Abstract
Introduction
Type 2 diabetes mellitus (T2DM) is associated with long-term complications in different organs, and this is attributable to macrovascular and microvascular changes as reported by Fowler. Pulmonary complications, however, have been poorly characterised.
Materials and methods
The present study was a case–control study done at SRN Hospital, Prayagraj to correlate the pulmonary functions with glycemic status and insulin resistance in 100 patients with diabetes (cases) and compare these parameters in patients without diabetes (controls). Baseline values of fasting plasma glucose (FPG), prandial plasma glucose (PPG) and glycated hemoglobin (A1C) were significantly increased in cases as compared with controls.
Results
Forced expiratory volume (FEV1) (78.71% compared with 88.15%) and forced vital capacity (FVC) (67.48% compared with 96.58%) were both decreased in cases compared with controls but as decline in FVC was more compared with FEV1; their ratio, FEV1/FVC (121.70 as compared to 90.19), was increased in cases. FVC decreased with increase in A1C values (96.2%, 84.2%, 71.2% for A1C values 5.7%, 5.7–6.4% and > 6.4% respectively). FVC was also decreased for greater values of Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) (98.2% for HOMA-IR < 2.5 and 74.6% for HOMA-IR > 2.5). The ratio of FEV1/FVC was more with higher values of A1C (103.3 for A1C > 2.5 and 91.1 for A1C < 2.5). FVC also decreased with increasing values of FPG (97.4%, 91.1% and 71.2% for FPG values of < 100 mg%, 100–125 mg% and ≥ 126 mg%).
Conclusion
A total of 65% of patients had abnormal pulmonary function tests with predominance of restrictive pattern. This restrictive decline is significantly associated with increasing dysglycemia and insulin resistance. However, it is unrelated to levels of low-density lipoprotein (LDL) and duration of T2DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reduced pulmonary functions have been seen in patients with diabetes [2]. Pulmonary diseases are broadly classified as obstructive and restrictive based on the pulmonary function tests (PFTs). Diabetes causes pulmonary complications by microangiopathy of the alveolar capillary network. Impairment in lung function of patients with diabetes is believed to be the consequences of biochemical alterations in the connective tissue constituents of the lung, particularly collagen and elastin, as well as microangiopathy due to the nonenzymatic glycosylation of proteins induced by chronic hyperglycemia [3]. The functional abnormalities ensuing from these changes manifest clinically by way of a reduction in elastic recoil of the lung, lung volumes and pulmonary capacity for the diffusion of carbon monoxide. There is a predominant reduction in spirometric parameters of the diabetic patients towards the restrictive pattern [4]. PFTs in type 2 diabetes mellitus (T2DM) have demonstrated varied and frequently conflicting results. Despite the unclear nature, the relationship between the diabetes and the lung function remains important because of potential epidemiological and clinical implications. The present study is an effort to correlate the pulmonary functions with glycemic status and insulin resistance in patients with diabetes and compare these parameters in patients without diabetes, so that appropriate interventions could be taken up to improve the quality of life in these patients.
Materials and methods
This study was a case–control study conducted in Moti Lal Nehru Medical College Allahabad and its associated Swaroop Rani Nehru Hospital from May 2017 to August 2018. The study included 100 patients > 18 years of age, diagnosed with T2DM, attending the outpatient department of the hospital. One hundred age- and sex-matched subjects were taken as controls. Patients with acute and chronic pulmonary diseases, history of smoking for any duration, gross abnormalities of vertebral column or thoracic cage, neuromuscular diseases, those who had undergone major chest or abdominal surgeries, with ischemic heart disease and cardiomyopathies, chronic liver disease and chronic renal failure were excluded from the study. Patients underwent a morning fasting plasma glucose estimation and fasting insulin estimation after 8 h of fasting at least. Serum liver function tests (LFTs) and kidney function tests (KFTs) were also performed for all the patients. Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) was performed on all patients. At present, computer software is available for calculation of HOMA-IR, the value of which > 2.5 was considered as insulin resistance.
All patients underwent a series of pulmonary function tests to assess forced expiratory volume (FEV1) and forced vital capacity (FVC), and the ratio of both was calculated. It was done by using a RMS Helios 401 spirometer after explaining the procedure properly to the patient. Patients who could not exhale properly for a minimum period of 6 s were also excluded. Fasting lipid profile and A1C were performed for all the patients. In order to assess the glycemic status, cutoff values for FPG were < 100 mg/dl for normal glucose tolerance, 100–125 mg/dl for impaired fasting glucose (IFG), and ≥ 126 mg/dl for T2DM. For A1C, values < 5.7% for normal glucose tolerance, 5.7–6.4% for impaired glucose tolerance (IGT) and ≥ 6.5% for T2DM were considered.
Baseline characteristics were compared between both the groups. Patients were sub-classified into different groups on the basis of values of A1C, FPG, HOMA-IR, LDL and duration of diabetes. FEV1 and FVC were calculated, and FVC and ratio of FEV1 to FVC were compared in relevant groups.
Spirometer model, RMS 701 with Helios software (Recorders and Medicare Systems, Chandigarh) was used for PFTs. Blood glucose was determined by glucose oxidase method, and A1C level was assessed by using glycohemoglobin HbA1 test kit (fast ion exchange resin separation method). Statistical analysis was performed using Statistical Package for Social Science software (SSPS version 20.1). The numerical data was compared using two tailed Student’s t test. The level of significance was considered p < 0.05. Prior to the test, all the subjects (control and patients) underwent a detailed history taking, general physical examination and systemic examinations.
Results
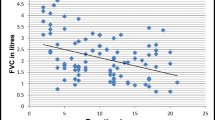
A total of 100 cases and 100 age- and sex-matched controls were analysed. Results showed that 65% patients had abnormal PFTs as shown in Fig. 1. There was a significant reduction in FEV1 (78.71 ± 1.51 in cases compared with 88.15 ± 6.19 in cases) and FVC (67.48 ± 14.06 in cases compared with 96.58 ± 2.58 in controls). The reduction in FVC was more compared with FEV1 and as a result, the FEV1/FVC ratio (121.70 in cases compared with 90.19 in controls) was increased significantly suggesting restrictive pathology as shown in (Table 1) and Fig. 2.
For three subgroups based on FPG values (< 100 mg%, 100–125 mg% and ≥ 126 mg%), the values of mean FVC declined progressively (97.4%, 91.1%, 71.2%), respectively for each group. The difference was statistically significant for groups representing patients with and without diabetes. For the subgroups based on A1C values (< 5.7%, 5.7–6.4%, > 6.4%), the values of mean FVC declined with increasing A1C values (96.2%, 84.2%, 72.1%). With the division of the population in two groups, insulin sensitive and insulin resistance, based on HOMA-IR values (< 2.5 and > 2.5), mean FVC declined in the insulin resistant group compared with insulin sensitive group (98.2% compared with 74.6%). When the population was divided on the basis of LDL values into two groups (LDL > 130 mg% and LDL < 130 mg%), the mean FVC declined in the group with higher LDL values (96.2% compared with 92.7%). Duration of diabetes formed the basis of division of population in two groups (duration < 10 years and > 10 years). Mean FVC declined in the group with longer duration of diabetes (71.2% compared with 68.6%). This reduction in mean FVC values was statistically significant in all groups except those for LDL levels and duration of diabetes as shown in Tables 2 and 3 and Fig. 3.
Discussion
In this study, 52% patients with diabetes were found to have restrictive pattern on pulmonary function testing using spirometry. This was consistent with the findings of Meo et al. [5] who found that there was a combined obstructive and restrictive pattern of pulmonary function in patients with diabetes but it was predominately restrictive. The possible explanation for this includes the involvement of the neuromuscular respiratory muscles due to diabetic neuropathy of the thoracic nerves that contributes to the respiratory dysfunction. This hypothesis is strengthened by the fact that postmortem examination has revealed thickened alveolar epithelial and pulmonary capillary basal lamina in patients with diabetes which explains the deteriorated pulmonary gas exchange leading to restrictive pattern. It was also seen in the study that A1C is negatively correlated with FVC. These findings were consistent with those in the study done by Davis et al. [6]. This can be understood by the fact that A1C serves as an indicator of glycemic control over a period which can significantly correlate with the deterioration of pulmonary function in that given period of time. However, in another study done by Shah et al. [7], no significant correlation could be established between A1C and PFTs.
FVC was shown to be negatively correlated with HOMA-IR values. Similar findings were observed in studies by Lee et al. [8], Lawlor et al. [9] and Lazarus et al. [10]. This study was also able to demonstrate a significant negative correlation between FPG and lung function in the study group. Timothy [11] et al. also found similar results in their studies that higher levels of FPG were associated with lower pulmonary function. The study could not find any significant correlation between FVC and LDL values. The study also tried to correlate the effect of the duration of T2DM on the forced residual capacity. No significant correlation could be found between them. However, in the study done by Kanyakumari et al. [12], they concluded that a significant correlation exists between the duration of T2DM and reduction in FVC. In a study by Davis et al. [6], the decrease in FEV1 was at an annual rate of 71 ml/year. Possible explanation can be a thickening of alveolar epithelium and pulmonary capillary basal lamina leading to pulmonary microangiopathy, reduced pulmonary elastic recoil due to nonenzymatic glycosylation of connective tissue reducing the FEV1. The major limitation was a relatively small sample size due to time-bound nature of the study. Pulmonary functions other than FEV1 and FVC were not taken into consideration. DLCO, which is a strong predictor of restrictive pattern of pulmonary disease, was not measured, due to nonavailability of facility.
Conclusion
Majority of patients (65%) had abnormal PFTs (restrictive, obstructive and mixed pattern). Restrictive pattern was predominant (52%) in patients with diabetes. Restrictive decline in pulmonary function was significantly correlated with increasing dysglycemia and insulin resistance. There was a decline in pulmonary functions with increasing duration of diabetes and extent of dyslipidemia; however, it was not significant. More studies with a higher number of patients and greater number of spirometry criteria under evaluation will be required to establish a clear cut relationship between glycemic status, insulin resistance and pulmonary function tests.
References
Fowler MJ. Microvascular and macrovascular complications of diabetes. Clinical Diabetes. 2008;26(2):77–82.
Yadav A, Saxena AK, Gaur K, Punjabi P, Meena G. Study of pulmonary function test in type 2 diabetes mellitus. IOSR-JDMS.2013;10(2) :74–7.
Irfan M, Jabbar A, Haque AS, Awan S, Hussain SF. Pulmonary functions in patients with diabetes mellitus. Lung India. 2011;28(2):89–92.
Agarwal AS, Fuladi AB, Mishra G, Tayade BO. Spirometry and diffusion studies in patients with type 2 diabetes mellitus and their association with microvascular complications. Indian J Chest Dis Allied Sci. 2010;52:213–6.
Meo A, et al. Effect of duration of disease on ventilator function in an ethnic Saudi group of diabetic patients. J Diabetes Sci Technol. 2007 Sep;1(5):711–7.
Davis, W., Knuiman, M., Kendall, P.,Grange, V., & Davis, T. (2004). Glycemic exposure is associated with reduced pulmonary function in type 2 diabetes: the Fremantle Diabetes Study. Diabetes care.2004; 27(3): 752-7.
Shah S, Sonawane P, Nahar P, Vaidya S et al. PFTs in type 2 diabetes mellitus and their association with glycemic control and duration of the disease. Lung India2013;30(2):108–112.
Lee et al. Association between HOMA-IR and lung function in Korean young adults based on the Korea National Health and Nutrition Examination Survey. Sci Rep.2017;7:117–26.
Lawlor DA, Ebrahim S, Smith GD. Associations of measures of lung function with insulin resistance and type 2 diabetes : findings from the British Women's Heart and Health Study. Diabetologia 2004;(47):195–203.
Lazarus R, Sparrow D, Weiss ST. Impaired ventilator function and elevated insulin levels in non diabetic males: the normative ageing study. Eur Respir J. 1998;12:635–40.
Timothy ME, Knuimann M, Kendall P. Reduced pulmonary function and its association in type 2 diabetes. Diabetes Res Clin Pract. 2000;50:152–9.
Kanyakumari DH, Nataraj SM, Devaraj HS. Correlation of duration of diabetes and pulmonary function tests in type 2 diabetes mellitus patients. Int J Biol Med Res. 2011;2(4):1168–70.
Acknowledgments
The authors convey their gratitude to Research Society for Studies of Diabetes in India (RSSDI) for funding the project and to the technical staff of hospital laboratory.
Funding
The study was funded by Research Society for Studies of Diabetes in India (RSSDI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
An informed consent was obtained from all included subjects after explaining them the nature and purpose of the study. All procedures performed in the study were in accordance with the ethical committee of the institution, and a prior consent for the same was obtained.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bajaj, S., Anil, S. & Prajapati, R. Pulmonary function tests in type 2 diabetes mellitus and their association with glycemic status and insulin resistance. Int J Diabetes Dev Ctries 40, 406–409 (2020). https://doi.org/10.1007/s13410-020-00795-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-020-00795-7