Abstract
Aim
Current knowledge regarding the changes in cardiac autonomic nerve function during asymptomatic hypoglycemia in type 2 diabetes (T2D) is limited. This study aimed to investigate the association between the severity of nocturnal asymptomatic hypoglycemia and short-term heart rate variability (HRV) changes in patients with T2D.
Methods
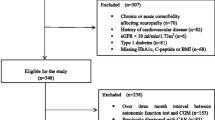
Comparison of changes was performed in a short-term time domain and frequency domain analysis of HRV during nocturnal asymptomatic hypoglycemia [interstitial glucose (IG) ≤ 3.5 mmol/L] and during euglycemia in T2D subjects treated with insulin (n = 58). Further stratification was performed according to the degree of hypoglycemia. All patients underwent 72 h of simultaneous Holter and continuous interstitial glucose monitoring (CGM).
Results
Fifty-two nocturnal asymptomatic hypoglycemia episodes were included in the spectral analysis of HRV in the participants. In the hypoglycemic (IG < 3 mmol/L) subjects, the short-term time domain parameters (standard deviation of normal R-R intervals (SDNN), RMSSD (the square root of the mean squared difference of successive RR intervals)) and normalized high-frequency (HF) were significantly lower than those during the matched euglycemic period (IG 5–10 mmol/L) (all p < 0.01), and the normalized low-frequency (LF)/HF ratio was increased (p < 0.05). In the hypoglycemic (≤ 3 IG ≤ 3.5 mmol/L) subjects, although HF was significantly lower than that in the euglycemic subjects (p < 0.01), no differences were observed in the SDNN, RMSSD, or the LF/HF ratio.
Conclusions
The spectral analysis of HRV showed that reduced HRV was associated with the severity of nocturnal asymptomatic hypoglycemia; severe hypoglycemia aggravates the cardiac autonomic nerve imbalance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many studies have confirmed that hypoglycemia in patients with diabetes during intensive glycemic therapy is associated with an increased risk of cardiovascular events and mortality. However, the mechanism is not completely clear [1]. Emerging evidence suggests that this relationship is likely multifactorial [2]. Some studies suggest that the increased risk of cardiovascular events and mortality is related to hypoglycemia leading to cardiac autonomic dysfunction [3] and is associated with the severity of hypoglycemia [4]. These studies mostly focused on type 1 diabetes, and knowledge regarding the changes in cardiac autonomic nerve function during hypoglycemia in type 2 diabetes mellitus (T2D) is limited. Decreased heart rate variability (HRV) is a sign of cardiac autonomic dysfunction. However, the impact of the severity of hypoglycemia on HRV is currently unknown. Continuous glucose monitoring (CGM) can detect hypoglycemia that is not easily detected by traditional monitoring methods, especially nocturnal asymptomatic hypoglycemia [5]. This study used retrospective CGM synchronization combined with Holter to observe changes in the short-term HRV parameters in asymptomatic hypoglycemia in patients with T2D treated with insulin and explore the effects of different degrees of hypoglycemia on cardiac autonomic function.
Methods
Patients
Fifty-eight patients (30 males, 28 females) with type 2 diabetes based on the WHO diagnosis and classification criteria aged between 20- and 75 -year Chinese from the Department of Endocrinology and Metabolism of Shaoxing People’s Hospital (Zhejiang Province, China) were enrolled between January 2018 and May 2020. The inclusion criteria included T2D patients treated with insulin with a history of repeated episodes of hypoglycemia and HbA1c < 8.0%. The exclusion criteria included the following: before inclusion, the ST segment depression > 0.1 mm; preexcitation syndrome; persistent atrial fibrillation, premature ventricular beats, atrioventricular block, and other obvious arrhythmias; use of antiarrhythmic drugs; digoxin affected repolarization of the ST segment; other drugs affected the HRV changes; acute myocardial infarction (AMI) and coronary artery bypass grafting (CABG) within the past 1 year; uncontrolled hypertension (systolic blood pressure > 160 mmHg or diastolic blood pressure > 90 mmHg) or angiotensin-converting enzyme inhibitors; and diabetic retinopathy, diabetic nephropathy, and diabetic peripheral neuropathy. Among the enrolled patients, 40 patients were treated with premixed insulin (18 with NovoMix 30, 12 with Humulin 70/30, and 10 with Novolin 30R), and the other 18 patients were treated with basal + dietary insulin (11 with Lantus, 5 with Levemir, and 2 with Novolin N; 12 patients received NovoRapid, and 6 patients received Novolin R before mealtime). Most drugs were used in combination with other oral drugs, including glycosidase inhibitors, metformin, or DDP IV inhibitors. After enrollment, the patients were asked to keep a diary detailing their mealtimes, insulin injections, and exercise.
Measurements
Clinical data collection
Each subject was asked for his or her medical history and medication history. After a 10-h overnight fast and rest for 20 min, the participants’ blood pressure, height, and weight were measured. The body mass index (BMI) was calculated as the weight (kg) divided by height squared (m2). Blood samples were collected before and 2 h after a fixed breakfast for the measurements of glycosylated hemoglobin A1c (HbA1c), fasting lipid profiles, liver and kidney function, myocardial enzyme spectrum, electrolytes, and fasting and 2 h postprandial plasma glucose (FPG and 2 hPG), and urinary measurements were performed to determine the urine microalbumin-creatinine ratio (ACR).
CGMS data collection
Continuous glucose monitoring (CGM) measures the glucose concentration in subcutaneous interstitial fluid and non-venous blood glucose, and CGM is currently a useful tool for discovering and assessing patients at high risk of hypoglycemia or hypoglycemia. CGM can be used in clinical research and is a valuable method [5, 6]. All subjects underwent 72-h continuous interstitial glucose (IG) monitoring (CGM) with the Medtronic Carelink ipro2, and each subject underwent at least 4 capillary blood glucose monitoring sessions per day during the CGM period for calibration. After 72 h, ipro2 was uploaded to the software by the same investigator, and a retrospective blood glucose analysis report was generated. An episode of low IG (≤ 3.5 mmol/L) on CGM without simultaneous self-reporting of symptoms was regarded as asymptomatic hypoglycemia. The period during which asymptomatic hypoglycemia occurs was selected to be more than 20 min [7]. Further stratification was performed according to the degree of hypoglycemia as follows: a level of IG < 3 mmol/L was considered clinically significant hypoglycemia [8, 9]), and 23:00–6:00 was defined as the night period.
Collecting ECG data during the hypoglycemia period
All patients underwent 72 h of simultaneous 12-lead Holter and CGM using a Holter electrocardiograph (CardioTrak Holter Analysis System, CT-08 Holter Recording Box) from the Hangzhou Baihui Medical Equipment Co., Ltd. To observe changes in the HRV when hypoglycemia occurs [10, 11], the ECG data of HRV during each period of asymptomatic hypoglycemia were collected in Holter data. Various ectopic heart rhythms and artifacts were automatically eliminated, and the average heart rate was recorded. The spectral analysis included the short-term frequency domain and the time domain. In the short-term analysis, the total power under different conditions, namely, the high-frequency power (HF, 0.15 ~ 0.4 Hz, ms2) and low-frequency power (LF, 0.04 ~ 0.15 Hz, ms2) values, differed. Therefore, the HF and LF were normalized (HFnu and LFnu) and then compared. The normalized low-frequency to high-frequency ratio was calculated (LF/HF). The SDNN (standard deviation of normal R-R intervals), SDANN (standard deviation of the R-R interval averages per 5-min segment), RMSSD (the square root of the mean squared difference of successive RR intervals), and PNN50 (the percentage of adjacent R-R intervals > 50 ms in the total number of R-R intervals) were used as time-domain measures of HRV. As a control, each episode of asymptomatic hypoglycemia was matched with a euglycemic period (IG 5–10 mmol/L) of an equal duration at the same time of day on a different day.
Treatment of symptomatic hypoglycemia
Treatment was performed according to the 2017 China Type 2 Diabetes Prevention and Control Guidelines [12].
Statistical analysis
The normally distributed continuous variables are presented as the means ± standard deviations. The short-term frequency domain or time domain data were analyzed using a paired t-test by comparing the hypoglycemia period with the euglycemia period. Their correlation was analyzed by a Pearson correlation analysis. Using the occurrence of clinically significant hypoglycemia as the dependent variable and HRV parameters as the independent variable, a logistic binary regression analysis was performed to identify the predictive risk factors for clinically significant hypoglycemia. All statistical analyses were performed with SPSS 20.0 (IBM, Armonk, NY, USA). Significance was defined as a p-value < 0.05.
Results
Anthropometric and laboratory characteristics of the subjects
The average parameters of the 58 participants were as follows: age (62.2 ± 11.2) years, BMI (21.7 ± 1.7) kg/m2, HbA1c (7.5 ± 0.8)%, duration of diabetes (12.1 ± 6.0) years, FPG (6.7 ± 1.9) mmol/L, fasting C peptide (201 ± 167) pmol/L, total cholesterol (4.3 ± 0.8) mmol/L, low-density lipoprotein cholesterol (2.4 ± 0.6) mmol/L, triglyceride (0.8 ± 0.7) mmol/L, high-density lipoprotein cholesterol (1.5 ± 0.4) mmol/L, urine albumin-creatinine ratio (ACR, 26.8 ± 13.4) mg/cr, blood creatinine (78.2 ± 10.5) µmol/L, systolic blood pressure (126 ± 12) mmHg, and diastolic blood pressure (73 ± 6) mmHg.
CGMS data
Forty-eight of the 58 participants experienced at least one episode of hypoglycemia. Excluding the period of symptomatic hypoglycemia, there were 62 asymptomatic hypoglycemia episodes. Among these episodes, 52 segments of asymptomatic hypoglycemia at night were available for analysis. At the onset of hypoglycemia, the average IG level was 3.0 ± 0.5 mmol/L, the lowest IG value was 1.9 mmol/L, the average duration was 77.2 ± 37.4 min, and the longest duration was 200 min.
HRV analysis of nocturnal asymptomatic hypoglycemia
The HFnu, SDNN, SDANN, RMSSD, and PNN50 during the nocturnal asymptomatic hypoglycemia episodes were significantly lower than those during the matched euglycemic period, and the LF/HF ratio was increased; the difference was statistically significant (all p < 0.01). The LFnu exhibited a downward trend, but the difference was not statistically significant (p > 0.05) (Table 1). According to further stratified analysis of the degree of hypoglycemia, there were 22 episodes of clinically significant hypoglycemia (IG < 3 mmol/L). The HFnu, SDNN, SDANN, RMSSD, and PNN50 were significantly lower than those during the euglycemic period (all p < 0.01), and the LF/HF ratio was increased (p < 0.05) (Table 2). In hypoglycemia (≤ 3 IG ≤ 3.5 mmol/L), except for the HFnu, which was significantly lower than that in euglycemia (p < 0.01), the SDNN, SDANN, RMSSD, PNN50, and LF/HF ratios did not significantly differ (p > 0.05) (Table 3).
Pearson correlation analysis of hypoglycemia degree and HRV parameters
Pearson correlation analysis showed that the degree of hypoglycemia was negatively correlated with the LF/HF ratio (r = − 0.348, p = 0.011) and positively correlated with the SDNN and RMSSD (r = 0.391 and 0.397, respectively, both p = 0.004) but was not correlated with the HFnu and LFnu (p > 0.05).
Logistic binary regression analysis of predictors of clinically significant hypoglycemia
With the occurrence of clinically significant hypoglycemia as the dependent variable and the LFnu, HFnu, SDNN, SDANN, RMSSD, PNN50, and LF/HF as the independent variables, a logistic binary regression analysis was performed. The results showed that LF/HF was a predictor of clinically significant hypoglycemia [Exp(B) = 6.428, p = 0.032] (Table 4).
Discussion
Population-based studies have confirmed that the incidence of hypoglycemia in T2D during intensive insulin therapy is significantly increased, and there are more cardiovascular events and a higher mortality [13]. Some studies have suggested that this finding may be related to an imbalance in sympathetic-parasympathetic tension in the cardiac autonomic nerve [14]. Different methods are used to evaluate cardiac autonomic neuropathy (CAN). The standard cardiovascular reflex test proposed by Ewing [15] is usually considered the gold standard. However, it has been reported that impairment indicators in HRV spectrum analyses can appear before abnormal cardiac autonomic nerve function tests [16]. In clinical practice, high HRV reflects an individual’s ability to adapt to changes in the microenvironment, and a decline in HRV has become an auxiliary marker of susceptibility to cardiovascular events in the process of intensive blood glucose control [17]. The cardiac autonomic nerve includes the sympathetic and vagus nerves, which complement and antagonize each other and together finely regulate the physiological functions of the heart. HRV analysis methods include the time domain and frequency domain. It is generally believed that HF can better reflect vagus nerve activity, while LF comprehensively reflects sympathetic and parasympathetic nerve activity. The LF/HF ratio can represent the balance of sympathetic and parasympathetic nerves. The time domain parameter SDNN is jointly regulated by sympathetic and parasympathetic pathways. RMSSD and PNN50 often reflect the activity of the parasympathetic nerve. In this study, we selected the period of asymptomatic hypoglycemia in T2D patients at night and analyzed the changes in the frequency domain and time domain parameters of short-duration HRV to explore the influence of different degrees of hypoglycemia on cardiac autonomic function.
This study found that asymptomatic episodes of hypoglycemia were more frequent when patients slept at night, with an average duration of 77.2 min, longest duration of 200 min, and an average IG of 2.98 mmol/L. Further stratification was performed according to the degree of hypoglycemia and clinically significant hypoglycemia (IG < 3 mmol/L). HRV was clearly abnormal during asymptomatic hypoglycemia, which directly affected CAN, and the HFnu, RMSSD, and PNN50 were significantly decreased compared with those during euglycemia, suggesting that the activity of the parasympathetic nerve was significantly weakened. The SDNN and SDANN were significantly decreased, and the LFnu, which mainly represents sympathetic nerve activity, also showed a downward trend. The heart rate did not significantly increase but showed a slowdown trend, indicating that both sympathetic and parasympathetic nerve function were damaged, and the damage to the parasympathetic nerve was more serious than the sympathetic nerve pathway. We found that the response of increased LF/HF ratio was a reflection of an imbalance of sympathetic and parasympathetic activity when hypoglycemia occurred. It was suggested that the imbalance of cardiac autonomic nerve activity was the result of hypoglycemia [18].Studies had found that the baroreflex sensitivity of the cardiac vagus nerve was inhibited significantly during hypoglycemia, indicating reduced vagal control and impaired cardiovascular homeostasis during hypoglycemia[19].The weakened antagonism of the parasympathetic nerve to the sympathetic nerve may increase the electrical instability of the heart and lead to the risk of arrhythmia, which can be explained by the greater damage to the parasympathetic nervous system. These patients have a central nervous system-mediated deficiency in the sympathetic response to hypoglycemia and lack a glucagon response to hypoglycemia after insulin treatment without obvious autonomic nervous warning symptoms of hypoglycemia; this condition is not easy to detect, diagnose, or treat in a timely manner. These changes in electrocardiograms may have fatal consequences, such as sudden death, for diabetic patients who already have cardiovascular disease. In the case of nonsevere hypoglycemia (≤ 3 IG ≤ 3.5 mmol/L), the HFnu was significantly decreased compared with that during euglycemia, but there was no statistically significant difference in the SDNN, SDANN, RMSSD, PNN50, or LF/HF ratio. This finding suggests that HRV changes are more significant only when clinically significant or severe hypoglycemia is present. HF was significantly decreased in the patients with nonclinically significant hypoglycemia but did not decrease further with lower blood glucose. This finding may be related to sympathetic nerve excitation after transient vagus nerve suppression, followed by an increase in compensatory activity of the vagus nerve.
In the Pearson correlation analysis of the parameters of hypoglycemia and HRV, the degree of blood glucose was positively correlated with the SDNN and RMSSD and negatively correlated with the LF/HF ratio. These results suggest that both sympathetic and parasympathetic fiber activities are significantly impaired in patients with asymptomatic hypoglycemia episodes, which may lead to the occurrence of cardiovascular adverse events caused by cardiac electrical instability. HRV parameters are related to the severity of hypoglycemia [20]. Similarly, CAN disorder can predict severe hypoglycemia in patients with T2D [21]. The logistic binary regression analysis showed that LF/HF was a predictor of clinically significant hypoglycemia, suggesting that the imbalance of the sympathetic and parasympathetic nerves is the main risk factor for hypoglycemia.
Some related studies, such as Chow et al. [7], observed changes in arrhythmia and HRV in T2D patients with cardiovascular disease during hypoglycemia. Unfortunately, the study failed to find changes in parameters that could reflect sympathetic-parasympathetic activity at night, and the changes in the SDNN, HF, and LF did not reach statistical significance. However, in individuals with severe asymptomatic hypoglycemia, HF was found to change (first decrease and then increase) with the continuous decrease in blood glucose, which is consistent with the trend of HF in our study. Considering that there are defects in sympathetic and parasympathetic regulation during nocturnal hypoglycemia, the excessive activation of the vagus nerve is associated with the occurrence of sinus bradycardia and even long gap and fatal arrhythmias [22].
Klimontov et al. [23] found a correlation between blood glucose fluctuation and HRV in female T2D patients treated with insulin. There were no significant changes in the LF, HF, or LF/HF during nocturnal hypoglycemia compared with those during euglycemia. This finding is inconsistent with the results observed in this study and may be related to the small sample size (only 7 data segments were included in the analysis) or the different degrees of hypoglycemia [24]. An expanded sample size and more clinical studies are required to explore this further.
There are some shortcomings in this study. First, there were differences in LF and HF between day and night in the normal subjects. However, this paper did not compare HRV at night and day because fewer data were available for analysis of hypoglycemia during the day. In addition, there were differences between hypoglycemic autonomic dysfunction and cardiac autonomic dysfunction. We cannot completely rule out hypoglycemic autonomic dysfunction in the enrolled subjects.
In conclusion, when insulin-treated hypoglycemia occurs in T2D, it manifests as an imbalance between the sympathetic and parasympathetic nervous systems, is associated with the severity of hypoglycemia, and is harmful in terms of the electrical stability of the heart, which is associated with a poor prognosis of cardiac function.
More studies investigating asymptomatic hypoglycemia are needed to determine the effect of hypoglycemia on the regulation of cardiac autonomic function.
Conclusion
In this study, we investigated the association between the severity of nocturnal asymptomatic hypoglycemia and short-term HRV changes in patients with T2D and reported that reduced HRV was associated with the severity of nocturnal asymptomatic hypoglycemia, severe hypoglycemia aggravates the CAN imbalance, and the imbalance between sympathetic and parasympathetic nerves is the main risk factor for severe hypoglycemia.
References
ACCORD Study Group, Gerstein HC, Miller ME, Genuth S, et al. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med. 2011;364(9):818–28.
International Hypoglycaemia Study Group. Hypoglycaemia, cardiovascular disease, and mortality in diabetes: epidemiology, pathogenesis, and management. Lancet Diabetes Endocrinol. 2019;7(5):385–96.
Reno CM, Daphna-Iken D, Chen YS, VanderWeele J, Jethi K, Fisher SJ. Severe hypoglycemia-induced lethal cardiac arrhythmias are mediated by sympathoadrenal activation. Diabetes. 2013;62(10):3570–81.
Davis SN, Duckworth W, Emanuele N, Hayward RA, Wiitala WL, Thottapurathu L, et al. Effects of severe hypoglycemia on cardiovascular outcomes and death in the veterans affairs diabetes trial. Diabetes Care. 2019;42(1):157–63.
Schnell O, Barnard K, Bergenstal R, Bosi E, Garg S, Guerci B, et al. Role of continuous glucose monitoring in clinical trials: recommendations on reporting. Diabetes Technol Ther. 2017;19(7):391–9.
Diabetes Society of Chinese Medical Association. Guidelines for clinical application of continuous glucose monitoring in China (2017 Edition). Chin J Diabetes. 2017;9(11):667–75.
Chow E, Bernjak A, Williams S, Fawdry RA, Hibbert S, Freeman J, et al. Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk. Diabetes. 2014;63(5):1738–47.
Heller SR, Buse JB, Ratner R, Seaquist E, Bardtrum L, Hansen CT, et al. Redefining hypoglycemia in clinical trials: validation of definitions recently adopted by the American Diabetes Association/European Association for the Study of Diabetes. Diabetes Care. 2020;43(2):398–404.
Home P. How valid are the new hypoglycemia definitions for use in clinical trials? Diabetes Care. 2020;43(2):272–4.
Sun RL, Wu N, Yang SH. Recommendation of clinical application of heart rate variability detection. Chin J Cardiol. 1998;26(4):252–5.
Vest AN, Da Poian G, Li Q, Liu C, Nemati S, Shah AJ, et al. An open source benchmarked toolbox for cardiovascular waveform and interval analysis. Physiol Meas. 2018;39(10):105004.
Chinese Diabetes Society. Guidelines for the prevention and treatment of type 2 diabetes in China (2017 edition). Chin J Diabetes. 2018;10(1):4–67.
Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–39.
Infusino F, Pitocco D, Zaccardi F, Scalone G, Coviello I, Nerla R, et al. Low glucose blood levels are associated with abnormal cardiac sympatho-vagal balance in type 2 diabetic patients with coronary artery disease. Eur Rev Med Pharmacol Sci. 2010;14(3):203–7.
Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285–93.
Bernardi L, Spallone V, Stevens M, Hilsted J, Frontoni S, Pop-Busui R, et al. Methods of Investigation methods for cardiac autonomic function in human research studies. Diabetes Metab Res Rev. 2011;27(7):654–64.
Pop-Busui R, Evans GW, Gerstein HC, Fonseca V, Fleg JL, Hoogwerf BJ, et al. Effects of cardiac autonomic dysfunction on mortality risk in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care. 2010;33(7):1578–84.
Koeneman M, Olde Bekkink M, Meijel LV, et al. Effect of hypoglycemia on heart rate variability in people with type 1 diabetes and impaired awareness of hypoglycemia. J Diabetes Sci Technol. 2021;15:19322968211007484.
Rao AD, Bonyhay I, Dankwa J, et al. Baroreflex sensitivity impairment during hypoglycemia: implications for cardiovascular control. Diabetes. 2016;65(1):209–15.
Benichou T, Pereira B, Mermillod M, Tauveron I, Pfabigan D, Maqdasy S, et al. Heart rate variability in type 2 diabetes mellitus: a systematic review and meta-analysis. PLoS ONE. 2018;13(4):e0195166.
Yun JS, Kim JH, Song KH, Ahn YB, Yoon KH, Yoo KD, et al. Cardiovascular autonomic dysfunction predicts severe hypoglycemia in patients with type 2 diabetes: a 10-year follow-up study. Diabetes Care. 2014;37(1):235–41.
Nordin C. The proarrhythmic effect of hypoglycemia: evidence for increased risk from ischemia and bradycardia. Acta Diabetol. 2014;51(1):5–14.
Klimontov VV, Myakina NE, Tyan NV. Heart rate variability is associated with interstitial glucose fluctuations in type 2 diabetic women treated with insulin. Springerplus. 2016;15(5):337–46.
Silva TP, Rolim LC, SallumFilho C, Zimmermann LM, Malerbi F, Dib SA. Association between severity of hypoglycemia and loss of heart rate variability in patients with type 1 diabetes mellitus. Diabetes Metab Res Rev. 2017;33(2):e2830.
Acknowledgments
The authors appreciate the patients and study investigators who participated in this study.
Funding
This research was supported by the Medical and Health Science and Technology Program of Zhejiang Province, China (2020KY324), and the Shaoxing Bureau of Science and Technology, Zhejiang Province, China (2016CX006).
Author information
Authors and Affiliations
Contributions
All authors reviewed and approved the final version of the manuscript. YQY elaborated the study design, collected the data for the study, and wrote the manuscript. ZGFY collected the data and performed statistical analysis. XB collected the data for the study and critically revised the manuscript.
Corresponding author
Ethics declarations
The study received local ethics approval, and all subjects provided written informed consent before participation.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
You, QY., Xu, B. & Zuge, FY. Association between the severity of nocturnal asymptomatic hypoglycemia and heart rate variability change in patients with type 2 diabetes. Int J Diabetes Dev Ctries 43, 719–724 (2023). https://doi.org/10.1007/s13410-022-01151-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-022-01151-7