Abstract
There is a curious case in Alveolar macrophages (AM), the frontline defence recruits that contain the spread of all intruding bacteria. In response to Mycobacterium tuberculosis (M.tb), AM either contain the spread or are modulated by M.tb to create a region for their replication. The M.tb containing granulomas so formed are organised structures with confined boundaries. The limited availability of drugs inside AM aid drug tolerance and poor therapeutic outcomes in diseases like tuberculosis. The present work proves the glycotargeting efficiency of levofloxacin (LVF) to AM. The optimised formulation developed displayed good safety with 2% hemolysis and a viability of 61.14% on J774A.1 cells. The physicochemical characterisations such as Fourier-transform infrared spectroscopy (FTIR), X-ray diffraction (XRD), differential scanning calorimetry (DSC) and thermogravimetric analysis (TGA) proved that carubinose linkage was accomplished and LVF is entrapped inside carubinose-linked hybrid formulation (CHF) and hybrid formulation (HF) in amorphous form. The transmission electron microscopy (TEM) images revealed a core–shell structure of HF. The particle size of 471.5 nm estimated through dynamic light scattering (DLS) is enough to achieve active and passive targeting to AM. The nanoparticle tracking analysis (NTA) data revealed that the diluted samples were free from aggregates. Fluorescence-activated cell sorting (FACS) data exhibited excellent uptake via CHF (15 times) and HF(3 times) with reference to plain fluorescein isothiocyanate (FITC). The pharmacokinetic studies revealed that CHF and HF release the entrapped moiety LVF in a controlled manner over 72 h. The stability studies indicated that the modified formulation remains stable over 6 months at 5 ± 3℃. Hence, hybrid systems can be efficiently modified via carubinose to target AM via the parenteral route.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB) is the frontrunner in the infectious disease group. It possessed the highest mortality rate in 2019, with 1.4 million deaths and 10 million new cases. Mycobacterium tuberculosis (M.tb), a bacillus spread from an infected individual with active TB during coughing, is the leading cause of tuberculosis. About 1/4th of the world’s population is affected by it. It can be pulmonary or extrapulmonary. BCG, the only vaccine for TB, was discovered 100 years ago [1]. Search for an effective drug to overcome the side effects (of existing medications) and improve efficiency is still on. 1/4th population is still affected by TB and research is ongoing makes up a solid ground for further investigations. The severity of the situation is evident because a disease with a vaccine in place and a standard dosage regimen retains top mortality rates year after year. Pulmonary TB occurs when the lungs are afflicted by M.tb.
Alveolar macrophages (AM) form the first line of defence for all incoming particulate matter through the nasal route and, in process, clears them through phagocytosis. AM, the prominent warriors of the body’s defence mechanism, are transformed to harbour the bacteria or promote pro-inflammatory milieu in the lungs leading to progression of inflammatory diseases like chronic obstructive pulmonary disease (COPD) and communicable diseases such as tuberculosis [2, 3]. As in latent and active TB cases, the bacillus resides under a controlled environment in AM [4].
AM phagocytose pathogenic agents and airborne particles acing the primary defence. They produce interleukins avoiding inflammation when subjected to harmless antigens, which affect homeostasis in the lungs. AM mediate inflammatory responses by encouraging the release of reactive oxygen species (ROS) and inflammatory mediators, including neutrophil staffing in the alveolus. During active inflammation, macrophages possess high phagocytic movement and there is an increased recruitment of antigens on its surface [5]. The granuloma so formed harbours M.tb until dysregulation of immune response occurs. It leads to further reactivation of the latent M.tb leading to the progression of the disease. Alveolar macrophages have surface receptors that identify glycoconjugation with carubinose residues and an increased binding affinity i.e. binding with a specific carbohydrate followed by its receptor-mediated internalisation. Carubinose shares the same pathway of internalisation via AM as that of M.tb [6].
Levofloxacin (LVF), a broad-spectrum antibiotic that belongs to the Quinolone group, is useful in bacterial infections. It is a valuable drug in respiratory infections, MDR-TB, diseases caused by gram-negative bacteria, gastrointestinal (GI) tract infections, typhoid and septicaemia. It is a DNA gyrase inhibitor [7,8,9,10,11]. Delivering the minimum inhibitory concentration (MIC) of antitubercular drugs to the site of infection is a challenge. Several approaches to improve targeted delivery to the lungs, such as inhalation and oral and systemic delivery, have achieved feat at different levels [4, 12,13,14,15,16,17]. Nanoformulations are nowadays in vogue for delivering antibiotics to the site of infection.
Glycotargeting approach comprises specific molecular signatures articulated over the cell surface which interacts with ligands (e.g. lactose, carubinose, fructose, galactose). Carubinose is the most common ligand in surface decoration [2, 18,19,20,21,22,23,24]. AM express C-type carbohydrate recognition domains (CRD)on cell surface. It can easily recognise thyrotropin and lutropin alongside D-mannose (carubinose), N-acetylglucosamine and L-fucose residues. CRD quickly checks lipoarabinomannan that leads to phagocytosis of bacilli inside macrophage and inhibition of phagosome-lysosome fusion enables bacterial survival within AM. Inhibition of the intracellular survival of M.tb can be furnished by M1 macrophage activation [18, 22, 25].
When administered, a hybrid formulation has dual functionality since it encompasses the benefits of two types of material, a polymer and a lipid. Lipid–polymer systems are core–shell structures comprising both polymer and lipid and imbibe the physical stability and biocompatibility of both ingredients. PLGA (poly-lactic-co-glycolic acid), a generally recognised as safe (GRAS) polymer, is used significantly in different submissions and encapsulating a wide array of therapeutic agents such as vaccines, nucleic acids, proteins, anticancer drugs and immunomodulators. Besides being a biocompatible, biodegradable, versatile and a tuneable polymer, PLGA comes with its set of limitations when it encounters lipophilic drugs and shows poor loading, burst release, easily phagocytosed and uncontrolled tissue distribution. The introduction of lipid can overcome these limitations of the PLGA formulations. The lipid, in this case, provides a coating in the case of polymer core and lipid coat formulations. The core-coat structure provides relief from burst release and increases the stability of the formulation to hydrolytic degradation, thereby achieving controlled release [26,27,28,29,30]. Significantly, the hybrid nanoformulations have recently demonstrated better in vivo cell uptake vis-a-vis polymeric nanoparticles and liposomes. To avert drug escape and improve upon the stability of the system, encapsulation of drugs into hybrid systems (HS) can be undertaken. The HS minimises toxicity and prolongs drug release with desired biological features. Site-specificity can be achieved by further surface modifications [31]. The age-old technique of two-step synthesis of HS is now overtaken by one-step synthesis characterised by good understanding of material properties and drug characteristics. The one-step synthesis also achieves the advantage of better reproducibility as well as stability as the formulation is self-assembled and achieves better dynamic stability [30].
The current work focused on developing carubinose functionalised hybrid systems to deliver the levofloxacin payload to alveolar macrophage. The successful delivery of levofloxacin to AM will enable the intracellular killing of M.tb more efficiently than ever and lead to dose reduction and higher patient compliance.
Materials and method
Materials
Purasorb PDLG 5010 (PLGA) and Phospholipon90G (Soy lecithin) were procured as free samples from Corbion Biomaterials, Holland and Lipoid, Germany, correspondingly. Levofloxacin was received as a gift from Sun Pharma; carubinose (D-mannose) was purchased from HiMedia laboratories. Milli Q water from Millipore (Bedford, USA) in the research facility was used throughout for RP-HPLC quantifications. Chromatographic grade solvents were used in RP-HPLC studies. Analytical grade chemicals and reagents from Merck Germany were used throughout the study.
Methods
Experimental design and optimisation
Preliminary investigations were done to select the factors and levels for ideal application of Box-Behnken design. A 17 run no block quadratic response surface design was generated with the help of Design-Expert (Design-Expert software, trial version 11.0). The dependent factors selected for the study were PVA(%), PLGA(%) and soya lecithin(%), and the outcome on particle size, zeta potential and entrapment was estimated (Supplementary Table 1). To formulate HF and CHF, a particle size range of 300–400 nm was ideal along with maximum entrapment and zeta potential. To validate the design space generated data, the confirmatory formulation was prepared in triplicate and matched with the predicted response. The optimisation was carried out through one-way analysis of variance (ANOVA), and model reduction was carried out wherever necessary to keep the adjusted and predicted R2 values within range and to obtain a good s/n ratio [27, 32].
Formulation of hybrid formulation
The hybrid formulation (HF) was prepared according to Zheng et al. [33]. Briefly, soya lecithin, PLGA and levofloxacin were dissolved in dichloromethane in separate beakers. The lipid phase and the polymeric solution containing levofloxacin was added to the aqueous phase (PVA solution) under continuous stirring followed by sonication (probe sonication for 5 min leaving rest of 2 min amidst each cycle of sonication). The solution was stirred for 24 h till. HF was centrifugated at 10,000 rpm for 30 min. The HF was collected precisely, washed with double-distilled water (DDW) and then lyophilised and stored in a desiccator [29, 31, 33]. Carubinose coating was done as per Saraogi et al. [34]. Sodium acetate buffer (pH 4.0) was utilised as a medium to accomplish the ring-opening of carubinose. The carubinose containing buffer solution is eventually mixed with lyophilised formulation and kept at room temperature for 48 h under stirring at 600 rpm. It was further concentrated under vacuum at 70 °C. Carubinose-linked hybrid formulation (CHF) was purified and unreacted carubinose is removed by dialysing against DDW in a dialysis tube (MWCO 12–14 kDa, HiMedia, Mumbai, India) for 24 h. The formulation was further lyophilised for storage and characterisation [34].
Particle size and zeta potential characterisation
The particle size and surface characterisations of formulations were carried out on zeta/nanoparticle analyser -Nanoplus. All the measurements were done in triplicate. The samples were suitably diluted with DDW in a ratio of 1:10 (Formulation: DDW) [35].
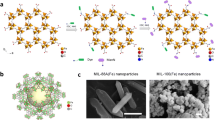
Particle morphology by SEM and TEM
Scanning electron microscopy (SEM) (JSM-6490LV, JEOL, Japan) studies were done to assess the morphology of HF and CHF. For SEM, well-dispersed powdered samples were stuck upon carbon tape placed on a metal disc and further coated with 80 nm gold/palladium in Blazers 120B sputtering device. The mounted samples were examined [36]. The transmission electron microscopy was carried out on JEOL 1230 TEM fitted with GATAN ORIUS CCD camera. Briefly, the samples were dispersed in ethanol and positioned on a copper grid and dried at room temperature. The dried grid was loaded on the sample holder and visualised [37, 38].
Nanoparticle tracking analysis (NTA)
NTA analyses were carried out on reconstituted HF and CHF powders. The samples were reconstituted in DDW at 1% w/v concentration. The samples were subjected to hydrodynamic diameter measurement and concentration estimation in terms of particles/ml. The instrument measures the concentration and size of nanoparticles while they are under Brownian motion. The samples were kept at ambient conditions throughout the study. The samples were further diluted during analysis at a 10−2 concentration. A green laser with sCMOS camera was used in the study [39].
Fourier-transform infrared spectroscopy (FTIR)
To verify the structure of the LVF and to study its interaction with the components, FTIR spectroscopy was performed. The samples LVF, HF, CHF, PLGA and soya lecithin were assorted individually with potassium bromide (KBr) and constrained (1 ton applied pressure) into pellets. All the steps were done under humidity-controlled conditions to curtail the risk of moisture contamination [40].
Differential scanning calorimetry (DSC) and thermo gravimetric analysis
Thermal properties were examined using TA instruments SDT Q600 V 20.9 simultaneous DSC-TGA analyser. The product was weighed prior to analysis and placed in a platinum pan—the heating rate of 5 ºC min−1 was employed in the range of 25 to 300 °C. Instantaneous weight is used in heat flow calculations which is dynamically normalised at a given temperature [41].
Powder X-ray diffraction (XRD)
Diffractograms for LVF, HF and CHF were obtained from Rigaku, Miniflex 600 X-ray diffractometer with a Cu anode material (wavelength-1.54Å). XRD studies were done at 40 kV voltage under continuous scan, over a 2θ range of 2–90° with a step size of 0.02 [42].
Entrapment efficiency (%EE)
The formulations were reconstituted in DDW and subjected to centrifugation of 5000 rpm for 30 min thrice. The supernatant was analysed for the presence of the free drug by RP-HPLC Shimadzu (Shimadzu Corporation, Japan). 100 mM ammonium acetate buffer (mobile phase A) and 1:1 mix of acetonitrile and methanol (mobile phase B). Binary gradient mode at 35% B was utilised at an overall flow rate of 0.93 ml/min for 6 min run time. An injection volume of 25 µl and detection wavelength set at 295 nm was set for the detector. The oven was maintained at 30 °C, and the samples were kept at ambient conditions. The samples were analysed in triplicate, and the %EE was deliberated by the following formula [43].
Drug loading
The lyophilised samples of HF and CHF were weighed and suspended in alkaline SDS (5%w/v sodium dodecyl sulphate in 0.1 M NaOH) at 60° C to hasten the hydrolysis of PLGA. The suspension was centrifuged and the supernatant was evaluated for drug loading by RP-HPLC. Each supernatant was analysed thrice [43]. The following equation calculated drug loading.
Drug release
HF and CHF were suspended in phosphate-buffered system 7.4 (PBS) and were placed in preactivated dialysis bags (MWCO 12–14 kDa; HiMedia, Mumbai, India). The bags were immersed in PBS (25 ml) at 30 °C. One hundred–microlitre samples were reserved at varying time points and were replaced with 100 µl of PBS to uphold sink conditions. The samples were further diluted and analysed through RP-HPLC. The prepared formulation showed extended release up to 72 h. Different kinetic models were used via DD solver to assess the release kinetics of HF and CHF [16].
Haemolysis
Blood samples were collected from healthy Wistar rats in EDTA-lined tubes. These were then centrifuged for 10 min at 3000 rpm; the separated plasma was collected and the solid RBCs were washed with PBS 4–5 times or until the supernatant became clear. The supernatant was discarded, and the hematocrit diluted ten times with PBS making it a 10% hematocrit solution.
The test samples were prepared in PBS solution and the hematocrit solution was added to it. It was kept for some time and then centrifuged, the supernatant was placed in a 96-well plate, absorbance measured at 540 and 570 nm. % Haemolysis was calculated. All the experiments were done in triplicate [44, 45].
Macrophage targeting
Viability assay
A sterile 96-well plate was seeded with the cell suspension of J774A.1 cell culture from the reservoir with mild shaking and sited in an incubator at 37 °C and 5% CO2 for 24–48 h. The old media was cast off, and the wells were washed thrice with PBS. The samples to be checked for viability were added (1.563 ppm–100 ppm), and the wells were replenished with complete RPMI media. The plates were set aside in an incubator at 37 °C and 5% CO2 for 24 h. The media was cast off from 96-well plates and washed with PBS. 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) solution (0.5 mg/ml) was added and incubated for 1–2 h. The MTT solution was then discarded and DMSO was added to the plates to terminate the reaction. The plates were placed for mild shaking for 15–20 min, and the absorbance measured at 570 nm. MTT assay was done in triplicate [46].
Quantitative cell uptake
J774A.1 cell culture was incubated with LVF, HF and CHF in complete RPMI medium at 37 °C and 5% CO2 for 6 h. After incubation, the supernatant media was collected and processed for estimation of free extracellular LVF in it. For intracellular LVF content, cells were scrapped with the help of a sterile cell scraper and transferred to well-labelled microcentrifuge tubes (MCT), washed with PBS; furthermore, 100 µl of 1X lysis buffer was added. They were then rapidly freeze-thawed twice and sonicated to rupture the cells. The samples were then centrifuged and the supernatant (cell lysate) was processed via RP-HPLC [47].
Fluorescence-activated cell sorter (FACS) analysis
FITC-tagged formulations of HF and CHF were prepared as described earlier. LVF was replaced by FITC during formulation. Flow cytometry studies were carried out on J774A.1 cell culture. They were harvested in their logarithmic growth phase and plated on a 6-well plate. FITC-labelled formulations were then added to the plates after 24 h of growth and placed in 37 °C and 5% CO2 for the next 6 h. After the stipulated time, the cells were washed with PBS twice and were scrapped. Four hundred microlitres of PBS was further added to it and the cells were transferred to fluorescence-activated cell sorter ( FACS) tubes for further analysis. Cell uptake was studied by BD FACS Aria, Heidelberg, Germany, at λEX 480 nm and λEM 520 nm [48].
Fluorescence microscopy
J774A.1 cells were used for the study. The cells were harvested for 24–48 h till they reach the logarithmic growth phase. FITC-tagged formulations HF and CHF were added to the 6-well plate and placed in 37 °C and 5% CO2 for 6 h. The plates were then taken out and washed twice with PBS. Diluted DAPI solution was added to the wells to submerge the cells completely. The plates were incubated for another 10 min. The sample was rinsed thrice with PBS, mounted and viewed under a fluorescence microscope.
In vivo studies
Wistar rats were procured from IVRI Bareilly under the approval number BBDNIIT/IAEC/2019/01. The animals were acclimatised for 15 days prior to the study and were fed standard chow and water ad libitum. The animals were kept on a 12 h light and dark cycle. Before the study, they were randomly divided into 4 treatment groups (LVF, HF, CHF and control) with 5 animals each. Rats were fasted overnight before treatment. They were administered the prepared formulations and standard drug according to their weight (20 mg/kg body weight i.v. LVF). The control group was administered normal saline. Blood samples were withdrawn through retro-orbital venous plexus puncture by capillary tubes at different time points and kept for pharmacokinetic studies. Clinical signs (food intake, faeces, hair and behaviour of rat) were observed on a daily basis.
Pharmacokinetics
The plasma samples were deproteinated with the help of acetonitrile and methanol. Vortexing was done for 5 min and centrifuged at 13,500 rpm for 30 min. The clear supernatant obtained was separated and dried in an N2 evaporator. The dried product was reconstituted using the diluent (acetonitrile: methanol). The prepared samples were clarified by passing through 0.22 µm syringe filters and examined through RP-HPLC [43].
Stability studies
The stability study of CHF was carried out as per International Conference on Harmonization (ICH) Q1A (R2) guidelines for 6 months [49]. Stability studies were done to assess the shelf life of the formulation as well as to ensure the best storage condition for the formulation for extended periods. CHF and HF were kept at 5 ± 3 °C. The samples were evaluated for particle size, zeta potential and drug loading after three months and 6 months [35, 43].
Statistical design
Design-Expert, Version 11, Stat-Ease Inc., Minneapolis, MN, USA, was utilised for response surface design and related ANOVA. BBD was chosen as a response surface design, which created 17 formulations. Graph Pad Prism 8 software was used for statistical analyses. OriginPro 2020b Learning edition was used for XRD and IR data analysis. All the data are presented in triplicate (n = 3). DD solver and PK solver were utilised for dissolution kinetics and pharmacokinetic profiling, respectively.
Results
Formulation of hybrid formulation
The results obtained for the randomised response surface design were used to optimise HF. A quadratic model was developed with 17 runs and no blocks. Throughout the design evaluation procedure, it was ensured that the lack of fit was insignificant; the difference between adjusted and predicted R2 values was not more than 0.2. Adequate precision values remained > 4 for all three dependent variables to ensure a good signal-to-noise ratio. Model reduction was done as necessary. The inference drawn from the Design-Expert values indicates that for particle size PVA (p value = < 0.001) and soya lecithin (p value = 0.0108) play a significant role along with the quadratic factors of soya lecithin (p = 0.0044) and PLGA (p = 0.0034. For zeta potential (reduced linear model), soya lecithin (p = 0.0070) was significant, and for entrapment efficiency, PLGA (p = < 0.0001) and soya lecithin (B2 p = 0.0010) are significant (Fig. 1). The design results were tabulated in the form of equations with coded values. As evident from the equations and design graphs, the constraints set up for optimisation yielded a set of 100 solutions. The topmost solution was selected as the optimised formulation. It can be concluded from the data obtained that the size of nanoparticles is controlled linearly by PVA and soya lecithin and quadratically by soya lecithin and PLGA. The coded equation for particle size, zeta potential and entrapment efficiency are as follows. A, B and C refer to PVA, soya lecithin and PLGA, respectively.
The surface modification was done on optimised formulation and CHF was collected. The particle size of CHF was slightly more than that of HF due to absorption of carubinose to HF through chemical linkages of the amine group of soya lecithin and the hydroxyl group of open chain carubinose. The zeta potential and EE values for HF were − 11.29 mV and 61% and for CHF were 1.21 mV and 56%, respectively (Fig. 2).
Shape and surface morphology
The particle size and shape of HF and CHF were investigated through SEM and TEM. SEM was used to assess the surface of the nanoparticles. It exhibited nanoparticles with smooth, somewhat spherical particles. The TEM images are clear to the extent that the layers are visible in the core–shell structure of HF and CHF; in CHF, a separate coating layer can also be visualised. There was a trivial increase in particle size of the CHF when compared to that of HF (Fig. 3) [50].
Nanoparticle tracking analysis (NTA)
NTA analysis was carried out on reconstituted HF and CHF powders. The mode values of NTA data were considered, which exhibit that the particle size of diluted samples was 137.2 nm and 222.8 nm for HF and CHF, respectively. The intensity distribution graph depicts that the sample consisted of discrete particles and aggregates were absent, indicating good reconstitution properties. The intensity graph also illustrates the variance in the size distribution of the two samples (Fig. 4).
Entrapment efficiency
Entrapment efficiency (%EE) was part of the optimisation criteria based on the design of experiments. The %EE was found to be in the range of 20.65–64.36%, respectively. The decrease in entrapment can be attributed to several washings before lyophilisation and carubinose-linkage, which required overnight stirring. The results are given in Supp Table 1.
Drug loading
Drug loading of the optimised formulation was calculated by the formula as mentioned in “Drug loading.” HF contained 21% LVF, whereas CHF had 15% LVF loading.
In vitro release studies
The in vitro release studies were carried out in PBS for 72 h. The dissolution profiles of HF and CHF are given in Fig. 5. As levofloxacin is a stable drug and has good permeability, the initial spike in drug release can be owed to the free drug present on the surface of the formulation. The release profiles show that the HF as compared to CHF shows a higher burst release and then a slow release similar to that of CHF. The CHF initially has a lesser burst release of LVF due to several washings and an increased particle size owing to adsorption of carubinose to the surface leading to slow and sustained release. The extra coating of carubinose applied to HF also hampers the surface wetting property of the nanoparticle. The formulations’ release profiles did not vary significantly as the in vitro properties are least affected by the presence or absence of a surface modifier [51, 52]. The presence of surface functionalisation affects its targeting ability, not the release character.
Kinetic modelling
Diverse kinetic models were applied to the drug release profile to categorise the release phenomenon. As per the fitting criteria, the highest correlation coefficient (R2) value corresponds to the best fit kinetic model describing the kinetics as per Table 1 [51].
Infrared spectrum
Soya lecithin gives a signal of symmetric CH2 at 2856 cm−1, asymmetric CH2 at 2926 cm−1 and CH3 stretch at 2971 cm−1, a –C = O stretch at 1711 cm−1 while PLGA shows the signals corresponding to –CH, –CH2, –CH3 stretching 2845–3000 cm−1, carbonyl –C = O stretching 1709 cm−1, C–O stretching 1054–1250 cm−1 and –OH stretching 3596, 3526, 3412 ca. 3000, 2759 cm−1, which were broad. Levofloxacin gives characteristic signals for carboxyl groups at 1723.6 cm−1 and conjugated carbonyl group at 1620 cm−1, and 1292 cm−1 C-O acid group. The soya lecithin linked with carubinose and PLGA hybrid with levofloxacin indicates the presence of linked carubinose with soya lecithin due to the presence of a broadband of OH group from 3756 to 2400 cm−1, the signals of NH overlapped with the OH signal of carubinose. The levofloxacin conjugated carbonyl group slightly shifted to 1623 cm−1 whereas the acid COOH group is shifted to 1756 cm−1, Indicating a strong bond formation with the hybrid formulation (Fig. 6) [16, 53]. The absence of determinate peaks of levofloxacin indicates its encapsulation within the HF and CHF and dispersion of LVF in the formulation, which is further correlated through XRD, DSC and TGA studies.
DSC and TGA
The thermal characterisation of LVF, HF and CHF was analysed and results have been shown in Fig. 7, which illustrated that the TGA curve consisted of the following stages. The first initial weight loss ∆W = 17.56% for CHF was observed in the temperature range of 25.75 to 84.23 °C; for LVF, the first initial significant weight loss ∆W = 3.505% was observed in the temperature range of 24.52 to 80.06 °C; this region can be sub-categorised in two regions with insignificant losses of 0.91% and 0.45% at 36.96 °C and 50.58 °C respectively. For HF, the first initial weight loss ∆W = 9.59% was observed in the temperature range of 25.07 to 70.87 °C.
The second weight loss ∆W = 21.63% can be seen in the temperature range of 84.23 to 224.12 °C; for HF and LVF, it was 24.99% and 4.351%, respectively. The third weight loss of ∆W = 14.72% for CHF starts at 224.12 °C. For LVF, the thermal degradation started at the temperature range 244.15 °C and beyond with significant weight loss. For HF, the third stage of ∆W = 16.73% begun at 217.86 °C and beyond. The DSC graph plotted shows an initial small endothermic region upto 70 °C with a 209.9 J/g energy in accordance with the TGA data and no melting peak of pure drug can be seen. Similarly, for HF, the DSC graph plotted shows an initial small endothermic region corresponding to glass transition of PLGA upto 70 °C with a 312.2 J/g. As for LVF, the DSC graph plotted shows 2 small endothermic regions upto 100 °C and a sharp melting peak of the pure drug at 232.77 °C. The melting peak is further characterised by 56.31 J/g heat of fusion.
X-ray diffraction
The XRD data obtained from the instrument was processed and plotted on OriginPro 2020b, Learning edition. XY graph was plotted and smoothing was done to remove the irregularities and the noise signals. The Savitzky-Golay method with 25 points window and first-order polynomial were undertaken. The noise corrected data was further processed for baseline correction. The baseline was subtracted using asymmetric least square smoothing. Furthermore, peak detection was carried out, and peaks less than 20% of height were rejected. The selected gaussian peaks were labelled for the study Fig. 8. The obtained data was matched with the pre-existing patent literature of levofloxacin physical parameters to identify crystalline and amorphous states [54]. The analytical records reveal (Supp Table 2) that pure levofloxacin hemihydrate exists in crystalline form. It is converted to an amorphous state during formulation, which is cross-matched with the patented and various other experimental literature available in the public domain.
Haemolysis
Hemolytic behaviour is dose-dependent, as is evident from the results; the increasing concentrations correspond to higher haemolysis. Triton X was used to mark complete haemolysis and PBS as a negative control for the study [55]. After 6 h of study, the results indicate the low hemolytic potential of CHF compared to HF and LVF at varying concentrations (12.5–200 ppm). A two-way ANOVA followed by Dunnett’s multiple comparison was done to estimate the level of significance (Fig. 9).
Percent haemolysis plot for LVF, HF and CHF (12.5 ppm (LVF vs. HF *p = 0.0126, LVF vs. CHF *p = 0.0104); 25 ppm (LVF vs. HF **p = 0.0067, LVF vs. CHF **p = 0.0074); 50 ppm (LVF vs. HF ***p = 0.0002, LVF vs. CHF ***p = 0.0001); 100 ppm (LVF vs. HF **p = 0.0025, LVF vs. CHF **p = 0.0012); 200 ppm (LVF vs. HF ****p = < 0.0001LVF vs. CHF ****p = < 0.0001)
Macrophage targeting
Cell line studies (MTT assay)
Viability studies were carried out on J774A.1 cells. MTT assay was utilised for this assessment. The results indicated a downward trend in viability with increasing concentrations of LVF, HF and CHF. The viability of the cells decreases with increasing concentrations of LVF. CHF (61.14%) and HF (56.07%) were seen to possess better viability than LVF (51.47%) at 50 ppm. At 100 ppm, the viability of the cells fell below 50% for LVF, HF and CHF (Fig. 10).
Quantitative cell uptake
The cell uptake studies indicate higher uptake of carubinose-linked formulation (CHF) as compared to that of HF and LVF and follow the order CHF > HF > LVF. The mean values are 0.12 μg/103 cells for LVF, 0.27 μg/103 cells for HF and 0.58 μg/103 cells for CHF (Fig. 11).
Fluorescence-activated cell sorter (FACS) analysis
FACS data further strengthened the hypothesis that carubinose functionalised HS are readily uptaken by the macrophages. The quantitation of the FITC values are as follows: FITC (119.07), HF (309.96) and for CHF (1512.72). The fifteen times increase in CHF uptake and three times in HF compared to that of FITC is proof of functionalisation of CHF and passive uptake of HF (Fig. 12a, b).
Fluorescence microscopy
Fluorescence microscopy data qualitatively proves that CHF was internalised more as compared to HF. The qualitative data demonstrates the efficacy of carubinose linkage and hence affirms that surface modification improves the internalisation of the formulation (Fig. 12c).
In vivo pharmacokinetics
The pharmacokinetics of LVF, HF and CHF were through intravenous injection of the test samples and frequent sampling through retro-orbital route for 72 h. The collected samples were analysed through the RP-HPLC method developed for the same. The blood samples were collected in heparin-coated tubes. The samples were centrifuged to separate the plasma. Plasma was stored at −20℃ for analysis. The pharmacokinetic data obtained was processed on a PK solver and is presented in Table 2. The pharmacokinetic data showed that the half-life was increased to the ratio of 7X and 9X in the case of HF and CHF. The AUC values were double for CHF and HF when compared to LVF indicating their increased bioavailability. The AUMC for CHF, HF and LVF indicate that it is highest for CHF followed by HF and LVF. AUMC values are further used in the calculation of MRT which shows that CHF has the highest residence time followed by HF and LVF. The increased values for HF and CHF point to the fact that the formulation is a controlled release formulation that enhances the bioavailability of LVF and increases the residence time of drug in the body, which can lead to further dose reduction. The decreased clearance rates and increased volume of distribution also prove the efficacy of the system (Fig. 13).
Stability studies
Stability study data is tabulated below for particle size, zeta potential and percent drug loading of HF and CHF for 6 months at 5 ± 3 °C (Table 3).
Discussion
AM drug delivery encompasses drug targeting to infected organs via passive and active targeting, which is well documented. Mononuclear phagocyte system (MPS) and enhanced permeability and retention (EPR) effects are the two main mechanisms that are responsible for passive uptake. In contrast, active targeting to the inflamed tissue or infected organ includes affixing a surface modifier which is easily recognised by the tumour microenvironment/infected organ [56]. Drug targeting to AM was the main aim of this experiment. Several formulations have been reported till date for TB treatment, and a few are in the trial stage. The standard regimen approved by WHO for TB still remains oral drug delivery followed by i.v. administration of antibiotics. Several new antitubercular drugs with improved efficacy have come up like bedaquiline, pretomanid and delamanid, and have been approved for oral administration in MDR-TB patients. But the associated toxic effects are also reported [6]. Levofloxacin-based formulations were prepared for the study, which was further functionalised to improve the therapeutic outcome of the study. PLGA and soya lecithin were used in combination, and a double emulsion solvent evaporation technique was used for the preparation of self-assembling nanoparticles. The formulation prepared was in the form of a core-coat with PLGA-entrapped LVF core and a lecithin coat to improve its uptake and circulation life. The combination of PLGA and lecithin gives a dual advantage to the formulation of long-circulating particles with controlled release characteristics.
The response surface design aims at selecting the best combination of lipid and polymer and surfactant which helps in controlling the size of the particles. The developed formulations were characterised for size, zeta potential and entrapment efficiency. The particle size of the optimised formulation was 314.4 nm with a zeta potential of −11.29 mV, and CHF was found to have a particle size of 471.5 nm and a zeta potential of 1.21 mV. The TEM and SEM figures clearly indicate a bilayer spherical structure. NTA analysis was also carried out on the samples. The results of NTA promulgate the fact that upon dilution the aggregates are lost. The intensity distribution profile indicates that HF consists of smaller particles at a mode of 137.2 nm, and CHF had a mode of 222.8 nm. These results are in stark difference with DLS data obtained through Nanoplus analyser. As the DLS measures the hydrodynamic diameter of the particles in solution with the solvent layer surrounding it and finally makes a measure of the mean, which in the presence of aggregates, leans towards a higher value. NTA measures the hydrodynamic diameter through sCMOS camera, and to evade counting aggregates, it relies on mode. The same is highlighted in the intensity plots obtained. The smaller size obtained via NTA is due to an extra step of sonication which was carried out during reconstitution followed by dilution. The TEM and SEM results also indicate that the individual nanoparticles were smaller than those assessed by Nanoplus. TEM and SEM measure the particles in their native states without a solvent or other vehicles. Electron microscopy is carried out to estimate the surface character of the nanoparticles.
The higher range obtained in the Nanoplus can be attributed to impurities, aggregates and solvent halo around the particles. The ease of carrying out size and zeta potential analysis via DLS makes it a frontrunner in nanoparticle analysis techniques. The other physical parameters studied for HF and CHF prove that LVF is completely incorporated in HF and CHF as studied via IR spectra of the formulations and raw materials. The broadband of -OH from 3756 cm−1 to 2400 cm−1 indicates carubinose linkage with soya lecithin. The overlapping signals of NH with OH of carubinose also indicate the same. The levofloxacin conjugated carbonyl group is slightly shifted to 1623 cm−1 whereas the acid COOH group is shifted to 1756 cm−1 which indicates a strong bond formation with HF [16, 53]. HF and CHF do not particularly express the peaks of LVF indicating complete entrapment of LVF in the formulation which is also further extended by the DSC and TGA data.
HF also indicates a linkage of LVF which was also encountered during drug loading estimation. During drug loading estimation, HF and CHF required prior hydrolysis of the formulation in alkaline SDS solution, releasing free LVF. PLGA also undergoes slow hydrolysis in vivo which explains its sustained release character and also explains the release of drug from the PLGA matrix. The TGA curve showed different regions of weight loss during the analysis which can be explained via reference to the thermal behaviour of LVF, PLGA and soya lecithin. The TGA and DSC curves are characteristic for a given material and elicit the thermal character of the materials in question. LVF followed the characteristic profile as mentioned [57] and other studies with an initial 3.5% water loss and a degradation curve beginning at 244.15 °C. It also presented a sharp melting peak at 232.77 °C characteristic of its crystalline nature. CHF and HF, however, had a different and completely new show of character with an initial loss of ∆W = 17.56% and ∆W = 9.59% that indicates water loss as well as mass loss at lower temperatures as that of body fluids. This can also be an indicator of the initial burst release of the formulation. The second and third regions of weight loss indicate a breakdown of polymeric structure and loss of functional groups due to pyrolysis. The DSC data for HF and CHF show small endothermic regions initially indicative of glass transition of PLGA and soya lecithin in their native form and presence of unreacted material. No sharp or broad melting peaks or regions can be derived from the data showing complete drug incorporation. The CHF and HF show significant differences in initial weight loss, indicating that the CHF releases drug at body temperature due to melting assisted with diffusion. A decrease in the energy of the initial endotherms indicates that lesser energy is required to release the drug from the system. The individual components do not lose their characteristic peak, which confirms the compatibility of the system.
The change in physical properties of the drug and characteristic endotherms of PLGA and lecithin shows the system is stable and possesses better in vivo performance. The XRD and thermal data reveal that the crystalline LVF is converted to an amorphous form which can be seen in XRD data. Furthermore, weight losses point towards the degradation behaviour of the formulation at higher temperatures which is also seen in stability studies. The XRD data of LVF, HF and CHF were mapped with available literature. The matching leads us to a view that native LVF existed as a crystalline material and HF and CHF although indicate the presence of various peaks of LVF. The loss in intensity indicates the conversion of the crystalline drug to an amorphous state. The amorphous state was also confirmed by the literature. This conversion indicates that HF and CHF have LVF present but in an entrapped state [54].
The presence of phospholipid bilayer acts as a boundary for delivery systems and resists intracellular targeting. To overcome this hurdle, various endosomal membrane disrupting carriers have been designed. These carriers are hemolytic in nature and thereby are not biocompatible. The hemocompatibility test is designed to rapidly assess the compatibility of the nanocarriers with the cell membrane. Drug delivery systems which have a long circulation time come directly in contact with RBCs and are required to have a lesser hemolytic activity to remain biocompatible. The reduced hemolytic property of CHF can be attributed to the shielding of amine groups due to carubinose linkage [58]. The slightly increased but significantly less hemolytic property of HF compared to LVF can be due to the presence of an amine group of soya lecithin on its surface. The presence of these groups is confirmed by the FTIR data. The in vitro dissolution behaviour of HF and CHF point towards a biphasic release of LVF characterised by a small burst release (30% in 5 h) followed by slow diffusion. The release kinetics curve fitting indicated the best fit for the Higuchi model as well as Korsmeyer-Peppas model. The Higuchi release kinetics is governed by the fact that diffusion is the controlling mechanism for drug release from the system. The small n value for Korsmeyer-Peppas model indicates zero-order diffusion. Similar release characteristics were observed for in vivo pharmacokinetics data which showed that the release continued for 72 h. The core-coat structural characteristic of HF and CHF contributes to the diffusion release mechanism. The coat of carubinose modified HF and unmodified HF acts as a hindrance to drug release. Since LVF is a hydrophilic drug with good permeation characteristics, it was required to be formulated in a manner so as to control the release as well as to make it target-oriented. Modification with carubinose gives it the targeting ability and the interplay of PLGA and lecithin controls the release. The lipid coat hinders the entry of water in the core–shell structure and PLGA controls the shedding of the nanoparticle layers. This combination of nanoparticle degradation for release of LVF gives HF and CHF its unique release character i.e. burst release of surface tagged drug and then diffusion-controlled release. The pharmacokinetic data also confirm the same release pattern with an initial burst release followed by a diffusion release pattern.
The release depends on the degradation of PLGA in vivo, which was seen in the HPLC estimation of drug content. The drug content values increased drastically when the formulations were placed in alkaline SDS (sodium dodecyl sulphate) solution. The SDS degrades PLGA which in turn releases LVF. Therefore, when it was attempted to estimate LVF initially by dissolving in dichloromethane (DCM), the results were not exhibiting the true drug load. Whereas, when alkaline SDS was used, the LVF content in HF and CHF increased drastically, implying that PLGA and soya lecithin are individually soluble in DCM, but the hybrid formulation with its new configuration renders itself less liable to dissolution in DCM. At this point, alkaline SDS denatures PLGA and releases the LVF for estimation. The same conditions prevail in the AM. The presence of various enzymes and buffering agents helps in the degradation of lecithin and PLGA, thereby releasing LVF at the site of action.
Macrophage targeting was achieved successfully as indicated by the FACS data as well as quantitative uptake studies. The viability assay carried out via MTT exhibited the safety profile of CHF and HF upto 50 ppm. The viability of the cells was above 50% till 50 ppm which reduced to 48 and 44 for CHF and HF respectively. This ensures that at therapeutic levels CHF and HF retain maximum cell viability. The cell viability results also emphasise the fact that the GRAS excipients used in the formulation do not affect the test results. Proper washing of the formulation to get rid of surfactants facilitated in accomplishing good viability results. Furthermore, the rapid internalisation of CHF as estimated quantitatively through RP-HPLC studies is due to the presence of carubinose on the surface which is easily recognised by the macrophages and the size of the formulation which enables quick phagocytosis of the formulation. HF possessed lesser internalisation than CHF but more than that of LVF because it is internalised by passive diffusion only. The efficacy of quantitative cellular uptake can be further corroborated by FACS results, both qualitative and quantitative. The fluorescence intensity is a time-dependent feature; the formulations were kept under incubation for 6 h before taking the readings. The high fluorescence in CHF is due to receptor-mediated activity of carubinose as well as passive uptake of the formulation. The uptake of HF is due to non-specific internalisation by endocytosis/phagocytosis. HF also possessed better uptake than LVF as is evident from the data and can be correlated to a few previous works which indicate that HF is better internalised and uptaken by the cells than the pure drug alone as the presence of lipid in the coating layer promotes rapid internalisation. The enhanced uptake of CHF as compared to HF is due to the presence of surface modifier on CHF and it enjoys a two-way uptake of active and passive methods. Fluorescence microscopy results also add up to the concept of better uptake of surface functionalised formulation.
The in vivo pharmacokinetic data revealed the controlled release pattern of the formulation. The pharmacokinetic data indicates a long MRT for HF, and CHF indicates better retention of LVF by the two formulations. The increase in AUC is indicative of better bioavailability of LVF from HF and CHF. The decrease in Cl rate and increased Vss are indicative of better retention of LVF in target organ/AM. These improved characters owe it to the HS where the lipid coat provides a sheath to the PLGA. Thus, the reduced available surface area for entry of fluids was a limiting step in drug release. The presence of carubinose on the surface imparted better entry CHF in the AM. The slightly acidic environment of AM leads to a further reduction in drug release from the formulation, which extended its release profile. The stability data obtained after 6 months of study puts forward the fact that CHF and HF are stable under long-term storage conditions of refrigeration. When stored at low temperatures, the formulations retained their size with a slight change of 1.7%. The drug loading was reduced by 2.58%. CHF remained stable as evident from zeta potential values with a 2.58% reduction. HF placed under long-term storage conditions exhibited degradation but the change does not qualify as significant in terms of drug loading (1.59%), particle size (0.93%) and zeta potential (1.24%). ICH guidelines verify stability in terms of drug content specifically which remained well within limits for the entire duration of 6 months. Both HF and CHF showed insignificant changes within 3 months; therefore, the samples were placed under testing conditions for another 3 months. As the formulations are meant to be administered intravenously, the stability studies were done for lyophilised formulations which are meant to be reconstituted just before administration. The stability readings confirm the data obtained by the thermal characterisation that the formulation remains stable at lower temperatures.
The above results conclude that HS is one of the new emerging delivery systems for targeting drugs to AM. The viability assay ensured that the formulations are safe for normal cells and are not toxic in their therapeutic range. They also show sufficient potential to be explored as an alternative for enhanced targeting to the AM resident bacteria.
Conclusions
A hybrid formulation comprising a lipid and a polymer in tandem can overcome the disadvantages of a singular system such as polymeric nanoparticles, liposomes, SLN and NLCs. Lipid-based systems possess better entrapment, scalability; however, the limitations are instability and restricted surface modifications. Polymeric systems often provide scaffolds for chemical transformations, controlled release potential and better stability; however, insufficient drug loading capacities and scale-up are major limitations. A stable surface-modified lipid-polymer hybrid system (CHF) was prepared through a proper selection of lipid and polymer with desired characteristics. LVF-entrapped hybrid systems are successful in incorporating and controlling the release characteristics of hydrophilic LVF. The safety profile of the prepared system and the hemocompatibility offered by them make hybrid systems a safer drug delivery system. The enhanced uptake of CHF (15X) and HF (3X) as compared to FITC helps in better targeting and achieving higher local drug concentrations. The spherical morphology of the HS aids in better release characteristics. The improved release characters help in reducing the dosing frequency and advance patient compliance and better therapeutic outcomes. The reported hybrid system(s) are expected to prove themselves as attractive alternatives to single nanoparticulate systems regarding their efficacy.
Availability of data and material
All the data generated during the study are included in the article and the supplementary files.
Code availability
Not applicable.
References
World Health Organization. Global tuberculosis report 2020. https://www.who.int/publications/i/item/9789240013131. Accessed 28 Dec 2020. ISBN 978 92 4 156539 4.
Costa A, Sarmento B, Seabra V. Targeted drug delivery systems for lung macrophages. Curr Drug Targets. 2015;16(14):1565–81.
Misra A, Hickey AJ, Rossi C, Borchard G, Terada H, Makino K, Fourie PB, Colombo P. Inhaled drug therapy for treatment of tuberculosis. Tuberculosis. 2011;91(1):71–81. https://doi.org/10.1016/j.tube.2010.08.009.
Pham DD, Fattal E, Tsapis N. Pulmonary drug delivery systems for tuberculosis treatment. Int J Pharm. 2015;478(2):517–29. https://doi.org/10.1016/j.ijpharm.2014.12.009.
Greco E, Quintiliani G, Santucci MB, Serafino A, Ciccaglione AR, Marcantonio C, Papi M, Maulucci G, Delogu G, Martino A, et al. Janus-faced liposomes enhance antimicrobial innate immune response in mycobacterium tuberculosis infection. Proc Natl Acad Sci U S A. 2012;109(21):E1360–7. https://doi.org/10.1073/pnas.1200484109.
Baranyai Z, Soria-Carrera H, Alleva M, Millán-Placer AC, Lucía A, Martín-Rapún R, Aínsa JA, la Fuente JM. Nanotechnology-based targeted drug delivery: an emerging tool to overcome tuberculosis. Adv Ther. 2020;4:2000113. https://doi.org/10.1002/adtp.202000113.
Shahwal V, Dubey BK, Bhoumick M. Preformulation study of levofloxacin. Int J Adv Pharm. 2012;1(1):225–7.
Lourenço MCS, Junior IN, De Souza MVN. In vitro activity of ciprofloxacin, ofloxacin, levofloxacin, sparfloxacin and gatifloxacin against multidrug-resistant mycobacterium tuberculosis in Rio de Janeiro Brazil. Méd Mal Infect. 2007:295–96. https://doi.org/10.1016/j.medmal.2007.03.011.
Schulte S, Ackermann T, Bertram N, Sauerbruch T, Paar WD. Determination of the newer quinolones levofloxacin and moxifloxacin in plasma by high-performance liquid chromatography with fluorescence detection. J Chromatogr Sci. 2006;44(4):205–8. https://doi.org/10.1093/chromsci/44.4.205.
Raizman MB, Rubin JM, Graves AL, Rinehart M. Tear concentrations of levofloxacin following topical administration of a single dose of 0.5 % levofloxacin ophthalmic solution in healthy volunteers. Clin Ther. 2002;24(9):1439–50. https://doi.org/10.1016/S0149-2918(02)80047-9.
Bedini A, Garlassi E, Stentarelli C, Petrella S, Meacci M, Meccugni B, Meschiari M, Franceschini E, Cerri S, Brasacchio A, et al. Multidrug-resistant tuberculosis outbreak in an Italian prison: tolerance of pyrazinamide plus levofloxacin prophylaxis and serial interferon gamma release assays. New Microbes New Infect. 2016;12:45–51. https://doi.org/10.1016/j.nmni.2016.03.010.
Gupta S, Kumar P, Gupta MK, Vyas SP. Colloidal carriers: a rising tool for therapy of tuberculosis. Crit Rev Ther Drug Carrier Syst. 2012;29(4):299–353. https://doi.org/10.1615/CritRevTherDrugCarrierSyst.v29.i4.20.
Patil-Gadhe A, Pokharkar V. Single step spray drying method to develop proliposomes for inhalation: a systematic study based on quality by design approach. Pulm Pharmacol Ther. 2014;27(2):197–207. https://doi.org/10.1016/j.pupt.2013.07.006.
Trapani A, Di Gioia S, Castellani S, Carbone A, Cavallaro G, Trapani G, Conese M. Nanocarriers for respiratory diseases treatment: recent advances and current challenges. Curr Top Med Chem. 2014;14(9):1133–47.
Blasi P, Schoubben A, Giovagnoli S, Rossi C, Ricci M. Fighting tuberculosis: old drugs, new formulations. Expert Opin Drug Deliv. 2009;6(9):977–93. https://doi.org/10.1517/17425240903130577.
Kumar G, Sharma S, Shafiq N, Khuller GK, Malhotra S. Optimization, in vitro–in vivo evaluation, and short-term tolerability of novel levofloxacin-loaded PLGA nanoparticle formulation. J Pharm Sci. 2012;101(6):2165–76. https://doi.org/10.1002/jps.23087.
Abed N, Couvreur P. Nanocarriers for antibiotics: a promising solution to treat intracellular bacterial infections. Int J Antimicrob Agents. 2014;43(6):485–96. https://doi.org/10.1016/j.ijantimicag.2014.02.009.
D’Addio SM, Baldassano S, Shi L, Cheung L, Adamson DH, Bruzek M, Anthony JE, Laskin DL, Sinko PJ, Prud’Homme RK. Optimization of cell receptor-specific targeting through multivalent surface decoration of polymeric nanocarriers. J Control Release. 2013;168(1):41–9. https://doi.org/10.1016/j.jconrel.2013.02.004.
Jain NK, Mishra V, Mehra NKK. Targeted drug delivery to macrophages. Expert Opin Drug Deliv. 2013;10(3):353–67. https://doi.org/10.1517/17425247.2013.751370.
Kurmi BD, Kayat J, Gajbhiye V, Tekade RK, Jain NK. Micro- and nanocarrier-mediated lung targeting. Expert Opin Drug Deliv. 2010;7(7):781–94. https://doi.org/10.1517/17425247.2010.492212.
Moretton MA, Chiappetta DA, Andrade F, Das Neves J, Ferreira D, Sarmento B, Sosnik A. Hydrolyzed galactomannan-modified nanoparticles and flower-like polymeric micelles for the active targeting of rifampicin to macrophages. J Biomed Nanotechnol. 2013;9(6):1076–87. https://doi.org/10.1166/jbn.2013.1600.
Irache JM, Salman HH, Gamazo C, Espuelas S. Mannose-targeted systems for the delivery of therapeutics. Expert Opin Drug Deliv. 2008;5(6):703–24. https://doi.org/10.1517/17425247.5.6.703.
Costa A, Pinheiro M, Magalhães J, Ribeiro R, Seabra V, Reis S, Sarmento B. The formulation of nanomedicines for treating tuberculosis. Adv Drug Deliv Rev. 2016;102:102–15. https://doi.org/10.1016/j.addr.2016.04.012.
Dube D, Agrawal GP, Vyas SP. Tuberculosis: from molecular pathogenesis to effective drug carrier design. Drug Discov Today. 2012;17(13–14):760–73. https://doi.org/10.1016/j.drudis.2012.03.012.
Dascher CC, Hiromatsu K, Xiong X, Morehouse C, Watts G, Liu G, McMurray DN, LeClair KP, Porcelli SA, Brenner MB. Immunization with a mycobacterial lipid vaccine improves pulmonary pathology in the Guinea pig model of tuberculosis. Int Immunol. 2003;15(8):915–25. https://doi.org/10.1093/intimm/dxg091.
Ma P, Li T, Xing H, Wang S, Sun Y, Sheng X, Wang K. Local anesthetic effects of bupivacaine loaded lipid-polymer hybrid nanoparticles: in vitro and in vivo evaluation. Biomed Pharmacother. 2011;2017(89):689–95. https://doi.org/10.1016/j.biopha.2017.01.175.
Bhardwaj A, Mehta S, Yadav S, Singh SK, Grobler A, Goyal AK, Mehta A. pulmonary delivery of antitubercular drugs using spray-dried lipid–polymer hybrid nanoparticles. Artif Cells Nanomed Biotechnol. 2016;44(6):1544–55. https://doi.org/10.3109/21691401.2015.1062389.
Varghese SE, Fariya MK, Rajawat GS, Steiniger F, Fahr A, Nagarsenker MS. Lecithin and PLGA-based self-assembled nanocomposite, lecithmer: preparation, characterisation, and pharmacokinetic/pharmacodynamic evaluation. Drug Deliv Transl Res. 2016;6(4):342–53. https://doi.org/10.1007/s13346-016-0314-y.
Sengel-Turk CT, Hascicek C. Design of lipid-polymer hybrid nanoparticles for therapy of BPH: Part I Formulation optimization using a design of experiment approach. J Drug Deliv Sci Technol. 2017;39:16–27. https://doi.org/10.1016/j.jddst.2017.02.012.
Ghitman J, Biru EI, Stan R, Iovu H. Review of hybrid PLGA nanoparticles: future of smart drug delivery and theranostics medicine. Mater Des. 2020;193: 108805. https://doi.org/10.1016/j.matdes.2020.108805.
Maurya P, Singh S, Saraf SA. Inhalable hybrid nanocarriers for respiratory disorders. Target Chronic Inflamm Lung Dis Using Adv Drug Deliv Syst. 2020:281–302. https://doi.org/10.1016/B978-0-12-820658-4.00013-3.
Gajra B, Dalwadi C, Patel R. Formulation and optimisation of itraconazole polymeric lipid hybrid nanoparticles (lipomer) using Box Behnken design. DARU, J Pharm Sci. 2015;23(1). https://doi.org/10.1186/s40199-014-0087-0.
Zheng M, Gong P, Zheng C, Zhao P, Luo Z, Ma Y, Cai L. Lipid-polymer nanoparticles for folate-receptor targeting delivery of doxorubicin. J Nanosci Nanotechnol. 2015;15(7):4792–8. https://doi.org/10.1166/jnn.2015.9604.
Saraogi GK, Sharma B, Joshi B, Gupta P, Gupta UD, Jain NK, Agrawal GP. Mannosylated gelatin nanoparticles bearing isoniazid for effective management of tuberculosis. J Drug Target. 2011;19(3):219–27. https://doi.org/10.3109/1061186X.2010.492522.
Parashar P, Rathor M, Dwivedi M, Saraf SA. Hyaluronic acid decorated naringenin nanoparticles: appraisal of chemopreventive and curative potential for lung cancer. Pharmaceutics. 2018;10(1). https://doi.org/10.3390/pharmaceutics10010033.
Parashar P, Tripathi CB, Arya M, Kanoujia J, Singh M, Yadav A, Saraf SA. A facile approach for fabricating CD44-targeted delivery of hyaluronic acid-functionalized PCL nanoparticles in urethane-induced lung cancer: Bcl-2, MMP-9, Caspase-9, and BAX as Potential Markers. Drug Deliv Transl Res. 2019;9(1):37–52. https://doi.org/10.1007/s13346-018-0575-8.
Assadullah I, Zaman MB, Malik KA, Malik JH, Bhat AA, Tomar R. Growth and properties of hydrothermally derived crystalline ZnSe quantum dots. Environ Sci Pollut Res. 2020. https://doi.org/10.1007/s11356-020-11026-1.
Burhanuz Zaman M, Mir RA, Poolla R. Growth and properties of solvothermally derived highly crystalline Cu2ZnSnS4 nanoparticles for photocatalytic and electrocatalytic applications. Int J Hydrogen Energy. 2019;44(41):23023–33. https://doi.org/10.1016/j.ijhydene.2019.07.026.
Kumar A, Das N, Satija NK, Mandrah K, Roy SK, Rayavarapu RG. A novel approach towards synthesis and characterization of non-cytotoxic gold nanoparticles using taurine as capping agent. Nanomaterials. 2020;10(1). https://doi.org/10.3390/nano10010045.
Sajeev Kumar B, Saraswathi R, Dhanaraj SA. Solid-state characterization studies and effect of PEG 20000 and P90G on particle size reduction and stability of complexed glimepiride nanocrystals. J Young Pharm. 2013;5(3):83–9. https://doi.org/10.1016/j.jyp.2013.08.002.
Semalty A, Semalty M, Singh D, Rawat MSM. Preparation and characterization of phospholipid complexes of naringenin for effective drug delivery. J Incl Phenom Macrocycl Chem. 2010;67(3–4):253–60.
Kumar S, Gokhale R, Burgess DJ. Sugars as bulking agents to prevent nano-crystal aggregation during spray or freeze-drying. Int J Pharm. 2014;471(1–2):303–11.
Nisha R, Kumar P, Kumar U, Mishra N, Maurya P, Singh S, Singh P, Guleria A, Saha S, Saraf SA. Fabrication of imatinib mesylate-loaded lactoferrin-modified PEGylated liquid crystalline nanoparticles for mitochondrial- dependent apoptosis in hepatocellular carcinoma. Mol Pharm. 2020. https://doi.org/10.1021/acs.molpharmaceut.0c01024.
Huang B, Tong F, Chen Y, Zhu Q, Xing L, Lv M, Mao C, Lu Z, Shen J. Fabrication and bioproperties of raspberry-type hybrid nanoparticles of Au-thioethyl pendant ligand@chitosan. J Biomed Nanotechnol. 2013;9(1):115–23. https://doi.org/10.1166/jbn.2013.1476.
Chen LQ, Fang L, Ling J, Ding CZ, Kang B, Huang CZ. Nanotoxicity of silver nanoparticles to red blood cells: size dependent adsorption, uptake, and hemolytic activity. Chem Res Toxicol. 2015;28(3):501–9. https://doi.org/10.1021/tx500479m.
Rojanarat W, Nakpheng T, Thawithong E, Yanyium N, Srichana T. Levofloxacin-proliposomes: opportunities for use in lung tuberculosis. Pharmaceutics. 2012;4(3):385–412. https://doi.org/10.3390/pharmaceutics4030385.
Nguyen HA, Grellet J, Paillard D, Dubois V, Quentin C, Saux MC. Factors influencing the intracellular activity of fluoroquinolones: a study using levofloxacin in a Staphylococcus Aureus THP-1 monocyte model. J Antimicrob Chemother. 2006;57(5):883–90. https://doi.org/10.1093/jac/dkl079.
Asthana S, Gupta PK, Jaiswal AK, Dube A, Chourasia MK. Overexpressed macrophage mannose receptor targeted nanocapsules- mediated cargo delivery approach for eradication of resident parasite: in vitro and in vivo studies. Pharm Res. 2015;32(8):2663–77. https://doi.org/10.1007/s11095-015-1651-0.
Guideline IH. Stability testing of new drug substances and products. Q1A (R2), current step. 2003 Feb;4:1-24.
Sharma RK, Dutta S, Sharma S. Quinoline-2-carboimine copper complex immobilized on amine functionalized silica coated magnetite nanoparticles: a novel and magnetically retrievable catalyst for the synthesis of carbamates via C-H activation of formamides. Dalt Trans. 2014;44(3):1303–16. https://doi.org/10.1039/c4dt03236e.
Zhang Y, Huo M, Zhou J, Zou A, Li W, Yao C, Xie S. DDSolver : an add-in program for modeling and comparison of drug dissolution profiles. AAPS J. 2010;12(3):263–71. https://doi.org/10.1208/s12248-010-9185-1.
Mircioiu C, Voicu V, Anuta V, Tudose A, Celia C, Paolino D, Fresta M, Sandulovici R, Mircioiu I. Mathematical modeling of release kinetics from supramolecular drug delivery systems. Pharmaceutics. 2019;11(3):140. https://doi.org/10.3390/pharmaceutics11030140.
Gaspar MC, Pais AACC, Sousa JJS, Brillaut J, Olivier JC. Development of levofloxacin-loaded PLGA microspheres of suitable properties for sustained pulmonary release. Int J Pharm. 2019;556:117–24. https://doi.org/10.1016/j.ijpharm.2018.12.005.
Singh SS, Thakur TS. New crystalline salt forms of levofloxacin: conformational analysis and attempts towards the crystal structure prediction of the anhydrous form. CrystEngComm. 2014;16(20):4215–30. https://doi.org/10.1039/c4ce00263f.
Evans BC, Nelson CE, Yu SS, Beavers KR, Kim AJ, Li H, Nelson HM, Giorgio TD, Duvall CL. Ex Vivo Red Blood Cell Hemolysis Assay for the Evaluation of PH-responsive endosomolytic agents for cytosolic delivery of biomacromolecular drugs. J Vis Exp. 2013;73:6–10. https://doi.org/10.3791/50166.
Lee W-H, Loo C-Y, Traini D, Young PM. Nano- and micro-based inhaled drug delivery systems for targeting alveolar macrophages. Expert Opin Drug Deliv. 2015;12(6):1009–26. https://doi.org/10.1517/17425247.2015.1039509.
Gorman EM, Samas B, Munson EJ. Understanding the dehydration of levofloxacin hemihydrate. J Pharm Sci. 2012;101(9):3319–30. https://doi.org/10.1002/jps.23200.
Jain A, Agarwal A, Majumder S, Lariya N, Khaya A, Agrawal H. Mannosylated solid lipid nanoparticles as vectors for site-specific delivery of an anti-cancer drug. J Control Release. 2010;148(3):359–67. https://doi.org/10.1016/j.jconrel.2010.09.003.
Acknowledgements
Authors are thankful to University Science Instrumentation Centre, BBAU, Lucknow, Central Instrumentation Facility, Jiwaji University, Gwalior and CSIR-CDRI, Lucknow, for providing research facilities. We acknowledge CSIR-IITR for timely NTA analysis.
Author information
Authors and Affiliations
Contributions
Conceptualisation, Priyanka Maurya, Manish K. Chourasia and Shubhini A Saraf. Data curation, Priyanka Maurya, Nidhi Mishra and Abhiram Kumar. Formal analysis, Priyanka Maurya and Shubhini A Saraf. Investigation, Priyanka Maurya, Ravi Saklani, Samipta Singh and Priya Singh. Methodology, Priyanka Maurya, Ravi Saklani, Raquibun Nisha and Abhiram Kumar. Resources, Manish K. Chourasia and Shubhini A Saraf. Software, Ravi Saklani, Ravi Raj Pal, Nidhi Mishra and Priya Singh. Supervision, Shubhini A Saraf. Visualization, Nidhi Mishra and Priya Singh. Writing—original draft, Priyanka Maurya and Shubhini A Saraf. Writing—review and editing, Priyanka Maurya, Samipta Singh, Raquibun Nisha, Ravi Raj Pal, Priya Singh, Manish K. Chourasia and Shubhini A Saraf.
Corresponding author
Ethics declarations
Ethics approval
The approval number for in vivo studies is BBDNIIT/IAEC/2019/01.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Maurya, P., Saklani, R., Singh, S. et al. Appraisal of fluoroquinolone-loaded carubinose-linked hybrid nanoparticles for glycotargeting to alveolar macrophages. Drug Deliv. and Transl. Res. 12, 1640–1658 (2022). https://doi.org/10.1007/s13346-021-01055-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-021-01055-9