is likely a subset of patients with a higher risk of locoregional recurrence for which adjuvant chemoradiation would provide a higher benefit [5]. Clinical factors that predict for optimal survival include patient age, T-category, N-category, and extent of resection [9], yet clinical factors to select patients that would most benefit from adjuvant chemoradiation are lacking.
In this single-institution series, we update previous published results [10] and compare outcomes of patients with resected head of pancreas adenocarcinoma that received adjuvant chemotherapy or adjuvant chemoradiation to define clinical factors that are most predictive of a benefit for adjuvant chemoradiation.
Methods
Patients with resected primary malignancy of the pancreatic head (2000–2012) were included in this IRB approved single-institution series. All patients were included and were non-selected. Patients underwent a classic or pylorus preserving pancreatoduodenectomy (PD) with no gross residual disease noted on operative report. Pathology specimens were reported using a standardized institutional pathology template for pancreatic cancer derived from the College of American Pathologists (CAP). Almost all (98.5 %) patients received a lymph node dissection with involved and total lymph nodes reported. Resected margins were defined as positive by the 0 mm definition (tumor cells at the inked border), and close margins were defined by tumor within 1 mm of the inked border. Surgical margins evaluated were pancreatic, peripancreatic, bile duct, retroperitoneal/uncinate/SMV, portal vein, distal duodenal, and proximal duodenal. Perineural invasion (PNI), lymphovascular space invasion (LVSI), and histologic grade were also reported in addition to the number of lymph nodes with disease and lymph nodes dissected.
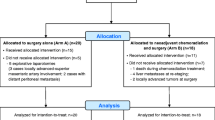
Patients were grouped based on adjuvant treatment received: no adjuvant treatment (group A), adjuvant chemotherapy with 5-fluorouracil (5-FU) or gemcitabine (group B), or adjuvant chemoradiation with concurrent 5-FU or gemcitabine and planned daily radiotherapy to 45–54 Gy using three-dimensional conformal radiotherapy (3D-CRT) or intensity-modulated radiation therapy (IMRT) (group C). Adjuvant therapy was either completed at our institution or referred to other treatment centers. Outcomes and survival were recorded from retrospective chart review and the Social Security Death Index (SSDI). Patients receiving neoadjuvant treatment were excluded.
Statistical analysis
Statistical analyses were performed using JMP Pro v10 (SAS, Cary, NC). Summary statistics and difference tests were obtained from χ 2 analysis. The primary endpoint of our study was overall survival defined from the date of PD to documented death. Kaplan-Meier-estimated survival with statistical significance was determined by log-rank tests. Univariate analyses correlated patient, tumor, and treatment factors to recurrence and survival. Multivariable analysis was based on significant factors from univariate analysis and constructed using a forward planning approach; factors which were associated with higher risk features were also tested in our multivariable models. Patients with missing data were excluded from univariate and multivariable analyses. Lymph node ratio (LNR) was defined by the number of positive lymph nodes dissected compared to the total lymph nodes dissected.
Results
Three hundred thirty-nine patients met inclusion criteria with no significant difference in patient and tumor factors between the groups except for a higher percentage of T1 tumors and adenocarcinomas in group C and a higher percentage of T3 tumors in group B (Table 1). The median number of lymph nodes dissected was 13. Median follow-up was 17.5 months and median survival was 19.5 months. Groups A, B, and C had median survivals of 13, 24, and 26 months, respectively.
To analyze the difference in adjuvant treatment, we considered differences between groups B and C. Figure 1 presents Kaplan-Meier survival curves for groups B and C with median survivals of 24 and 26 months, respectively (p = 0.24). Locoregional recurrence (LRR) was significantly lower for group C compared to group B (p = 0.01) and distant recurrence was not significantly different (Table 1). Twenty-one patients (18 %) had LRR without distant metastases. Additionally, in patients who had adjuvant chemoradiation and did not have locoregional recurrence, there was a statistically significant improvement in survival (Fig. 2).
Kaplan-Meier survival curve for patients treated with a adjuvant chemotherapy and b adjuvant chemoradiation with curves grouped by no LRR (black solid line) vs LRR (gray dashed line). Median survivals are a 16 vs 22 months (p = 0.85) and b 31 vs 23 months (p = 0.0007) for no LRR and LRR, respectively
On univariate proportional hazards modeling, LRR (p = 0.0038), N-category (p < 0.0001), PNI (p= 0.007), and positive margin (p = 0.018) were significant predictors of survival. Subgroup analysis showed a survival benefit for patients with a positive margin who received adjuvant chemoradiation (Fig. 3). Median survivals in patients receiving adjuvant chemotherapy were 25 vs 25 months (p = 0.79) for margin positive and negative, respectively. For those who received adjuvant chemoradiation, median survival was 31 vs 23 months (p = 0.008) for margin positive and margin negative, respectively. Additionally, there was a median survival improvement from 20 to 47 months in the subset of N0 patients with close margins (≤1 mm) who received adjuvant chemoradiation compared to adjuvant chemotherapy alone (p = 0.04). Additionally, for the subset of patients who had LNR >0.2, median survival was 27 months while for patients with LNR ≤0.2, median survival was 18 months. In the favorable subgroup of patients with LNR ≤0.2 in patients with ≥8 lymph nodes dissected, there was a statistically significant survival difference between groups B and C (Fig. 4, p = 0.04). Within group B, there was no significant survival difference between patients receiving 5-FU or gemcitabine, and within group C, there was no significant difference between patients receiving IMRT vs 3D-CRT. However, we do note that only about 20 % of patients treated at our institution were treated with IMRT.
Kaplan-Meier survival curve for patients treated with a margin negative and b microscopic margin positive with curves grouped by adjuvant chemotherapy (black solid line) vs adjuvant chemoradiation (gray dashed line). Median survivals are a 25 vs 25 months (p = 0.79) and b 31 vs 23 months (p = 0.008) for adjuvant chemotherapy and adjuvant chemoradiation, respectively
Kaplan-Meier survival curve for patients treated with a LNR ≤0.2 and ≥8 lymph nodes dissected and b all other patients with curves grouped by adjuvant chemotherapy (black solid line) vs adjuvant chemoradiation (gray dashed line). Median survivals are a 24 vs 32 months (p = 0.04) and b 22 vs 23 months (p = 0.83) for adjuvant chemotherapy and adjuvant chemoradiation, respectively
On multivariable proportional hazards modeling, LRR (p = 0.004) and N-category (p = 0.01) remained significant predictors of survival (Table 2).
Discussion
This large single-institution series of pancreatic head cancers presents data comparing outcomes and survival between patients that received adjuvant chemotherapy and adjuvant chemoradiation after surgery. On multivariable analysis, the significant factors predicting for patient survival were LRR and N-category. While adjuvant chemoradiation significantly reduces LRR overall compared to adjuvant chemotherapy, subsets of patients with the highest risk of local recurrence may draw the most benefit from adjuvant chemoradiation. These groups include M0 patients with positive surgical margin (R1 resection) and/or patients with LNR ≤0.2 who have ≥8 lymph nodes dissected.
Group 1 (no adjuvant treatment) included patients that died before receiving adjuvant therapy, refused adjuvant treatment, lost to follow-up, or unknown adjuvant treatment. As expected, comparison of group 1 with groups 2 and 3 showed a statistically significant improved survival; improved survival with the addition of adjuvant treatment has been consistently demonstrated [4, 5, 10, 11]. Two reports have noted that the survival benefit was most significant for negative surgical margins, node positivity, and tumors >3 cm. Regardless of other tumor-related factors, modern treatment recommendations include an upfront adjuvant recommendation for chemotherapy or chemoradiation.
Understanding an individual patient’s patterns of failure would help guide adjuvant treatment recommendations. For example, a patient who is likely to recur locally would get chemoradiation. As adjuvant chemoradiation significantly reduces LRR, the patients with the highest risk of LRR will likely gain the most benefit in terms of survival and morbidity from additional procedures and symptoms related to a LRR. While molecular profiling promises to help elucidate this subset [6], clinical parameters have been used to guide adjuvant therapies for pancreatic cancer patients.
However, the choice between adjuvant chemotherapy and chemoradiation remains controversial [5, 12]. Randomized data and meta-analysis have concluded that adjuvant chemotherapy should be standard as there was no reported survival benefit for adjuvant chemoradiation over chemotherapy, but these data are not free of criticism. For example, the ESPAC 1 trial results were confounded by a few factors including background treatments (including radiotherapy) that were not part of the initial trial design, making the results difficult to interpret. To contrast these results, other reports have described improved survival for adjuvant chemoradiation over adjuvant chemotherapy [13]. Meta-analysis data does show a trend to improved survival in R1 resection patients receiving adjuvant chemoradiation compared to adjuvant chemotherapy, but this result was not statistically significant [12] likely due to non-standard pathology specimen review and non-standard definition of a positive margin between the included trial data. For example, it is unclear how well these pathologic specimens were evaluated, especially considering that modern standardized pathologic assessment increases the reported R1 resection status [14, 15].
A concern with meta-analysis and multi-institutional data is that it addresses a heterogeneous population compared with a single-institution experience. Thus, large single-institution series consistently using standardized pathology reporting have helped guide modern adjuvant recommendations. One such result from the Johns Hopkins data is the independent prognostic LNR threshold of 0.2 [16]. Other possible predictors conferring a worse outcome include higher T-category, LNR, histologic grade, and positive surgical margin [17, 18].
In our single-institution analysis, multivariable analysis showed that LRR and N-categorization are important factors that predict for improved survival. While chemoradiation reduced the rate of LRR, chemoradiation itself did not remain significant on multivariable analysis. This presents an interesting dilemma. While median survival did improve by 2 months with chemoradiation vs chemotherapy in our series, it did not statistically reach significance. Most patients in this series received radiotherapy using 3D-CRT. Additionally, only 75 % of patients in our series received 45 Gy or higher suggesting that with modern and high-quality treatment planning delivering conformal radiotherapy to higher doses, outcomes may be even better [19]. Our interpretation is that there may be a role for well-targeted and more aggressive local therapy to reduce the rate of local recurrence and in turn improve overall survival. Newer radiotherapy techniques including IMRT and potentially SBRT may be able to achieve this while reducing toxicity and may achieve a better correlation between adjuvant chemoradiation and survival.
On subgroup analysis, one significant factor from our analysis is a positive surgical margin (R1 resection). A positive surgical margin is correlated with the development of LRR, and R1 patients who did not receive adjuvant chemoradiation had worse survival. Patients who received adjuvant chemotherapy had a median survival of 16 months; however, patients with R1 resection who received adjuvant chemoradiation had a median survival (24 months) equivalent to patients with an R0 resection. When we considered patients with close margins (≤1 mm), there was an improved survival trend, but this was not statistically significant; this is consistent with other published reports [20]. The close margin subset likely represents a combination of patients who truly have a positive margin and a subset of those who do not.
For those patients with regional nodal disease (N1), we hypothesized that a lower LNR may be a proxy for lower metastatic disease burden and thus the benefit of adjuvant chemoradiation may be more significant. From previous studies, LNR ≤0.2 has been prognostic for better survival with at least 10–12 lymph nodes dissected [21]. From the present study, on subgroup analysis, patients who have LNR ≤0.2 with ≥8 lymph nodes dissected have a significant survival benefit with adjuvant chemoradiation compared with adjuvant chemotherapy alone.
Limitations to this review include its retrospective nature and that, for some patients, particular details of treatment were unknown. In addition, common biases associated with retrospective series should be considered. Despite these limitations, this report presents compelling evidence that LRR plays a significant role in pancreatic cancer patient survival and that adjuvant chemoradiation has an important role in well-selected resectable pancreatic cancer patients. Additional studies are needed to validate our findings.
Conclusion
Grossly resected pancreatic head adenocarcinoma has a high rate of distant failure, but patients may still have a significant risk of locoregional recurrence. Adjuvant chemoradiation is effective in significantly reducing the rate of locoregional recurrence compared to adjuvant chemotherapy. Locoregional recurrence and N-category were significantly correlated with patient survival. On subset analysis, patients with R1 resection and/or LNR ≤0.2 who had ≥8 lymph nodes may derive the most benefit from adjuvant chemoradiation.
References
Hartwig W et al (2013) Improvement of surgical results for pancreatic cancer. Lancet Oncol 14:e476–e485. doi:10.1016/S1470-2045(1013)70172-70174
Hishinuma S et al (2006) Patterns of recurrence after curative resection of pancreatic cancer, based on autopsy findings. J Gastrointest Surg 10:511–518
Whittington R et al (1991) Adjuvant therapy of resected adenocarcinoma of the pancreas. Int J Radiat Oncol Biol Phys 21:1137–1143
Corsini MM et al (2008) Adjuvant radiotherapy and chemotherapy for pancreatic carcinoma: the Mayo Clinic experience (1975–2005). J Clin Oncol 26:3511–3516
Stocken DD et al (2005) Meta-analysis of randomised adjuvant therapy trials for pancreatic cancer. Br J Cancer 92:1372–1381
O’Reilly EM (2013) Adjuvant therapy for pancreas adenocarcinoma. J Surg Oncol 107:78–85
Hattangadi JA et al (2009) Results and patterns of failure in patients treated with adjuvant combined chemoradiation therapy for resected pancreatic adenocarcinoma. Cancer 115:3640–3650
Winter JM et al (2013) Failure patterns in resected pancreas adenocarcinoma: lack of predicted benefit to smad4 expression. Ann Surg 258:331–335
Moghanaki D et al (2011) Resection status, age and nodal involvement determine survival among patients receiving adjuvant chemoradiotherapy in pancreatic adenocarcinoma. JOP 12:438–444
Kim R et al (2010) A single institution review of adjuvant therapy outcomes for resectable pancreatic adenocarcinoma: outcome and prognostic indicators. J Gastrointest Surg 14:1159–1169
Herman JM et al (2008) Analysis of fluorouracil-based adjuvant chemotherapy and radiation after pancreaticoduodenectomy for ductal adenocarcinoma of the pancreas: results of a large, prospectively collected database at the Johns Hopkins Hospital. J Clin Oncol 26:3503–3510. doi:10.1200/JCO.2007.3515.8469
Butturini G et al (2008) Influence of resection margins and treatment on survival in patients with pancreatic cancer: meta-analysis of randomized controlled trials. Arch Surg (Chicago, Ill: 1960) 143:75–83, discussion 83
Kooby DA et al (2013) Impact of adjuvant radiotherapy on survival after pancreatic cancer resection: an appraisal of data from the national cancer data base. Annals Surg Oncol
Gnerlich JL et al (2012) Microscopic margins and patterns of treatment failure in resected pancreatic adenocarcinoma. Arch Surg (Chicago, Ill: 1960) 147:753–760
Rau BM et al (2012) R1 resection in pancreatic cancer has significant impact on long-term outcome in standardized pathology modified for routine use. Surgery 152:S103–S111
Wentz SC et al (2012) Lymph node ratio and preoperative ca 19–9 levels predict overall survival and recurrence-free survival in patients with resected pancreatic adenocarcinoma. World J Gastrointest Oncol 4:207–215
Zhang Y et al (2012) Loco-recurrence after resection for ductal adenocarcinoma of the pancreas: predictors and implications for adjuvant chemoradiotherapy. J Cancer Res Clin Oncol 138:1063–1071
Asiyanbola B et al (2009) Determining pattern of recurrence following pancreaticoduodenectomy and adjuvant 5-flurouracil-based chemoradiation therapy: effect of number of metastatic lymph nodes and lymph node ratio. J Gastrointest Surg 13:752–759
Hall WA et al (2013) The influence of adjuvant radiotherapy dose on overall survival in patients with resected pancreatic adenocarcinoma. Cancer 119:2350–2357
Konstantinidis IT et al (2013) Pancreatic ductal adenocarcinoma: is there a survival difference for r1 resections versus locally advanced unresectable tumors? What is a “true” r0 resection? Ann Surg 257:731–736
Pawlik TM et al (2007) Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery 141:610–618
Conflict of interest
All authors declare that they have no conflict of interest.
Ethics statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, A.M.S., Falk, G.A., Pelley, R. et al. Adjuvant chemoradiation may improve survival over adjuvant chemotherapy in resected pancreatic cancer patients who are high risk for locoregional recurrence. J Radiat Oncol 4, 271–276 (2015). https://doi.org/10.1007/s13566-015-0186-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-015-0186-7