Abstract
Objective
To study the 24-h glucose profile of patients with mild GDM using the commercially available Abbot Libre continuous glucose monitoring system (CGMS) and compare them with pregnant women with normoglycemia (gestational age comparable).
Methods
A case control study conducted between 2019-2020 followed eligible pregnant women diagnosed with GDM according to Diabetes in Pregnancy Study Group India criteria, after the placement of a CGMS.
Results
Twenty-one GDM patients whose mean age was 27.1 ± 3.3 years with gestational age 28 weeks (24–32) and thirty pregnant women with normoglycemia whose mean age was 25.7 ± 4.2 years and gestational age 26 weeks (23–34) were enrolled in the study. Fasting, pre-breakfast, 2 h post lunch, day time and lowest nocturnal glucose were significantly higher in the GDM group than in controls. Glycemic variability indices like standard deviation of blood glucose, J index, and mean amplitude of glycemic excursions were also significantly higher in GDM patients. GDM patients spent more time above >140 mg/dl than controls.
Conclusion
GDM patients, who have mild hyperglycemia but not overt diabetes, also have an abnormal 24 h glucose profile as compared to normal pregnancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM) is diabetes diagnosed during pregnancy that was not overt prior to gestation. Hyperglycemia during pregnancy not only is associated with adverse pregnancy outcomes but has major long term metabolic and cardiovascular implications for both the mother and the child [1,2,3,4]. In utero exposure to excess nutrition leads to fetal programming resulting in increased risk of obesity, type 2 diabetes, metabolic syndrome and cardiovascular disease in adulthood, “theory of fetal origins of adult diseases” [5]. To prevent transgenerational transmission of these metabolic disorders is the major consideration for optimal glycemic control. The treatment goal is to achieve normoglycemia as far as possible without causing hypoglycemia or marked fluctuations in glucose levels, glycemic variability which in itself is a high-risk factor for diabetes complications [6, 7]. Diagnostic criteria for GDM have evolved with time. The widely followed criterion is by the International Association of the Diabetes and Pregnancy Study Group (IADPSG) based on the results of Hyperglycemia and adverse pregnancy outcome (HAPO) study [8].
Diabetes in Pregnancy Study Group India (DIPSI) followed the World Health Organisation 1999 criteria, but using only the 2-h post glucose value >140 mg/dl as GDM irrespective of their meal time [9]. It is well understood that this low cut off will overdiagnose women, but as has been shown in the HAPO study, there is no single cut off of glucose level which increases the perinatal risk, rather it is a continuum. According to the standard guidelines from National Health Mission, in 2014 all pregnant women should undergo testing for glucose tolerance abnormality at their first antenatal visit and DIPSI criteria are to be followed nationally. Seshiah et al. have shown that there is close agreement between prevalence of GDM in a community if diagnosed by IADPSG or DIPSI criteria [10].
With the lowering of the threshold for diagnosis of GDM, prevalence of pregnancies complicated with diabetes has markedly increased. The prevalence of GDM in Indians was earlier reported as 7–18% [11]. Using the IADPSG criteria, prevalence of GDM has been reported as high as 41.9% from North India [12] and 38% in South Asians settled outside India [13]. In addition, it is likely to classify mild hyperglycemia as GDM in a subgroup of women who may have less severe metabolic disturbances. Whether these women with GDM who have minimal elevation of blood glucose but not overt diabetes also have glycemic variability and warrant active treatment is unanswered.
Self-monitoring of blood glucose by finger stick determines glucose at that specific point and is unable to depict the glucose profile for the whole day. Continuous glucose monitor system (CGMS) is a wearable body sensor that automatically measures glucose at regular intervals (ranging from every 5 to 15 min) from interstitial fluid and enables us to study glucose profiles in detail, helping to unmask differences otherwise not detected by the finger stick glucose determinations. There is paucity of literature on use of CGMS in women GDM who have minimal elevation of blood glucose but not overt diabetes. Previous studies have used CGMS for 3 days and also variability index of glycemia in GDM has not been studied in detail. With this background, the present study was designed to evaluate glycemic patterns and variability in women with mild GDM diagnosed by DIPSI criteria and compare them with controls (pregnant women with normal OGTT) with similar gestational age.
Material and methods
Study design
A case control study conducted in the outpatient clinics of a tertiary care hospital from North India from January 2019 to December 2020. The study was approved by the institutional ethics committee (Reference no. IEC code-2019-108-IMP-109). All women who fulfilled the inclusion criteria were informed about the study and the consenting participants were enrolled.
Inclusion criteria include age 18 to 35 years, singleton pregnancy, natural conception and not after assisted reproduction therapy, GDM according to DIPSI criteria [8]. Diagnosis of GDM is made if the 2-h post 75 g oral glucose load which is given irrespective of the last meal is ≥140 mg/dl.
Women who were > 35 years or had previous history of GDM, HbA1c > 7%, overt diabetes, or needed treatment with oral hypoglycemic agent or insulin for control of glycemia, had multiple pregnancy, pregnancy induced hypertension or any other complication of pregnancy, bad obstetric history or used drugs that affect glucose metabolism were excluded from the study.
Detailed questionnaire was completed for each participant, documenting demographic details, obstetric history and family history of diabetes mellitus. The details of anthropometric measurements (weight, height, body mass index BMI), blood pressure were noted. Hemoglobin, glycosylated hemoglobin (HbA1c), lipid profile and liver enzymes were estimated in a fasting sample.
Free Style Libre Pro flash continuous glucose monitoring system (Abbott Diabetes Care Ltd, Oxon UK) was implanted on the non-dominant arm as per standard insertion guidelines. All participants were advised to write the timing of their three major meals for all days the CGMS was inserted. Sensor data was accepted if the sensor recorded for >70% of the time of application, at least for 10 of the 14 days of use. All GDM patients received appropriate dietary advice and monitored blood glucose as per their treating physician’s advice.
CGMS parameters
The readings from the device were read by the CGMS reader and transferred to an EXCEL spreadsheet. The parameters calculated from the 14-day records were mean glucose, mean values of each meal-related parameter (pre-prandial, 1-h and 2-h post-prandial glucose values, peak glucose value and time to peak value, time in target range, hypoglycemia (<60) and above target >140 mg/dl as described below-
-
FBG — Glucose value after at least 8 h of fasting
-
Pre-prandial BG — Glucose value directly before breakfast, lunch, and dinner meal
-
1-h PP BG — Glucose value 1 h after the meal start time
-
2-h PP BG — Glucose value 2 h after the meal start time
-
Mean 24-h BG — Mean of all measures in 24 h
-
Mean daytime BG — Mean of all measures between 6 am to 12 am
-
Mean nocturnal BG — Mean of all measures between 12 am to 6 am
-
Lowest nocturnal — Lowest glucose value between 12 am to 6 am
-
Peak PP BG — Highest PP glucose within 2 h of meal start time
-
Time to PP peak — Time from meal start to peak PP BG
Glycemic variability indices which were calculated from the CGMS readings are as follows — (Details in Table 1).
The standard deviation (SD) of mean glycemia of CGM data is the simplest tool for assessment of glycemic variability.
J index [14]— It is a measure of quality of glycemic control dependent on the combination of information from the mean and SD calculated as 0.001 × (mean + SD)2
Continuous overall net glycemic action (CONGA) is identical to SD but assesses glucose variability within a predetermined time window. The estimation of this parameter is based on the measurement of the discrepancies between glucose values measured at regular time intervals than on the SD of these differences [15].
The mean amplitude of glucose excursion (MAGE) was designed to capture mealtime-related glucose excursions. Measurement based on the arithmetic mean of differences between successive peaks and nadirs of differences greater than one SD of mean glycemia. It is meant to major glucose swings and exclude minor ones [16].
Lability index (LI) was calculated based on the change in glucose levels over time and compared with a clinical assessment of glycemic lability [17].
Validity of CGM data is acceptable, CGM-derived glucose measurements correlate well with venous glucose levels [18,19,20].
Statistics analysis
IBM SPSS Statistics 27 was used for statistical analyses. Shapiro–Wilk test was used to assess normality of quantitative variables. Chi-square and Fisher exact test were used for categorical variable. Student’s t test for independent samples and Mann–Whitney U test were used to compare variables which were normally or not normally distributed, respectively in two groups. Data are presented as n (%), mean ± SD or median (quartile [q] 25–q75). p value of <0.05 was considered statistically significant.
Results
Baseline data
Twenty-one GDM patients, mean age of 27 .1 ± 3.3 years with gestational age 28 weeks (24–32) and the control group of thirty pregnant women with normoglycemia, mean age of 25.7 ± 4.2 years with gestational age 26 weeks (23–34) were enrolled in the study. The mean BMI of GDM patients was 25.5± 2.9 kg/m2 and of the control group was 24.7±3.8 kg/m2. GDM group had significantly higher glucose value at 2 h in the OGTT 155 (143–181) mg/dl vs 106 (92–121) mg/dl in control (p value = 0.000), HbA1c of the GDM group was 5.3% (5–5.7) and 5% (4.8–5.2) in the control group (p value = 0.003). Serum triglyceride was higher in the GDM group 261(233–286) mg/dl as compared to the controls 208 (156–257) mg/dl (p value = 0.003). Family history of diabetes was similar in both the groups.
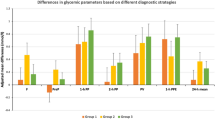
Comparison of CGMS-based glycemic data between GDM and controls is shown in Table 2. Readings in the sensors were available for 93% of the time they were applied, 13 of the 14 days used. Fasting glucose was significantly higher in GDM group 75.47 ± 11.8 mg/dl as compared to 67.34± 8.7 mg/dl in control group and (p value = 0.007).
Of the CGM parameters, pre-breakfast glucose was significantly higher 79± 15.7 mg/dl in the GDM group vs controls 71± 8.3mg/dl (p value=0.042) and 2 h post-lunch glucose was significantly higher 98.2(91.5–119.5) mg/dl in the GDM group vs controls 91.7(87.2–98.8) mg/dl (p value=0.028). GDM women spent significantly more time above >140 mg% glucose than control women (0.87% (0–7.6%) in GDM versus 0(0–0.57%) in control group, p =0.015). Day time glucose and lowest nocturnal glucose also was significantly higher in GDM group than control (p value < 0.05).
CGMS data for glycemic variability
Other calculated indices of glycemic variability including, SD, J index, CONGA, LI, and MAGE were also significantly higher in the GDM group as compared to controls p value< 0.05 (Table 3).
Taking the group as a whole, HbA1c showed a moderate correlation with mean sugar (Pearson correlation 0.619), fasting sugar (Pearson correlation 0.585), and indices of glycemic variability like SD (Pearson correlation 0.583), CONGA (Pearson correlation 0.496), LI (Pearson correlation 0.616), J index (Pearson correlation 0.648), MAGE (Pearson correlation 0.593) and lowest sugar (Pearson correlation 0.596) but had no correlation with time in range.
BMI had a weak correlation with fasting sugar and the lowest sugar value but did not correlate with other glycemic variability parameters.
Newborn or delivery outcomes were similar in both groups and no GDM mother delivered large gestational age (LGA) baby.
Discussion
CGMS data of GDM patients who have minimal elevation of blood glucose but not overt diabetes in our study showed that the overall glucose exposure was similar in the GDM patients and pregnant women of similar gestational age with normoglycemia. However, GDM patients were spending significantly higher amount of time with blood glucose >140 mg/dl and had significantly higher glycemic variability as compared to women with normoglycemia.
In our study, all glycemic variability indices SD, J index, CONGA, LI and MAGE were significantly higher in the GDM group as compared to controls. Using a 72-h glucose profile, Carriero et al. [21] also found similar results in 33 patients of mild GDM. Glycemic variability (GV) includes both upward (post prandial) and downward (mostly in between meals) variation in blood glucose. There is enough evidence in literature that GV plays an important role in diabetic complications and has more deleterious effect than sustained hyperglycemia [6]. MAGE is considered as the gold standard index of GV. Su et al. [22] found significantly higher GV indices especially MAGE in women with GDM as compared to pregnant women with normoglycemia and non-pregnant control women. In their study, early phase insulin secretion was the strongest independent contributor to MAGE in the GDM group.
Current recommendations for women with GDM is to monitor blood sugar by finger stick method 4 times a day and targets of glycemic control are fasting glucose targets of ≤5.3 mmol/L (≤95.4 mg/dL) and 1-h postmeal glucose ≤7.8 mmol/L (≤140.4 mg/dL). However, women who achieve these targets still have adverse outcomes including large for gestational babies. Law et al.[23] using functional data analysis on the CGMS readings showed that mean glucose was significantly higher in mothers who delivered large for gestational babies and the higher mean glucose was driven by a significantly higher glucose for 6 h overnight, which is unlikely to be detected by the standard finger prick testing method. Intermittent capillary glucose monitoring obviously has its inherent limitations; glucose abnormality will not be picked up at times other than when it has been recommended. CGMS giving a temporal profile highlights this limitation.
Cautious judgement has to be made of these findings as GDM patients who were managed with only medical nutritional therapy were included in both the studies; all those women who required pharmacological treatment were excluded.
Majority of our women had fasting blood glucose <92 mg/dl according to their CGMS data, similar to what has been reported by Nigam et al. [24] (all GDM women had values <92 mg/dl) and Carreiro et al. [18] (82% of their population). Nigam et al.[24] also used DIPSI criteria for diagnosis of GDM. All pre and post meal blood glucose values at all time points were significantly higher in the GDM women as compared to healthy pregnant subjects in their study (Nigam et al.), in contrast, in our study all the values were higher but only the 2-h post lunch value was statistically significant. It seems logical also as lunch is the heaviest meal rich in carbohydrates in Indians. Significantly higher blood glucose values post breakfast and post dinner were reported by Carreiro et al. as well. It is important to note that the glucose values in all the three studies were below the therapeutic targets advised for good control in GDM patients.
CGMS data shows that women with GDM who have minimal elevation of blood glucose but not overt diabetes also show significant GV and spend a significant amount of time (0.20 h) with blood glucose >140 mg/dl. If we had included all women who had GDM meaning even those women who required pharmacological therapy for glycemic control but not overt diabetes, the difference from normoglycemic women was likely to have been more.
A major limitation is the small study number and larger data set is needed to validate our results. Secondly as the number was small, we could not analyse the pregnancy outcomes which is of importance as it would highlight the importance or relevance of glycemic variability when the absolute values of blood sugar are less than the target set for glycemic control in GDM. In the hypoglycemic range reliability of CGMS readings are a limitation. Simultaneous capillary blood glucose values were not available in our study.
In the future, studies adequately powered need to be planned with the aim of using CGMS in women with GDM who have minimal elevation of blood glucose but not overt diabetes to improve glycemic variability and to study its effect of pregnancy outcomes.
GDM was diagnosed according to DIPSI criteria and not the IADPSG but this cannot be a major limitation as these are the national guidelines and followed by obstetricians in India. Moreover, the study was not designed to validate the DIPSI criteria.
Strength of the study: This is the first study that offered insight into 10 to 14 days use of CGM in women with GDM who have minimal elevation of blood glucose but not overt diabetes to calculate the various glycemic variability parameters.
Conclusion
GDM patients who have mild hyperglycemia but not overt diabetes also have an abnormal 24-h glucose profile with increased glycemic variability and spend more time above 140 mg/dl, as compared to pregnant women of similar age and gestational age with normoglycemia.
Data Availability
Data can be provided on a genuine request.
References
Sweeting A, Wong J, Murphy HR, Ross GP. A clinical update on gestational diabetes mellitus. Endocr Rev. 2022;bnac003.
Lowe WL Jr, Scholtens DM, Kuang A, Linder B, Lawrence JM, Lebenthal Y, et al. HAPO Follow-up Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcome follow-up study (HAPO FUS): maternal gestational diabetes mellitus and childhood glucose metabolism. Diabetes Care. 2019;42(3):372-80.
Arabin B, Baschat AA. Pregnancy: an underutilized window of opportunity to improve long-term maternal and infant health-an appeal for continuous family care and interdisciplinary communication. Front Pediatr. 2017;5:69.
Tam WH, Ma RCW, Ozaki R, Li AM, Chan MHM, Yuen LY, et al. In utero exposure to maternal hyperglycemia increases childhood cardiometabolic risk in offspring. Diabetes Care. 2017;40(5):679–86.
Rinaudo P, Wang E. Fetal programming and metabolic syndrome. Annu Rev Physiol. 2012;74:107–30.
Monnier L, Colette C. Glycemic variability: should we and can we prevent it? Diabetes Care. 2008;31(Suppl 2):S150-54.
Sun B, Luo Z, Zhou J. Comprehensive elaboration of glycemic variability in diabetic macrovascular and microvascular complications. Cardiovasc Diabetol. 2021;20(1):9.
Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, Damm P, et al. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82.
Seshia V, Balaji V, Balaji M, Sekar A, Sanjeevi C. Green A “One step procedure for screening and diagnosis of gestational diabetes mellitus.” J Obstetrics Gynecol India. 2005;55:525–9.
Seshiah V, Balaji V, Shah SN, Joshi S, Das AK, Sahay BK, et al. Diagnosis of gestational diabetes mellitus in the community. J Assoc Physicians India. 2012;60:15–7.
Seshiah V, Balaji V, Balaji MS, Paneerselvam A, Arthi T, Thamizharasi M, et al. Prevalence of gestational diabetes mellitus in South India (Tamil Nadu)–a community based study. J Assoc Physicians India. 2008;56:329–33.
Gopalakrishnan V, Singh R, Pradeep Y, Kapoor D, Rani AK, Pradhan S, et al. Evaluation of the prevalence of gestational diabetes mellitus in North Indians using the International Association of Diabetes and Pregnancy Study groups (IADPSG) criteria. J Postgrad Med. 2015;61(3):155–8.
Agarwal MM, Dhatt GS, Shah SM. Gestational diabetes mellitus: simplifying the international association of diabetes and pregnancy diagnostic algorithm using fasting plasma glucose. Diabetes Care. 2010;33:2018–20.
Wójcicki JM. “J”-index. A new proposition of the assessment of current glucose control in diabetic patients. HormMetab Res. 1995;27(1):41–2.
McDonnell CM, Donath SM, Vidmar SI, Werther GA, Cameron FJ. A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technol Ther. 2005;7(2):253–63.
Service FJ, Molnar GD, Rosevear JW, Ackerman E, Gatewood LC, Taylor WF. Mean amplitude of glycemic excursions, a measure of diabetic instability. Diabetes. 1970;19(9):644–55.
Ryan EA, Shandro T, Green K, Paty BW, Alexander Senior P, Bigam D, et al. Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Diabetes. 2004;53:955–62.
Merino J, Linenberg I, Bermingham KM, Ganesh S, Bakker E, Delahanty LM, et al. Validity of continuous glucose monitoring for categorizing glycemic responses to diet: implications for use in personalized nutrition. Am J Clin Nutr. 2022;115(6):1569–76.
Luijf YM, Mader JK, Doll W, Pieber T, Farret A, Place J, et al. Accuracy and reliability of continuous glucose monitoring systems: a head-to-head comparison. Diabetes Technol Ther. 2013;15(8):722–7.
Akintola AA, Noordam R, Jansen SW, Ballieux BE, Cobbaert CM, Mooijaart SP, et al. Accuracy of continuous glucose monitoring measurements in normo-glycemic individuals. PLOS ONE. 2015;10(10):e0139973.
Carreiro MP, Lauria MW, Naves GN, Miranda PA, Leite RB, Rajão KM, et al. Seventy two-hour glucose monitoring profiles in mild gestational diabetes mellitus: differences from healthy pregnancies and influence of diet counseling. Eur J Endocrinol. 2016;175(3):201–9.
Su JB, Wang XQ, Chen JF, Wu G, Jin Y, Xu F, et al. Glycemic variability in gestational diabetes mellitus and its association with β cell function. Endocrine. 2013;43(2):370–5.
Law GR, Ellison GT, Secher AL, Damm P, Mathiesen ER, Temple R, et al. Analysis of continuous glucose monitoring in pregnant women with diabetes: distinct temporal patterns of glucose associated with large-for-gestational-age infants. Diabetes Care. 2015;38(7):1319–25.
Nigam A, Sharma S, Varun N, Munjal YP, Prakash A. Comparative analysis of 2-week glycaemic profile of healthy versus mild gestational diabetic pregnant women using flash glucose monitoring system: an observational study. BJOG. 2019;126(S4):27–33.
Acknowledgments
I would like to acknowledge Prof Eesh Bhatia for his valuable inputs in reviewing the original manuscript, Prabhakar Misra Dr Bibhuti Mohanta for helping in recruiting patients, diabetes nurse in helping with CGMS application and contact with patients.
Funding
DM project funding from Endocrine Society of India (ESI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical clearance
A case control study conducted in the outpatient clinics of a tertiary care hospital from North India from January 2019 to December 2020. The study was approved by the institutional ethics committee (Reference no. IEC code-2019-108-IMP-109). All women who fulfilled the inclusion criteria were informed about the study and the consenting participants were enrolled.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Madan, S., Verma, M. & Dabadghao, P. 24-h Glucose profile of patients with gestational diabetes mellitus and comparison with pregnant women with normoglycemia. Int J Diabetes Dev Ctries 44 (Suppl 1), 27–32 (2024). https://doi.org/10.1007/s13410-024-01311-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-024-01311-x