Abstract
The aim of the study was to describe the clinical and epidemiological characteristics of the central nervous system (CNS) infection by varicella zoster virus (VZV) in patients older than 65 years in a tertiary community hospital. We retrospectively analysed the results of cerebrospinal fluid (CSF) testing in patients older than 65 years between 2007 and 2014 with clinically suspected VZV infection with CNS involvement. Patients whose CSF samples were positive for VZV DNA were included, as were those with negative results who simultaneously presented herpes zoster and CSF or magnetic resonance imaging findings suggestive of CNS infection, and in whom other possible aetiologies had been ruled out. The study included 280 patients. The disease was considered to be caused by a VZV infection in 32 patients (11.4%), of which 23 cases were virologically confirmed (detection of VZV DNA in CSF). The most frequent diagnosis of the patients with VZV CNS infection was encephalitis (83.3%), followed by meningitis (13.3%) and cerebellitis (3.3%). The mean annual incidence of VZV CNS infection was 3.0 cases per 100,000 inhabitants. VZV was the most common cause of encephalitis and viral meningitis, ahead of herpes simplex virus (n = 9). At the time of discharge, 12 (40%) patients showed neurological sequelae. Five patients (20%) died during hospitalization, all with encephalitis. Patients with a fatal outcome had significantly higher median age and longer delay before initiating acyclovir. In conclusion, VZV was the first cause of encephalitis in our elderly population. Despite acyclovir treatment, there was a high rate of case fatality and sequelae at discharge.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Reactivation of varicella zoster virus (VZV) is a common event in patients with decreased VZV-specific cell-mediated immunity, mainly in the context of age-related immunosenescence and/or the presence of disease- or treatment-related immunosuppression. Herpes zoster (HZ) is the most common manifestation of VZV reactivation (Nagel and Gilden 2014), the estimated incidence rate ranging from 3 to 5/1000 person/years in North America, Europe and Asia-Pacific. Approximately 30% of the general population will develop this illness in their lifetime (Yawn et al. 2007). Studies conducted in different countries have reported that the incidence rate of HZ has increased in recent decades, before the introduction of the varicella vaccination program, but reasons for these increases are unknown (Kawai et al. 2014; Yawn and Gilden 2013).
The incidence of VZV reactivation increases with age, most cases occurring after 50 years of age (Nagel and Gilden 2014; Kawai et al. 2014; Yawn et al. 2013). Complications of VZV reactivation are also more frequent and severe with increasing age, giving rise to an increase in the associated hospitalization and mortality rates (Studahl et al. 2013). Moreover, VZV reactivations can cause a wide range of different peripheral and central nervous system (CNS) manifestations, whose incidence in the population have been poorly investigated, including encephalitis, meningitis, cerebellitis, polyradiculoneuritis, myelitis and vasculopathy, among others (Nagel and Gilden 2014; Grahn and Studahl 2015) .
The main purpose of this study was to estimate the incidence of VZV infection with CNS involvement in patients older than 65 years admitted to a tertiary hospital with clinical suspicion of neurological syndromes associated with VZV and to describe their main clinical presentation, complications and sequelae as well as mortality.
Material and methods
This retrospective study included patients 65 years old or older (≥65 years old) admitted to the tertiary hospital of Gipuzkoa (Hospital Universitario Donostia) between 2007 and 2014. Gipuzkoa is one of three provinces in the Basque Country (Spain), a region of nearly 700,000 inhabitants, of which around 132,000 are over 65 years (2011 Census, Basque Institute of Statistics). During the study period, the varicella vaccine was not on the immunization schedule in our region, but it has been recommended since 2008 for susceptible children older than 10 years of age. That is, the studied population had not received vaccination against varicella, except in the case of individuals found to be non-immune prior to being immunosuppressed as a part of pre-transplant protocols. None of the patients had received the vaccine against HZ (a live-attenuated VZV vaccine against HZ has been commercialized in Spain since September 2014).
Patients ≥65 years old for whom requests had been made for testing of cerebrospinal fluid (CSF) for VZV and/or herpes simplex virus (HSV) were identified using the computerized records of the Microbiology Laboratory of the Hospital Universitario Donostia, the only laboratory performing molecular testing in this province during the study period. In the laboratory, testing was routinely performed for both VZV and HSV types I and II when testing was requested for either of them. VZV and HSV I/II detection was carried out using commercial polymerase chain reaction (PCR) methods (VZ-DNA detection kit, Progenie Molecular, Valencia, Spain, and LightCycler HSV1/HSV2 Qual Kit, Roche, Manheim, Germany) after total nucleic acid extraction from CSF (NucliSENS® system easyMag, bioMerieux, Marcy-l’Etoile, France). Intrathecal antibodies for VZV and HSV were not determined in these study cases.
Medical records were reviewed, and data were gathered on the following: demographic information, clinical manifestations, immune status, results of laboratory tests and neuroimaging, treatments, complications and outcome. A case was defined as a patient with clinical or clinical-radiological suspicion of VZV nervous system illness and one of the following: (1) fever or history of fever or/and HZ with symptoms and/or signs of meningeal inflammation (suspicion of meningitis); (2) fever or history of fever or/and HZ with altered consciousness or signs of cerebral parenchymal involvement (suspicion of encephalitis); (3) seizure with results of neuroimaging suggestive of herpetic encephalitis (hypodense/hyperintense areas in the frontotemporal lobes in T2-weighted and fluid-attenuated inversion recovery magnetic resonance imaging [MRI]) (suspicion of encephalitis); (4) acute-subacute signs and symptoms of spinal cord involvement with no evidence of a compressive cord lesion (suspicion of myelitis); (5) mononeuropathy, plexopathy, multineuritis or polyradiculoneuritis (suspicion of peripheral nervous system involvement); (6) subacute cerebellar syndrome (suspicion of cerebellitis) or (7) multifocal neurological deficit, headache, altered consciousness or seizures with cerebral angiography demonstrating segmental arterial narrowing or multiple infarcts in multiple vascular territories (suspicion of vasculitis).
When VZV DNA was detected in the CSF of a suspected case-patient, the case was considered confirmed. On the other hand, a case was considered probable in a suspected case-patient if clinical suspicion occurred simultaneously or shortly after HZ, and there were abnormal findings in the CSF (white blood cell count ≥5 cells and/or protein level >40 mg/dl) and/or MRI results compatible with herpetic encephalitis, myelitis or vasculitis, but without laboratory confirmation of VZV infection (PCR negative), and after the exclusion of other possible aetiologies.
Immunosuppressed patients were individuals with immunosuppression resulting from disease (e.g. neoplastic diseases or HIV infection) or from immunosuppressive/cytotoxic therapy (e.g. corticosteroids, or medications used during cancer chemotherapy, organ transplantation, or to treat autoimmune disorders).
Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 18. Categorical variables were analysed using either chi-square or Fisher’s exact tests. The Mann-Whitney U test was used for comparing means. p Values ≤0.05 were considered statistically significant. The study was approved by the Ethics Committee of the Hospital Universitario Donostia.
Results
Patient characteristics and incidence of VZV infection with CNS involvement
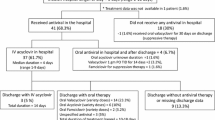
During the study period, CSF samples of 428 patients ≥65 years old were tested for VZV and HSV DNA. After reviewing their medical records, 280 patients met the criteria for clinical suspicion of VZV nervous system involvement, and in 32 (11.4%), the illness was considered to be the consequence of an infection by VZV. Twenty-three (8.2%) patients were classified as confirmed cases and nine (3.2%) as probable cases (Fig. 1). Patients with clinical suspicion of meningitis or encephalitis were the main group (n = 245, 87.5%), among which acute confusional state secondary to a systemic infection outside the nervous system (pneumonia, sepsis, etc.) was the most common aetiology (n = 74, 30.2%), followed by encephalitis caused by Herpesviridae, this accounting for more than half of the encephalitis cases (Fig. 2). VZV was the most common cause of viral encephalitis and meningitis, ahead of HSV (21 due to VZV vs 9 HSV PCR-positive cases of meningitis and encephalitis). Three cases of enterovirus infection were also diagnosed.
Patients with VZV CNS infection had a mean age of 79 years (range 65–95 years), with 22 (73%) being over the age of 75 years and 19 (63%) male. No clear seasonal pattern was found, with 12 patients being admitted in summer, 6 in winter, 5 in autumn and 7 in spring. One patient was immunosuppressed (stage 4 lung carcinoma). The average annual incidence of VZV CNS infections (confirmed and probable) during the period 2007–2014 was 3.0 cases per 100,000 inhabitants for the population over 65 years and 2.4 per 100,000 corresponding to cases of encephalitis. We observed a progressive increase in the requests for CSF testing for VZV over the study; nevertheless, the number of identified cases remained relatively stable (Table 1).
Clinical features
The primary diagnosis of the patients with VZV CNS infection were encephalitis (n = 25, 83.3%), meningitis (n = 4, 13.3%) and cerebellitis (n = 1, 3.3%). Two additional patients with CSF PCR positive for VZV, one with plexopathy and the other trigeminal HZ respectively, were not included in the analysis as these were not considered CNS manifestations. Patients with encephalitis had a higher median age than those with meningitis (80.3 ± 8.1 vs 69 ± 2.9 years; p = 0.019). Among the cases with encephalitis, 17 (68%) were confirmed cases with VZV DNA detected in the CSF by PCR, and 14 of them (82.4%) had HZ during their acute disease (Table 2).
The median CSF white blood cell count was 76.5 cells/μl (range 0–522), and the median protein level was 92 mg/dl (20–845). There was a dominance of lymphocytes in the CSF (median 95%; range 80–100%). Four patients had a normal CSF white blood cell count (<5 leucocytes/ml), two of them with elevated CSF protein levels. In three of these four patients, VZV DNA was detected in the CSF by PCR, and the fourth, with CSF PCR negative for VZV, was a patient who had started treatment with oral acyclovir a few days before CSF sample collection and the diagnosis was established based on MRI lesions and HZ. The characteristics of the eight patients with probable VZV encephalitis but no viral confirmation are shown in Table 3. Of these patients, four were being treated with oral valacyclovir because of HZ at the time of hospital admission.
All patients with VZV CNS infection underwent a cranial computed tomography scan (CT scan), and 20 (67%) underwent brain MRI. All CT scan images were found to be normal or showed abnormalities consistent with chronic lesions. Brain MRI findings were abnormal in five patients: three with abnormally high signal in the frontotemporal region, one with acute lacunar stroke and one with acute disseminated encephalomyelitis (ADEM).
All patients received intravenous acyclovir 10 mg/kg/8 h a day, except for two with renal impairment for whom the dose was reduced to 5 mg/kg/8 h. The median length of hospitalization until acyclovir therapy initiation was 1 day (range 1–6 days). Acyclovir was given for a period of 5–21 days (median 13 days) (14 days for cases of encephalitis, 8.5 days for meningitis and 21 days for cerebellitis). Steroids were used in five patients with encephalitis.
Complications during hospitalization
Systemic and neurological complications during hospital admission were common in encephalitis patients: infections (n = 8: 6 respiratory, and 2 urinary tract), alterations in fluid and electrolyte balance (n = 8; 6 hyponatremia, 2 hypokalemia), deterioration in level of consciousness (n = 7), seizures (n = 2) and transient ischemic attack (n = 1). Only one patient with meningitis in the rest of the group developed complications (respiratory infection). Two patients with encephalitis had other neurological manifestations related to VZV, one having polyneuropathy and the other myelitis with L5 radiculopathy. The median length of hospital stay of patients with VZV CNS infection was 13 days (range 4–46 days).
Outcome and mortality
At the time of discharge, 12 (40%) patients had neurological sequelae: cranial nerve involvement (n = 2), postherpetic neuralgia (n = 4), motor deficits (n = 1) and impaired physical mobility (n = 6). On discharge, 19 patients returned home (median hospital stay, 12 days) and 6 patients were transferred to a Convalescence Unit (median hospital stay, 18 days). All patients admitted to the Convalescence Unit returned home (mean Convalescence Unit stay, 37 days). Two months after discharge, one patient with encephalitis developed posterior uveitis due to VZV confirmed by PCR detection of viral DNA in the aqueous humour.
Five patients with encephalitis (20%), four of them men, died during hospitalization. Two other patients with encephalitis were admitted to the intensive care unit because of deterioration in their level of consciousness, but neither of them died. Patients with a fatal outcome had a significantly higher median age (88 years, 95% CI 82–96, vs 79 years, 95% CI 75–81; p = 0.009). The 65-year-old patient who died was considered an outlier as he had an underlying immunosuppressive condition and other debilitating comorbidities (stage 4 lung carcinoma discovered at necropsy, plus a history of bladder cancer, alcoholism and diabetes mellitus) that probably were more important determinants of the poor outcome, and he was excluded from the analysis. The median time to acyclovir initiation was significantly longer in patients who died than in survivors (3 days, 95% CI 0.8–5.5 vs 1 day, 95% CI 1–1.6, p = 0.007). We found no association between previous comorbidity and death.
Differences in the mortality rate between VHS and VZV encephalitis were not significant, although mortality was higher in the case of HSV-1 encephalitis (44.4% [4/9], p = 0.2).
Discussion
VZV reactivation represents a major health problem in the elderly. Over 90% of individuals aged at least 15 years are seropositive for VZV (Centers for Disease Control and Prevention, CDC, 1996). Hence, most adults are at potential risk of developing HZ. Moreover, considering the population is ageing rapidly, the incidence of HZ can be expected to increase (Kawai et al. 2014; Gil et al. 2004; Esteban-Vasallo et al. 2015). The decline in cell-mediated immunity due to immunosenescence, together with a higher incidence of comorbidities including disease- or treatment-related immunosuppression, makes this ageing population especially susceptible to VZV reactivation with more severe and disseminated disease, causing a significant health and economic burden (Blein et al. 2015). Nevertheless, few studies have investigated the incidence and clinical impact of CNS involvement due to VZV infection in elderly individuals.
According to most series, VZV is a common viral agent causing CNS infections in the adult population, usually ranking behind HSV (Parisi et al. 2016; Kadambari et al. 2014; de Ory et al. 2013; Mailles and Stahl 2009; Granerod et al. 2010). The dominant role of VZV in viral meningoencephalitis in elderly patients observed in our study highlights the importance of VZV-related CNS diseases with increasing age. The advanced age of the population included in the study and the simultaneous presence of HZ in many patients support the view that cases were mainly secondary to viral reactivation. Moreover, we found no significant outbreaks of VZV CNS involvement or consistent seasonal variation. Previously, it has been reported that 96.5% of hospitalizations due to VZV infection in people over 50 years of age in Spain occur as a result of VZV reactivation (Gil et al. 2004).
The frequency of the disease in our elderly patients was significant: the estimated annual incidence of VZV encephalitis in our cohort was 2.4 cases per 100,000 inhabitants (1.6 cases per 100,000 inhabitants considering just PCR-confirmed cases) which is higher than the incidence reported recently by Kadambari for England and Wales (0.65 cases per 100,000 inhabitants >65 years old) (Kadambari et al. 2014). The incidence of VZV infection with CNS involvement in adults has been poorly investigated. In Lugano (Switzerland), the incidence of VZV-related complications of the CNS was 1.0 case per 100,000 inhabitants older than 16 years for the period from 2003 to 2010 (Becerra et al. 2013). A higher rate (1.8 cases per 100,000) was observed in a study that included all age groups conducted in Gotland (Sweden) for the period from 1995 to 2006 (Persson et al. 2009). Both studies were based on VZV DNA detection in CSF for patient identification. Considering only PCR-confirmed cases, we found a similar incidence of VZV CNS infection among patients older than 65 years (2.1 cases per 100,000). Although there was a high rate of comorbidity, only one patient was immunosuppressed, reflecting the importance of natural age-related decline in cell-mediated immunity (Miller 1980; Burke et al. 1982).
Previous studies have shown that neurological complications of HZ can occur without skin lesions, such complications being observed in 38 to 69% of patients with no skin involvement (Pahud et al. 2011; Becerra et al. 2013; Persson et al. 2009; De Broucker et al. 2012). In our study, only 16.7% of patients had no signs of skin involvement. Hence, our data indicate that HZ occurring simultaneously or shortly after CNS neurological symptoms suggests causality in a high percentage of cases in the elderly. On the other hand, there were patients with HZ and neurological manifestations in whom CSF PCR was negative for VZV. In the eight patients with probable VZV encephalitis and no viral confirmation (PCR negative for VZV), the clinical syndrome in combination with skin involvement (the presence of an HZ rash) together with imaging and/or CSF findings supported the diagnosis and suggested a causative link. The negative PCR results may be related to a lack of sensitivity associated with early CSF sampling, as has been reported in the case of HSV, or to the administration of antiviral agent to treat HZ before CSF sampling (Weil et al. 2002). In patients with a high suspicion of VZV CNS infection and negative PCR result, detection of anti-VZV antibodies could help to establish the correct diagnosis, as in VZV vasculopathy, in which antibody detection has proven to be the best diagnostic test (Nagel et al. 2007).
Regarding patient outcome, previous studies have shown that a considerable percentage of patients with VZV CNS disease have persistent neurological sequelae (Persson et al. 2009; De Broucker et al. 2012). De Broucker et al. reported persistent neurological signs at discharge in 45% of patients and moderate-to-severe sequelae at 3 years in 41% of patients with VZV encephalitis (De Broucker et al. 2012). In agreement with these results, in our study, a high percentage of patients with encephalitis had neurological sequelae at discharge, confirming the severity of the infection. The case fatality of VZV encephalitis was also high (5 out of 25 patients died, 20%), this being higher than in previous studies (Persson et al. 2009; De Broucker et al. 2012). This higher mortality could reflect VZV producing more severe neuronal damage and astrogliosis in patients with encephalitis than in those with other types of VZV CNS disease. This view is supported by the findings of Grahn et al. that patients with encephalitis had more markedly elevated levels of light subunit neurofilament protein and glial fibrillary acidic protein in CSF; however, they found no significant correlation between clinical outcome or residual neurological sequelae and CSF biomarkers (Grahn et al. 2013).
Prognostic factors associated with poor outcome in VZV nervous system infections have been poorly studied. We identified two factors associated with mortality: advanced age and delay in the initiation of acyclovir treatment. A recent retrospective study of 98 patients with HSV and VZV CNS infections revealed a higher rate of adverse clinical outcomes (measured with the Glasgow Outcome Scale) in patients with comorbidities and an encephalitis presentation (Kaewpoowat et al. 2016). Studies attempting to investigate the relationship between viral load and the clinical course have produced contradictory results (Persson et al. 2009; Rottenstreich et al. 2014; Aberle et al. 2005).
In 2006, a live attenuated HZ vaccine received authorization in the USA and the European Union after the results of a study demonstrating a reduction in the incidence and severity of HZ in individuals over 60 years (Oxman et al. 2005). The vaccine showed 51.3% efficacy against HZ and 66.5% efficacy against postherpetic neuralgia. It is contraindicated for use in persons with immunosuppression. Recently, a randomized placebo-controlled trial with a subunit vaccine containing VZV glycoprotein demonstrated remarkable efficacy rates against HZ and postherpetic neuralgia of 89.8 and 88.8% respectively in adults ≥70 years of age (follow-up of 3.7 years) and that vaccine efficacy did not decrease with increasing age (Cunningham et al. 2016). The results with this vaccine are promising, and it can be hoped that use of such a vaccine will help to prevent VZV CNS complications and hospitalizations.
Our study is limited by the retrospective design. We were unable to obtain data to analyse certain relevant outcome-related factors such as neuropsychological sequelae and progress after discharge. Further, intrathecal antibody response against VZV was not measured, and this might have enabled us to detect additional cases.
In conclusion, VZV reactivation due to age-related immunosenescence in adults aged ≥65 years is a significant cause of CNS disease. VZV encephalitis is the first cause of encephalitis in the elderly population. Despite acyclovir treatment, the case fatality and sequelae at discharge are high. Treatment should be initiated immediately when there is clinical suspicion as it could prevent an unfavourable outcome.
References
Aberle SW, Aberle JH, Steininger C, Puchhammer-Stöckl E (2005) Quantitative real time PCR detection of varicella-zoster virus DNA in cerebrospinal fluid in patients with neurological disease. Med Microbiol Immunol 194:7–12
Becerra JC, Sieber R, Martinetti G, Costa ST, Meylan P, Bernasconi E (2013) Infection of the central nervous system caused by varicella zoster virus reactivation: a retrospective case series study. Int J Infect Dis 17:e529–e534
Blein C, Gavazzi G, Paccalin M, Baptiste C, Berrut G, Vainchtock A (2015) Burden of herpes zoster: the direct and comorbidity costs of herpes zoster events in hospitalized patients over 50 years in France. BMC Infect Dis 15:350
Burke BL, Steele RW, Beard OW, Wood JS, Cain TD, Marmer DJ (1982) Immune responses to varicella-zoster in the aged. Arch Intern Med 142:291–293
Centers for Disease Control and Prevention (CDC) (1996) Prevention of varicella. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 45:1–36
Cunningham AL, Lal H, Kovac M, Chlibek R, Hwang SJ, Díez-Domingo J et al (2016) Efficacy of the herpes zoster subunit vaccine in adults 70 years of age or older. N Engl J Med 375:1019–1032
De Broucker T, Mailles A, Chabrier S, Morand P (2012) Stahl JP; steering committee and investigators group. Acute varicella zoster encephalitis without evidence of primary vasculopathy in a case-series of 20 patients. Clin Microbiol Infect 18:808–819
de Ory F, Avellón A, Echevarría JE, Sánchez-Seco MP, Trallero G, Cabrerizo M et al (2013) Viral infections of the central nervous system in Spain: a prospective study. J Med Virol 85:554–562
Esteban-Vasallo MD, Domínguez-Berjón MF, Gil-Prieto R, Astray-Mochales J, Gil de Miguel Á (2015) Temporal trends in herpes zoster-related hospitalizations in Madrid (Spain), 2003-2013. J Infect 71:85–92
Gil A, San-Martín M, Carrasco P, González A (2004) Epidemiology of severe varicella-zoster virus infection in Spain. Vaccine 22:3947–3951
Grahn A, Studahl M (2015) Varicella-zoster virus infections of the central nervous system—prognosis, diagnostics and treatment. J Infect 71:281–293
Grahn A, Hagberg L, Nilsson S, Blennow K, Zetterberg H, Studahl M (2013) Cerebrospinal fluid biomarkers in patients with varicella-zoster virus CNS infections. J Neurol 260:1813–1821
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D et al (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 10:835–844
Kadambari S, Okike I, Ribeiro S, Ramsay ME, Heath PT, Sharland M et al (2014) Seven-fold increase in viral meningo-encephalitis reports in England and Wales during 2004-2013. J Infect. 69:326–332
Kaewpoowat Q, Salazar L, Aguilera E, Wootton SH, Hasbun R (2016) Herpes simplex and varicella zoster CNS infections: clinical presentations, treatments and outcomes. Infection 44:337–345
Kawai K, Gebremeskel BG, Acosta CJ (2014) Systematic review of incidence and complications of herpes zoster: towards a global perspective. BMJ Open 4(6):e004833
Mailles A, Stahl JP (2009) Steering Committee and Investigators Group. Infectious encephalitis in France in 2007: a national prospective study. Clin Infect Dis 49:1838–1847
Miller AE (1980) Selective decline in cellular immune response to varicella-zoster in the elderly. Neurology 30:582–587
Nagel MA, Gilden D (2014) Neurological complications of varicella zoster virus reactivation. Curr Opin Neurol 27:356–360
Nagel MA, Forghani B, Mahalingam R, Wellish MC, Cohrs RJ, Russman AN et al (2007) The value of detecting anti-VZV IgG antibody in CSF to diagnose VZV vasculopathy. Neurology 68:1069–1073
Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD et al (2005) A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults. N Engl J Med 352:2271–2284
Pahud BA, Glaser CA, Dekker CL, Arvin AM, Schmid DS (2011) Varicella zoster disease of the central nervous system: epidemiological, clinical, and laboratory features 10 years after the introduction of the varicella vaccine. J Infect Dis 203:316–323
Parisi SG, Basso M, Del Vecchio C, Andreis S, Franchin E, Dal Bello F et al (2016) Viral infections of the central nervous system in elderly patients: a retrospective study. Int J Infect Dis 44:8–10
Persson A, Bergström T, Lindh M, Namvar L, Studahl M (2009) Varicella-zoster virus CNS disease—viral load, clinical manifestations and sequels. J Clin Virol 46:249–253
Rottenstreich A, Oz ZK, Oren I (2014) Association between viral load of varicella zoster virus in cerebrospinal fluid and the clinical course of central nervous system infection. Diagn Microbiol Infect Dis 79:174–177
Studahl M, Petzold M, Cassel T (2013) Disease burden of herpes zoster in Sweden—predominance in the elderly and in women—a register based study. BMC Infect Dis 13:586
Weil AA, Glaser CA, Amad Z, Forghani B (2002) Patients with suspected herpes simplex encephalitis: rethinking an initial negative polymersae chain reaction result. Clin Infect Dis 34:1154–1157
Yawn BP, Gilden D (2013) The global epidemiology of herpes zoster. Neurology 81:928–930
Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, Sy LS (2007) A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 82:1341–1349
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Ethics Committee of the Hospital Universitario Donostia.
Conflict of interest
All authors declare that they have no conflict of interest.
Funding
No funding was received to perform this study.
Rights and permissions
About this article
Cite this article
Arruti, M., Piñeiro, L., Salicio, Y. et al. Incidence of varicella zoster virus infections of the central nervous system in the elderly: a large tertiary hospital-based series (2007–2014). J. Neurovirol. 23, 451–459 (2017). https://doi.org/10.1007/s13365-017-0519-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-017-0519-y