Abstract
Introduction
Limited evidence is available on real-world management of atopic dermatitis (AD) among Asian adults. This cross-sectional study aimed to assess current approaches in AD diagnosis and management in Asia.
Methods
Practising dermatologists regularly treating patients with moderate-to-severe AD were recruited from eight Asia–Pacific territories, namely Mainland China, Hong Kong, India, Japan, Singapore, South Korea, Taiwan, and Thailand. A survey was administered to eligible dermatologists after screening and taking informed consent. Data from fully completed submissions were analysed using descriptive statistics. The study was reviewed by the institutional review board in each territory.
Results
Data from 271 dermatologists were included for analysis. About one-third (31.7%) reported that they referred to the Hanifin and Rajka criteria during diagnosis. The majority of dermatologists used clinical impression when assessing AD severity and treatment response. Reduction of eczema and pruritus was the primary treatment objective when managing both acute (98.1%) and chronic (69.1%) AD. More than half of dermatologists preferred adding systemic anti-inflammatory medication for patients who did not respond to maximized topical treatment, while 43.6% would switch to another systemic medication for those failing to respond to maximized systemic treatment. Topical corticosteroids were frequently selected by dermatologists. For systemic therapies, oral corticosteroids were most frequently used, followed by cyclosporin and dupilumab. Narrow-band ultraviolet B was the most common phototherapy reported (84.9%). There was considerable variation in estimated average and maximum durations of therapies used to treat AD.
Conclusion
This study has provided insights on the real-world management of moderate-to-severe AD in the Asia–Pacific region. The diverse approaches in diagnosis and treatment highlight the multifactorial nature of AD, reliance on clinical judgement, and importance of personalized care. To improve outcomes in patients with AD, it will be crucial to develop biomarkers for diagnosis, reduce subjectivity in assessment, as well as promote access to newer and effective therapies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
A multinational cross-sectional survey was conducted among dermatologists to assess current approaches in atopic dermatitis (AD) diagnosis and management in Asia. |
Dermatologists commonly used the Hanifin and Rajka criteria, local guidelines, and their clinical impression to diagnose AD. |
For patients who did not respond to maximized topical treatment, dermatologists preferred to add on systemic anti-inflammatory medication. |
Topical corticosteroids were most frequently selected for AD management, while narrow-band ultraviolet B was the most common phototherapy used. |
For systemic treatment, oral corticosteroids were most commonly selected, followed by cyclosporin and dupilumab. |
There was considerable variation in reported average and maximum durations of therapies used to treat AD. |
Introduction
Atopic dermatitis (AD) is a common chronic and relapsing inflammatory skin disease that affects people of all ages and ethnicities. Although often considered a childhood disease, AD affects a significant number of adults, with a prevalence of up to 10% in developed countries [1] and an increasing trend in developing countries [2]. In the Asia–Pacific region, some countries (e.g. Singapore, Malaysia) have a higher prevalence of AD in adults than other countries (e.g. China), possibly due to higher rates of disease onset in adulthood [3]. AD is the leading cause of global burden from skin disease which significantly impacts patients’ quality of life, causing symptoms such as erythema, edema, xerosis, and pruritus [4, 5]. It is also associated with substantial psychosocial issues such as sleep disturbance, depression, and anxiety, contributing to work absenteeism and decreased productivity [6,7,8]. For those with moderate-to-severe AD, the worsening symptoms bring about heavier psychological and economic burden [9]. These patients may also suffer from concomitant atopic (e.g. asthma, food allergy) and/or non-atopic comorbidities (e.g. anxiety, depression).
The pathogenesis of AD is multifactorial and involves the complex interplay of impaired skin barrier function, immune dysregulation, genetic susceptibility, and environmental factors. Currently, there is no cure for AD. Disease management goals include symptom reduction and flare prevention [10]. While many patients respond to basic skin care (e.g. emollients), environment control, and topical medications including topical corticosteroids (TCS) and calcineurin inhibitors (TCIs), a significant percentage of them have recalcitrant disease which requires more holistic and systemic treatment [11]. Adults with moderate-to-severe AD refractory to topical treatments may be considered for phototherapy, which involves exposing the skin to specific wavelengths of ultraviolet (UV) light under controlled conditions [12]. In addition, systemic drugs such as corticosteroids and biologics taken orally or injected to manage moderate-to-severe AD are also considered when topical treatments are ineffective [12]. Although treatment guidelines are available, adherence to recommendations (especially systemic treatments) is low in Asian countries [13]. A previous review across several continents including Asia revealed that treatment modalities can vary across countries, potentially due to differences in patient preferences, availability of new therapies in the market, and multiple existing guidelines recommended for AD treatment [13]. For example, TCIs are recommended as first-line treatment in various guidelines including the ones adopted in the Middle East and Latin America, whereas they are recommended as second-line treatment in other guidelines more commonly used in Asia.
To date, the available evidence on real-world management of moderate-to-severe AD among Asian adults remains limited. The variability in diagnostic criteria, treatment preferences, and clinical decision-making may lead to inconsistencies in patient care and outcomes. This cross-sectional study aims to address this gap by evaluating the real-world practices in the diagnosis and treatment of moderate-to-severe AD, providing a comprehensive picture of the patient’s journey from diagnosis to treatment.
Methods
Setting
Practising dermatologists who regularly treat patients with AD were recruited from eight Asia–Pacific territories, namely Mainland China, Hong Kong, India, Japan, Singapore, South Korea, Taiwan, and Thailand. Ethical approval was received from the following institutional review boards (IRBs): Korea University Ansan Hospital, Chulalongkorn University, Father Muller Hospital, NPO MINS, National Taiwan University Hospital, Hong Kong Doctors Union, and Sir Run Run Shaw Hospital. The Parkway Independent Ethics Committee granted an exemption from review. The study was conducted in accordance with the protocol, Guidelines for Good Pharmacoepidemiology Practices, and the Declaration of Helsinki. All participants provided informed consent.
Study Population
To be eligible for participation, a physician was required to have at least 2 years of experience as a board-certified dermatologist, treat an average of two or more adult patients with moderate-to severe AD per month, and spend at least 60% of their working time in direct patient care (equivalent to three out of five working days).
We identified potential participants through physician panels, contact lists, and other relevant directories/databases in each territory of interest. Contact was established with eligible dermatologists via a study invitation email containing materials including links to screener, participant information sheet, informed consent form, and survey questionnaire. Interested physicians underwent a screening process to confirm their eligibility. All participants received fair compensation for their time spent in completing the survey.
Study Instrument
The survey was designed to capture information related to AD diagnosis and management from the perspective of practising dermatologists. Items to be included in the questionnaire were initially developed on the basis of a comprehensive literature review which included systematic reviews, clinical guidelines, and key primary studies focused on the management of moderate-to-severe AD in adult patients [14,15,16]. These proposed items were then selected by members of a steering committee (StC) on the basis of their clinical knowledge to ensure relevance and accuracy within the local context. The StC, comprising one dermatology expert from each territory, totalling eight members, was formed as part of the research team. The StC played a critical role in validating the study design and refining study materials. Multiple online meetings with the StC members were conducted to improve the clarity, comprehensibility, and clinical relevance of the survey questionnaire. Specific suggestions included rephrasing ambiguous questions, adding options for commonly used diagnostic criteria, and ensuring that the treatment options are appropriate in local context and able to comprehensively cover all common therapies used in the included territories. Subsequently, the questionnaire was revised by incorporating feedback from the StC and translated into local languages by a professional translation agency. The translated study materials were reviewed by the IRB in each territory. After IRB approval was obtained, the local language version of the survey was piloted among two dermatologists (including one StC member and one eligible dermatologist) from each territory to ensure that there was no issue with language and survey programming. The survey was then finalized, and enrolment continued.
The 33 items in the questionnaire were finalized and sorted into three sections: diagnosis of moderate-to-severe AD (6 items), overall management (7 items), and specific treatment options (20 items). For the purpose of results interpretation, moderate-to-severe AD was defined as a condition not adequately controlled by standard and optimised topical treatment (including emollients, TCS, and TCI), apart from occasional short-term flares caused by factors such as skin infection [16]. The detailed questionnaire is included in the Supplementary Materials.
Data Collection
The survey was administered from March to June 2023. During data collection, we observed varied responses rates across different territories, with some regions showing lower participation. To address this, we extended the data collection period and used multiple channels (e.g. emails, phone calls) to reach out to potential participants. To reduce selection biases, dermatologists were randomly invited from physician panels and relevant directories in each territory to ensure a more representative sample. In addition, participants’ identities were kept confidential to avoid response bias. The questionnaire was pilot tested among a small group of dermatologists, including StC members, to refine the questions and improve clarity. Data from the pilot phase were excluded from the final analysis.
Statistical Analysis
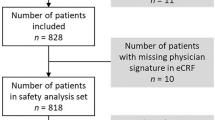
Only data from fully completed submissions were analysed using descriptive statistics. Categorical variables were reviewed for consistency and encoded appropriately. Where applicable, integer values were assigned to categories of an ordinal variable based on their order, while each category of a nominal variable was represented using binary values in a separate column. Categorical variables were presented using frequencies and percentages, while continuous variables were presented using medians and interquartile ranges (IQRs).
Results
A total of 271 dermatologists from eight territories were included for analysis. As presented in Table S1 (see Supplementary Materials), more than half (59.0%) had more than 10 years of post-training experience in AD management. The recruited dermatologists reported that they treat a median of 30 (IQR 50.0) patients with moderate-to-severe AD monthly. The majority practised in university teaching hospitals (32.8%), followed by public or government hospitals (26.9%), private clinics (26.2%), and private hospitals (15.2%).
Diagnosis of AD
Higher proportions of dermatologists reported that they referred to the Hanifin and Rajka criteria (31.7%) and local guidelines (27.7%), compared to other international guidelines; 21.4% of them also indicated that their diagnosis of AD was based on their own clinical judgment or impression (Table 1). The majority assessed the severity of AD on the basis of clinical impression (74.5%), instead of subjective symptoms only or utilizing existing severity measurement scales such as the Eczema Area and Severity Index (EASI) and Scoring atopic dermatitis (SCORAD). Similarly, more dermatologists used clinical impression (61.3%) than scoring tools (55.7%) when differentiating between mild and moderate-to-severe AD. When asked about how they would define a flare, most dermatologists defined it as the return of symptoms (80.4%), or an episode requiring either escalation of treatment or seeking additional medical advice (74.2%).
Among the total of 271 dermatologists, 258 provided responses on the frequency of clinical tests performed for diagnosing AD, while 13 indicated that they have never conducted any test. As shown in Table 2, serum IgE and differential blood count were the most frequently conducted tests, with 121 (46.9%) and 113 (43.8%) dermatologists performing them for more than 50% of the time, respectively. Patch testing, skin biopsies, potassium hydroxide preparation, and skin prick test were less commonly used, with over 80% of dermatologists reporting that they either never used these tests or used them for less than 25% of the time. Genetic testing was least frequently used, with 83.3% of dermatologists indicating that they did not utilize it at all.
Management of AD
Almost all dermatologists (97.8%) indicated that they routinely distinguish between acute and chronic phases of AD during their clinical practice. The reduction of eczema and pruritus was the primary treatment objective when managing both acute (98.1%) and chronic (69.1%) AD. While promoting healthy skin lesions was identified as a prominent objective in treating acute AD (57.7%), the management focus shifted towards enhancing productivity in daily activities for chronic AD (46.0%). In both conditions, preventing exacerbations remained a key priority, with 47.2% and 64.9% of physicians indicating this for acute and chronic AD, respectively. More details are presented in Fig. S1 (see Supplementary Materials).
Figure 1a illustrates the treatment preferences of dermatologists when managing adult patients with moderate-to-severe AD who did not respond to maximized topical treatment. Of all surveyed dermatologists, 265 (97.8%) would add on treatment for such patients. Among them, the majority (50.9%) favoured using systemic anti-inflammatory medication as the primary or first choice add-on treatment option. This was followed by phototherapy (26.8%), biologics (17.0%), and small molecules (3.0%). Figure 1b shows the preferred strategies for patients who did not respond to maximized systemic treatment, based on responses from 257 (94.8%) dermatologists. For this group, the most common choice was switching to another systemic medication (43.6%). Other alternatives included augmenting treatment with phototherapy (20.6%), adding another systemic treatment (17.5%), or supplementing with topical treatments (16.7%). Few of them expressed preference for switching to phototherapy as their primary option.
The main reasons for dermatologists’ choice of different add-on agents when managing patients with moderate-to-severe AD who were not responding to maximized topical treatment are shown in Table S2 (see Supplementary Materials). When asked about the main reason for choosing systematic anti-inflammatory medication as their first choice, the majority of 135 dermatologists who selected this treatment reasoned that it costs less (39.3%) or has higher efficacy (34.1%) than other therapies. Other dermatologists indicated phototherapy, biologics, and small molecules as their most preferred add-on treatment options mainly due to relatively fewer side effects, compared to systemic anti-inflammation medication.
As presented in Table 3, most dermatologists (76.8%) evaluated the patient’s response to treatment based on clinical judgment or observation, including the pattern and distribution of skin lesions. In addition, some dermatologists (18.5%) utilized scoring tools, while a smaller percentage (4.8%) relied on patient’s self-reported symptoms as their primary method. Treatment failure was predominantly defined as no improvement in clinical efficacy after continuous treatment for 3 months and 1 month by 49.1% and 47.1% of dermatologists, respectively.
Topical Treatment
Topical agents serve as the cornerstone of AD management, often complemented by systemic or phototherapy in moderate-to-severe cases. When addressing acute flares, a comparatively higher proportion of dermatologists (43.5%) chose high-potency TCS for non-sensitive areas (Fig. 2a), while a respective 35.1% and 35.8% favoured medium-potency and low-potency TCS for sensitive areas (Fig. 2b). For treatment of chronic AD, high-potency (28.4%) and medium-potency (26.9%) TCS were predominantly selected as the top choices for non-sensitive areas (Fig. 2c). However, low-potency TCS (30.6%) and tacrolimus (29.5%) were the preferred options for treating sensitive areas (Fig. 2d).
Relative reported priority of atopic therapies in the management of a non-sensitive areas in patients with acute flares, b sensitive areas in patients with acute flares, c non-sensitive areas in patients with chronic AD, and d sensitive areas in patients with chronic AD. AD atopic dermatitis, TCS topical corticosteroid. Crisaborole was unavailable in some markets including India, Japan, Thailand, and Korea at the time of the survey
Super high-potency TCS were used by some dermatologists as most preferred treatment for non-sensitive areas in both acute and chronic AD (24.4% and 15.9%, respectively), although their application in sensitive areas was much less frequently reported. Most dermatologists also did not report use of crisaborole as treatment for acute or chronic AD.
Phototherapy
Figure 3 shows that the majority (84.9%) of dermatologists chose narrow-band ultraviolet B (NB-UVB) as their most preferred modality and broad-band UVB as second choice (31.7%). Although the combination of psoralen and long-wave ultraviolet A (PUVA) was rarely indicated as the most preferred agent, it was ranked as the third choice (24.7%). High proportions of dermatologists indicated that they would never consider the use of UVA1 and UVA (TL09) (79.3% and 73.8%, respectively).
Systemic Treatment
As shown in Fig. 4, oral steroids (39.9%) emerged as the most commonly selected systemic treatment agent, ahead of alternatives including cyclosporin, dupilumab, methotrexate, azathioprine, and upadacitinib. Notably, cyclosporin was frequently utilized as either the second (24.0%) or third (17.7%) choice for systemic treatment. In contrast, the usage of mycophenolate mofetil appeared to be limited. Systemic omalizumab, rituximab and abrocitinib, apremilast, baricitinib and upadacitinib were rarely selected (data not shown in figure).
Figure 5a shows marked differences in the average duration of treatment among agents. Among dermatologists who opted for oral steroids, the typical prescription duration averaged less than 1 month. Conversely, dermatologists indicated longer treatment timeframes for azathioprine, cyclosporin, and mycophenolate mofetil, typically spanning 3–6 months. Notably, a considerable proportion of dermatologists reported using cyclosporin and mycophenolate mofetil for a maximum of 7–12 months, compared with 1–2 months for oral steroids, 3–6 months for azathioprine and methotrexate (Fig. 5b). However, some indicated that the maximum duration for using oral steroids exceeded 3 months, and in certain instances it was more than 1 year.
Discussion
To the best of our knowledge, this multinational cross-sectional study is the first to capture information on diagnosis and treatment approaches for moderate-to-severe AD across eight Asia–Pacific territories. We found that diagnostic practices frequently incorporated the Hanifin and Rajka criteria, local guidelines, and serum IgE test results. When assessing severity of AD, most dermatologists leaned heavily on clinical impression rather than more objective scoring tools. In cases where topical treatments were insufficient, dermatologists predominantly opted for adding systemic anti-inflammatory medication because of their lower costs and higher efficacy. Clinical judgment also played a central role in assessing treatment response. The diverse preferences for topical treatment, systemic treatment, and phototherapy indicate diverse AD management and practices in the region. Dermatologists frequently chose between different potencies of TCS on the basis of the nature (acute vs. chronic) and location (sensitive vs. non-sensitive area) of AD. Oral steroids were commonly selected as systemic therapies, while NB-UVB was the most common form of phototherapy used.
Our study showed that dermatologists practising in the Asia–Pacific region often relied on clinical judgment, local guidelines, and a range of clinical tests, particularly serum IgE levels when diagnosing AD. These findings align with the multifactorial nature of AD [5]. Existing guidelines in the USA highlight the importance of considering individual patient characteristics in clinical practice [5]. The detection of total and specific IgE antibodies to inhalant and/or food allergens is one important aspect in diagnosing AD, though concerns about its limited clinical relevance and low specificity exist [17]. Incorporating possible differential diagnoses into assessment has been recommended to exclude various skin diseases (e.g. allergic contact eczema, microbial eczema, cutaneous lymphoma) that clinically resemble AD and could be associated with increased total serum IgE [18]. Use of clinical judgment based on the presence and distribution pattern of lesions with specific morphologic features, relevant clinical findings, and personal or family medical history is in line with recommendations from various sources from Europe [19,20,21]. This emphasizes the critical role of holistic assessment including clinical judgment combined with other tests in the accurate diagnosis of AD.
The diversity in use of diagnostic criteria (e.g. Hanifin and Rajka, American Academy of Dermatology, local guidelines) suggests that none of these criteria are considered wholly or mutually exclusive in the diagnosis of AD. Dermatologists may also depend on their clinical experience to make the final diagnosis. In particular, the Hanifin and Rajka criteria were used by a considerable proportion of physicians in our study. This could reflect that respondents are experienced dermatologists who are familiar with the classical criteria, which include precise description of the skin disorder. Additionally, this may be due to its frequent use in randomized controlled trials (RCTs), as reported by a systematic review of AD diagnostic criteria [22]. Both our study and the review indicate a similar lack of uniformity in AD diagnosis [22].
To date, topical treatments are deemed the mainstay of AD therapy [12, 23]. Consistent with existing evidence in Europe, our findings suggest that adults with moderate-to-severe AD refractory to topical treatments are considered for add-on therapy, primarily systemic anti-inflammatory medications such as oral steroids, cyclosporin, and methotrexate [24]. When patients do not respond to maximized systemic treatment or have concerns about adverse effects from continuous usage of the systemic agent, dermatologists preferred switching to another systemic medication. The preference for systemic anti-inflammatory medications as a first choice for add-on treatment echoes guidelines in Europe and the USA [19, 25] and a systematic review [26], reflecting the widespread acceptability of this approach for managing moderate-to-severe AD. However, concerns about their safety profiles remain. To improve long-term management of patients with AD, it is important to continue development of treatment options that are synergistic, effective, fast-acting, and with fewer serious adverse effects.
While some studies have recommended measurement scales, especially EASI and SCORAD, as objective instruments to evaluate the AD severity [27], our study suggests that dermatologists predominantly used clinical assessment and observation to assess skin lesions and determine treatment response. The commonly selected definitions of treatment failure (i.e. no improvement after continuous treatment for 1 vs. 3 months) are likely attributable to expectations regarding a treatment’s onset of action and hence response. Given that the choice of assessment method may impact treatment decisions and patient outcomes [27, 28], additional efforts to standardize AD assessment through guidelines and consensus meetings may be necessary to ensure greater consistency and objectivity in clinical practice.
This study revealed varied dermatologist preferences for topical treatments for AD, influenced by the affected area’s nature and location. For acute flares, super high-potency and high-potency TCS were preferred for non-sensitive body parts where the skin is less delicate or more resilient (e.g. back, chest, outsides of elbows, or fronts of knees) to quickly reduce symptoms [29, 30]. In contrast, for sensitive areas where the skin is delicate and thinner (e.g. face or genital areas), medium to low-potency TCS were chosen to minimize side effects such as skin atrophy, striae, or rosacea [31]. For chronic AD, high-potency TCS continued to be favoured for non-sensitive areas, in line with consensus-based European guidelines that recommend the use of high-potency topical TCS as first-line treatment for moderate-to-severe AD, regardless of the area affected [21]. For sensitive areas, there was a cautious shift towards lower-potency TCS and TCIs (including tacrolimus and pimecrolimus) [32, 33], though their use was less than expected, possibly because of side effects and cost issues [34]. Although newer treatment such as crisaborole (phosphodiesterase 4 inhibitor) has been recommended in some guidelines from the USA [12], our study reported minimal use of it in clinical practice. This is likely due to limited availability and reimbursement in markets including India [35], Japan [36], Korea [37], and Thailand [38].
In addition to topical treatment, NB-UVB was the most preferred phototherapy modality in managing moderate-to-severe AD. It works by suppressing the itch and immune system, and reducing inflammation in the skin [39]. The preference for NB-UVB is supported by its superior efficacy, more favourable side effect profile, and improved re-pigmentation and colour matching, compared with other phototherapies (e.g. PUVA) [40]. Our findings are in alignment with emerging evidence from RCTs, and are consistent with Asia and international guidelines recognizing NB-UVB as an effective AD treatment option [41,42,43,44,45].
Oral corticosteroids, despite their unfavourable long-term risk-to-benefit ratio [46], have emerged as the first-line systemic treatment among most dermatologists. However, as reported by our study participants, they were often prescribed for short durations, typically less than 1 month. Such practice is supported by regional and international guidelines recommending short-term use of systemic steroids for acute flares, but discouraging them from prolonged use [19, 25, 47]. Oral corticosteroids may cause wide-ranging systemic side effects such as weight gain, high blood pressure, diabetes mellitus, adrenal suppression, and osteoporosis. Abrupt discontinuation of systemic corticosteroids may result in withdrawal syndrome, characterized by the extreme recurrence or worsening of generalized AD symptoms and rebound flares [19, 25, 47], occasionally accompanied by adrenal insufficiency. The reported utilization of cyclosporin as the most common second-line option aligns with its immunosuppressive properties [48] and rapid onset of action [49]. Guidelines and real-world studies in Asia [19, 47] and Europe [50,51,52] have also indicated cyclosporin as a suitable alternative for managing moderate-to-severe AD. Meanwhile, other immunosuppressants appeared to be less frequently prescribed. Previous research has demonstrated that azathioprine and mycophenolate mofetil have delayed time to effect in AD treatment, and methotrexate may reach maximum efficacy after 3–4 months even with dose escalation [16]. Dupilumab was the preferred newer systemic treatment, supported by phase 3 trials [53] and real-world settings [54, 55]. However, its limited use in our study could be due to it being reserved for patients who have a poor response to other more established therapies, high costs, and the risk of serious side effects.
Though most dermatologists adhered to recommendations for systemic steroids for a maximum of 6 weeks [56], more than 30% of dermatologists reported using oral steroids for more than 1 month on average and a surprisingly high percentage (37.7%) even estimated the maximum duration to be more than 2 months. This finding may be attributed to factors such as lack of effective alternatives for certain patients with more serious AD, challenges in tapering off medication before another flare, or patient preferences. The reported average and maximum durations with cyclosporin, azathioprine, methotrexate, and mycophenolate mofetil are consistent with guidelines from the Asian Pacific Journal of Allergy and Immunology (APJAI) guidelines [38], suggesting an average of 3–6 months of use, with possible extension up to 12 months with close monitoring. This indicates that some dermatologists considered them as longer-term alternatives to oral corticosteroids. Differences in treatment durations for each systemic agent might reflect variations in prescription practices, with some physicians opting for very low doses over longer periods as maintenance treatment.
The treatment goals were categorized into acute and chronic phases. In the acute phase, goals included reducing dermatitis and itching, and early resolution of symptoms, while the emphasis in the chronic phase was on the minimization of side effects. Other goals were similar in both phases. Many physicians prioritized enhancing productivity in daily activities for chronic AD and preventing exacerbations in both the acute and chronic phases, indicating a need for continuing treatment in the chronic phase. Hence, it is important to promote the use of systemic drugs with superior long-term safety profiles as alternatives to current standard systemic treatments.
This is the first survey study which investigated the treatment approaches of dermatologists across eight Asia–Pacific territories. We received responses from a good cross-section of experienced dermatologists working in various clinical settings. However, there are several limitations to be acknowledged. As our participants were recruited from physician panels, the selected sample may have a stronger interest in research compared with other practising dermatologists. In addition, some patients with AD could be managed by general practitioners, whose clinical management of AD will not be reflected in this study. These, combined with the relatively small sample size in each territory, could limit the generalizability of our findings. Furthermore, this study used a self-reported questionnaire, which is a subjective measure. Although the questionnaire was developed on the basis of existing literature and experts’ opinion, its reliability and validity have not been assessed in the target populations. Self-reporting may introduce measurement error and recall bias, hence potentially affecting the accuracy of our findings. Another limitation is the varying availability of treatments across territories, which may influence dermatologists’ responses. Differences in healthcare access, drug availability, and reimbursement policies could affect treatment choices and management practices. Future research to study drug utilization and management of patients with AD using electronic medical records may be useful to validate our study findings.
Conclusion
Our study has provided insights into the management of moderate-to-severe AD in the Asia–Pacific region. Clinical judgment plays a central role in AD diagnosis, assessment of severity, and treatment response in real-world practice. The diversity in management approaches and choice of medications reflects the inherent multifactorial nature of AD and clinicians’ consideration of individual patient needs. Oral corticosteroids were frequently selected as systemic treatment. However, physicians should avoid prolonged use of oral corticosteroids because of potentially serious adverse effects. With the availability of newer therapies, dermatologists now have more treatment options at their disposal. To improve outcomes in patients with AD, international collaboration among dermatologists, researchers, and policymakers will be crucial to develop useful biomarkers for diagnosis, reduce subjectivity in assessment, and promote more equitable access to novel treatments.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020;396(10247):345–60.
Williams H, Stewart A, von Mutius E, Cookson W, Anderson HR, International Study of Asthma and Allergies in Childhood (ISAAC) Phase One and Three Study Groups. Is eczema really on the increase worldwide? J Allergy Clin Immunol. 2008;121(4):947-54.e15.
Yong AM-Y, Tay Y-K. Atopic dermatitis: racial and ethnic differences. Dermatol Clin. 2017;35(3):395–402.
Carroll CL, Balkrishnan R, Feldman SR, Fleischer AB Jr, Manuel JC. The burden of atopic dermatitis: impact on the patient, family, and society. Pediatr Dermatol. 2005;22(3):192–9.
Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70(2):338–51.
Linnet J, Jemec GBE. An assessment of anxiety and dermatology life quality in patients with atopic dermatitis. Br J Dermatol. 1999;140(2):268–72.
Cheng CM, Hsu JW, Huang KL, et al. Risk of developing major depressive disorder and anxiety disorders among adolescents and adults with atopic dermatitis: a nationwide longitudinal study. J Affect Disord. 2015;178:60–5.
Kiebert G, Sorensen SV, Revicki D, et al. Atopic dermatitis is associated with a decrement in health-related quality of life. Int J Dermatol. 2002;41(3):151–8.
Girolomoni G, Luger T, Nosbaum A, et al. The economic and psychosocial comorbidity burden among adults with moderate-to-severe atopic dermatitis in Europe: analysis of a cross-sectional survey. Dermatol Ther (Heidelb). 2021;11(1):117–30.
Krakowski AC, Eichenfield LF, Dohil MA. Management of atopic dermatitis in the pediatric population. Pediatrics. 2008;122(4):812–24.
Flohr C. How we treat atopic dermatitis now and how that will change over the next 5 years. Br J Dermatol. 2022;188(6):718–25.
Eichenfield LF, Tom WL, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies. J Am Acad Dermatol. 2014;71(1):116–32.
Carrera YIL, Al Hammadi A, Huang Y-H, Llamado LJ, Mahgoub E, Tallman AM. Epidemiology, diagnosis, and treatment of atopic dermatitis in the developing countries of Asia, Africa, Latin America, and the Middle East: a review. Dermatol Ther (Heidelb). 2019;9(4):685–705.
Taylor K, Swan DJ, Affleck A, et al. Treatment of moderate-to-severe atopic eczema in adults within the U.K.: results of a national survey of dermatologists. Br J Dermatol. 2017;176(6):1617–23.
Sastre J, Baldrich ES, Armario Hita JC, et al. Consensus on the clinical approach to moderate-to-severe atopic dermatitis in Spain: a Delphi survey. Dermatol Res Pract. 2020;2020:1524293.
Boguniewicz M, Alexis AF, Beck LA, et al. Expert perspectives on management of moderate-to-severe atopic dermatitis: a multidisciplinary consensus addressing current and emerging therapies. J Allergy Clin Immunol Pract. 2017;5(6):1519–31.
Wichmann K, Heratizadeh A, Werfel T. In-vitro diagnostic in atopic dermatitis: options and limitations. Allergologie Select. 2017;1(2):150.
Silvestre Salvador J, Romero-Pérez D, Encabo-Durán B. Atopic dermatitis in adults: a diagnostic challenge. J Investig Allergol Clin Immunol. 2017;27(2):78–88.
Saeki H, Nakahara T, Tanaka A, et al. Clinical practice guidelines for the management of atopic dermatitis 2016. J Dermatol. 2016;43(10):1117–45.
Bieber T, D’Erme AM, Akdis CA, et al. Clinical phenotypes and endophenotypes of atopic dermatitis: where are we, and where should we go? J Allergy Clin Immunol. 2017;139(4s):S58–S64.
Wollenberg A, Barbarot S, Bieber T, et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part I. J Eur Acad Dermatol Venereol. 2018;32(5):657–82.
Vakharia PP, Chopra R, Silverberg JI. Systematic review of diagnostic criteria used in atopic dermatitis randomized controlled trials. Am J Clin Dermatol. 2018;19(1):15–22.
Sideris N, Paschou E, Bakirtzi K, et al. New and upcoming topical treatments for atopic dermatitis: a review of the literature. J Clin Med. 2022;11(17):4974.
Adam DN, Gooderham MJ, Beecker JR, et al. Expert consensus on the systemic treatment of atopic dermatitis in special populations. J Eur Acad Dermatol Venereol. 2023;37(6):1135–48.
Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71(2):327–49.
Megna M, Napolitano M, Patruno C, et al. Systemic treatment of adult atopic dermatitis: a review. Dermatol Ther (Heidelb). 2017;7(1):1–23.
Schmitt J, Langan S, Deckert S, et al. Assessment of clinical signs of atopic dermatitis: a systematic review and recommendation. J Allergy Clin Immunol. 2013;132(6):1337–47.
Boguniewicz M, Fonacier L, Guttman-Yassky E, Ong PY, Silverberg JI, Farrar JR. Atopic dermatitis yardstick: practical recommendations for an evolving therapeutic landscape. Ann Allergy Asthma Immunol. 2018;120(1):10–22.
Symptoms. https://www.nhs.uk/conditions/atopic-eczema/symptoms/?ssp=1&setlang=en-SG&safesearch=moderate. Accessed 13 Nov 2023.
Mehta A, Nadkarni N, Patil S, Godse K, Gautam M, Agarwal S. Topical corticosteroids in dermatology. Indian J Dermatol Venereol Leprol. 2016;82:371.
Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006;54(1):1–5.
Charman C, Morris AD, Williams HC. Topical corticosteroid phobia in patients with atopic eczema. Br J Dermatol. 2000;142(5):931–6.
Wollenberg A, Oranje AP, Deleuran M, et al. ETFAD/EADV eczema task force 2015 position paper on diagnosis and treatment of atopic dermatitis in adult and paediatric patients. J Eur Acad Dermatol Venereol. 2016;30(5):729–47.
Luger TA, Paller AS, Irvine AD, et al. Topical therapy of atopic dermatitis with a focus on pimecrolimus. J Eur Acad Dermatol Venereol. 2021;35(7):1505–18.
Godse K, De A, Sharma N, et al. Crisaborole for the treatment of atopic dermatitis in Indian patients: an evidence-based consensus statement. Indian J Drugs Dermatol. 2021;7(1):7.
Ma L, Zhang L, Kobayashi M, et al. Efficacy and safety of crisaborole ointment in Chinese and Japanese patients aged ≥ 2 years with mild-to-moderate atopic dermatitis. J Dermatol. 2023;50(7):847–55.
Lee JH, Kim JE, Park G-H, et al. Consensus update for systemic treatment of atopic dermatitis. Ann Dermatol. 2021;33(6):497.
Kulthanan K, Tuchinda P, Nitiyarom R, et al. Clinical practice guidelines for the diagnosis and management of atopic dermatitis. Asian Pac J Allergy Immunol. 2021;39(3):145–55.
Dogra S, Kanwar AJ. Narrow band UVB phototherapy in dermatology. Indian J Dermatol Venereol Leprol. 2004;70:205–9.
Rodrigues M, Ezzedine K, Hamzavi I, Pandya AG, Harris JE. Current and emerging treatments for vitiligo. J Am Acad Dermatol. 2017;77(1):17–29.
Fekete GL, Fekete L. Clinical and therapeutic trial for the efficacy of narrow band—UVB phototherapy versus systemic therapy in moderate and severe atopic dermatitis of the adult. Acta Medica Marisiensis. 2018;64(1):17–21.
Vangipuram R, Feldman SR. Ultraviolet phototherapy for cutaneous diseases: a concise review. Oral Dis. 2015;22(4):253–9.
Katayama I, Aihara M, Ohya Y, et al. Japanese guidelines for atopic dermatitis 2017. Allergol Int. 2017;66(2):230–47.
Hönigsmann H. Phototherapy for psoriasis. Clin Exp Dermatol. 2001;26(4):343–50.
Ring J, Alomar A, Bieber T, et al. Guidelines for treatment of atopic eczema (atopic dermatitis) part I. J Eur Acad Dermatol Venereol. 2012;26(8):1045–60.
Girolomoni G, Busà VM. Flare management in atopic dermatitis: from definition to treatment. Ther Adv Chronic Dis. 2022;13:20406223211066730.
Kim JE, Kim HJ, Lew BL, et al. Consensus guidelines for the treatment of atopic dermatitis in Korea (part II): systemic treatment. Ann Dermatol. 2015;27(5):578–92.
Khattri S, Shemer A, Rozenblit M, et al. Cyclosporine in patients with atopic dermatitis modulates activated inflammatory pathways and reverses epidermal pathology. J Allergy Clin Immunol. 2014;133(6):1626–34.
Lee S, Tan A, Giam Y. Cyclosporin in the treatment of severe atopic dermatitis: a retrospective study. Ann Acad Med Singap. 2004;33:311–3.
O’Donovan P, Perrett CM, Zhang X, et al. Azathioprine and UVA light generate mutagenic oxidative DNA damage. Science. 2005;309(5742):1871–4.
Taylor K, Swan DJ, Affleck A, Flohr C, Reynolds NJ. Treatment of moderate-to-severe atopic eczema in adults within the U.K.: results of a national survey of dermatologists. Br J Dermatol. 2017;176(6):1617–23.
Ring J, Alomar A, Bieber T, et al. Guidelines for treatment of atopic eczema (atopic dermatitis) Part II. J Eur Acad Dermatol Venereol. 2012;26(9):1176–93.
Simpson EL, Bieber T, Guttman-Yassky E, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375(24):2335–48.
Faiz S, Giovannelli J, Podevin C, et al. Effectiveness and safety of dupilumab for the treatment of atopic dermatitis in a real-life French multicenter adult cohort. J Am Acad Dermatol. 2019;81(1):143–51.
Jang DH, Heo SJ, Jung HJ, Park MY, Seo SJ, Ahn J. Retrospective study of dupilumab treatment for moderate to severe atopic dermatitis in Korea: efficacy and safety of dupilumab in real-world practice. J Clin Med. 2020;9(6):1982.
Arkwright PD, Motala C, Subramanian H, Spergel J, Schneider LC, Wollenberg A. Management of difficult-to-treat atopic dermatitis. J Allergy Clin Immunol Pract. 2013;1(2):142–51.
Acknowledgements
The authors would like to thank Dr James Wee from Pfizer and Chee Wen Eng from IQVIA for their contribution in managing this project (at time of data collection) as well as Xiaoyun Chen from IQVIA for performing the statistical analysis. In addition, the authors would like to extend our gratitude to the participants of the study.
Medical Writing Assistance
Medical writing support was provided by Rachel Lee-Yin Tan from IQVIA.
Funding
This study (including publication fees) was funded by Pfizer Hong Kong Corporation Limited. IQVIA was contracted to conduct study activities. The sponsor was also involved in the study design, data interpretation and manuscript review.
Author information
Authors and Affiliations
Contributions
All authors were involved in the conception and design of this study, interpretation of the results, and critical revision of the manuscript. Sophie Bozhi Chen and See-Hwee Yeo were involved in data analysis and drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Han-Fang Liao and Sean Gardiner are employees of Pfizer. Yoko Kataoka has received lecturer honoraria from Sanofi, AbbVie, Pfizer and Maruho, and research funding from Sanofi, Leo Pharma, Pfizer, Maruho, Lilly, AbbVie, Otsuka, Taiho and Amgen. Yung Chan is a speaker for AbbVie, Bioderma, Galderma, Inova, Eli Lily, Lumenis, Menarini and Pfizer; an advisory board member for AbbVie, Bayer, Bioderma, CeraVe, Eli Lilly, Menarini, Pfizer, Sanofi, Quanta System and Janssen. Chia-Yu Chu is an investigator for AbbVie, Amgen, Dermira, Eli Lilly, Janssen, Novartis, Oneness Biotech, Pfizer, Regeneron Pharmaceuticals Inc., Roche and Sanofi; a consultant for AbbVie, Amgen, Eli Lilly, GlaxoSmithKline, Janssen, Novartis, Pfizer, Roche and Sanofi; a speaker for AbbVie, Eli Lilly, GlaxoSmithKline, Janssen, Mylan, Novartis, Pfizer, Roche, Sanofi and Viatris; and an advisory board member for AbbVie, Amgen, Mylan, Pfizer, Roche, Sanofi and Viatris. Nisha Suyien Chandran has received fees for participation in advisory boards from AbbVie, Johnson & Johnson, Sanofi, Pfizer, DKSH, L’Oreal and Novartis; investigator fees for clinical trials from AbbVie, Novartis, Amgen, Sanofi and Boehringer Ingelheim; and speaker honoraria from Galderma, Johnson & Johnson, LEO, Pfizer, Sanofi and Lion Corporation. All other authors have no conflict of interest.
Ethical Approval
Ethical approval was received from the following IRBs: Korea University Ansan Hospital, Chulalongkorn University, Father Muller Hospital, NPO MINS, National Taiwan University Hospital, Hong Kong Doctors Union, and Sir Run Run Shaw Hospital. The Parkway Independent Ethics Committee granted an exemption from review. The study was conducted in accordance with the protocol, Guidelines for Good Pharmacoepidemiology Practices, and the Declaration of Helsinki. All participants provided informed consent.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chu, CY., Chan, Y., Wananukul, S. et al. Management of Moderate-to-Severe Atopic Dermatitis in Adults: A Cross-Sectional Survey of Dermatologists Within the Asia–Pacific Region. Dermatol Ther (Heidelb) 14, 2559–2576 (2024). https://doi.org/10.1007/s13555-024-01246-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01246-5