Abstract
To verify brain and spinal changes using magnetic resonance imaging in patients with HTLV-1–associated myelopathy/tropical spastic paraparesis. This was a systematic review. The descriptors used were tropical spastic paraparesis and magnetic resonance image. The keyword HTLV-1–associated myelopathy was also used. Twenty-three articles were included: 16 detected brain changes and 18 detected spinal changes. White matter lesions were the most frequent finding in the brain. Brain injuries were most frequently identified in the periventricular region, in the subcortical region, in the centrum semiovale, in the brain stem, and corpus callosum. Atrophy was the most frequent finding of the spinal cord, affecting the thoracic and cervical regions, and was associated with a longer evolution of myelopathy. White matter lesions in these regions were also observed. Cortical white matter lesions and thoracic spinal cord atrophy were the most frequently reported changes in patients with HTLV-1–associated myelopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human T-cell Lymphotropic virus type 1 (HTLV-1) infects approximately 20 million people worldwide. Brazil concentrates 12% of these individuals (Carneiro-Proietti et al. 2002, 2006; Marano et al. 2016). Although approximately 95% of patients remain asymptomatic, HTLV-1 infection may be associated with neurological manifestations such as HTLV-1–associated myelopathy/tropical spastic paraparesis (HAM/TSP) (Gessain et al. 1985; Osame et al. 1986) in 0.5 to 4% (Nicolás et al. 2015; Nozuma et al. 2016), cognitive changes (Silva et al. 2003; Raulino Goncalves et al. 2017), isolated neurogenic bladder dysfunction, peripheral neuropathy, and amyotrophic lateral sclerosis (Silva et al. 2007).
The pathophysiology of HAM/TSP involves the migration of infected T-lymphocytes through the blood–brain barrier (BBB), favoring chronic inflammation in the central nervous system (CNS) and demyelination (Yamano and Sato 2012). The damage mediated by the immune response occurs preferentially in the lower thoracic and lumbar regions of the spinal cord, which explains the occurrence of hyperreflexia, muscle weakness and spasticity in the lower limbs (Martin et al. 2014), sexual dysfunction, and neurogenic bladder disorders (Proietti et al. 2005).
Different criteria have been used for the diagnosis of HAM/TSP in various studies on this topic. The World Health Organization (WHO) criteria for diagnosing patients with HAM/TSP are based on the following clinical characteristics: slowly progressive spastic paraparesis associated with sphincter disorders such as neurogenic bladder disorders, sensory symptoms such as neuropathic pain and low back pain, changes in the proprioception, and laboratory alterations such as the presence of HTLV-1 antigens or antibodies in the blood or cerebrospinal fluid (CSF). Osame (1986) proposed another diagnostic model that classifies patients as definitive HAM, those patients with slowly progressive paraparesis with symmetrical involvement of the pyramidal tracts and HTLV-1 antibodies in the blood and CSF, and probable HAM, those who present paraparesis along with HTLV-1 antibodies in the blood or CSF (but not both), or non-compressive myelopathy not consistent with the previous group and antibodies to HTLV-1 in both (serum and CSF). For De Castro-Costa (2006), there are three classifications: patients with definitive HAM have non-remitting paraparesis with impaired gait, presence of antibodies (blood and CSF), and urinary and sensory symptoms may or may not be present; patients with probable HAM have a monosymptomatic clinical presentation (spasticity or hyperreflexia or Babinski’s sign in the lower limbs); and patients with possible HAM are those with complete or incomplete clinical presentation.
Patients infected with HTLV-1 may also have brain damage (Bagnato et al. 2005; Mendes et al. 2014). However, it is still unclear to what extent abnormalities in the spinal cord or brain found through neuroimaging tests can be considered as markers of disease duration and severity in patients with HAM/TSP (Griffith et al. 2006). Magnetic resonance imaging (MRI) is a highly sensitive tool for verifying the integrity of CNS structures, with reduced risks for patients (Hemond and Bakshi 2018). In this context, the finding of lesions in the CNS of patients with HAM/TSP can facilitate the understanding of the clinical picture and direct the choice of the best alternatives for monitoring these individuals.
The aim of this study is to verify changes in brain and spinal magnetic resonance imaging in patients with HAM/TSP.
Methods
Searches were carried out in the Pubmed, Scopus, Science Direct, and Web of Science databases. No time or language limitations were applied to the articles. The descriptors used were “Tropical Spastic Paraparesis” and “Magnetic Resonance Imaging”, and the keyword “HTLV I Associated Myelopathy”. The following combination was used in the search: tropical spastic paraparesis or HTLV I–associated myelopathy and magnetic resonance imaging. The articles from other sources were identified through the reverse search (in the references of the articles that passed to the eligibility phase). The search identified 477 articles in the databases and 7 articles from other sources, totaling 484 articles.
Inclusion criteria were studies whose population studied included patients with tropical spastic paraparesis and carriers of human T-cell lymphotropic virus type 1 (HTLV-1), adult individuals (over 18 years), and studies that used magnetic resonance to detect abnormalities in the brain and/or spinal cord.
The exclusion criteria were studies with individuals co-infected with human T-cell lymphotropic virus type 2 (HTLV-2), leukemia or T-cell lymphoma, Sjögren’s syndrome, and other causes of spastic paraparesis; articles including animals; studies of review; and articles that investigated only genetic and immunological factors; there is no information in the text about the equipment and resonance images as the type of examination, the magnetic field used, and the sequence and weighting.
The research and data extraction were performed by two evaluators. After reading the titles and abstract, a meeting was held between the evaluators to align the choice of articles that would pass to the stage of complete reading of the article. In case of disagreement, a third evaluator was called. The calibration between the evaluators was done through the simple agreement index, performed after the selection of articles in the databases (where 95% agreement was reached). The protocol for this systematic review was registered with PROSPERO, under number CRD 42,018,098,917. The search for articles was carried out in August of 2021.
Data extraction was composed of the study information (authors and year of publication), patient characteristics (number of patients, mean age, gender, time of illness or infection, distribution of groups), anatomical regions evaluated, characteristics related to magnetic resonance imaging (type, field, sequence, weighting), use of contrast, measures of functionality, criteria for diagnosing HAM/TSP, way of classifying injuries, brain findings and spinal cord findings, and differences between groups (HAM/TSP patients, HTLV-1 carriers without HAM/TSP, and controls).
The quality analysis of the articles was performed using the validated Portuguese version of the PEDro scale (Shiwa et al. 2011).
Results
Initially, 484 articles were identified in the databases: Pubmed (40), Scopus (158), Science Direct (225), and Web of science (54), and 7 articles obtained by reverse search. Then, a total of 67 duplicates were removed. The 417 articles that remained had their titles and abstracts analyzed in relation to the inclusion and exclusion criteria. It was observed that there were a large number of articles that involved genetic factors and related to the immune system in all databases. After analyzing the titles and abstract, 29 articles remained, which were submitted to complete reading.
After reading the articles in full, 23 articles were included in the systematic review. Figure 1 follows the model of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al. 2009) and details the process of selecting articles and the reasons for exclusions.
Table 1 shows the analysis of the articles included in the systematic review according to the PEDro scale. It is observed that 17 of 23 articles defined the eligibility criteria for patients with HAM/TSP; however, the criteria used to classify patients as having this myelopathy varied between studies. In addition, 9 of 23 studies identified the professionals responsible for interpreting MRI and 6 of 23 studies did not define a standard to guide the investigation of injuries.
Supplementary Table 1 shows the characteristics of the studies included in the review. Thirteen of 23 studies (56.5%) used comparison groups (Kira et al. 1988, 1991; Rudge et al. 1991; Fukushima et al. 1994; Howard et al. 2003; Griffith et al. 2006; Morgan et al. 2007; Kuriyama et al. 2009; Evangelou et al. 2014; Vilchez et al. 2014; Liu et al. 2014; Taniguchi et al. 2017; Kalil et al. 2021) composed of patients with HTLV-1 without HAM/TSP (Kira et al. 1991; Howard et al. 2003; Griffith et al. 2006; Morgan et al. 2007; Evangelou et al. 2014; Liu et al. 2014; Vilchez et al. 2014; Kalil et al. 2021), patients with other diseases (Kira et al. 1988, 1991; Rudge et al. 1991; Howard et al. 2003; Liu et al. 2014), and/or healthy controls (Fukushima et al. 1994; Griffith et al. 2006; Kuriyama et al. 2009; Evangelou et al. 2014; Liu et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017; Kalil et al. 2021). The resonance equipment most frequently used in the studies had 1.5 T (Kira et al. 1988, 1991; Fukushima et al. 1994; Ferraz et al. 1997; Howard et al. 2003; Cervilla et al. 2006; Griffith et al. 2006; Morgan et al. 2007; Yukitake et al. 2008; Kuriyama et al. 2009; Evangelou et al. 2014) and 3.0 T (Puccioni-Sohler et al. 2012; Liu et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017; Kalil et al. 2021). Most studies (52.2%) used some tool to assess the functionality of patients, with the Expanded Disability Status Scale (EDSS) (Kira et al. 1988, 1991; Howard et al. 2003; Griffith et al. 2006; Morgan et al. 2007; Yukitake et al. 2008; Kuriyama et al. 2009; Puccioni-Sohler et al. 2012; Liu et al. 2014; Taniguchi et al. 2017) and Osame’s Motor Disability Score (OMDS) (Morgan et al. 2007; Kuriyama et al. 2009; Taniguchi et al. 2017; Kalil et al. 2021) being the most frequently chosen. The WHO criteria were used by 34.8% of the studies to diagnose cases of HAM/TSP.
Supplementary Table 2 shows the brain and spinal changes observed in MRI. White matter injuries were the most frequent finding of the brain, verified in 16 of 23 (69.6%) articles. Brain injuries were most frequently identified in the periventricular region (Tournier-Lasserve et al. 1987; Kira et al. 1988, 1991; Rudge et al. 1991; Alcindor et al. 1992; Melo et al. 1993; Fukushima et al. 1994; Douen et al. 1997; Howard et al. 2003; Vilchez et al. 2014; Kalil et al. 2021), in the subcortical region (Kira et al. 1988, 1991; Alcindor et al. 1992; Melo et al. 1993; Douen et al. 1997; Cervilla et al. 2006), in the centrum semiovale (Cervilla et al. 2006; Vilchez et al. 2014; Kalil et al. 2021), in the brain stem (Rudge et al. 1991; Ferraz et al. 1997), and in the corpus callosum (Rudge et al. 1991). However, 2 of 16 articles (12.5%) did not specify the location of the lesions found (Morgan et al. 2007; Yukitake et al. 2008). Brain atrophy was a poorly evaluated outcome (4 of 16 articles) (Fukushima et al. 1994; Ferraz et al. 1997; Morgan et al. 2007; Puccioni-Sohler et al. 2012).
Spinal cord changes were verified by 18 of 23 studies and atrophy was the most frequent finding (71.4%), affecting the thoracic (Rudge et al. 1991; Melo et al. 1993; Yukitake et al. 2008; Kuriyama et al. 2009) and cervical (Puccioni-Sohler et al. 2012) regions alone or both (Ferraz et al. 1997; Howard et al. 2003; Cervilla et al. 2006; Evangelou et al. 2014; Liu et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017). Focal lesions in white matter (Howard et al. 2003; Umehara et al. 2007; Yukitake et al. 2008; Vilchez et al. 2014; Gao et al. 2018) have also been observed by some studies. Only two study did not specify the abnormalities found (Tournier-Lasserve et al. 1987; Alcindor et al. 1992).
Table 2 shows brain and spinal lesions observed in MRI of HAM/TSP’s patients, HTLV-1 patients without HAM/TSP, and healthy controls. Brain white matter lesions were more frequent in HAM/TSP than HTLV-1 carriers (Kira et al. 1991; Vilchez et al. 2014) and healthy controls (Kira et al. 1991; Fukushima et al. 1994; Vilchez et al. 2014). Theses lesions were associated with cognitive impairment (Cervilla et al. 2006; Kalil et al. 2021), and reduced myelination of the ventral (corticospinal) and dorsal (spinothalamic) tracts (Vilchez et al. 2014), but not associated with age or duration of disease (Fukushima et al. 1994). HTLV-1 carriers had more white matter lesions on the corpus striatum than HAM/TSP patients (Howard et al. 2003). Three of 18 studies did not show location of lesions (Morgan et al. 2007; Yukitake et al. 2008; Puccioni-Sohler et al. 2012).
Cervical and thoracic atrophy was more frequent in HAM/TSP patients than HTLV-1 carriers (Liu et al. 2014; Vilchez et al. 2014) and healthy controls (Evangelou et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017). Thoracic atrophy was associated with a longer symptom duration (Vilchez et al. 2014). These conditions were not associated with EDSS and OMDS scales (Evangelou et al. 2014; Taniguchi et al. 2017). One study demonstrated that the number of white matter lesions on cervical spinal cord could increase after 1 year of symptoms and is highlighted by contrast (Gao et al. 2018). Nine of 23 studies did not use case–control or comparative group methodology (Tournier-Lasserve et al. 1987; Alcindor et al. 1992; Melo et al. 1993; Douen et al. 1997; Umehara et al. 2007; Yukitake et al. 2008; Kuriyama et al. 2009; Puccioni-Sohler et al. 2012; Gao et al. 2018).
Discussion
The evaluated studies show that patients with HAM/TSP can present brain white matter lesions (Tournier-Lasserve et al. 1987; Kira et al. 1988, 1991; Rudge et al. 1991; Alcindor et al. 1992; Melo et al. 1993; Fukushima et al. 1994; Douen et al. 1997; Howard et al. 2003; Cervilla et al. 2006; Griffith et al. 2006; Vilchez et al. 2014; Kalil et al. 2021), these are in greater number than those found in healthy controls (Kira et al. 1988, 1991; Fukushima et al. 1994; Vilchez et al. 2014; Kalil et al. 2021). In addition to the white matter lesions, brain atrophy was also found. These neuroimaging findings and their association with cognitive impairment reinforce that the brain is also a target organ in HTLV-1 infection. However, the absence of information related to the sample (Alcindor et al. 1992; Fukushima et al. 1994; Griffith et al. 2006; Yukitake et al. 2008), disease duration of patients with HTLV-1 with or without HAM/TSP (Tournier-Lasserve et al. 1987; Kira et al. 1991; Alcindor et al. 1992; Melo et al. 1993; Howard et al. 2003; Griffith et al. 2006; Umehara et al. 2007; Morgan et al. 2007; Evangelou et al. 2014; Liu et al. 2014; Kalil et al. 2021), specifications of the resonance apparatus (Tournier-Lasserve et al. 1987; Fukushima et al. 1994; Douen et al. 1997; Cervilla et al. 2006; Griffith et al. 2006; Umehara et al. 2007; Puccioni-Sohler et al. 2012; Taniguchi et al. 2017; Gao et al. 2018; Kalil et al. 2021), and the clinical/functional evaluation (Kira et al. 1988, 1991; Fukushima et al. 1994; Howard et al. 2003; Evangelou et al. 2014; Taniguchi et al. 2017) are significant limitations presented by the articles. These situations make it difficult to compare the results of these studies and the association between the clinical assessments carried out by the physician and imaging tests.
Patients with HAM/TSP have chronic CNS inflammation. The presence of chronic lymphocytic perivascular infiltrate in the central nervous system suggests vasculitis (Yamano and Sato 2012). In addition, pro-inflammatory cytokines produced by macrophages, astrocytes, and oligodendrocytes favor progressive gliosis and demyelination in the CNS (Lepoutre et al. 2009). This may explain the asymmetry of brain injuries and atrophy seen in MRI (Ferraz et al. 1997; Griffith et al. 2006; Morgan et al. 2007; Puccioni-Sohler et al. 2012). There is an association between an increase in the proviral load (Kalil et al. 2021) both with an increase in serum INF-γ levels and with the occurrence of white matter lesions (Morgan et al. 2007).
Lesions of the subcortical white matter can contribute to a variety of behavioral syndromes. HTLV-1 patients present psychiatric and cognitive symptoms such as anxious and depressive symptoms (Raulino Goncalves et al. 2017), impaired verbal fluency and visual and verbal memory (Silva et al. 2003), and lower memory score and percentage of information retention (Kalil et al. 2021) when compared to healthy individuals. Lesions in the subcortical white matter of these patients, oval and round in shape and with a diameter of less than 5 mm (Cervilla et al. 2006), and increase of proviral load were significantly associated with cognitive changes (Cervilla et al. 2006; Kalil et al. 2021). Even patients with HTLV-1 and without HAM/TSP have more cognitive changes than controls without HTLV-1. These patients presented milder impairment, affecting the fluency of words, associative capacity, reasoning, and short-term memory.(Gascón et al. 2017) These cognitive changes, found in patients with or without myelopathy, together with the changes found in brain neuroimaging, corroborate the hypothesis that the brain is also affected by HTLV-1.
The studies analyzed included patients with different times of illness (means varied from 1.37 to 19.2 years) and different ages (means varied from 28.7 to 67 years) for groups of patients with HAM/TSP. The influence of the duration of the patient’s age and disease on the appearance of brain injuries is controversial. Lesions in the white matter of the brain were more observed in the first 10 years after the onset of myelopathy (Kira et al. 1991), and were less frequent in the chronic phase of the disease (Vilchez et al. 2014). However, in a study of patients with HAM/TSP, longer disease duration was associated with a greater number of white matter lesions in the brain (Kira et al. 1991). Increasing age was associated with lesions in the periventricular region (Puccioni-Sohler et al. 2012) in patients with HAM/TSP, and with an increase in the number of lesions in white matter in patients with HTLV-1 and without HAM/TSP (Morgan et al. 2007).
Spinal changes were seen in 16 of 18 articles. Atrophy was the most frequent finding, being more frequent in the thoracic (Rudge et al. 1991; Melo et al. 1993; Ferraz et al. 1997; Howard et al. 2003; Cervilla et al. 2006; Yukitake et al. 2008; Kuriyama et al. 2009; Evangelou et al. 2014; Liu et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017) and cervical (Ferraz et al. 1997; Howard et al. 2003; Cervilla et al. 2006; Yukitake et al. 2008; Puccioni-Sohler et al. 2012; Evangelou et al. 2014; Liu et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017) regions. This atrophy is greater than in controls (Evangelou et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017), and is associated with the time of disease progression (Ferraz et al. 1997; Cervilla et al. 2006; Vilchez et al. 2014), motor disability (supported gait or without march) (Cervilla et al. 2006; Liu et al. 2014), and increase of IgG on CSF (Rudge et al. 1991). Besides, mild or severe cases of spinal atrophy also showed lesions in the subcortical white matter in patients with HAM/TSP. (Cervilla et al. 2006).
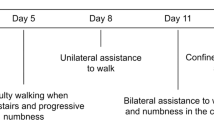
White matter involvement was also more frequent in the cervical and thoracic regions (Howard et al. 2003; Umehara et al. 2007; Yukitake et al. 2008; Puccioni-Sohler et al. 2012; Vilchez et al. 2014; Gao et al. 2018). The clinical/neurological manifestations in these patients are more severe and involve paraparesis (Puccioni-Sohler et al. 2012; Vilchez et al. 2014), urinary incontinence, sensory loss to light touch (Vilchez et al. 2014), and EDSS score (6.5–7.5) (need bilateral assistance to walk or wheelchair users) (Yukitake et al. 2008; Puccioni-Sohler et al. 2012). It is not yet clear why the neurological damage appears preferably in these specific regions. A factor that could explain this selectivity would be the migration of immune cells through the blood–brain barrier where blood flow is slower, that is, in the thoracic sections of the vertebral and Adamkiewicz arteries (Izumo 2010).
Neuroinflammation favors the occurrence of spinal cord damage in patients with HAM/TSP. The articles in this review show that active inflammation in the cerebrospinal fluid (CSF) (Puccioni-Sohler et al. 2012), the increase in IgG in the CSF (Yukitake et al. 2008), and the increase in the proviral load (Rudge et al. 1991) are associated with greater severity of myelopathy. This more severe form is developed by 10% of patients with HAM/TSP and is associated with lesions in the spinal cord and brain white matter (Yukitake et al. 2008).
Most of the included studies describe spinal cord white matter injuries and mean age over 50 in the groups of patients with HAM/TSP. Therefore, it is possible that microdegeneration resulting from senescence, which also promotes nonspecific lesions in white matter, may contribute to changes in the MRI of the infected population (Puccioni-Sohler et al. 2012).
Functional capacity was assessed in 19 of 23 articles. Neurological/functional impairment was assessed using scores from six different scales: EDSS (3.5–7.0) (Kira et al. 1988, 1991; Ferraz et al. 1997; Howard et al. 2003; Griffith et al. 2006; Morgan et al. 2007; Yukitake et al. 2008; Kuriyama et al. 2009; Puccioni-Sohler et al. 2012; Evangelou et al. 2014; Liu et al. 2014; Taniguchi et al. 2017), SNRS (56) (Liu et al. 2014), IPEC (15–17.8) (Evangelou et al. 2014; Liu et al. 2014), OMDS (3.4–6.0) (Puccioni-Sohler et al. 2012; Taniguchi et al. 2017), FIM (111) (Kuriyama et al. 2009), and AI (5) (Liu et al. 2014), and few studies used cognitive tests (Kalil et al. 2021), manual muscle testing (MMT) (Douen et al. 1997; Gao et al. 2018) or gait assessment (Cervilla et al. 2006), or description of the neurological condition (Tournier-Lasserve et al. 1987). Three of them found an association between spinal cord alterations and functional impairment (Cervilla et al. 2006; Yukitake et al. 2008; Liu et al. 2014), four found no association (Ferraz et al. 1997; Evangelou et al. 2014; Vilchez et al. 2014; Taniguchi et al. 2017), and ten did not perform this analysis (Tournier-Lasserve et al. 1987; Kira et al. 1988, 1991; Fukushima et al. 1994; Douen et al. 1997; Howard et al. 2003; Griffith et al. 2006; Kuriyama et al. 2009; Puccioni-Sohler et al. 2012; Gao et al. 2018). In patients with HAM/TSP, thoracic spinal cord atrophy (Cervilla et al. 2006; Liu et al. 2014) and thoracic and cervical spinal cord white matter lesions (Yukitake et al. 2008) were associated with functional worsening.
Eighteen of the twenty-three studies included defined the eligibility criteria for patients with HAM/TSP. The way to classify patients as having this myelopathy varied between studies. Despite this, in four studies, a neurological examination was performed for the diagnosis of HAM/TSP, which may have reduced the classification error (Kira et al. 1988; Rudge et al. 1991; Melo et al. 1993; Vilchez et al. 2014). Thirteen out of twenty-three articles did not identify the distribution of the participants by gender (Kira et al. 1991), the duration of the disease (Tournier-Lasserve et al. 1987; Kira et al. 1991; Alcindor et al. 1992; Melo et al. 1993; Howard et al. 2003; Umehara et al. 2007; Morgan et al. 2007; Yukitake et al. 2008; Evangelou et al. 2014; Liu et al. 2014; Kalil et al. 2021), and the average age of a group of participants (Alcindor et al. 1992; Fukushima et al. 1994; Griffith et al. 2006; Yukitake et al. 2008), impairing the evaluation of the external validity of these studies.
Sixteen of twenty-three studies did not define which professionals performed the interpretation of the MRI (Kira et al. 1991, 1988; Rudge et al. 1991; Alcindor et al. 1992; Melo et al. 1993; Fukushima et al. 1994; Douen et al. 1997; Ferraz et al. 1997; Howard et al. 2003; Cervilla et al. 2006; Griffith et al. 2006; Umehara et al. 2007; Liu et al. 2014; Evangelou et al. 2014; Taniguchi et al. 2017; Gao et al. 2018). In only three of these studies, blinding was performed at this stage (Morgan et al. 2007; Vilchez et al. 2014; Kalil et al. 2021). This lack of blinding may have led to a greater appreciation of changes in imaging tests among symptomatic patients, overestimating the results found.
Seven out of twenty-three studies defined a standardization to direct the investigation of brain injuries. As for the spinal cord, there was a variation in the anatomical regions evaluated. Magnetic fields ranging from 0.5 to 3.0 T were used, and ten of 23 articles did not specify the sequences used to obtain the images, and four of the 23 articles did not report the quality of the resonance equipment. The quality of the equipment used over the years may have underestimated the findings of the oldest studies.
This review points to some gaps in the literature. There are no cohort studies evaluating whether the clinical progression of spinal cord disease occurs in parallel with brain and spinal cord atrophy or the progression of brain and spinal cord white matter lesions. These prospective studies would make it possible to assess whether progression of cognitive changes is associated with worsening brain neuroimaging in both asymptomatic patients and those with HAM/TSP.
Conclusion
The systematic review of the literature on brain and spinal changes verified through magnetic resonance in patients with HAM/TSP reveals a small number of studies, with several methodological differences. The data on patients such as age at onset of the disease, duration of disease progression, diagnostic criteria for HAM/TSP disease, ethnic origin of the patients, analysis methodology, and MRI device used varied a lot and were not always available in the articles. In addition, the heterogeneity of the methods employed proved to be a problem for comparing the results and makes it difficult to replicate the studies.
In these studies, lesions in the brain white matter and spinal cord atrophy were the most frequently reported changes. Changes in spinal cord white matter and brain atrophy have also been described. There was no contrast uptake in brain injuries, but there was in spinal cord injuries.
References
Alcindor E, Valderrama R, Canavaggio M et al (1992) Imaging of human T-lymphotropic virus type I-associated chronic progressive myeloneuropathies. Neuroradiology 35:69–74. https://doi.org/10.1007/BF00588283
Bagnato F, Butman J, Mora CA et al (2005) Conventional magnetic resonance imaging features in patients with tropical spastic paraparesis. J Neurovirol. https://doi.org/10.1080/13550280500385039
Carneiro-Proietti ABF, Catalan-Soares BC, Castro-Costa CM et al (2006) HTLV in the Americas: challenges and perspectives. Rev Panam Salud Publica/pan Am J Public Heal 19:44–53. https://doi.org/10.1590/S1020-49892006000100007
Carneiro-Proietti ABF, Ramos Ribas JG, Catalan-Soares BC et al (2002) Infection and disease caused by the human T cell lymphotropic viruses type I and II in Brazil. Rev Soc Bras Med Trop. https://doi.org/10.1590/s0037-86822002000500013
Cervilla J, Cartier L, García L (2006) Brain and spinal cord magnetic resonance imaging in spastic paraparesis associated to human T-lymphotropic virus. Rev Med Chil. https://doi.org/10.4067/S0034-98872006000800010
De Castro-Costa CM, Araújo AQC, Barreto MM et al (2006) Proposal for diagnostic criteria of tropical spastic paraparesis/HTLV-I- associated myelopathy (TSP/HAM). AIDS Res Hum Retroviruses 22:931–935. https://doi.org/10.1089/aid.2006.22.931
Douen AG, Elizabeth Pringle C, Guberman A (1997) Human T-cell lymphotropic virus type 1 myositis, peripheral neuropathy, and cerebral white matter lesions in the absence of spastic paraparesis. Arch Neurol 54:896–900. https://doi.org/10.1001/archneur.1997.00550190084018
Evangelou IE, Massoud R, Jacobson S (2014) HTLV-I-associated myelopathy/tropical spastic paraparesis: semiautomatic quantification of spinal cord atrophy from 3-dimensional MR images. J Neuroimaging 24:74–78. https://doi.org/10.1111/j.1552-6569.2011.00648.x
Ferraz AC, Gabbai AA, Abdala N, Nogueira RG (1997) Ressonância magnética na mielopatia associada ao HTLV-I: Leucoencefalopatia e atrofia medular. Arq Neuropsiquiatr. https://doi.org/10.1590/s0004-282x1997000500008
Fukushima T, Ikeda T, Uyama E et al (1994) Cognitive event-related potentials and brain magnetic resonance imaging in HTLV-1 associated myelopathy (HAM). J Neurol Sci 126:30–39. https://doi.org/10.1016/0022-510X(94)90091-4
Gao H, Ye X, Cai R et al (2018) Multiple spotty lesions of the spinal cord in a Chinese patient with human T-lymphotropic virus type 1-associated myelopathy/tropical spastic paraparesis. Int J Infect Dis 68:1–3. https://doi.org/10.1016/j.ijid.2017.12.022
Gascón MRP, Casseb J, Smid J et al (2017) Cognitive impairment is frequent among symptomatic carriers of human T-cell lymphotropic virus type 1 (HTLV-1), regardless of their clinical status. J Neurol Sci. https://doi.org/10.1016/j.jns.2017.04.019
Gessain A, Vernant JC, Maurs L et al (1985) Antibodies to human T-lymphotropic virus type-I in patients with tropical spastic paraparesis. Lancet 326:407–410. https://doi.org/10.1016/S0140-6736(85)92734-5
Griffith C, Bagnato F, Gupta S et al (2006) Brain volume measurements in patients with human T-cell lymphotropic virus-1-associated tropical spastic paraparesis. J Neurovirol. https://doi.org/10.1080/13550280600941665
Hemond CC, Bakshi R (2018) Magnetic resonance imaging in multiple sclerosis. Cold Spring Harb Perspect Med 8:1–21. https://doi.org/10.1101/cshperspect.a028969
Howard AK, Li DKB, Oger J (2003) MRI contributes to the differentiation between MS and HTLV-I associated myelopathy in British Columbian coastal natives. Can J Neurol Sci 30:41–48. https://doi.org/10.1017/S0317167100002420
Izumo S (2010) Neuropathology of HTLV-1-associated myelopathy (HAM/TSP): the 50th anniversary of Japanese society of neuropathology. In: Neuropathology
Kalil RS, Vasconcellos I, Rosadas C et al (2021) Association between high proviral load, cognitive impairment, and white matter brain lesions in HTLV-1-infected individuals. J Neurovirol. https://doi.org/10.1007/s13365-021-00944-6
Kira JI, Fujihara K, Itoyama Y et al (1991) Leukoencephalopathy in HTLV-I-associated myelopathy/tropical spastic paraparesis: MRI analysis and a two year follow-up study after corticosteroid therapy. J Neurol Sci. https://doi.org/10.1016/0022-510X(91)90192-A
Kira JI, Minato SI, Itoyama Y et al (1988) Leukoencephalopathy in HTLV-I-associated myelopathy: MRI and EEG data. J Neurol Sci. https://doi.org/10.1016/0022-510X(88)90247-X
Kuriyama N, Niwa F, Watanabe Y et al (2009) Evaluation of autonomic malfunction in HTLV-1 associated myelopathy (HAM). Auton Neurosci Basic Clin. https://doi.org/10.1016/j.autneu.2009.05.252
Lepoutre V, Jain P, Quann K et al (2009) Role of resident CNS cell populations in HTLV-1-associated neuroinflammatory disease. Front Biosci. https://doi.org/10.2741/3300
Liu W, Nair G, Vuolo L et al (2014) In vivo imaging of spinal cord atrophy in neuroinflammatory diseases. Ann Neurol. https://doi.org/10.1002/ana.24213
Marano G, Vaglio S, Pupella S et al (2016) Human T-lymphotropic virus and transfusion safety: does one size fit all? Transfusion. https://doi.org/10.1111/trf.13329
Martin F, Taylor GP, Jacobson S (2014) Inflammatory manifestations of HTLV-1 and their therapeutic options. Expert Rev Clin Immunol
Melo A, Moura L, Rios S et al (1993) Magnetic resonance imaging in HTLV-I associated myelopathy. Arq Neuropsiquiatr 51:329–332. https://doi.org/10.1590/S0004-282X1993000300006
Mendes GB, Kalil RS, Rosadas C et al (2014) Temporal lesions and widespread involvement of white matter associated with multi-organ inflammatory disease in human T-lymphotropic virus type 1-associated myelopathy/tropical spastic paraparesis (HAM/TSP). Int J Infect Dis. https://doi.org/10.1016/j.ijid.2014.03.1374
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med
Morgan DJ, Caskey MF, Abbehusen C et al (2007) Brain magnetic resonance imaging white matter lesions are frequent in HTLV-I carriers and do not discriminate from HAM/TSP. AIDS Res Hum Retroviruses 23:1499–1503. https://doi.org/10.1089/aid.2007.0077
Nicolás D, Ambrosioni J, Paredes R et al (2015) Infection with human retroviruses other than HIV-1: HIV-2, HTLV-1, HTLV-2, HTLV-3 and HTLV-4. Expert Rev Anti Infect Ther 13:947–963. https://doi.org/10.1586/14787210.2015.1056157
Nozuma S, Matsuura E, Matsuzaki T et al (2016) Erratum: familial clusters of HTLV-1-associated myelopathy/tropical spastic paraparesis (PLoS ONE (2014) 9:5. https://doi.org/10.1371/journal.pone.0086144). PLoS ONE 11:3–5. https://doi.org/10.1371/journal.pone.0152954
Osame M, Usuku K, Izumo S et al (1986) Htlv-I associated myelopathy, a new clinical entity. Lancet 327:1031–1032. https://doi.org/10.1016/S0140-6736(86)91298-5
Proietti FA, Carneiro-Proietti ABF, Catalan-Soares BC, Murphy EL (2005) Global epidemiology of HTLV-I infection and associated diseases. Oncogene. https://doi.org/10.1038/sj.onc.1208968
Puccioni-Sohler M, Gasparetto E, Cabral-Castro MJ et al (2012) HAM/TSP: association between white matter lesions on magnetic resonance imaging, clinical and cerebrospinal fluid findings. Arq Neuropsiquiatr 70:246–251. https://doi.org/10.1590/s0004-282x2012000400004
Raulino Goncalves L, Fernandes Barbosa LN, Machado Ribeiro Magalhaes P, Sampaio Rocha-Filho PA (2017) Characterization of cognitive performance and evaluation of quality of life among patients with HTLV-1. Clin Neurol Neurosurg. https://doi.org/10.1016/j.clineuro.2017.07.008
Rudge P, Ali A, Cruickshank JK (1991) Multiple sclerosis, tropical spastic paraparesis and HTLV-1 infection in Afro-Caribbean patients in the United Kingdom. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp.54.8.689
Shiwa SR, Costa LO, de Moser AD, Aguiar ID, Oliveira LV et al (2011) PEDro: a base de dados de evidências em fisioterapia. Fisioter Em Mov. https://doi.org/10.1590/s0103-51502011000300017
Silva MTT, Harab RC, Leite AC et al (2007) Human T lymphotropic virus type 1 (HTLV-1) proviral load in asymptomatic carriers, HTLV-1-associated myelopathy/tropical spastic paraparesis, and other neurological abnormalities associated with HTLV-1 infection. Clin Infect Dis. https://doi.org/10.1086/510679
Silva MTT, Mattos P, Alfano A, Araújo AQC (2003) Neuropsychological assessment in HTLV-1 infection: a comparative study among TSP/HAM, asymptomatic carriers, and healthy controls. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp.74.8.1085
Taniguchi A, Mochizuki H, Yamashita A et al (2017) Spinal cord anteroposterior atrophy in HAM/TSP: magnetic resonance imaging and neuropathological analyses. J Neurol Sci 381:135–140. https://doi.org/10.1016/j.jns.2017.08.3243
Tournier-Lasserve E, Gout O, Gessain A, Iba-Zizen MT, Lyon-Caen O, Lhermitte F (1987) HTLV-I, brain abnormalities on magnetic resonance imaging, and relation with multiple sclerosis. Lancet 4:49–50. https://doi.org/10.1016/s0140-6736(87)93092-3
Umehara F, Nose H, Saito M et al (2007) Abnormalities of spinal magnetic resonance images implicate clinical variability in human T-cell lymphotropic virus type I-associated myelopathy. J Neurovirol 13:260–267. https://doi.org/10.1080/13550280701258431
Vilchez C, Gonzalez-Reinoso M, Cubbison C et al (2014) Atrophy, focal spinal cord lesions and alterations of diffusion tensor imaging (DTI) parameters in asymptomatic virus carriers and patients suffering from human T-lymphotrophic virus type 1 (HTLV-1)-associated myelopathy/tropical spastic paraparesis (HAM/. J Neurovirol. https://doi.org/10.1007/s13365-014-0282-2
Yamano Y, Sato T (2012) Clinical pathophysiology of human T-lymphotropic virus-type 1-associated myelopathy/tropical spastic paraparesis. Front Microbiol. https://doi.org/10.3389/fmicb.2012.00389
Yukitake M, Takase Y, Nanri Y et al (2008) Incidence and clinical significances of human T-cell lymphotropic virus type I-associated myelopathy with T2 hyperintensity on spinal magnetic resonance images. Intern Med. https://doi.org/10.2169/internalmedicine.47.1284
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brazil (CAPES) – finance code 001. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance code 001
Author information
Authors and Affiliations
Contributions
APBF–conception and design of the study; data collection; analysis and interpretation of data; preparation and review of the article; and approved the final version to be published. ADFSN–data collection; analysis and interpretation of data; and approved the final version to be published. ASRF–conception and design of the study; analysis and interpretation of data; review of the article; and approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bastos Ferreira, A.P., do Nascimento, A.D.F.S. & Sampaio Rocha-Filho, P.A. Cerebral and spinal cord changes observed through magnetic resonance imaging in patients with HTLV-1–associated myelopathy/tropical spastic paraparesis: a systematic review. J. Neurovirol. 28, 1–16 (2022). https://doi.org/10.1007/s13365-021-01043-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-021-01043-2