Abstract
In high-mortality contexts, research examining the effects of child mortality has focused almost exclusively on couples’ fertility responses while overlooking other potential family consequences. Using nationally representative survey data from 13 West and Central African countries, we estimate multilevel discrete-time hazard models to determine how women’s risk of intimate partner violence (IPV) varies with the death of children. We assess heterogeneity in this association across two surrounding circumstances: children’s age at death and regional prevalence of child bereavement. Findings indicate that the risk of IPV initiation rises with the death of children under age 5—for whom women are most intensely responsible—but not with the death of older children. The effect of young child bereavement is most pronounced in regions where it is least prevalent among mothers—a finding not explained by concomitant regional variation in gender inequality, family norms, and infrastructural development. These findings highlight the importance of child mortality for family outcomes beyond fertility in the African context and demonstrate the prominent role of the broader mortality context in shaping these implications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The death of a child can be a highly stressful experience with the potential to alter the course of couples’ relationships. Although many studies have examined the effects of child bereavement (experiencing the death of a child) on parents’ relationship quality and stability in the United States and Europe (for a review, see Albuquerque et al. 2016; Oliver 1999), surprisingly little research has taken up similar questions in countries where child mortality is concentrated. Instead, studies of high-mortality contexts have focused primarily on couples’ fertility responses (Aksan 2014; Bongaarts et al. 1984; Defo 1998; Gyimah and Fernando 2004; Lindstrom and Kiros 2007). The resulting chasm prevents scholars from fully comprehending the familial consequences of child mortality in areas of the world where most child deaths occur. We examine how the death of a child affects the risk of intimate partner violence (IPV) among mothers in West and Central Africa, where both IPV and child mortality rates remain particularly high (Devries et al. 2013; World Bank 2015).
West and Central African countries today host 17 of the world’s 20 highest child mortality rates (World Bank 2015). For instance, in Angola, Chad, and the Central African Republic, 16%, 14%, and 13% of children (respectively) die before age 5 (World Bank 2015). Within these countries, however, child mortality is unevenly spatially distributed (Balk et al. 2004), meaning that some communities experience higher rates of child mortality and bereavement than others (Smith-Greenaway and Trinitapoli 2019). Previous research suggests that the community prevalence of child bereavement should shape local interpretations of child loss, social support for bereaved parents, and perceptions of the average woman’s ability to protect her child from harm (Sandberg 2006; Scheper-Hughes 1992; Trinitapoli and Yeatman 2018). We therefore also investigate how the broader mortality context in which a child’s death takes place conditions its implications for IPV. To ensure that we do not conflate the prevalence of child bereavement with underlying conditions, we additionally assess concomitant heterogeneity in the effects of child bereavement across contextual levels of gender inequality, family norms, and infrastructural development.
Leveraging new information on the timing of IPV initiation, collected through the most recent wave of Demographic and Health Surveys (DHS), we estimate a series of multilevel discrete-time hazard models that assess how the risk of IPV onset varies with child bereavement and how this relationship varies across context. Given that most child mortalities occur before age 5, and that the effects of child bereavement may vary with a child’s age at death (Rogers et al. 2008; Song et al. 2010), we distinguish between the effects of losing children under and over age 5. To bolster our conclusions, we further use information on the timing of IPV to conduct a supplementary analysis in which we carefully assess the reverse scenario—for example, whether IPV predicts subsequent child fatalities.
Our emphasis and assessment of IPV as a potential consequence of child death not only expands current understandings of the familial repercussions of child mortality but further moves beyond long-standing assumptions that negative associations between IPV and child well-being are driven exclusively by an effect of IPV on the quality of parental caregiving and the household environment (Emery et al. 2015; Letourneau et al. 2013; Nixon et al. 2017; Sullivan et al. 2001). Drawing on previous studies indicating a degradation of parents’ marriage following the death of a child (Lyngstad 2013; Rogers et al. 2008) and suggesting that women are often blamed for children’s adverse outcomes (Castle 1994; Haws et al. 2010), we propose and test an alternative account of positive associations between IPV and child mortality. Our analyses challenge common conceptualizations of the relationship between IPV and child survival, broaden current understandings of the implications of child death for parents in Africa, and illustrate how the surrounding mortality context shapes these implications.
Background
Child Death and IPV
Numerous studies have found that mothers’ history of IPV is associated with negative child health outcomes (Karamagi et al. 2007; Rico et al. 2011; Silverman et al. 2009; Sobkoviak et al. 2012; Yount et al. 2011) and higher rates of child mortality before age 5 (Ackerson and Subramanian 2009; Åsling-Monemi et al. 2003; Jejeebhoy 1998; Rico et al. 2011). Although negative associations between IPV and child health and survival are documented across diverse countries, most studies have drawn on data sources in which IPV is measured in terms of lifetime prevalence or the last year only (Ackerson and Subramanian 2009; Åsling-Monemi et al. 2003; Jejeebhoy 1998; Karamagi et al. 2007; Rico et al. 2011). As such, scholars have been unable to disentangle the temporal ordering of events. It thus remains possible that some of the previously observed associations are due to child illness or death elevating women’s risk of abuse.
In fact, extant scholarship points to a number of reasons why women may be at heightened risk of IPV after a child’s death. One is that social narratives of “good mothering” (Hays 1998; Lupton 2012) blame women when children do not thrive (Dunn et al. 1991; Fish 1986; Sisay et al. 2014; Wing et al. 2001), including in sub-Saharan Africa, where caring for young children is considered women’s work. That is, because women are predominantly responsible for childrearing, their husbands, in-laws, and other community members often view and treat them as responsible for child health outcomes (Hays 1998; Jackson and Mannix 2004; Lupton 2012) and correspondingly blame women for the death of young children (Castle 1994; Haws et al. 2010). If a husband blames his wife for the death of their child, this blame could spawn IPV, as one study from the United States suggests (Gold et al. 2018). Notably, however, maternal blame may be conditional on a child’s age at death: to the extent that children become less fragile, gain physical independence (e.g., discontinue breastfeeding), and spend less time with mothers as they age (Abdullah et al. 2007; Milkie et al. 2004), women may be perceived as decreasingly responsible for children’s outcomes as they grow older (Ricci et al. 1996).
Even if men do not directly blame wives for a child’s death, the psychological distress experienced as a result of bereavement may exacerbate the risk of IPV. Research from the United States and Europe suggests that in the wake of bereavement, parents experience stress, anxiety, grief, depression, and identity loss (Wijngaards-de Meij et al. 2008; Murphy et al. 2002; Toller 2008). These conditions can persist for years (Murphy et al. 2002, 2003a, b) and, because of a longer attachment period, may be especially pronounced after the death of an older child (Rogers et al. 2008). Such distress can lead to anxious attachment, in which one spouse becomes troubled that the other will not be available when needed (Wijngaards-de Meij et al. 2008). Considering that IPV often serves as a control tactic within relationships (Anderson 2008; Villarreal 2007), anxiety resulting from a child’s death may contribute to IPV as a way of controlling one’s spouse and her whereabouts. Grief, depression, and other types of psychological distress may also lead to communication breakdowns between parents, elevating conflict (Reilly-Smorawski et al. 2002; Schwab 1998; Toller and Braithwaite 2009) potentially to the point of violence. Such breakdowns and conflict commonly occur when parents’ emotional reactions are dissimilar, one parent grieves longer than the other, or parents’ coping tactics differ (Albuquerque et al. 2016; Oliver 1999; Toller and Braithwaite 2009). Gender differences in the grieving process, with women reporting stronger feelings of guilt and longer grief periods than men, frequently give rise to such incongruences (Reilly-Smorawski et al. 2002; Schwab 1996; Wing et al. 2001).
Moreover, research from the United States suggests that having a child die is a socially isolating experience (Murphy et al. 1998; Umberson 2017). When a child dies, many parents withdraw from social networks because they feel misunderstood, stigmatized, or ashamed (Hastings 2000; Riches and Dawson 1996); believe that others trivialize their experiences and emotional responses (Meyer et al. 2016); or feel psychologically drained by social situations in which they are simultaneously encouraged to talk about their deceased child and discouraged from talking about him or her too much (McBride and Toller 2011; Toller 2005). Likewise, talking about deceased children can be uncomfortable, sometimes leading friends and family to withdraw from relationships with bereaved parents (Toller 2008). Of course, in some West and Central African settings, the normative nature of child mortality (which we discuss in the following section) may buffer couples against these experiences, at least in contexts where child bereavement is a common maternal experience. However, in other settings—perhaps particularly those where child death is less common—parents in West and Central Africa may also become isolated or stigmatized after the loss of a child because of cultural beliefs that untimely deaths are the result of witchcraft, evil, or a curse (Caldwell and Caldwell 1987; Havik 2016; Madhavan 2001; Towns et al. 2014; Wilkinson and Callister 2010). Social isolation may thus exacerbate couples’ stress or conflict in ways that contribute to the risk of IPV following a child’s death.
In sum, there are multiple social, psychological, and cultural mechanisms by which a child’s death may instigate IPV in West and Central Africa. Research from the United States and Europe generally supports this hypothesis, with multiple studies finding a higher risk of divorce and separation (Lyngstad 2013; Rogers et al. 2008) and lower levels of sexual activity and marital satisfaction among bereaved parents than among nonbereaved parents (Arnold et al. 2005; Dyregrov and Gjestad 2011; Murphy et al. 2003b; Oliver 1999). However, different mechanisms may play out with the loss of younger and older children: when children die young, at a point when they are still dependent on mothers for care and survival, IPV may be indicative of maternal blame. When children die at older ages, after a longer attachment period, IPV may more likely stem from extreme psychological distress and/or discordant grieving processes between parents. As we describe shortly, social isolation may exacerbate both of these mechanisms and thus contribute to IPV risk regardless of a child’s age at death.
Variation in the Effects of Child Death Across the Prevalence of Child Bereavement
Given that West and Central Africa represent a large, diverse area of the world, the consequences of child bereavement may be heterogeneous across context—governed by the social norms, institutions, and belief systems within a couple’s community. The local prevalence of child bereavement is likely especially salient to how parents understand and experience the death of a child and, by extension, the marital consequences of this experience. In settings where child bereavement is somewhat rare (even if still high by international standards), parents may face social isolation and perhaps even stigmatization in the aftermath of a child’s death. That is, the lower the prevalence of child bereavement is, the lower the share of community members will be who have had first- or secondhand experiences with child loss, leading to potentially lower levels of social support. Where child loss is a less common experience, social isolation may intensify the potential stress of losing a child (Hastings 2000; Riches and Dawson 1996; Toller 2008), thereby exacerbating the risk of negative consequences, including IPV. Moreover, where child loss is rare, parents may view child survival as a matter of personal responsibility, especially maternal responsibility (Gold et al. 2018), given that mothers are often the primary caretakers of young children. Thus, child loss may be more likely to result in maternal blame—and IPV as a form of maternal castigation—when child bereavement is a less common occurrence.
To the extent that parents receive greater social support and understanding after losing a child in high-mortality settings, this may alleviate bereavement-related stress and conflict, minimizing the risk of IPV. Moreover, in communities where child loss is extremely common, parents may view child survival as beyond their own control (Scheper-Hughes 1992; Sisay et al. 2014), reducing the likelihood of maternal blame. Indeed, a handful of studies have found that experiencing a child’s death has no effect on parental relationships in the United States (Oliver 1999; Schwab 1998) or that the grieving process bonds couples and ultimately results in greater relationship stability (Barrera et al. 2009; Eilegård and Kreicbergs 2010; Essakow and Miller 2013). These findings may be most applicable to communities in West and Central Africa, where child bereavement is more common: in high-mortality contexts, it is possible that child bereavement bears no observable implications for couples’ marriages, including the risk of violence. Thus, we explore whether the broader setting in which couples reside—and where bereavement and the grieving process take place—moderate the influence of child loss on IPV.
Understanding whether and how the effects of child bereavement vary across its contextual prevalence is complicated by the prevalence of child mortality being correlated with other contextual characteristics, such as local gender and family norms and infrastructural development (Hatcher et al. 2013; Hung et al. 2012; Sievert 2015; Smith-Greenaway 2017; Smith-Greenaway and Trinitapoli 2014; Trussell and Pebley 1984; VanderEnde et al. 2012; Yount et al. 2014). Although child mortality and child loss (child bereavement) rates are not perfectly correlated (because some parents may lose multiple children), regional associations between these different characteristics leave open the possibility that variation in the effects of child loss across its regional prevalence may be spuriously driven by corresponding variation in other regional attributes. To test whether this is the case, we explore whether regional gender, family, and infrastructural conditions modify the effect of child bereavement on IPV and whether concomitant variation across these regional conditions mediates the modifying effect of the prevalence of child bereavement.
Data and Methods
Sample
We draw on standardized, nationally representative data from the DHS in West and Central Africa, including all countries with the latest IPV module. This yields a sample from 13 countries: Burkina Faso, Cameroon, Chad, the Democratic Republic of Congo, Gabon, the Gambia, Ghana, Ivory Coast, Liberia, Mali, Nigeria, Sierra Leone, and Togo (Table A1, online appendix).Footnote 1 In each of these countries, the DHS surveyed all women aged 15–49 from participating households. To protect women’s safety and to ensure data quality, however, only one woman per household was randomly selected to participate in the IPV module and only if she could answer the questions in privacy. Across the 13 surveys, 99% of randomly selected respondents agreed to participate.
Our analytic sample is defined by three restrictions (shown in Fig. 1), each of which is intended to minimize measurement error. First, we limit our analysis to women who are still in their first union whose first birth occurred within that union.Footnote 2 This allows us to ascertain the correct temporal ordering of IPV and child mortality given how IPV initiation was measured in the DHS (as described later).Footnote 3 Second, we restrict the sample to women whose first birth occurred five or more years prior to the survey. This prevents women whose entire parity was still at risk of under-5 child mortality from attenuating our results.Footnote 4 Third, we confine the sample to women whose last birth occurred within the previous 10 years. Doing so minimizes recall error and ensures that current contextual characteristics are reasonable indicators of couples’ environment during their childbearing years. These restrictions yield a final analytic sample of N = 33,279 women. To the extent that IPV may contribute to separation and/or to premature death among women, our sample restrictions may yield conservative estimates (see Table A2 in the online appendix for a comparison of the analytic sample to the full sample of mothers in the IPV module).
To facilitate our discrete-time hazard modeling approach (described shortly), we create a panel data set where the unit of analysis is person-years, starting with the year of first birth. The number of times a woman appears in the data set depends on the number of years between her first birth and the year of survey. For example, a mother whose first birth occurred in 2003 and who was surveyed in 2010 would appear eight times (once for each year). This approach allows us to develop time-varying measures of IPV initiation, fertility, and child deaths while also drawing on time-invariant measures of respondents’ circumstances and contextual characteristics at survey.
Measures
Bereavement
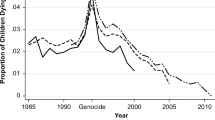
For every live birth a woman reported during the survey, she was asked to provide the year of birth and whether that child was still alive. If deceased, she was asked to provide the date when the child died. This information allows us to identify each year in which a woman experienced a child death and that child’s age at death. Based on this information, we create a time-varying indicator of whether, as of each year, respondents had lost a child <5 years old. Years including and subsequent to the first time a respondent was bereaved by the death of a child <5 years old are coded as 1; years prior are coded as 0. Women who never experienced the death of a child under age 5 are coded as 0 in all years.Footnote 5 In our sample, 35% of mothers experienced at least one child’s death before the age of 5 (Table 1), although the prevalence of young child bereavement varied greatly across and within countries (Fig. 2).
Regional variation in the prevalence of maternal bereavement. Authors’ calculations from Demographic and Health Surveys. Three regions in Mali were not surveyed by the DHS and are thus not shaded. The map was created at mapchart.net.
We also create an analogous time-varying indicator of whether as of each year, respondents had become bereaved by the loss of a child ≥5 years old. Only 5% of mothers in our sample experienced the death of a child after his or her 5th birthday (Table 1). Given our necessary focus on continuously married couples, this subset of mothers bereaved by older children is more selective than the sample of mothers who (only) experience a child death at younger ages (because they had to be married longer in order to be at risk of losing an older child). Accordingly, conclusions drawn about the relationship between older child bereavement and IPV should be drawn with greater caution.
Intimate Partner Violence
In the DHS, mothers were asked a series of questions about past experiences of physical and sexual IPV from their current partner, based on a modified version of the Conflict Tactics Scale (Straus et al. 1996). Types of violence included whether a respondent’s husband had ever: “pushed, shaken, or thrown something at [her]; “slapped [her]”; “twisted [her] arm or pulled [her] hair”; “kicked, dragged, or beaten [her] up”; “tried to choke or burn [her]”; “threatened to attack [her] with a weapon”; “attacked [her] with a weapon”; “forced [her] to have sex”; or “forced [her] to perform any other sexual acts.”
Respondents who reported experiencing any form of physical or sexual IPV ever in their lifetime were asked, “How long after you first (got married/started living together) with your (husband/partner) did (this/any of these things) first happen?”Footnote 6 Respondents provided the number of years from the start of marriage/living together. This information allows us to identify when IPV first began but does not allow us to distinguish between the start of physical and sexual IPV. We combine information on whether and when any physical or sexual IPV first occurred to create a right-censored, time-varying measure of experienced IPV for the first time. This measure is coded as 1 in the year violence began and as 0 every year before. Women who never experienced violence are coded as 0 in all years.
As shown in Table 1, 20% of respondents reported that at least one form of IPV had ever happened to them. Among women who reported both losing a child under age 5 and experiencing IPV (n = 1,455; 4% of the analytic sample), the onset of IPV began an average of 3.69 years after their first experience of a young child’s death. The modal and median distances between young child bereavement and IPV onset were 1 and 2 years, respectively (Fig. 3). This distribution indicates that when IPV onset follows the death of a young child, it most commonly occurs in the immediately following years, although for some women, it does not commence until much later.
Respondent-Level Characteristics
We control for respondent-level attributes that previous research indicates are associated with child well-being and IPV, including her personal attributes and attributes of her partner and household (Kiros and Hogan 2001; Takyi and Mann 2006). Respondent’s personal attributes include her years of schooling; age at union formation (marriage or cohabitation, in exact years ranging from 9 to 40)Footnote 7; age at first birth (ranging from 10 to 43);Footnote 8,Footnote 9 and a time-variant measure of her cumulative number of births. This last measure is updated yearly and increases as a woman bears more children (coded as 1 every year she has borne a total of one child, as 2 every year she has borne a total of two children, and so on).
Her partner’s characteristics include his years of schooling and whether he has other wives. Household characteristics include whether the household head is male, urban versus rural residence, and whether the household has electricity.
Contextual Characteristics
We conceptualize subnational regions as indicators of respondents’ local context. Subnational regions (N = 124) represent a combination of political districts and administrative or geographical boundaries, depending on the country. These regions are more suitable indicators than survey clusters because they capture a larger area than respondents’ immediate neighborhood and thus take into account additional fields where social interactions take place. Moreover, because of tremendous within-country variation in the prevalence of child bereavement (Fig. 2), subnational regions more accurately convey respondents’ local context than country. For instance, in the Democratic Republic of Congo, the regional prevalence of young child bereavement (under age 5) ranges from 21% of mothers in Kinshasa to twice as much—43%—in Sud-Kivu (Fig. 2). Likewise, in Chad, regional variation in this prevalence ranges from 20% of mothers in Bahr el Ghazal to 51% in Logone Oriental. Even in countries that are geographically much smaller, such as Ghana, the regional prevalence of young child bereavement varies from 14% in Greater Accra to three times as much—41%—of mothers in Upper West (Fig. 2).
On average, 1,494 respondents are nested within a given subnational region, with the smallest region containing 334 women and the largest containing 9,673. Given such a large number of cases per region, we include the focal respondent when generating contextual indicators. To create these indicators, we calculate characteristics of interest by subnational region using the weighted DHS women’s data files for each country, including all women aged 15–49. Where appropriate, we also use the weighted DHS men’s data files, including all men aged 15–59. Our regional indicators are thus based on nationally representative samples of individuals of reproductive age.
Regional prevalence of child bereavement is operationalized in two ways: the percentage of mothers ever bereaved by a child <5 years old and the percentage of mothers ever bereaved by a child ≥5 years old. Regional gender inequality is also operationalized in two ways. One is the prevalence of women who report experiencing any form of IPV in their lifetime. The other is the ratio of women’s average years of schooling to men’s average years of schooling—a common indicator of gender inequality (Smith-Greenaway and Trinitapoli 2014). Regional family norms include fertility levels, which we operationalize as the average woman’s parity in a given region, and the percentage of women who report being in a polygynous union. Finally, regional infrastructural development is operationalized as the percentage of women who reside in an urban area and the percentage who have electricity in their homes (separately).
Cross-Level Interactions
We interact our time-varying indicators of bereavement—by the death of children <5 years old and children ≥5 years old, separately—with their respective regional prevalence. Doing so allows us to test whether how common or uncommon it is to lose a younger or older child conditions the association between individual child loss and IPV risk. Given that variation in the prevalence of child loss may be partly driven by regional variation in gender inequality, family norms, and/or infrastructural development and that these other sources of contextual variation may additionally condition the relationship between personal child bereavement and IPV risk, we further test analogous interactions between women’s own experience of child loss and each of these contextual factors.
Country
Considering that a wide range of country-level characteristics may influence the association between child loss and women’s risk of IPV, we include a set of country dummy variables. This country fixed-effects approach accounts for constant, unobserved characteristics varying across West and Central African countries that may be associated with the risk of child bereavement and the risk of IPV. For instance, the three countries with the highest prevalence of young child bereavement—Sierra Leone, Chad, and Liberia—each had a civil war within approximately one decade of survey. Including country fixed effects accounts for the history of war shared among women within each of these countries.
Years Since Firth Birth
To accommodate our discrete-time hazard models, we adjust for the time-varying, discrete number of years since first birth, coded as 0 when the firstborn is <1 year, as 1 when she/he is 1 year old, and so on.
Estimation Strategy
We focus on the sequence of events occurring to mothers (rather than to children) to understand the consequences of child mortality from the maternal perspective. As a first step, we estimate the relationship between child bereavement (this year or earlier) and the risk of IPV initiation. Considering that our dependent variable is right-censored and that our data are hierarchal—where women (N = 33,279) are nested within regions (N = 124), which are nested within countries (N = 13)—we estimate a multilevel discrete-time hazard model with random effects:
where hirct is the hazard that respondent i in region r in country c experiences IPV initiation at time t;Xirc is a vector of respondent’s characteristics (including her, her partners’, and her household’s attributes); Yrc is a vector of region-level covariates; Cc is a series of country dummy variables that account for unobserved confounders at the country level; ur is a subnational region-level random effect; and αt is a series of dummy variables for each year since first birth. An important assumption of this strategy is that the effect of losing a child on the risk of IPV is constant across time. We test this assumption by examining a categorical indicator of years since young child bereavement (<1, 1–2, 3–5, 6–9, ≥10). Post-estimation Wald tests examining the equality of coefficients confirm that the effects of bereavement do not vary with subsequent time elapsed.
Next, to assess whether the regional prevalence of child bereavement conditions the relationship between the individual experience of bereavement and IPV initiation, we reestimate our model including an interaction term between individual bereavement by a child <5 years old and its regional prevalence and a second interaction term between individual bereavement by a child ≥5 years old and its corresponding prevalence:
Finally, where appropriate, we assess the extent to which any significant variation in the effects of child bereavement across its corresponding prevalence is attributable to variation in the gender, family, or infrastructural context. To do this, we reestimate our second model adding interactions between individual child bereavement (this year or earlier) and these regional indicators.Footnote 10 For instance, when examining the potential mediating effect of concomitant variation in the effects of young child bereavement across regional gender inequality, our model is as follows:
Including interactions between individual child bereavement (this year or earlier) and indicators of the gender, family, and infrastructural context in separate models allows us to better understand which, if any, underlying regional characteristics drive the conditioning effect of regional prevalence of bereavement.
Although the central goal of this analysis is to investigate the implications of child bereavement for IPV, previous research generally assumes the reverse—for example, that negative associations between the two are indicative of IPV increasing the risk of child mortality. Therefore, as a supplement, we conduct a series of logistic and discrete-time hazard models estimating the effect of IPV on children’s subsequent risk of dying before age 5. We more fully describe these models and their results following the presentation of our main findings.
For the ease of interpretation, we present all results in their original form and exponentiated such that values less than 1 indicate negative associations and values greater than 1 indicate positive associations. When discussing them in the text, we focus our attention on the exponentiated results.
Results
Table 2 presents estimates from our multilevel discrete-time hazard models investigating the relationship between child bereavement and IPV initiation. The results of Model 1 confirm that net of respondent and contextual characteristics, years since first-birth, and country, the estimated risk of IPV initiation increases with the loss of a child under age 5 (Table 2). That is, compared with women who have never lost a child, women’s risk of experiencing IPV for the first time increases by 12% starting in the year they first experience a young child die. This finding aligns with the positive association between IPV and child mortality found in previous studies, but it provides an important new explanation: namely, that the risk of IPV onset increases with a young child’s death. Model 1 does not, however, indicate any significant independent effects of older child bereavement or of either contextual prevalence of child bereavement.Footnote 11
Turning to other contextual characteristics, regional gender inequality is predictive of the risk of IPV onset. That is, women’s risk of IPV increases by 5% for each percentage point increase in its prevalence. Moreover, consistent with studies that found a positive association between women’s education (both absolute and relative to men’s) and IPV in sub-Saharan Africa (Behrman 2016; Peterman et al. 2015), women’s risk of IPV is higher in settings where schooling is more gender-equal. Regional levels of fertility, polygyny, urbanicity, and electrification are not significantly associated with a woman’s risk of IPV net of regional levels of child bereavement, IPV, and gender inequality in schooling (Model 1, Table 2).
To understand whether the effects of individual child loss vary as a function of the commonality of child bereavement in a woman’s region, and thus to get a better sense of whether the salience of hypothesized mechanisms contextually vary as expected, we interact the two indicators of respondent-level child bereavement (this year or earlier) with the region-level indicators of their corresponding prevalence. As can be seen in Model 2, the coefficient on the first interaction term indicates that the effect of losing a child under age 5 is significantly smaller in regions where the loss of young children is a more common experience (Table 2). Because the interpretation of interactions is notoriously difficult in nonlinear regression (Ai and Norton 2003), Fig. 4 converts these results into marginal effects—differences in the estimated annual probability of IPV onset in years before and after young child bereavement, by its regional prevalence—and portrays them graphically. In one-fifth of the regions (n = 24), ≤ 20% of mothers lose a child <5 years old. In these regions, where young child bereavement is least common, losing a child of this age is associated with a ≥0.4 percentage point increase in the probability of IPV initiation. As the prevalence of young child bereavement increases to just under 40%, the effect of losing a young child decreases to nearly one-half the magnitude. In regions where young child bereavement is the most prevalent, with ≥40% of mothers losing a child—as is the case in 20% of the regions (n = 25)—the effect is not statistically distinguishable from 0 (Fig. 4). We find no comparable pattern in the effects of losing a child age 5 or older across its regional prevalence (Table 2, Model 2).
Variation in the effects of young child bereavement (child died before age 5) by corresponding regional prevalence of young child bereavement. Marginal effects are based on the results of Model 2 (Table 2), holding covariates at their means.
Considering that regional gender inequality, family norms, and infrastructural development may also condition the effect of child loss and potentially even explain the conditioning effect of the prevalence of young child bereavement in Model 2, Models 3–5 introduce additional interaction terms between respondent-level child bereavement (under age 5) and region-level indicators of these contextual characteristics. As can be seen in each of these models, we find limited evidence that region-level gender, family, or infrastructural conditions moderate the effect of child bereavement. The one exception is that the effects of young child bereavement on the risk of IPV onset are found to be greater in regions where IPV is more prevalent.Footnote 12 Converting the results from this interaction into marginal effects, however, reveals that the effect of young child bereavement is largely consistent across IPV prevalence and becomes smaller only in the very few regions (n = 2) where at least half of the women experience IPV (Fig. A1, online appendix). Moreover, the coefficient on the interaction between young child bereavement and the regional prevalence of mothers who have experienced such bereavement remains statistically significant and similar in magnitude when these additional interaction terms are included. The results of Models 3–5 thus bolster our conclusion that the effects of individual-level child bereavement are conditioned by the surrounding mortality environment rather than by concomitant regional characteristics.
Supplemental Analyses
Is IPV Associated With an Increased Risk of Child Mortality?
Thus far, we have examined the risk of IPV initiation following child bereavement. Yet extant research emphasizes the reverse—that IPV may increase the risk of child mortality (Emery et al. 2015; Letourneau et al. 2013; Nixon et al. 2017; Sullivan et al. 2001). As a supplement, we therefore model this association from the child’s perspective, investigating whether the risk of child mortality increases following IPV onset. To begin, we conduct cross-sectional models that replicate the commonly found positive association between IPV and child mortality and then reexamine this association, distinguishing between IPV that could have plausibly led to a child’s death (because it originated before the child’s birth or fewer than five years after it) and IPV that could not have plausibly led to a child’s death (because it originated five or more years after birth and thus after the window for under-5 child mortality closed). To do so, we treat individual offspring born to mothers in our analytic sample as the unit of analysis and focus on those who were born more than five years before survey to minimize censoring issues (see Table A3 in the online appendix for descriptive statistics for this supplemental sample).Footnote 13
We code our dependent variable, child mortality prior to age 5, as 1 if a child died before age 5 and as 0 if a child lived beyond his or her fifth birthday. We code mothers’ lifetime history of IPV as 1 if she ever experienced physical or sexual IPV prior to survey and as 0 if not. Our models include the same controls as in our primary analysis, as well as additional controls for child characteristics: whether any siblings died before him/her, sex, whether he/she is a twin,Footnote 14 whether he/she was born two or more years after any preceding birth, and birth order (from 1 to 16). To replicate the positive association found in prior studies, we estimate a simple logistic regression predicting whether a child died before age 5. To account for the clustering of children within women, we cluster standard errors by mother. Consistent with extant research, children whose mothers ever experienced IPV have 13% higher odds of dying before age 5 than children whose mothers never experienced IPV (Model 6, Table A4, online appendix). This translates to a 1.5 percentage point difference in the likelihood of child mortality between the two groups (Fig. 5).
Marginal effects of maternal IPV history on the probability of child mortality. N = 118,219 children born more than five years before the survey. Marginal effects convey the difference in the predicted probability of dying before age 5 and are calculated from the results presented in Table A4 (online appendix).
Next, to distinguish between IPV that could and could not contribute to a child’s death before age 5, we include an interaction between maternal history of IPV and an indicator of whether IPV onset began earlier than five years from the child’s birth (Model 7, Table A4, online appendix). The significant coefficient on this interaction term indicates an important difference in the association between IPV and child mortality conditional on when IPV began. Figure 5 translates these results into marginal effects and reveals no significant difference in the likelihood of dying before age 5 between children whose mothers never experienced IPV and children whose mothers began experiencing IPV either before the child was born or within five years of the child’s birth. Yet, the probability of dying before age 5 is 3.7 percentage points higher among children whose mothers experienced IPV starting more than five years after their birth than among children whose mothers never experienced IPV. In this latter case, IPV could have occurred only after a child died. These supplemental findings suggest that an association between IPV and child mortality primarily emerges after the death of a child in our sample.
To further confirm that there is no association between IPV and a child’s risk of death before age 5, we next estimate a discrete-time hazard model. This model accounts for censoring of the dependent variable by treating offspring-years as the unit of analysis. This requires converting information on individual offspring (born to mothers in our analytic sample) into a panel data set in which each offspring is represented one to six times. The first offspring-year represents the year of birth, the second is the year the offspring turned age 1, and so on, until the child reaches age 5. The number of times any one offspring appears in the data set depends on the child’s age at survey or age at death. We populate this data set with time-varying information on children’s age, number of siblings, whether any sibling has ever died, and mothers’ history of IPV (as of a given year), and with time-invariant information on all other child, mother, and region characteristics included in our cross-sectional supplement.
We code our dependent variable, child mortality, as 1 if the child in question died as of a given year and as 0 if that child was still alive in that year. Children who survived past their fifth birthday are coded as 0 in all six years they appear in the data set. We code IPV history as 1 if a child’s mother had ever experienced IPV as of a given year and as 0 if not. Children whose mothers never experienced IPV are coded as 0 in all years. We estimate a discrete-time hazard model with random effects, akin to those in our primary analysis, employing child age as the discrete measure of time. Like the results of the first two models in Table A4 (online appendix), the results of this third model offer no evidence to suggest that IPV increases a child’s risk of dying before his fifth birthday. These results further attest to the theoretical and empirical contribution of our study, which highlights child death as a major event in couples’ lives with the power to alter the course of their relationship.
Discussion
Child mortality rates remain considerably higher in West and Central Africa than elsewhere, yet scholars continue to know little about the consequences of child death for couples in these regions. With a few exceptions, most studies from the United States have suggested that experiencing a child death elevates conflict between parents and undermines the quality and stability of their relationships. Our findings suggest a similar phenomenon in West and Central Africa: on average, the loss of children under age 5 elevates the risk of IPV. This effect is largest and primarily concentrated in subnational regions where the experience of child bereavement is least common among mothers. We find no analogous effect—or regional variation in the effect—of losing children of older ages.
Previous research has underscored at least three potential explanations for the link between child bereavement and IPV: intense emotional responses, such as anger and grief, that elevate conflict to the point of violence; maternal blame in which husbands view wives as responsible for the survival of children; and social isolation and stigmatization that can exacerbate relationship stress and the blaming of bereaved mothers. Although we are unable to rule out the first explanation entirely, previous research suggests parents’ emotional responses to child bereavement should increase as children age and parents grow more attached (Rogers et al. 2008; Smith-Greenaway and Sennott 2016). Considering that we observe a significant positive effect only for deaths occurring before a child’s fifth birthday, we view this explanation as comparatively weaker than the other potential mechanisms. However, because a small number of women experience the death of older children, and these women are a select group, additional research is needed to further verify variation in the effects of bereavement by child age at death.
Nonetheless, observed variation across children’s age at death aligns with the maternal blame perspective. To the extent that children become less physically vulnerable and less dependent on mothers as they grow and mature (Abdullah et al. 2007; Collins and Russell 1991), husbands and community members may decreasingly view mothers as responsible for child outcomes at later ages. In such a scenario, maternal castigation, in the form of IPV, should emerge primarily in response to the death of young children, as we find here. Future research is nevertheless needed to further verify the extent to which maternal blame is at play. One possible test of this mechanism would be an investigation of heterogeneous effects of child bereavement across cause of death—a test we are unable to conduct because of data limitations. However, that the risk of IPV is concentrated among couples who lose young children in contexts where this experience is less common and thus is potentially more stigmatizing provides further support for the maternal blame perspective.
That the effects of child loss are especially pronounced in contexts where such loss is uncommon and thus where fewer individuals can relate to the experience of child bereavement also provides support for the social isolation perspective. Of course, an alternative explanation for variation across the prevalence of child bereavement could be that underlying gender inequality, family norms, and infrastructural development simultaneously drive the risk of child loss and IPV. Interaction terms between child loss and these regional attributes, however, provide little evidence of this and fail to mediate the interaction between young child bereavement and its regional prevalence.
These findings challenge the dominant paradigm that solely conceives of IPV as a cause of child death rather than as a potential byproduct of it. Scrutinizing assumptions about the causes and consequences of IPV is imperative to developing more comprehensive models of dynamic demographic processes. Our analysis provides an important first step in this direction: supplementary models in which we conceive of IPV as potentially preceding child death suggest that this more common framework is ill-fitting for the case of married mothers in West and Central Africa, where a significant positive association between child death and IPV emerges only after a child’s death could have occurred.
Despite these novel contributions, this study comes with limitations. The first is that we rely on cross-sectional data with self-reported retrospective measures of child death and IPV. Because of social desirability bias and recall bias, these phenomena may be underreported, leading to an underestimation of their prevalence and the relationship between them. Relatedly, our reliance on cross-sectional data sources prevents us from better identifying precise causal pathways driving the relationship we uncover. This same reliance also limits the extent to which we can control for time-varying confounders, such as household economic shocks, that may simultaneously contribute to the evolving risk of child mortality and IPV over time.
This study raises new questions about the consequences of child death for the mothers and fathers who endure it. Rather than continuing to conceptualize child mortality as relevant only to fertility-related behaviors in Africa, our study confirms that a child dying can alter relationship dynamics among bereaved couples as well, and further calls attention to contextual sources of variation in this effect.
Notes
To ensure that observations from no one country drive our conclusions, we conduct a jackknife analysis in which we omit all observations from a given country, one country at a time. The results remain similar in terms of magnitude, direction, and significance to those we present here.
Childless women are excluded because they are never at risk of child bereavement.
Because we estimate IPV initiation, women who experienced IPV onset before first birth are implicitly censored out of our analytic sample.
We perform two sets of supplementary analyses, wherein we (1) relax our sample restrictions and include these women and (2) tighten our sample restrictions and include only women whose lastborn child was born more than five years ago. The results from both supplements are substantively similar to those reported here.
We conduct three sensitivity tests related to our predictor. The first includes a time-varying indicator of infant loss (<1 year old) and a time-varying indicator of child loss (1 to <5 years old) in the same model. A post-estimation Wald test indicates that the two coefficients are not statistically distinguishable. The second tests time-varying indicators of son and daughter loss in the same model and again indicates no significant difference. The third examines a time-varying indicator of the cumulative number of child deaths, which yields substantively similar results to those presented here.
The DHS also asked questions about psychological violence. However, respondents were asked about the timing of IPV initiation only if they responded “yes” to at least one physical or sexual IPV question. Thus, our analysis of IPV initiation is restricted to the onset of physical or sexual violence specifically.
Child marriage is still practiced in some parts of West and Central Africa. As such, a small percentage of respondents partnered at very young ages, including 3.5% who partnered at ages 9, 10, and 11. One woman reported partnering at age 4; we bottom-code this outlying woman at age 9.
Age at first birth was self-reported. Only 0.04% of respondents reported that their first birth occurred at age 10 or 11 (n = 12).
We do not control for women’s participation in household decisions, attitudes toward IPV, or household wealth because these characteristics may be influenced by child bereavement. As a sensitivity test, we reestimate our models including these controls and find the results to be similar to those presented here.
Because we do not find that the effect of losing a child ≥5 years old varies significantly with its regional prevalence, we do not include additional interactions between losing a child ≥5 years old and the regional gender, family, or infrastructural context.
A post-estimation Wald test indicates that the effects of bereavement by a child <5 years old and bereavement by a child ≥5 years old at death do not significantly differ, despite being in the opposite direction. This lack of significant difference may be partly attributable to the relative rarity of losing an older child and/or to the greater selectivity of women who have been continuously married long enough to be at risk of losing an older child.
In a separate model, we test a three-way interaction among individual child bereavement (under age 5), regional prevalence of child bereavement (under age 5), and regional prevalence of IPV. We find the coefficient on this three-way interaction term to be nonsignificant.
Our primary analytic sample of mothers censors out those who experienced IPV initiation before first birth. Because this could downwardly bias our estimates here, we test additional models in which we include these women’s offspring. Results lead to substantively similar conclusions.
Because triplets and quadruplets are rare, they are included in the “twin” category.
References
Abdullah, S., Adazu, K., Masanja, H., Diallo, D., Hodgson, A., Ilboudo-Sanogo, E.,... Smith, T. (2007). Patterns of age-specific mortality in children in endemic areas of sub-Saharan Africa. American Journal of Tropical Medicine and Hygiene, 77(Suppl. 6), 99–105.
Ackerson, L. K., & Subramanian, S. V. (2009). Intimate partner violence and death among infants and children in India. Pediatrics, 124, e878–e889. https://doi.org/10.1542/peds.2009-0524
Ai, C., & Norton, E. C. (2003). Interaction terms in logit and probit models. Economics Letters, 80, 123–129.
Aksan, A.-M. (2014). Effects of childhood mortality and morbidity on the fertility transition in sub-Saharan Africa. Population and Development Review, 40, 311–329.
Albuquerque, S., Pereira, M., & Narciso, I. (2016). Couple’s relationship after the death of a child: A systematic review. Journal of Child and Family Studies, 25, 30–53.
Anderson, K. L. (2008). Is partner violence worse in the context of control? Journal of Marriage and Family, 70, 1157–1168.
Arnold, J., Gemma, P. B., & Cushman, L. F. (2005). Exploring parental grief: Combining quantitative and qualitative measures. Archives of Psychiatric Nursing, 19, 245–255.
Åsling-Monemi, K., Peña, R., Ellsberg, M. C., & Persson, L. Å. (2003). Violence against women increases the risk of infant and child mortality: A case-referent study in Nicaragua. Bulletin of the World Health Organization, 81, 10–16.
Balk, D., Pullum, T., Storeygard, A., Greenwell, F., & Neuman, M. (2004). A spatial analysis of childhood mortality in West Africa. Population, Space and Place, 10, 175–216.
Barrera, M., O’Connor, K., D’Agostino, N. M., Spencer, L., Nicholas, D., Jovcevska, V.,... Schneiderman, G. (2009). Early parental adjustment and bereavement after childhood cancer death. Death Studies, 33, 497–520.
Behrman, J. (2016, March–April). Educational assortative mating and implications for between and within household inequality: Evidence from East Africa. Paper presented at the annual meeting of the Population Association of America, Washington, DC.
Bongaarts, J., Frank, O., & Lesthaeghe, R. (1984). The proximate determinants of fertility in sub-Saharan Africa. Population and Development Review, 10, 511–537.
Caldwell, J. C., & Caldwell, P. (1987). The cultural context of high fertility in sub-Saharan Africa. Population and Development Review, 13, 409–437.
Castle, S. E. (1994). The (re)negotiation of illness diagnoses and responsibility for child death in rural Mali. Medical Anthropology Quarterly, 8, 314–335.
Collins, W. A., & Russell, G. (1991). Mother-child and father-child relationships in middle childhood and adolescence: A developmental analysis. Developmental Review, 11, 99–136.
Defo, B. K. (1998). Fertility response to infant and child mortality in Africa with special reference to Cameroon. In M. R. Montgomery & B. Cohen (Eds.), From death to birth: Mortality decline and reproductive change (pp. 254–315). Washington, DC: National Academies Press.
Devries, K. M., Mak, J. Y. T., Garcia-Moreno, C., Petzold, M., Child, J. C., Falder, G.,... Rosenfeld, R. (2013). The global prevalence of intimate partner violence against women. Science, 340, 1527–1528.
Dunn, D. S., Clinton Goldbach, K. R., Lasker, J. N., & Toedter, L. J. (1991). Explaining pregnancy loss: Parents’ and physicians’ attributions. Omega: Journal of Death and Dying, 23, 13–23.
Dyregrov, A., & Gjestad, R. (2011). Sexuality following the loss of a child. Death Studies, 35, 289–315.
Eilegård, A., & Kreicbergs, U. (2010). Risk of parental dissolution of partnership following the loss of a child to cancer: A population-based long-term follow-up. Archives of Pediatrics & Adolescent Medicine, 164, 100–101.
Emery, C. R., Thapa, S., Do, M. H., & Chan, K. L. (2015). Do family order and neighbor intervention against intimate partner violence protect children from abuse? Findings from Kathmandu. Child Abuse & Neglect, 41, 170–181.
Essakow, K. L., & Miller, M. M. (2013). Piecing together the shattered heirloom: Parents’ experiences of relationship resilience after the violent death of a child. American Journal of Family Therapy, 41, 299–310.
Fish, W. C. (1986). Differences of grief intensity in bereaved parents. In T. A. Rando (Ed.), Parental loss of a child (pp. 415–428). Champaign, IL: Research Press.
Gold, K. J., Sen, A., & Leon, I. (2018). Whose fault is it anyway? Guilt, blame, and death attribution by mothers after stillbirth or infant death. Illness, Crisis & Loss, 26, 40–57.
Gyimah, S. O., & Fernando, R. (2004). Intentional replacement of dead children in sub-Saharan Africa: Evidence from Ghana and Kenya. Canadian Studies in Population, 31, 33–53.
Hastings, S. O. (2000). Self-disclosure and identity management by bereaved parents. Communication Studies, 51, 352–371.
Hatcher, A. M., Romito, P., Odero, M., Bukusi, E. A., Onono, M., & Turan, J. M. (2013). Social context and drivers of intimate partner violence in rural Kenya: Implications for the health of pregnant women. Culture, Health & Sexuality, 15, 404–419.
Havik, P. J. (2016). Hybridising medicine: Illness, healing and the dynamics of reciprocal exchange on the Upper Guinea Coast (West Africa). Medical History, 60, 181–205.
Haws, R. A., Mashasi, I., Mrisho, M., Schellenberg, J. A., Darmstadt, G. L., & Winch, P. J. (2010). “These are not good things for other people to know”: How rural Tanzanian women’s experiences of pregnancy loss and early neonatal death may impact survey data quality. Social Science & Medicine, 71, 1764–1772.
Hays, S. (1998). The cultural contradictions of motherhood. New Haven, CT: Yale University Press.
Hung, K. J., Scott, J., Ricciotti, H. A., Johnson, T. R., & Tsai, A. C. (2012). Community-level and individual-level influences of intimate partner violence on birth spacing in sub-Saharan Africa. Obstetrics & Gynecology, 119, 975–982.
Jackson, D., & Mannix, J. (2004). Giving voice to the burden of blame: A feminist study of mothers’ experiences of mother blaming. International Journal of Nursing Practice, 10, 150–158.
Jejeebhoy, S. J. (1998). Associations between wife-beating and fetal and infant death: Impressions from a survey in rural India. Studies in Family Planning, 29, 300–308.
Karamagi, C. A. S., Tumwine, J. K., Tylleskar, T., & Heggenhougen, K. (2007). Intimate partner violence and infant morbidity: Evidence of an association from a population-based study in Eastern Uganda in 2003. BMC Pediatrics, 7(Article: 34). https://doi.org/10.1186/1471-2431-7-34
Kiros, G.-E., & Hogan, D. P. (2001). War, famine and excess child mortality in Africa: The role of parental education. International Journal of Epidemiology, 30, 447–455.
Letourneau, N. L., Morris, C. Y., Secco, L., Hughes, J., & Critchley, K. (2013). Mothers and infants exposed to intimate partner violence compensate. Violence and Victims, 28, 571–586.
Lindstrom, D. P., & Kiros, G.-E. (2007). The impact of infant and child death on subsequent fertility in Ethiopia. Population Research and Policy Review, 26, 31–49.
Lupton, D. (2012). “Precious cargo”: Foetal subjects, risk and reproductive citizenship. Critical Public Health, 22, 329–340.
Lyngstad, T. H. (2013). Bereavement and divorce: Does the death of a child affect parents’ marital stability? Family Science, 4, 79–86.
Madhavan, S. (2001). Female cooperation and conflict in rural Mali: Effects on infant and child survival. Journal of Comparative Family Studies, 32, 75–98.
McBride, M. C., & Toller, P. (2011). Negotiation of face between bereaved parents and their social networks. Southern Communication Journal, 76, 210–229.
Meij, L. W.‐d., Stroebe, M., Schut, H., Stroebe, W., van den Bout, J., Heijden, P. G. M., & Dijkstra, I. (2008). Parents grieving the loss of their child: Interdependence in coping. British Journal of Clinical Psychology, 47, 31–42.
Meyer, A. C., Opoku, C., & Gold, K. J. (2016). “They say I should not think about it”: A qualitative study exploring the experience of infant loss for bereaved mothers in Kumasi, Ghana. Omega: Journal of Death and Dying, 7, 267–279.
Milkie, M. A., Mattingly, M. J., Nomaguchi, K. M., Bianchi, S. M., & Robinson, J. P. (2004). The time squeeze: Parental statuses and feelings about time with children. Journal of Marriage and Family, 66, 739–761.
Murphy, S. A., Chung, I.-J., & Johnson, L. C. (2002). Patterns of mental distress following the violent death of a child and predictors of change over time. Research in Nursing & Health, 25, 425–437.
Murphy, S. A., Johnson, L. C., Chung, I.-J., & Beaton, R. D. (2003a). The prevalence of PTSD following the violent death of a child and predictors of change 5 years later. Journal of Traumatic Stress, 16, 17–25.
Murphy, S. A., Johnson, L. C., Wu, L., Fan, J. J., & Lohan, J. (2003b). Bereaved parents’ outcomes 4 to 60 months after their children’s deaths by accident, suicide, or homicide: A comparative study demonstrating differences. Death Studies, 27, 39–61.
Murphy, S. A., Lohan, J., Dimond, M., & Fan, J. (1998). Network and mutual support for parents bereaved following the violent deaths of their 12-to 28-year-old children: A longitudinal, prospective analysis. Journal of Personal & Interpersonal Loss, 3, 303–333.
Nixon, K. L., Tutty, L. M., Radtke, H. L., Ateah, C. A., & Ursel, E. J. (2017). Protective strategies of mothers abused by intimate partners: Rethinking the deficit model. Violence Against Women, 23, 1271–1292.
Oliver, L. E. (1999). Effects of a child’s death on the marital relationship: A review. Omega: Journal of Death and Dying, 39, 197–227.
Peterman, A., Behrman, J., & Palermo, T. (2015, April–May). Effect of education on women’s experience of inimate partner violence: Universal primary education as a natural experiment in Malawi and Uganda. Paper presented at the annual meeting of the Population Association of America, San Diego, CA. Retrieved from http://paa2015.princeton.edu/abstracts/151336
Reilly-Smorawski, B., Armstrong, A. V., & Catlin, E. A. (2002). Bereavement support for couples following death of a baby: Program development and 14-year exit analysis. Death Studies, 26, 21–37.
Ricci, J. A., Jerome, N. W., Sirageldin, I., Aly, H., Moussa, W., Galal, O.,... Kirksey, K. (1996). The significance of children’s age in estimating the effect of maternal time use on children’s well-being. Social Science & Medicine, 42, 651–659.
Riches, G., & Dawson, P. (1996). Communities of feeling: The culture of bereaved parents. Mortality, 1, 143–161.
Rico, E., Fenn, B., Abramsky, T., & Watts, C. (2011). Associations between maternal experiences of intimate partner violence and child nutrition and mortality: Findings from Demographic and Health Surveys in Egypt, Honduras, Kenya, Malawi and Rwanda. Journal of Epidemiology & Community Health, 65, 360–367.
Rogers, C. H., Floyd, F. J., Seltzer, M. M., Greenberg, J., & Hong, J. (2008). Long-term effects of the death of a child on parents’ adjustment in midlife. Journal of Family Psychology, 22, 203–211.
Sandberg, J. (2006). Infant mortality, social networks, and subsequent fertility. American Sociological Review, 71, 288–309.
Scheper-Hughes, N. (1992). Death without weeping: The violence of everyday life in Brazil. Berkeley: University of California Press.
Schwab, R. (1996). Gender differences in parental grief. Death Studies, 20, 103–113.
Schwab, R. (1998). A child’s death and divorce: Dispelling the myth. Death Studies, 22, 445–468.
Sievert, M. (2015). Rural electrification and domestic violence in sub-Saharan Africa (RWI Working Paper No. 570). Retrieved from https://doi.org/10.2139/ssrn.2706469
Silverman, J. G., Decker, M. R., Gupta, J., Kapur, N., Raj, A., & Naved, R. T. (2009). Maternal experiences of intimate partner violence and child morbidity in Bangladesh: Evidence from a national Bangladeshi sample. Archives of Pediatrics & Adolescent Medicine, 163, 700–705.
Sisay, M. M., Yirgu, R., Gobezayehu, A. G., & Sibley, L. M. (2014). A qualitative study of attitudes and values surrounding stillbirth and neonatal mortality among grandmothers, mothers, and unmarried girls in rural Amhara and Oromiya regions, Ethiopia: Unheard souls in the backyard. Journal of Midwifery & Women’s Health, 59(Suppl. 1), S110–S117.
Smith-Greenaway, E. (2017). Community context and child health: A human capital perspective. Journal of Health and Social Behavior, 58, 307–321.
Smith-Greenaway, E., & Sennott, C. (2016). Death and desirability: Retrospective reporting of unintended pregnancy after a child’s death. Demography, 53, 805–834.
Smith-Greenaway, E., & Trinitapoli, J. (2014). Polygynous contexts, family structure, and infant mortality in sub-Saharan Africa. Demography, 51, 341–366.
Smith-Greenaway, E., & Trinitapoli, J. (2019, April). New population indicators of mortality: Maternal-oriented measures of infant and under-five mortality. Paper presented at the annual meeting of the Population Association of America, Austin, TX. Retrieved from http://paa2019.populationassociation.org/uploads/193182
Sobkoviak, R. M., Yount, K. M., & Halim, N. (2012). Domestic violence and child nutrition in Liberia. Social Science & Medicine, 74, 103–111.
Song, J., Floyd, F. J., Seltzer, M. M., Greenberg, J. S., & Hong, J. (2010). Long-term effects of child death on parents’ health-related quality of life: A dyadic analysis. Family Relations, 59, 269–282.
Straus, M. A., Hamby, S. L., Boney-McCoy, S., & Sugarman, D. B. (1996). The Revised Conflict Tactics Scales (CTS2). Journal of Family Issues, 17, 283–316.
Sullivan, C. M., Nguyen, H., Allen, N., Bybee, D., & Juras, J. (2001). Beyond searching for deficits. Journal of Emotional Abuse, 2(1), 51–71.
Takyi, B. K., & Mann, J. (2006). Intimate partner violence in Ghana, Africa: The perspectives of men regarding wife beating. International Journal of Sociology of the Family, 32, 61–78.
Toller, P. W. (2005). Negotiation of dialectical contradictions by parents who have experienced the death of a child. Journal of Applied Communication Research, 33, 46–66.
Toller, P. W. (2008). Bereaved parents’ negotiation of identity following the death of a child. Communication Studies, 59, 306–321.
Toller, P. W., & Braithwaite, D. O. (2009). Grieving together and apart: Bereaved parents’ contradictions of marital interaction. Journal of Applied Communication Research, 37, 257–277.
Towns, A. M., Eyi, S. M., & van Andel, T. (2014). Traditional medicine and childcare in Western Africa: Mothers’ knowledge, folk illnesses, and patterns of healthcare-seeking behavior. PLoS One, 9(8), e105972. https://doi.org/10.1371/journal.pone.0105972
Trinitapoli, J., & Yeatman, S. (2018). The flexibility of fertility preferences in a context of uncertainty. Population and Development Review, 44, 87–116.
Trussell, J., & Pebley, A. R. (1984). The potential impact of changes in fertility on infant, child, and maternal mortality. Studies in Family Planning, 15, 267–280.
Umberson, D. (2017). Black deaths matter: Race, relationship loss, and effects on survivors. Journal of Health and Social Behavior, 58, 405–420.
VanderEnde, K. E., Yount, K. M., Dynes, M. M., & Sibley, L. M. (2012). Community-level correlates of intimate partner violence against women globally: A systematic review. Social Science & Medicine, 75, 1143–1155.
Villarreal, A. (2007). Women’s employment status, coercive control, and intimate partner violence in Mexico. Journal of Marriage and Family, 69, 418–434.
Wijngaards-de Meij, L., Stroebe, M., Schut, H., Stroebe, W., van den Bout, J., Heijden, P. G. M., & Dijkstra, I. (2008). Parents grieving the loss of their child: Interdependence in coping. British Journal of Clinical Psychology, 47, 31–42.
Wilkinson, S. E., & Callister, L. C. (2010). Giving birth: The voices of Ghanaian women. Health Care for Women International, 31, 201–220.
Wing, D. G., Burge-Callaway, K., Rose Clance, P., & Armistead, L. (2001). Understanding gender differences in bereavement following the death of an infant: Implications of or treatment. Psychotherapy: Theory, Research, Practice, Training, 38, 60–73.
World Bank. (2015). Data bank: Mortality rate, under-5 (per 1,000 live births). Washington, DC: World Bank. Retrieved from https://data.worldbank.org/indicator/SH.DYN.MORT?end=2015&start=1960
Yount, K. M., DiGirolamo, A. M., & Ramakrishnan, U. (2011). Impacts of domestic violence on child growth and nutrition: A conceptual review of the pathways of influence. Social Science & Medicine, 72, 1534–1554.
Yount, K. M., Zureick-Brown, S., Halim, N., & LaVilla, K. (2014). Fertility decline, girls’ well-being, and gender gaps in children’s well-being in poor countries. Demography, 51, 535–561.
Acknowledgments
The authors are grateful to Julia Behrman, Monica Caudillo, Kelly Raley, Alex Weinreb, and Rob Crosnoe for their insightful comments on earlier iterations of this study. This research was supported by Grant P2CHD042849, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(PDF 375 kb)
Rights and permissions
About this article
Cite this article
Weitzman, A., Smith-Greenaway, E. The Marital Implications of Bereavement: Child Death and Intimate Partner Violence in West and Central Africa. Demography 57, 347–371 (2020). https://doi.org/10.1007/s13524-019-00846-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-019-00846-7