Abstract
The objective of this study is to describe the chronic pain characteristics in individuals infected with human T cell lymphotropic virus type 1 (HTLV-1) per subgroup (asymptomatic, oligosymptomatic, and HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP)) compared with controls with chronic pain without HTLV-1. This is a cross-sectional study investigating associations between pain profile, psychopathological symptoms, and quality of life. Individuals infected with HTLV-1 refer high-intensity pain compared with controls, with more severe characteristics being present in oligosymptomatic and HAM/TSP individuals. Oligosymptomatic individuals have a tendency of diffuse and frequent pain, mainly in the head/neck region and more depressive symptoms, resembling nociplastic pain. Neuropathic pain was localized in the lower limbs in all infected groups, worse in HAM/TSP individuals, and associated with a worse perception of quality of life. Pain was associated to higher levels of TNF-alpha and interferon-gamma. HTLV-1 pain is generally more severe when compared with other chronic pain syndromes, being present mainly in the lower limbs. Certain characteristics are typical, depending on the affected group. Oligosymptomatic and HAM/TSP individuals present more diffuse pain, with higher intensity and greater impact in quality of life. Increased levels of inflammatory cytokines are associated with HTLV-1-related pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The human T cell lymphotropic virus type 1 (HTLV-1) is a retrovirus that affects millions of people worldwide (Gessain and Cassar 2012). HTLV-1 is endemic in Japan, sub-Saharan Africa, the Caribbean Islands, and South America (Hlela et al. 2009). In Brazil, the virus is found in all regions, but the largest seroprevalence among blood donors is in the north and northeast of the country (Vrielink and Reesink 2004; Catalan-Soares et al. 2005). Salvador is the most affected city, with about 1.76% of the population infected (Dourado et al. 2003). Between 2 and 3% of infected individuals develop HTLV-1-associated myelopathy or tropical spastic paraparesis (HAM/TSP) (Araujo and Silva 2006), but morbidities related to the virus are present in approximately 56% of those infected (Tanajura et al. 2015).
Chronic pain (CP) is one of the main symptoms with a prevalence of 35.3 to 88.4% (San-Martin et al. 2016; Santos et al. 2017). CP in HTLV-1 is associated with self-medication and depression (San-Martin et al. 2016; Santos et al. 2017), with negative impact on quality of life (Martins et al. 2012; Macêdo et al. 2016) and functional independence (Franzoi and Araújo 2007). It often presents as diffuse and difficult to control (Martin et al. 2010; San-Martin et al. 2016; Santos et al. 2017). Its nature is also diverse, as nociceptive (NoP) and neuropathic pain (NeP) have been described (San-Martin et al. 2016; Santos et al. 2017). However, it is often difficult to disentangle NeP from neuropathic symptoms (NeSymp), which could be related to other processes not directly related to lesion of the somatosensory system such as central sensitization(Kamen 2018) or nociplastic pain (Kosek et al. 2016). NeSymp seem to be present in about 57.1–78.9% of infected patients (Castro-Costa et al. 2009; Netto and Brites 2011), with moderate to severe intensity (Martin et al. 2010; San-Martin et al. 2016), and located mainly in the low back and lower limbs (San-Martin et al. 2016). However, these data are related mainly to people with clinical characteristics of HAM/TSP, and much less is known about pain in the other subgroups of infected people (asymptomatics and oligosymptomatics).
CP impact may be associated with sociodemographic factors, type, intensity and location of pain, reactive aspects to pain, and dimensions of quality of life. It may also present distinct characteristics according to the subgroups of asymptomatic, oligosymptomatic, and defined for myelopathy (HAM/TSP). As such, the analysis of these differences can help in a better understanding of the diagnosis, the prognosis, and therapeutics, increasing the possibility of pain control. Taking into consideration these limitations in the knowledge about CP in HTLV-1, the present study therefore aims to compare the characteristics of CP (intensity, location, and type), psychoaffective symptoms, and quality of life in subgroups of individuals with and without HTLV-1, to better characterize pain associated to the infection.
Methods
This cross-sectional study was carried out in a multidisciplinary HTLV-1 outpatient clinic at the “Hospital Universitário Professor Edgard Santos” (Salvador-BA, Brazil). Individuals at this clinic are first diagnosed using the ELISA test (Cambridge Biotech, Worcester, MA) followed by the Western blot examination (HTLV Blot 2.4, Genelabs, Science Park Drive, Singapore) to detect antibodies to the virus. They were stratified as asymptomatic, oligosymptomatic (possible or probable HAM/TSP) and defined to HAM/TSP (Castro-Costa et al. 2009).
The number of participants was defined by a sample size calculation that considered a difference in pain prevalence of 80% between subjects with and without myelopathy, with a confidence interval of 95% (Mendes et al. 2013). The outpatient clinic had 440 seropositive individuals registered during the study period (July 2012 to February 2014); of these, 143 individuals were investigated about CP (Santos et al. 2017). A comparison group of blood donors was voluntarily recruited at the Hematology and Hemotherapy Foundation of Bahia (HEMOBA, Salvador-BA, Brazil). Of the four groups analyzed in this study, three were formed by individuals infected by HTLV-1 and one by seronegative, paired by sex and age. We included individuals with 20 years or older, presenting pain for at least 6 months, of a continuous or recurrent nature in the last 3 months (Merskey 1986). We did not include individuals with HTLV-1 greater than 68 years.
The sociodemographic and clinical data were collected by means of a standardized form. For the characterization of pain, a body diagram was used to localize the symptoms, and a visual analog scale (VAS) with 0–10 cm was used to quantify pain intensity. To assess the quality of pain, we applied the McGill (Pimenta and Teixeira 1996) and DN4 questionnaires (Santos et al. 2010) in those individuals who reported the presence of pain. Pain was characterized as diffuse if it was present on both sides of the body plus above and below the waistline, and concomitant in the axial skeleton (cervical spine and/or anterior chest and/or thoracic spine and/or low back), pain in the buttock or shoulder was considered as pain for each side involved, and low back pain as lower segment pain (Bellato et al. 2012). The International Association for the Study of Pain introduced a recent terminology to characterize pain arising from altered nociception called Nociplastic Pain (Kosek et al. 2016), which may be an explanation for the diffuse and debilitating pain frequently seen in patients with HTLV-1. We tried to identify some of its characteristics in our sample by using items related to central sensitization that were present in the individuals’ data sheets. The identifiable items included the presence of diffuse pain, headache, pain in the pelvic region, signs of anxiety and depression, impact on daily life, sleep disturbances, burning sensations and increased frequency of urination. Complementarily, we applied the NeuPSIG criteria (Finnerup et al. 2016) to add to the DN4 classification of NeP in HTLV-1 individuals only. We searched in their data sheets information regarding the presence of relevant neurological lesions or disease and pain distribution in a neuroanatomically plausible territory. Individuals who presented these characteristics were classified as having possible NeP. In a second step, we identified in their body diagrams those whose pain was distributed in a classical neuroanatomically plausible territory, i.e., the low back and/or lower limbs and was classified as NeP according to the DN4. Those who attended these criteria were classified as having definite NeP.
The Hospital Anxiety and Depression (HAD) scale was used to identify symptoms suggestive of anxiety and/or depression (Castro et al. 2006), and the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) to evaluate quality of life (Ciconelli 1997). We also screened participant for other comorbidities including glaucoma, uveitis, thyroidism, labyrinthitis, psoriasis, pancreatitis, asthma, lupus, heart, disease, depression, gastric ulcer, gastroesophageal reflux, hiatus hernia, umbilical hernia, osteopenia, and osteoporosis. Proviral load and the level of interleukin 5 (IL-5), interleukin 10 (IL-10), interferon-gamma (IFN-y), and tumor necrosis factor alpha (TNFα) cytokines were also assessed.
Initially, a descriptive analysis was made by calculating the absolute and relative frequencies of the sociodemographic and behavioral variables and the clinical conditions, as well as the measures of central tendency and dispersion, with the purpose of characterizing the profile of the studied population. The Kruskal-Wallis non-parametric test for independent samples was used to compare the medians between the groups with the post hoc test of Dunn for comparison between pairs, and the chi-square test to compare the proportions of the categorical variables. Proviral load and the levels of cytokines were Log10 transformed and their association with the presence of pain was assessed through a multivariate general linear model using the Bonferroni test as a post hoc. This study was approved by the Ethics Committee of the Professor Edgard Santos University Hospital, Federal University of Bahia, Salvador-BA, Brazil. All participants signed an Informed Consent before inclusion on the study (protocol 21/2011).
Results
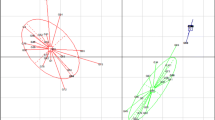
The sample included 100 individuals infected by HTLV-1 (51 asymptomatics, 29 oligosymptomatics, and 20 defined to HAM/TSP) and 31 individuals seronegatives blood donors (Fig. 1). The age mean, gender, and marital status were similar in the different groups (P > 0.05). Regarding schooling, 65.0% of the oligosymptomatic and those defined for HAM/TSP reported study time equal to or less than 12 years, while 54.9% of the asymptomatic individuals and 64.5% of the uninfected control group reported having a study time equal to or greater than 13 years (P < 0.05) (Table 1).
There were a higher proportion of retirees among HTLV-1 infected groups, occurring in 86.4% of patients with HAM/TSP, 50.0% of oligosymptomatic, and 29.9% of asymptomatic patients. In the control group, only 6.9% were in this condition. Unemployment was present in 23.9% of the asymptomatic individuals, in 21.9% of the oligosymptomatic ones, in 9.1% of those defined for HAM/TSP, and in 22.4% of the control group (Table 1).
It was observed that 17 (53.1%) of the oligosymptomatic, 26 (38.8%) of the asymptomatic, and eight (36.4%) of the HAM/TSP individuals were hypertensive, for only five (8.6%) in the control group. This same proportion of hypertensive individuals was maintained in the groups with pain, 17 (55.2%) of the oligosymptomatic individuals, seven (35.0%) of the HAM/TSP, and 17 (33.3%) of the asymptomatic ones were hypertensive, against four (12.9%) of the controls (P < 0.05). Other relevant clinical conditions were uniformly distributed between the studied groups (Table 1).
CP was reported in 73.2% of the sample. Among those infected, 90.9% of those defined for HAM/TSP, 90.6% of the oligosymptomatic, and 76.1% of the asymptomatic ones reported CP, while the control group had a chronic pain prevalence of 53.4% (P < 0.001). Medication usage is described in Table 1. Regarding pain characteristics, the frequency of pain was similar between the studied groups (Table 2). The same happened for pain location, except for pain in the head/neck region, which was more frequent in the oligosymptomatic individuals. However, when only NeP (according to the DN4) was considered, individuals with HAM/TSP presented more pain in the lower limbs (Table 2). This pain was classified as neuropathic by the DN4 in 55.6% of the individuals with HAM/TSP, 33.3% of the oligosymptomatic, and 31.8% of the asymptomatic individuals, compared with 13.0% of the control individuals (P < 0.05). Using the NeuPSIG criteria, 55% of the individuals with HAM/TSP and 34% individuals oligosymptomatic presented NeP (Fig. 2). No asymptomatic was classified as having NeP because we only applied the NeuPSIG criteria for those with the presence of neurological symptoms, i.e., oligosymptomatic and HAM/TSP individuals. Regarding the presence of characteristics of central sensitization, we found that oligosymptomatic participants presented more diffuse pain, headache, depression, and urinary symptoms than all other groups (P < 0.05) (Table 2). There was no difference in pain intensity between the studied groups, although it was seen a trend to increased pain in the total score of the McGill questionnaire on the oligosymptomatic and HAM/TSP individuals (P = 0.56). Those with HAM/TSP used more cognitive-evaluative (P < 0.05) and miscellaneous (P < 0.05) words to describe their pain (Table 2).
Among the infected groups, the negative perception of QoL was more frequent among oligosymptomatic and HAM/TSP individuals, with scores ≤ 50% in virtually all domains (Table 3). Functional capacity (P < 0.001), general health (P < 0.001), vitality (P < 0.05), and social function (P < 0.05) were decreased in these two groups, and generally more affected in the HAM/TSP individuals (Table 3).
The presence of pain was associated with the levels of IFN-y and TNFα. IFN-y was higher in HAM/TSP participants when compared with asymptomatics (P < 0.05) and oligosymptomatic (P < 0.05); TNFα was higher in HAM/TSP participants when compared only with asymptomatics (P < 0.05). Proviral load, IL-5, and IL-10 were not associated with the presence of pain in our sample (Table 4).
Discussion
This is the first study investigating CP in individuals infected by HTLV-1—classified according to Castro-Costa criteria (De Castro-Costa et al. 2006)—that included a seronegative control group. CP is a common symptom that reaches around 40% of the Brazilian population(Sá et al. 2008, 2019; de Souza et al. 2017) specially affecting people with low educational and socioeconomic level, which corresponds to the majority of individuals (around 90%) infected by HTLV-1 (San-Martin et al. 2016). In the present study, CP, depression, and lower scores of quality of life were more present in the subgroups of individuals infected by HTLV-1 than seronegative control groups. The oligosymptomatic subgroup presented the worst scores on several variables, diffuse pain, a higher frequency of pain in the head/neck region, and more depressive symptoms.
Although the cross-sectional nature of this study does not allow for the establishment of causal relationships, many sociodemographic characteristics of the infected individuals may partially explain their pain profile. Low educational level is associated with greater reporting of pain (de Souza et al. 2017) and with the dissemination of virus by the sexual path (Soares et al. 2003; Baptista et al. 2017). Adding to these factors, infected patients are more prone to depressive symptoms and poor quality of life perception, retiring early because of physical incapacity related to sensory-motor deficits (de Souza et al. 2017). CP is also more prevalent in females in the productive age (Tunks et al. 2008; Dionne et al. 2001), which are also the majority of patients with HTLV-1 reporting neurological symptoms (San-Martin et al. 2016). Regarding pain characteristics, there was no difference in the location of NoP by regions, but NeP was more frequent in the lower limbs of the infected groups, being worse in the individuals with HAM/TSP. The presence of NeP is a possible explanation why individuals with HAM/TSP reported lower scores of quality of life, as this type of pain is generally more severe than nociceptive pain (Ellis and Bennett 2013; Ji et al. 2014).
In our sample, individuals with HTLV-1 made use of analgesics, anti-inflammatory, and anti-depressants drugs prescribed for pain control, corroborating with the literature (San-Martin et al. 2016) and differing from the control group. However, especially the use of anti-depressants in lower doses or without an integrative approach to mental disorders may contribute to the underdiagnosed depression in HTLV-1 individuals (Stumpf et al. 2008; Boa-Sorte et al. 2015). This may be a greater problem in oligosymptomatic and HAM/TSP individuals, who present a more intense pain pattern and a higher frequency of depressive symptoms, as in other CP syndromes (Tunks et al. 2008). However, in our study, oligosymptomatic individuals presented higher scores of pain and depression. This phenomenon may be explained by insecurity with progression of the disease, producing reactions of fear as the first symptoms to HAM/TSP (Boa-Sorte et al. 2015). The appearance of virus-related symptoms, pain, and central sensitization may be events that add up and increase the risk of psychoaffective disorders in oligosymptomatic individuals. One study observed a higher frequency of anxiety and/or depression besides suicide risk in these individuals when compared with asymptomatic individuals (Orge et al. 2015). Increased depressive symptoms were also associated with a longer diagnosis time for HAM/TSP (Stumpf et al. 2008; Boa-Sorte et al. 2015). However, the causal relationship between depression and pain was not assessed in any of these studies and remains to be investigated in future studies.
It is unclear why the oligosymptomatic subgroup reports more pain in the neck and head region than other subgroups and the control group. This data differs from other studies with HTLV-1 individuals that found a higher prevalence of lumbar pain (Mendes et al. 2013; San-Martin et al. 2016) and from the profile of CP in the general population in the same city, which affects mainly the lumbar and knee regions (Sá et al. 2009). We suggest that the higher presence of pain in the neck and head region may be a consequence of the spread of pain, as oligosymptomatics individuals also presented the characteristic lower limbs pain. The presence of diffuse pain has been investigated in subgroups infected by HTLV-1 (Mendes et al. 2013) and has been associated with psychoaffective symptoms (Santos et al. 2017), immunological changes, and chronic diseases and infections (Cruz et al. 2005). It is possible that the diffuse nature of pain associated with psychoaffective symptoms share similar mechanisms with what is found in fibromyalgia (Cruz et al. 2005) being central sensitization and/or nociplastic pain mechanisms as possible candidates to explain this condition. Accordingly, we observed that the oligosymptomatic individuals had more diffuse pain, depressive symptoms, and comorbidities that contribute to the diffuse pain profile in this group, suggesting that future studies should approach this topic specifically.
NeP in lower limbs was more severe in HAM/TSP individuals, a serious neurological condition associated with HTLV-1. It is not known when the manifestations of HTLV-1-related diseases begin to appear; however, there is evidence that increased proviral load worsens the neuroinflammatory status and consequently the progression of myelopathy associated with the virus (Lepoutre et al. 2009). Neuroinflammation caused by HTLV-1 favors the development of NeP generally by the interaction of immune cell activity with the glial cells (microglia and astrocyte) (Ellis and Bennett 2013). Both the peripheral nerve injury and the central lesion result in rupture of the blood-spinal cord barrier allowing the influx of peripheral immune cells. This fact contributes to the NeP phenotype (Ellis and Bennett 2013). The central inflammatory response involves microglial and astrocyte cells, known as important in the onset and maintenance of NeP (Ellis and Bennett 2013). Also, the HTLV-1 neurological symptoms primarily compromise the thoracolumbar spinal cord(Liu et al. 2014), favoring the appearance of symptoms in lower segments, a characteristic that may be present even in some of the asymptomatic individuals(Carvalho et al. 2001; Santos et al. 2004), as an early stage of the progression of the neurological manifestations (Tanajura et al. 2015).
Although NeP is a common and debilitating problem in HTLV-1, NoP is also present, and a review study suggests that it is the most prevalent type of pain related to the disease (San-Martin et al. 2016) and was present in our sample. Lumbar pain can be caused by tension and muscle spasm, zygapophyseal joint dysfunction, sacroiliac and discogenic pain, and spinal stenosis (Baron et al. 2016). NoP results from the activation of nociceptors that innervate the ligaments, joints, muscles, fascia, and tendons in response to tissue injury or inflammation and to biomechanical stress (Baron et al. 2016). As the disease progresses, biomechanical changes may increase mechanical load to musculoskeletal structures, predisposing the appearance of nociceptive pain. The mix of NeP and NoP is a hallmark of pain in HTLV-1, which should be properly identified and treated. Clinicians in charge of treating these problems should be aware that there are different sources of pain to be addressed, as generally, the pain in HTLV-1 is indistinctly related to the neurological symptoms, i.e., classified as neuropathic. Also, as the combination of socioeconomic, psychoaffective and disease-related factors are dramatic in HTLV-1; probably, a multidisciplinary approach will give better results than the classical approach with anti-inflammatory and anti-depressant drugs which have very poor or absent clinical evidence of effectiveness in HTLV-1 pain.
The association of the levels of proinflammatory cytokines IFN-y and TNFα with chronic pain in HTLV-1 is a novel finding. However, we cannot rule out that this association was a consequence of their function in the pathophysiology of HTLV-1 invasion into the nervous system, as both cytokines are known to mediate the infiltration of HTLV-1-infected T cells into the neural tissue (Futsch et al. 2018). IFN-y increased levels are seen in viral infections (Lee and Ashkar 2018), which is the case of HTLV-1; however, it is less frequently associated with pain. Even so, IFN-y receptors were shown to be expressed in the spinal cord of rats with neuropathic pain (Robertson et al. 1997; Sonekatsu et al. 2016; Reischer et al. 2020) IFN-y in HTLV-1-related pain (Robertson et al. 1997; Sonekatsu et al. 2016; Reischer et al. 2020). TNFα is much a more recognized mediator of both nociceptive (Hermann et al. 2018) and neuropathic pain (Leung and Cahill 2010), as well as central sensitization (Andrade et al. 2011), but no clear association was established until now with HTLV-1-related pain. The use of IFN-y and TNFα blockers in the control of HTLV-1-related pain may provide further insights into the role of these cytokines in its pathophysiology.
Our results present some limitations regarding the identification of NeP and nociplastic pain in our HTLV-1 individuals. NeP pain was screened through the DN4 and not by the use of the NeuPSIG or IASP criteria for nociplastic pain, which were not well established at the time this project was initiated. In the attempt of overcoming this limitation, we retrieved some relevant data in the individuals’ research records, which reinforced our findings that NeP is present in HTLV-1 infection and that its chronicity is related, at least in part, to altered nociceptive processing.
Conclusion
HTLV-1 pain is generally more severe when compared with other chronic pain syndromes, being present mainly in the lower limbs. Certain characteristics are typical, depending on the affected group. Oligosymptomatic and HAM/TSP individuals present more diffuse pain, with higher intensity, and greater impact in quality of life. Increased levels of inflammatory cytokines are associated with HTLV-1-related pain.
References
Andrade P, Visser-Vandewalle V, Hoffmann C et al (2011) Role of TNF-alpha during central sensitization in preclinical studies. Neurol Sci 32:757–771
Araujo AQC, Silva MTT (2006) The HTLV-1 neurological complex. Lancet Neurol 5:1068–1076
Baptista CJ, Dourado I, Brignol S et al (2017) Factors associated with syphilis seroreactivity among polydrug users in Northeast Brazil: a cross-sectional study using respondent driven sampling. Int J Drug Policy 39:37–42
Baron R, Binder A, Attal N et al (2016) Neuropathic low back pain in clinical practice. Eur J Pain 20:861–873
Boa-Sorte N, Galvão-Castro AV, Borba D et al (2015) HAM/TSP and major depression: the role of age. Braz J Infect Dis 19:314–318
Carvalho EM, Bacellar O, Porto AF et al (2001) Cytokine profile and immunomodulation in asymptomatic human T-lymphotropic virus type 1-infected blood donors. J Acquir Immune Defic Syndr 27:1–6
de Castro-Costa CM, de AraújoQCCâmara ACC et al (2009) Pain in tropical spastic paraparesis/HTLV-I associated myelopathy patients. Arq Neuropsiquiatr 67:866–870
Castro MMC, Quarantini L, Batista-Neves S, et al (2006) Validade da escala hospitalar de ansiedade e depressão em pacientes com dor crônica. Rev Bras Anestesiol 56.: https://doi.org/10.1590/S0034-70942006000500005
Catalan-Soares B, Carneiro-Proietti AB de F, Proietti FA, Interdisciplinary HTLV Research Group (2005) Heterogeneous geographic distribution of human T-cell lymphotropic viruses I and II (HTLV-I/II): serological screening prevalence rates in blood donors from large urban areas in Brazil. Cad Saude Publica 21:926–931
Ciconelli RM (1997) Tradução para o português e validação do questionário genérico de avaliação de qualidade de vida “medical outcomes study 36-item short-form health survey (SF-36)”
Cruz BA, Catalan-Soares B, Proietti F (2005) Manifestações reumáticas associadas ao vírus linfotrópico humano de células T do tipo I (HTLV-I). Rev Bras Reumatol 45:71–77
De Castro-Costa CM, Araújo AQC, Barreto MM et al (2006) Proposal for diagnostic criteria of tropical spastic paraparesis/HTLV-I-associated myelopathy (TSP/HAM). AIDS Res Hum Retroviruses 22:931–935
de Souza JB, Grossmann E, Perissinotti DMN et al (2017) Prevalence of chronic pain, treatments, perception, and interference on life activities: Brazilian population-based survey. Pain Res Manag 2017:4643830
Dourado I, Alcantara LCJ, Barreto ML et al (2003) HTLV-I in the general population of Salvador, Brazil: a city with African ethnic and sociodemographic characteristics. J Acquir Immune Defic Syndr 34:527–531
Ellis A, Bennett DLH (2013) Neuroinflammation and the generation of neuropathic pain. Br J Anaesth 111:26–37
Finnerup NB, Haroutounian S, Kamerman P et al (2016) Neuropathic pain: an updated grading system for research and clinical practice. Pain 157:1599–1606
Franzoi AC, Araújo AQC (2007) Disability and determinants of gait performance in tropical spastic paraparesis/HTLV-I associated myelopathy (HAM/TSP). Spinal Cord 45:64–68
Futsch N, Prates G, Mahieux R, et al (2018) Cytokine networks dysregulation during HTLV-1 infection and associated diseases. Viruses 10.: https://doi.org/10.3390/v10120691
Gessain A, Cassar O (2012) Epidemiological aspects and world distribution of HTLV-1 infection. Front Microbiol 3:388
Hermann W, Lambova S, Muller-Ladner U (2018) Current treatment options for osteoarthritis. Curr Rheumatol Rev 14:108–116
Hlela C, Shepperd S, Khumalo NP, Taylor GP (2009) The prevalence of human T-cell lymphotropic virus type 1 in the general population is unknown. AIDS Rev 11:205–214
Ji R-R, Xu Z-Z, Gao Y-J (2014) Emerging targets in neuroinflammation-driven chronic pain. Nat Rev Drug Discov 13:533–548
Kamen LB (2018) Central sensitization, central sensitization syndromes, and chronic neuropathic pain. Challenging Neuropathic Pain Syndromes 7–20
Kosek E, Cohen M, Baron R et al (2016) Do we need a third mechanistic descriptor for chronic pain states? Pain 157:1382–1386
Lee AJ, Ashkar AA (2018) The dual nature of type I and type II interferons. Front Immunol 9:2061
Lepoutre V, Jain P, Quann K et al (2009) Role of resident CNS cell populations in HTLV-1-associated neuroinflammatory disease. Front Biosci 14:1152–1168
Leung L, Cahill CM (2010) TNF-alpha and neuropathic pain–a review. J Neuroinflammation 7:27
Liu W, Nair G, Vuolo L et al (2014) In vivo imaging of spinal cord atrophy in neuroinflammatory diseases. Ann Neurol 76:370–378
Macêdo MC, de MotaS R, Patrício NA et al (2016) Quality of life and pain multidimensional aspects in individuals with HTLV-1. Braz J Infect Dis 20:494–498
Martin F, Fedina A, Youshya S, Taylor GP (2010) A 15-year prospective longitudinal study of disease progression in patients with HTLV-1 associated myelopathy in the UK. J Neurol Neurosurg Psychiatry 81:1336–1340
Martins JVP, Baptista AF, de AraújoQC A (2012) Quality of life in patients with HTLV-I associated myelopathy/tropical spastic paraparesis. Arq Neuropsiquiatr 70:257–261
Mendes SMD, Baptista AF, Sá KN, et al (2013) Pain is highly prevalent in individuals with tropical spastic paraparesis. HC 1:47
Netto EC, Brites C (2011) Characteristics of chronic pain and its impact on quality of life of patients with HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP). Clin J Pain 27:131–135
Orge GO, Dellavechia TR, Carneiro-Neto JA et al (2015) Psychiatric disorders in HTLV-1-infected individuals with bladder symptoms. PLoS ONE 10:e0128103
Pimenta CA de M, Teixeira MJ (1996) Questionário de dor McGill: proposta de adaptação para a língua portuguesa. Rev Esc Enferm USP 30.: https://doi.org/10.1590/S0080-62341996000300009
Reischer G, Heinke B, Sandkühler J (2020) Interferon-γ facilitates the synaptic transmission between primary afferent C-fibres and lamina I neurons in the rat spinal dorsal horn via microglia activation. Mol Pain 16:1744806920917249
Robertson B, Xu XJ, Hao JX et al (1997) Interferon-gamma receptors in nociceptive pathways: role in neuropathic pain-related behaviour. NeuroReport 8:1311–1316
Sá KN, Baptista AF, Matos MA, Lessa I (2008) Chronic pain and gender in Salvador population, Brazil. Pain 139:498–506
Sá KN, Moreira L, Baptista AF et al (2019) Prevalence of chronic pain in developing countries: systematic review and meta-analysis. Pain Rep 4:e779
San-Martin DL, Santos DND, Baptista AF, Pain Study Group (2016) Pain prevalence, characteristics and associated factors in human T-cell lymphotropic virus type 1 infected patients: a systematic review of the literature. Braz J Infect Dis 20:592–598
Santos DND, Santos KOB, Paixão AB et al (2017) Factors associated with pain in individuals infected by human T-cell lymphotropic virus type 1 (HTLV-1). Braz J Infect Dis 21:133–139
Santos JG, Brito JO, de Andrade DC et al (2010) Translation to Portuguese and validation of the Douleur Neuropathique 4 questionnaire. J Pain 11:484–490
Santos SB, Porto AF, Muniz AL et al (2004) Exacerbated inflammatory cellular immune response characteristics of HAM/TSP is observed in a large proportion of HTLV-I asymptomatic carriers. BMC Infect Dis 4:7
Soares BC, Proietti AB de FC, Proietti FA, Interdisciplinary HTLV-I/II Research Group (2003) HTLV-I/II and blood donors: determinants associated with seropositivity in a low risk population. Rev Saude Publica 37:470–476
Sonekatsu M, Taniguchi W, Yamanaka M, et al (2016) Interferon-gamma potentiates NMDA receptor signaling in spinal dorsal horn neurons via microglia-neuron interaction. Mol Pain 12.: https://doi.org/10.1177/1744806916644927
Stumpf BP, Carneiro-Proietti AB, Proietti FA et al (2008) Higher rate of major depression among blood donor candidates infected with human t-cell lymphotropic virus type 1. Int J Psychiatry Med 38:345–355
Tanajura D, Castro N, Oliveira P et al (2015) Neurological manifestations in human T-cell lymphotropic virus type 1 (HTLV-1)-infected individuals without HTLV-1-associated myelopathy/tropical spastic paraparesis: a longitudinal cohort study. Clin Infect Dis 61:49–56
Tunks ER, Crook J, Weir R (2008) Epidemiology of chronic pain with psychological comorbidity: prevalence, risk, course, and prognosis. Can J Psychiatry 53:224–234
Vrielink H, Reesink HW (2004) HTLV-I/II prevalence in different geographic locations. Transfus Med Rev 18:46–57
Merskey HE (1986) Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 3:S1–226. PMID: 3461421.
Bellato E, et al (2012) Fibromyalgia syndrome: etiology, pathogenesis, diagnosis, and treatment. Pain Res Treat. PMID: 23213512
Dionne CE, et al (2001) Formal education and back pain: a review. J Epidemiol Community Health. PMID: 11413174
Sá K, et al (2009) Prevalence of chronic pain and associated factors in the population of Salvador, Bahia. Rev Saude Publica. PMID:19488666
Acknowledgments
We wish to acknowledge Dr. Edgar de Carvalho, Coordinator of the Multidisciplinary HTLV Ambulatory of Professor Edgard Santos Hospital for allowing this work to be held at this service. We also wish to thank to the Professors Harriet I. Kemop and Andrew Rice, and Pain Study Group (Iasmyn Adélia Victor Fernandes de Oliveira and Davi Tanajura Costa) for their valuable contribution in the participants’ assessment and critical review of the manuscript.
Funding
Studies developed in this outpatient clinic are funded by the National Council for Scientific and Technological Development (CNPq). This study was also funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001, Programa de Pós-Graduação em Medicina e Saúde, Faculdade de Medicina da Bahia, Universidade Federal da Bahia, Salvador, Bahia, Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
This study was approved by the Ethics Committee of the Professor Edgard Santos University Hospital, Federal University of Bahia, Salvador-BA, Brazil. All participants signed an Informed Consent before inclusion on the study (protocol 21/2011).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
dos Santos, D.N., Sá, K.N., Queirós, F.C. et al. Pain, psychoaffective symptoms, and quality of life in human T cell lymphotropic virus type 1 (HTLV-1): a cross-sectional study. J. Neurovirol. 27, 838–848 (2021). https://doi.org/10.1007/s13365-020-00914-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-020-00914-4