Abstract
Chemical burns are major causes of corneal blindness. Transforming growth factor beta-1 (TGFβ1) plays an important role in induction of corneal inflammation-related-fibrosis leading to the blindness. Here, a topical delivery system consisting anti-fibrotic TGF-β1 siRNA, an inflammatory suppressing gene, was designed for treatment of corneal injuries. TGF-β1 siRNA loaded in nanoparticles (NPs) made up of polyethyleneimine polymer demonstrated high fibroblast transfection efficiency. Moreover, TGF-β1 and PDGF genes and ECM deposition were suppressed in isolated human corneal fibroblasts. NPs inhibited proliferation and transformation of fibroblasts to myofibroblasts by S-phase arrest and α-SMA suppression in vitro, respectively. The mentioned finding was also confirmed in vivo, addressing high wound-healing potential of prepared gene delivery system which was superior to conventional betamethasone treatment. Besides, CD4+ and α-SMA antibody staining showed inhibited angiogenesis and myofibroblast accumulation in treated corneas. This study opens a new way for treating corneal fibrosis through topical siRNA delivery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemical injuries to the eye (cornea and conjunctiva) can produce extensive damage to the ocular surface and anterior segment leading to visual impairment. Corneal alkaline burns are more common and severe than acid burns. Generally, alkaline agents penetrate more rapidly to the tissues and internal compartment of the eye. These agents will degrade the fatty acids, proteoglycans, and collagen bundles that existed in the cell membrane, leading to corneal blindness [1, 2]. Considering the severity of injury, corneal alkaline burns are graded into four groups. Alkaline-burned corneas seldom heal properly, and they show reduced corneal transparency (hazy cornea) and opacity, except for a grade 1 injury [3]. Indeed, corneal blindness is a fibrotic situation in which the corneal haze results in corneal transparency loss. Corneal haze is characterized by cloudy appearance of cornea that will disturb or obstruct the patient’s vision. Myofibroblasts, α-smooth muscle actin (α-SMA)-positive cells, are the major cells involve in corneal haze development [4,5,6,7]. α-SMA, an altered crystalline protein production, leads myofibroblasts to be less transparent than fibroblasts. Moreover, the α-SMA filaments are responsible for cellular light scattering and blurry vision [8]. In addition, myofibroblasts secrete large quantities of collagen type I (Col I) and fibronectin (Fn) that will in turn worsen the corneal haze [5, 9, 10]. Transforming growth factor (TGF-β1) is a pivotal molecule in tissue repair. In corneal alkaline burn injury, TGF-β1 has been shown to promote migration of corneal epithelial cells and fibroblasts, and to induce differentiation of the fibroblasts to myofibroblasts, consequently contributing to the repair of the corneal epithelium and stromal layer [11]. Studies have shown that TGF-β1 will be up-regulated in corneal tissues following alkaline exposure. TGF-β1 also has the ability to induce the expression of other cytokines, such as matrix metalloproteinase 9 (MMP-9), vascular endothelial growth factor (VEGF), and monocyte/macrophage chemotactic protein-1, which is believed to be involved in matrix degradation, local neovascularization, and inflammation, respectively [3]. Actually, overexpression of TGF-β1 is regarded to exacerbate damage to the injured cornea [3]. As TGF-β1 can induce the differentiation of fibroblasts to myofibroblasts, overexpressed TGF-β1 reveals myofibroblast accumulation in the stromal layer of the burned cornea, which was suggested to be the main mechanism of corneal haze formation after injury [12, 13]. Besides, TGF-β1 up-regulates platelet-derived growth factor (PDGF) as another fibrotic growth factor that activates the differentiation of myofibroblasts [6, 14, 15]. Amniotic membrane transplantation, bone marrow-derived human mesenchymal stem cells therapy, human limbal allograft transplantation, and corneal transplantation have been investigated to prevent the corneal blindness after corneal chemical burns [16,17,18]. Moreover, studies showed the benefits of blocking TGF-β1 secretion or its cognate receptor to prevent fibrosis following corneal damages [19, 20]. Results from studies demonstrate potential therapeutic benefits of TGF-β1 suppression immediately or 1 h post-corneal injury [21, 22]. The therapeutics were used independent from severity of corneal damages or cytokine up-regulations. Although, there are researches to preserve patient health and transparency following alkaline burn injuries. However, studies for efficient topical therapeutics that can be applied immediately after corneal injuries seem to be essential to preserve patient eyesight. siRNA therapeutics can degrade the targeted mRNA in cytoplasm [23]. Generally, siRNA anti-sense strand goes through RNA-induced silencing complex (RISC) and explores and degrades the targeted mRNA [24]. The siRNA therapeutics are potent and selective therapeutics for down-regulation of the desired genes. However, some limitations still exist such as instability, cell penetration, and susceptibility of siRNA therapeutics to tissue and plasma RNAase. Additionally, due to their high negative charge, they cannot pass through the negatively charged cell membranes. Polymeric NPs (chitosan, polyethyleneimine (PEI), poly(l-lysine)) and lipid-based nanovehicles (stable nucleic acid lipid particles (SNALPs), liposome) have been investigated for siRNA delivery [25,26,27,28,29,30,31]. PEI, a positively charged polymer, is the most popular polymer for siRNA and gene delivery because of its high transfection efficiency [32, 33]. PEI can make ionic complexes with negatively charged siRNA for effective delivery [34, 35]. siRNA delivery is also interesting for targeting ocular disorders [36]. Some studies investigated the effect of subconjunctival injection of TGF-β receptor type II (TGF-βR2) siRNA and triple combination of TGF-β1, TGF-βR2, and connective tissue growth factor (CTGF) siRNAs for reducing the corneal scar formation after injury [37, 38]. Although, there are different in vivo studies for evaluating the effect of siRNA therapeutics to treat ocular disorders. However, there is no comprehensive data indicating the effectiveness of topical application of siRNAs for treating corneal disorders. In the current study, the potential of TGF-β1 siRNA-loaded PEI NPs on preventing the corneal fibrosis and angiogenesis was evaluated in vitro and in murine model of corneal alkaline burn. The effectiveness of the prepared formulation was compared with betamethasone eye drop, as the main therapeutic for treating corneal chemical burns.
Materials and methods
Materials
PEI (25 kDa) and humanized recombinant interleukin 6 (IL-6) were supplied from Sigma Aldrich, Taufkirchen, Germany. TGF-β1 siRNA and Cy3 scramble siRNA were obtained from Invitrogen, Waltham, MA, USA. Mouse anti-CD34+ antibody, mouse anti-α-SMA antibody, and mouse secondary antibody were purchased from Dako-Glostrup, Denmark. Fibroblasts were prepared from male cadaver cornea sample obtained from Eye Bank, Tehran, Iran.
Methods
Preparation and characterization of TGF-β1 siRNA-loaded NPs
Nanoparticles were prepared by loading TGF-β1 siRNA in branched PEI polymer, average molecular weight 25 kDa. To prepare TGF-β1 siRNA NP stock solutions, 100 pmol of siRNA was added to different amounts of PEI (2, 3, and 5 μg) dissolved in 5 μL distilled water, vortexed for 1 min, and incubated for 15 min at room temperature. The final concentration of TGF-β1 siRNA NP stock solutions was 10 μM. The prepared NPs were used freshly and diluted in supernatant culture medium to transfect the corneal fibroblasts. Condensation ability of PEI containing 100 pmol TGF-β1 siRNA was evaluated through electrophoresis onto 1% agarose gel plate. The electrophoresis was run in TAE (10 mM Tris/HCl, 1% acetic acid (v/v), 1 mM EDTA) buffer at 90 V for 30 min. Also, hydrodynamic mean diameter and zeta potential of NPs were measured by dynamic light scattering and laser Doppler electrophoresis, respectively, using Zetasizer (Nano-ZS, Malvern, UK) at 25 °C. The morphology of NPs was evaluated through field emission scanning electron microscope (FE-SEM; Hitachi S-4160, Germany) imaging at accelerating voltage of 30 kV. NP sample for FE-SEM imaging was prepared by placing 10 μL of the prepared ionic complexes on FE-SEM slide and was left at room temperature to become completely dry and then covered with thin layer of gold as conducting material.
For investigating NP stability, the prepared NPs containing siRNA was diluted in 500 μL Dulbecco’s modified Eagle’s medium (DMEM) cell culture medium and incubated at room temperature for 4, 12, and 24 h, respectively. Thereafter, the size of the prepared NPs was measured and the results were analyzed regarding NP primary size.
Human corneal fibroblasts cultivation
The cornea was dissected using aseptic techniques, and the tissue was washed three times with phosphate-buffered saline (PBS). The tissue was cropped into pieces of 1 mm3 in size and placed on the surface of a tissue culture dish with a cover slip on top of it and cultured in DMEM (Invitrogen, USA) contacting 10% FBS and incubated at 37 °C with 5% CO2. The growth medium was changed every 3–4 days. The cells were subcultured when they reached the 90% confluency.
Cell viability assay
For cell viability assay, 104 corneal fibroblasts were seeded in 96-well plate. After 24 h, the effect of different concentrations of TGF-β1 siRNA NPs (final concentration of 60, 80, and 100 nM TGF-β1 siRNA loaded in 5 μg PEI), different NP formulations containing TGF-β1 siRNA (mg PEI/0.1 nmol TGF-β1 siRNA—0.1, 0.2, 0.4, 0.6, and 0.8), different NP formulations containing Cy3-scrambled siRNA (mg PEI/0.1 nmol Cy3-scrambled siRNA—0.1, 0.2, 0.4, 0.6, and 0.8), naked TGF-β1 siRNA (60, 80, and 100 nM), and PEI solution (0.01, 0.02, 0.04, 0.06, and 0.08 mg/mL) on the viability of fibroblasts was evaluated 24 and 48 h post-treatment using MTT assay according to the instruction that was previously described by our group [39]. Because of the anti-proliferative properties of the TGF-β1 siRNA, the cytotoxicity of NPs containing TGF-β1 siRNA was evaluated through trypan blue assay according to the previously described method [40]. Each experiment was performed in triplicate.
Uptake study
Cy3-conjugated scrambled siRNA (Cy3 siRNA) was used to evaluate the transfection efficiency of PEI NPs by fibroblasts. For this purpose, Cy3 siRNA was loaded in PEI according to the procedure described earlier. About 5 × 105 fibroblasts were seeded in 6-well plate containing 4% FBS. Cy3 siRNA NPs were diluted in supernatant medium of cultivated fibroblasts to reach a final concentration of 60 nM Cy3 siRNA and incubated at 37 °C in the dark for 4 h. Each experiment was performed in triplicate. Then, the cells were washed multiple times with pre-warmed PBS to remove the excess amounts of Cy3 siRNA NPs at the surface of fibroblasts, and subsequently, the cells were evaluated by fluorescent microscope imaging. Thereafter, the cells were detached and re-suspended in PBS for flow cytometry (Applied Biosystem, USA) to quantify the uptake of Cy3 siRNA by fibroblasts.
In vitro inflammation induction
To imitate the inflammatory response and up-regulation of fibrotic genes in isolated human fibroblasts, humanized recombinant interleukin 6 (IL-6, 2 ng/mL) was used. After seeding the fibroblasts (final amounts of 106 cells/flask), 2 ng/mL of IL-6 was added to the medium. After 24 h incubation, the levels of TGF-β1 and α-SMA gene expression in the treated cells were quantified and compared with the levels of these genes in control group (cells with no IL-6 treatment) using qRT-PCR.
Gene expression study
To investigate the effect of TGF-β1 siRNA NPs on TGF-β1 and other fibrotic genes (PDGF, VEGF, collagen type Iα1 (Col Iα1), Col Iα2, and fibronectin (Fn)), 106 fibroblasts were seeded in tissue culture flasks containing 4% FBS to prevent the effect of FBS on myofibroblasts differentiation. After 24 h, IL-6 (2 ng/mL) was added to the cell culture supernatant medium to stimulate the expression of TGF-β1 and α-SMA genes. For fibroblasts transfection, TGF-β1 siRNA NPs were diluted in fibroblasts cell culture medium to reach the final concentration of 60 nM of TGF-β1 siRNA (the ideal concentration of siRNA for gene down-regulation in vitro as described by manufacturer). The gene expression was quantitatively determined 24 and 48 h post-treatment by qRT-PCR. The fibroblasts treated with IL-6 (2 ng/mL) were considered control group. The gene expression profile of fibroblast was detected to conform the effect of scrambled siRNA-loaded NPs on fibrotic genes. Each experiment was performed in triplicate. The total mRNA of fibroblasts was extracted by RNX reagent (Cinagene, Iran) and subsequently converted to cDNA. The cells were harvested, centrifuged, and lysed by RNX reagent. The aqueous phase containing mRNA was separated and mixed with cold isopropanol and kept at − 20 °C, overnight. A day after, the mixture was centrifuged at 12,000 RPM for 20 min at 4 °C. The precipitated mRNA was washed with cold ethanol (70%, v/v) and eluted with 20 μL MilliQ water. The isolated mRNA was converted to cDNA by Fermentas reverse transcriptase (Fermentas, USA) according to the standard instructions. qRT-PCR was performed using ABI System (USA). qRT-PCR Master Mix (Yekta, Iran) was used to detect the amplification procedure. Hypoxanthine phosphoribosyltransferase (HPRT1) gene was selected as the internal control. Forward and reverse primers (Table 1) were designed to selectively amplify the desired cDNA. The obtained results were analyzed by REST® software.
Cell cycle analysis
To assess the anti-proliferative effect of TGF-β1 siRNA NPs on the corneal fibroblasts, the cell cycle analysis was performed. Briefly, the treated cells were detached, centrifuged, and washed three times with PBS and were re-suspended in 50 μL PBS. To enhance the cell permeation to propidium iodide (PI) fluorescent dye, 450 μL of cold ethanol (70%, v/v) was added to the suspended cells. The cells were kept at − 20 °C, overnight. A day after, the suspended cells were centrifuged at 2000 RPM for 20 min at 4 °C. The cell pellet was re-suspended in 50 μL PI and RNase-A complex. The mixture was incubated for 40 min at 37 °C. The samples were analyzed by flow cytometry (Applied Biosystem, USA) for cell cycle analysis. Each experiment was performed in triplicate.
Animal study
The in vivo experiments were performed with the approval of the Ethics Committee for Animal Experiments at Tehran University of Medical Science (TUMS), Iran. For this purpose, 6-month-old male BALB/c mice (total number of animals, 15) were selected. To induce the corneal alkaline burn, the animals were anesthetized with ketamine/xylene. After induction of deep anesthetization, 1 μL of NaOH (0.5 N) was placed at the center of each mice right eye cornea. Immediately, the injured cornea was washed with 1 mL distilled water. The animals were divided into three groups containing five animals; negative control group received PBS and vehicle loaded with scramble siRNA, positive control group received betamethasone (0.1% (w/v), SinaDarou, Iran) three times a day, and TGF-β1 siRNA NP-treated group received TGF-β1 siRNA treatment at a final concentration of 10 μM three times a day. To prevent the microbial contamination, chloramphenicol (0.5% (w/v), SinaDarou, Iran) was administered to each damaged cornea at the day of inducing the injury. To evaluate the anti-fibrotic effect of treatments, the animals were killed 21 days following the treatment. Eye globes were fixed in 15% buffered formaldehyde, overnight, and later, parallel sections from globes were made and paraffin blocks were prepared. Multiple 3–5-μm sections from each block were obtained, and glass slides were stained by routine hematoxylin and eosin (H&E) staining, trichrome histochemical method, and immunohistochemical (IHC) staining method for CD34+ and α-SMA markers. All slides were examined twice and scored with respect to severity of inflammation, angiogenesis, fibrosis, and myofibroblastic cellular proliferation in injured areas of corneal stromal. To evaluate inflammation, density of neutrophilic leukocytes (PMNs) in H&E stained, the slides were examined and scored from 0 to 3+ (0; no PMN/× 1000 magnification, 1+; 1–10 PMN/× 1000 magnification, 2+; 11–20 PMN/× 1000 magnification, 3+; more than 20 PMN/× 1000 magnification). The angiogenesis was evaluated in CD34+-stained slides, and the density of new vessels was also scored from 0 to 3+ (0; no vessel/× 1000 magnification, 1+; 1–2 vessel/× 1000 magnification, 2+; 3–4 vessel/× 1000 magnification, 3+; 5 or more vessel/× 1000 magnification). The fibrosis and proliferation of myofibroblasts were evaluated as a semi-quantitative index, considering irregular arrangement of collagen bundles in trichrome-stained slides and density of myofibroblastic cells in α-SMA-stained IHC slides. The results were scored from 0 to 2 (0; null, 1+; slight to mild, 2+; moderate to severe).
Statistical data analysis
Significant differences between groups were indicated using two-tailed Student’s t test that level of significance was considered significant at p < 0.05 and very significant at p < 0.01.
Results
Characterization of TGF-β1 siRNA NPs
TGF-β1 siRNA NPs showed spherical shape (Fig. 1A (a′)) with average diameter of 148 ± 53 nm, 0.178 polydispersity index (PDI) (Fig. 1A (b′)), and slightly positive surface charge (+ 7 ± 3.2 mV). As confirmed by agarose gel electrophoresis retardation assay, 5 μg of PEI was almost enough for condensation of 100 pmol TGF-β1 siRNA and retardation of siRNA mobility. In lower amounts of polymer (2 and 3 μg), slight release and mobility of siRNA were seen (Fig. 1B) which shows the incomplete siRNA condensation.
The stability analysis of NPs, also, demonstrated acceptable results in which after 24 h incubation of the NPs with cell culture medium, the size of the NPs did not change significantly (p value > 0.05).
Isolation and cultivation of primary human corneal fibroblast
Human corneal fibroblasts were successfully isolated using explant technique [41]. The cells outgrew from tissue pieces 2 days after being plated in the culture flask. The migrated cells revealed a combination of epithelial- and fibroblast-like cell morphology. However, after four passages, the relative pure fibroblast cells were observed (Fig. 2). The cells displayed a typical long spindle shape.
Cell viability assay
MTT assay demonstrated that TGF-β1 siRNA NPs had no significant toxicity even at high concentration (100 nM siRNA). No significant cytotoxicity related to naked TGF-β1 siRNA was also observed in different concentrations. However, cell viability of fibroblasts next to PEI was dramatically reduced at concentrations above 0.01 mg/mL of the polymer; while, at 0.08 mg/mL of PEI, only18% fibroblast viability was seen (Fig. 3). Different NP formulations containing TGF-β1 siRNA also exhibited excellent viability when PEI concentration is lower than 0.01 mg/mL. However, at higher concentrations, a cytotoxicity related to PEI was detected. The same results was obtained for different NP formulations containing Cy3-scrambled siRNA.
Uptake study
As confirmed by fluorescent microscopy and flow cytometry, Cy3 siRNA NPs were efficiently up-taken and accumulated in the cytoplasm of fibroblasts as indicated as red shine under fluorescent microscope. Whereas, the naked Cy3 siRNA showed no sign of fluorescence (Fig. 4A). Flow cytometer analysis data also revealed a significant (p value < 0.05) difference in the fluorescent intensity of Cy3 siRNA NP-treated fibroblasts as compared with naked Cy3 siRNA (Fig. 4B). The fluorescent intensity of Cy3 siRNA NP-treated fibroblasts was comparable with those cells treated with Cy3 siRNA/Lipofectamine group. Cy3 siRNA was up-taken by almost 20.7 and 28.6% of the treated fibroblast with Cy3 siRNA NPs and Cy3 siRNA/Lipofectamine, respectively, which represent the potential of PEI NPs as efficient siRNA delivery vehicle to primary cells.
Fluorescent microscope images of fibroblasts (A) transfected with naked Cy3 siRNA (A (a′)), PEI/Cy3 siRNA (A (b′)), and Lipofectamine/Cy3 siRNA (A (c′)); quantitative evaluation of Cy3 siRNA uptake by fibroblasts (B) transfected with PEI/Cy3 siRNA (B (a″)) and Lipofectamine/Cy3 siRNA (B (b″)) as compared with naked Cy3 siRNA-treated control group
In vitro inflammation induction
The results obtained from qRT-PCR exhibited a significant (p value < 0.05) increase in the expression levels of TGF-β1 and α-SMA genes 24 h after adding IL-6 (2 ng/mL). TGF-β1 and α-SMA gene expressions showed 3 ± 1.2- and 2.5 ± 0.9-fold up-regulation, respectively, as compared with the control group.
Gene expression study
The gene expression profile of fibroblast cells demonstrated that TGF-β1 siRNA NPs could down-regulate a variety of fibrotic/angiogenic genes. As shown in Fig. 5, qRT-PCR analysis of fibroblasts genes 24 and 48 h after TGF-β1 siRNA NP transfection showed potent down-regulation of TGF-β1 and PDGF genes (p value < 0.05). It seems that the expression of PDGF was regulated by TGF-β1. Col type I and Fn, as two major extracellular matrix (ECM) components secreted from myofibroblasts, were also down-regulated due to myofibroblasts suppression by TGF-β1 siRNA. α-SMA, an internal filament feature of myofibroblasts, was suppressed both 24 and 48 h post-transfection. Furthermore, VEGF expression was inhibited which is clinically valuable for preventing the corneal angiogenesis after corneal injury. Scrambled siRNA-loaded NPs are shown to have no significant effect on the expression of TGF-β1 and other related fibrotic genes as compared with untreated control group (p value ≥ 0.05), confirming that the observed results were attributed to the effect of TGF-β1 siRNA on the mRNA level of TGF-β1.
Cell cycle analysis
Analyzing the cell cycle of fibroblast cells, 24 h after transfection showed significant (p value < 0.05) differences between control and TGF-β1 siRNA NP-transfected group. As indicated in Fig. 6, the number of cells in S-phase was significantly (p value < 0.01) increased in TGF-β1 siRNA NP-treated group as compared with the control group representing the S-phase arrest and prevention of fibroblasts to enter into mitosis and proliferation phases.
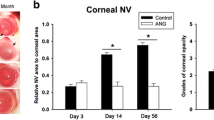
Animal study
Results from animal studies showed a promising potential of topical TGF-β1 siRNA NPs after corneal alkaline burn injuries. The histological evaluation confirmed the in vitro findings (Table 2; Fig. 7). TGF-β1 siRNA NP-treated group showed minor changes 21 days post-treatment which was comparable with the healthy cornea (p value ≥ 0.05) with no angiogenesis, irregular fibrosis, or myofibroblasts accumulation with significant superiority as compared with betamethasone-treated cornea (p value < 0.05). Only minor inflammation (number of PMN was less than 10 in × 1000 magnification) was detected in TGF-β1 siRNA NP-treated cornea. The histological changes in betamethasone and burned cornea with no treatment were moderate to severe with marked inflammation, angiogenesis, and fibrosis. Betamethasone-treated group exhibited twice the number of PMN [11,12,13,14,15,16,17,18,19,20] in comparison with TGF-β1 siRNA NP-treated cornea with one to two vessels and fibrosis at × 1000 magnification.
Histologic findings from endothelial cells (CD34+ cells) stained with anti-CD34+ secondary Ab (a′), α-SMA stained with anti-α-SMA secondary Ab (b′), irregular collagen deposition and irregular fibrosis stained with trichrome (c′), and PMN cells stained with H&E (d′) 21 days post-injury (×1000 magnification). Healthy subject: (A). TGF-β1 siRNA NP-treated group. Few sparse PMNs, slight stromal fibrosis, and rare blood vessels in injured stroma; (B). Positive control group (betamethasone-treated). Moderate neutrophilic infiltration and fibrosis with occasional CD34+ cells in stroma; (C) and negative control groups. Severe inflammation, marked fibrosis, and frequent CD34+ cells in stroma; (D). Vessels and α-SMA-positive cells indicated in brown shine as labeled with secondary antibody. Collagen fiber deposition demonstrated in blue color, and PMN nucleuses are shown in purple
Discussion
Corneal chemical burn is a disable situation in which patient vision will be lost. TGF-β1, as the most important inflammatory growth factor along with PDGF, can accelerate the differentiation of myofibroblasts as the most important cause of cornea transparency loss after corneal chemical burns [42,43,44]. ECM deposition in cornea and angiogenesis are two other causes of vision loss in patients during corneal damages [45]. The TGF-β1, as initiator of inflammatory fibrosis cascades, regulates other downstream cytokines and growth factors such as PGDF and VEGF [46, 47]. Efficient inhibition of key regulators of fibrosis cascades immediately after corneal chemical burns can preserve the patient eyesight. Several studies have been performed regarding stem cell and limbal cell implantation to maintain the patient eyesight after corneal injuries. However, there is a lack of efficient topical therapeutics to be applied immediately after corneal chemical injuries for suppressing fibrosis. siRNA strategies are novel nucleic acid-based therapeutics inspired from natural-occurring RNA interference (RNAi) process which is employed in an efficient and selective manner to suppress the targeted gene [23, 48]. Despite the high potential use of siRNA therapeutics, its clinical application is limited mainly due to its short half-life in vivo and poor transport across the cell membrane. However, packaging siRNA within nanoparticles has proven to protect nucleotides from the complex biological environment by increasing its stability and preventing RNase cleavage [49]. In this study, TGF-β1, as a key regulator of fibrotic cascades after corneal chemical burns, was down-regulated by TGF-β1 siRNA loaded in PEI NPs. PEI and its derivatives are used in many studies for siRNA and gene delivery [33, 50, 51]. Actually, poor transfection efficiency of non-viral vectors for corneal cells is a limiting factor in the development of non-viral gene therapy for corneal diseases. PEI, as a polymer with high transfection efficiency, is investigated for corneal gene delivery in some research. The mentioned studies demonstrated complete safety of PEI at optimized concentrations. PEI-DNA nanoparticles are reported to be efficient vector for delivering genes into corneal cells without compromising cellular proliferation, phenotype, or viability [52,53,54]. Ocular application of PEI/Cy3 siRNA NPs revealed to have higher transfection efficiency as compared with Lipofectamine 2000 or EntransterTM-in vivo [53]. The PEI complexation of siRNA into PEI/siRNA NPs provides a non-viral nucleic acid delivery platform that has been shown efficacious in other pathological models, especially in tumors. PEIs are positively charged polymers that form non-covalent complexes with nucleic acids, thus protecting siRNAs from degradation, mediating cellular uptake, and efficiently promoting lysosomal protection and escape into the cytoplasm. The efficiency and safety of PEI complex with gene/siRNA at the concentration used in the experiments are confirmed through several studies [55, 56]. Even infusion of PEI/siRNA NPs does not affect the integrity of ependymal cells and brain parenchyma [57]. The results obtained here was in accordance with previous studies considering PEI safety and efficiency. TGF-β1 siRNA was loaded in minimum amount of PEI (5 μg) which had the ability to condense the siRNA and transfect the primary fibroblasts with siRNA that was efficient as Lipofectamine without any detectable toxicity even after 48 h. Moreover, the NPs demonstrated acceptable stability considering their low zeta potential. Previously, it was shown that neutral-charged PEI NPs (through substitution of the primary amino groups of PEI with neutral hydrazine groups) do not only exhibited favorable biocompatibility, stability, and cell internalization efficiency in vitro but also allowed significant tissue uptake and gene silencing in zebra-fish heart in vivo [58]. These observations demonstrated that the tested PEI-siRNA NPs are safe for future development. Due to high cationic charge, the branched polymers exhibit high transfection efficiency, and particularly PEI of molecular weight of 25 kDa is considered a gold standard in gene delivery. The application of PEI in vivo promises to take the polymer-based vector to the next level wherein it can undergo clinical trials and subsequently could be used for delivery of therapeutics in humans [59]. Furthermore, simple production of PEI NPs is in favor for pharmaceutical production. The potential benefits of TGF-β1 down-regulation for corneal wound healing through anti-sense or siRNA are confirmed in vitro and ex vivo [60, 61]. In the present study, the in vitro model was designed in which inflammation-related fibrosis cascades were up-regulated in isolated fibroblasts through IL-6 addition. IL-6 modulates the proliferation and differentiation of myofibroblasts through induction of TGF-β1 and α-SMA gene expressions [62, 63]. IL-6, as modulatory cytokine, at concentration as low as 1 ng/mL, could induce α-SMA mRNA, whereas concentrations of 10 and 50 ng/mL showed a progressive decrease of α-SMA gene expression [62]. After induction of inflammatory fibrosis cascades in fibroblasts cells, the TGF-β1 siRNA NPs, at final concentration of 60 nM, exhibited an efficient down-regulation of TGF-β1 gene. PDGF and VEGF were also suppressed by TGF-β1 siRNA after 24 h. It seems that the secretion of PDGF and VEGF from fibroblasts was related to TGF-β1 secretion. The data was confirmed through previous studies in which they revealed that VEGF and TGF-β1 both induce angiogenesis [64, 65]. In a study performed by Sriram et al., triple siRNA was used to suppress the multiple inflammatory cascades after corneal injury without evaluating the potency of each siRNA to suppress inflammation and fibrosis [38]. The obtained results demonstrated that TGF-β1 siRNA, alone, could efficiently suppress other fibrotic/angiogenic cascades. In fact, PDGF and VEGF genes were efficiently down-regulated by TGF-β1 siRNA without any need for other medications. Furthermore, the TGF-β1 siRNA inhibited the production of Col type I and Fn by fibroblasts and myofibroblasts. Col type I and Fn are the major ECM components secreted from myofibroblasts that are considered the second cause of light scattering after corneal injuries [66]. α-SMA, the filamentous structure in differentiated myofibroblasts, is the first and major cause of light scattering after corneal injury [45]. Down-regulation of α-SMA by TGF-β1 siRNA is valuable in clinical investigations. Moreover, the NPs demonstrated to have anti-proliferative effect on fibroblasts through S-phase arrest which prevented cells to enter into mitosis phase.
Although, there are limited number of studies evaluating the effect of TGF-β down-regulation on corneal fibrosis. However, the efficiency of topical application of these biopharmaceutical products as simple eye drop has not yet been investigated [37, 38, 67]. In most of the studies, for in vivo consideration of corneal benefits of biopharmaceutical products, subconjunctival injection has been used or designated delivery systems for topical gene delivery are facing with challenges regarding NP chemical synthesis which limits their pharmaceutical production [68,69,70]. In the present study, topical application of NPs was used to evaluate in vivo efficiency of the siRNA NPs. The in vivo results were also excellently introduced with TGF-β1 siRNA loaded in PEI NPs as a potent anti-fibrotic/anti-angiogenic therapeutic. The siRNA was successfully delivered to the damaged cornea through PEI NPs, and the histological evaluation was comparable with the previous data obtained by subconjunctival injection of TGF-βR2 anti-sense oligonucleotide [37]. Murine model of cornea alkaline burn was completely cured by a three-time-a-day topical application of TGF-β1 siRNA NPs. Even after 1 week post-treatment, the cornea was completely treated. In the negative control group, a propagated hyphema was observed. Hyphema is an ocular emergency in which a blood pool develops in the front chamber of the eye [71]. Hyphema can enhance the ocular pressure and also increase the thickness of the cornea [72, 73]. Hyphema was developed at day 7 and persisted until day 21 in the negative control group. In the TGF-β1 siRNA NP-treated group, hyphema dis not developed due to inflammation prevention that can inhibit further damages. Histological investigations revealed that TGF-β1 siRNA NPs could prevent the differentiation of myofibroblasts and the irregular fibrosis beside from angiogenesis and inflammation as compared with positive and negative control groups. After 21 days, there was minor inflammation in the TGF-β1 siRNA NP-treated cornea while all other aspects of histologic damages reached the basement as was observed in healthy subjects. TGF-β1 siRNA NPs demonstrated excellent anti-fibrotic and anti-scarring properties after corneal chemical burns. Furthermore, the mentioned system would be considered a potent anti-angiogenesis therapeutic. Although, effectiveness, stability, and specificity of siRNA are still in debate. However, the concentrations needed are also generally very low as compared with small molecule therapeutics (in the nM range), whereas as the present study indicates, the siRNA is efficacious even at 60 nM. Down-regulation of multiple cellular cascades by TGF-β1 siRNA NPs makes it as a potent, non-toxic therapeutic treatment to prevent corneal haze and fibrosis after corneal chemical injuries. The most important is that TGF-β1 siRNA NPs could be applied as a simple eye drop without any requirement for additional device or invasive methods for siRNA transfection.
Conclusion
TGF-β1 siRNA was loaded in PEI to suppress TGF-β1 gene as a key regulator of inflammation-related-fibrotic after corneal burns. TGF-β1 siRNA was efficiently loaded into positively charged PEI to make NPs. TGF-β1 siRNA NPs down-regulated the fibrotic and angiogenic genes in isolated human corneal fibroblasts, with fibroblasts anti-proliferative effect. Moreover, topical application of TGF-β1 siRNA NPs in murine model of corneal alkaline burn prevented the fibrosis and angiogenesis in a way that pathologic findings were almost the same in TGF-β1 siRNA NP-treated and healthy subjects. In conclusion, TGF-β1 siRNA NPs would be regarded as potent topical therapeutics for preventing corneal haze and angiogenesis after chemical injuries.
References
Fish R, Davidson RS. Management of ocular thermal and chemical injuries, including amniotic membrane therapy. Curr Opin Ophthalmol. 2010;21(4):317–21.
Mead MD, Colby KA. Evaluation and initial management of patients with ocular and adnexal trauma. Principles and practice of ophthalmology. Philadelphia: WB Saunders; 1994. p. 3361–82.
Igarashi J, Fukuda N, Inoue T, Nakai S, Saito K, Fujiwara K, et al. Preclinical study of novel gene silencer pyrrole-imidazole polyamide targeting human TGF-β1 promoter for hypertrophic scars in a common marmoset primate model. PLoS One. 2015;10(5):e0125295.
Singh V, Torricelli AA, Nayeb-Hashemi N, Agrawal V, Wilson SE. Mouse strain variation in SMA+ myofibroblast development after corneal injury. Exp Eye Res. 2013;115:27–30.
Wilson SE. Corneal myofibroblast biology and pathobiology: generation, persistence, and transparency. Exp Eye Res. 2012;99:78–88.
Singh V, Jaini R, Torricelli AA, Santhiago MR, Singh N, Ambati BK, et al. TGFβ and PDGF-B signaling blockade inhibits myofibroblast development from both bone marrow-derived and keratocyte-derived precursor cells in vivo. Exp Eye Res. 2014;121:35–40.
Kane C, Cartledge J, Dias P, Camelliti P, Yacoub M, Terracciano C. 17 cardiomyocytes influence fibroblast proliferation and α-smooth muscle actin expression via the secretion of paracrine mediators. Heart. 2014;100(Suppl 1):A6–7.
Jester JV, Brown D, Pappa A, Vasiliou V. Myofibroblast differentiation modulates keratocyte crystallin protein expression, concentration, and cellular light scattering. Invest Ophthalmol Vis Sci. 2012;53(2):770–8.
Jeon K-I, Kulkarni A, Woeller CF, Phipps RP, Sime PJ, Hindman HB, et al. Inhibitory effects of PPARγ ligands on TGF-β1-induced corneal myofibroblast transformation. Am J Pathol. 2014;184(5):1429–45.
Bochaton-Piallat M-L, Gabbiani G, Hinz B. The myofibroblast in wound healing and fibrosis: answered and unanswered questions. F1000Research. 2016;5 https://doi.org/10.12688/f1000research.8190.1.
Reneker LW, Bloch A, Xie L, Overbeek PA, Ash JD. Induction of corneal myofibroblasts by lens-derived transforming growth factor β1 (TGFβ1): a transgenic mouse model. Brain Res Bull. 2010;81(2–3):287–96.
Cheng W, Xu R, Li D, Bortolini C, He J, Dong M, et al. Artificial extracellular matrix delivers TGFb1 regulating myofibroblast differentiation. RSC Adv. 2016;6(26):21922–8.
Biernacka A, Dobaczewski M, Frangogiannis NG. TGF-β signaling in fibrosis. Growth Factors. 2011;29(5):196–202.
Jaguin M, Fardel O, Lecureur V. AhR-dependent secretion of PDGF-BB by human classically activated macrophages exposed to DEP extracts stimulates lung fibroblast proliferation. Toxicol Appl Pharmacol. 2015;285(3):170–8.
Shah R, Reyes-Gordillo K, Arellanes-Robledo J, Lechuga CG, Hernández-Nazara Z, Cotty A, et al. TGF-β1 up-regulates the expression of PDGF-β receptor mRNA and induces a delayed PI3K-, AKT-, and p70S6K-dependent proliferative response in activated hepatic stellate cells. Alcohol Clin Exp Res. 2013;37(11):1838–48.
Maguire MG, Stark WJ, Gottsch JD, Stulting RD, Sugar A, Fink NE, et al. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Ophthalmology. 1994;101(9):1536–47.
Ma Y, Xu Y, Xiao Z, Yang W, Zhang C, Song E, et al. Reconstruction of chemically burned rat corneal surface by bone marrow-derived human mesenchymal stem cells. Stem Cells. 2006;24(2):315–21.
Gomes JAP, dos Santos MS, Cunha MC, de Nadai Barros J, de Sousa LB. Amniotic membrane transplantation for partial and total limbal stem cell deficiency secondary to chemical burn. Ophthalmology. 2003;110(3):466–73.
Sriram S, Gibson D, Robinson P, Tuli S, Lewin AS, Schultz G. Reduction of corneal scarring in rabbits by targeting the TGFB1 pathway with a triple siRNA combination. Adv Biosci Biotechnol. 2013;4(10):47–55.
Tovey J, Gronkiewicz KM, Giuliano EA, Siddiqui S, Sharma A, Brooke JL, et al. Role of cellular kinases and Smads in the modulation of SAHA-mediated corneal fibrosis inhibition. Invest Ophthalmol Vis Sci. 2014;55(13):5147.
Chen M, Matsuda H, Wang L, Watanabe T, Kimura MT, Igarashi J, et al. Pretranscriptional regulation of TGF-β1 by PI polyamide prevents scarring and accelerates wound healing of the cornea after exposure to alkali. Mol Ther. 2010;18(3):519–27.
Zahir-Jouzdani F, Mahbod M, Soleimani M, Vakhshiteh F, Arefian E, Shahosseini S, et al. Chitosan and thiolated chitosan: novel therapeutic approach for preventing corneal haze after chemical injuries. Carbohydr Polym. 2018;179:42–9.
Montgomery MK, Xu S, Fire A. RNA as a target of double-stranded RNA-mediated genetic interference in Caenorhabditis elegans. Proc Natl Acad Sci. 1998;95(26):15502–7.
Rand TA, Petersen S, Du F, Wang X. Argonaute2 cleaves the anti-guide strand of siRNA during RISC activation. Cell. 2005;123(4):621–9.
Semple SC, Akinc A, Chen J, Sandhu AP, Mui BL, Cho CK, et al. Rational design of cationic lipids for siRNA delivery. Nat Biotechnol. 2010;28(2):172–6.
Gary DJ, Puri N, Won Y-Y. Polymer-based siRNA delivery: perspectives on the fundamental and phenomenological distinctions from polymer-based DNA delivery. J Control Release. 2007;121(1):64–73.
Liu X, Howard KA, Dong M, Andersen MØ, Rahbek UL, Johnsen MG, et al. The influence of polymeric properties on chitosan/siRNA nanoparticle formulation and gene silencing. Biomaterials. 2007;28(6):1280–8.
Song WJ, Du JZ, Sun TM, Zhang PZ, Wang J. Gold nanoparticles capped with polyethyleneimine for enhanced siRNA delivery. Small. 2010;6(2):239–46.
Watanabe K, Harada-Shiba M, Suzuki A, Gokuden R, Kurihara R, Sugao Y, et al. In vivo siRNA delivery with dendritic poly (L-lysine) for the treatment of hypercholesterolemia. Mol BioSyst. 2009;5(11):1306–10.
Hughes J, Yadava P, Mesaros R. Liposomal siRNA delivery. In: Weissig V, editor. Liposomes: methods and protocols, volume 1: pharmaceutical nanocarriers; 2010. p. 445–59.
Heyes J, Palmer L, Bremner K, MacLachlan I. Cationic lipid saturation influences intracellular delivery of encapsulated nucleic acids. J Control Release. 2005;107(2):276–87.
Urban-Klein B, Werth S, Abuharbeid S, Czubayko F, Aigner A. RNAi-mediated gene-targeting through systemic application of polyethylenimine (PEI)-complexed siRNA in vivo. Gene Ther. 2005;12(5):461–6.
Merkel OM, Beyerle A, Librizzi D, Pfestroff A, Behr TM, Sproat B, et al. Nonviral siRNA delivery to the lung: investigation of PEG− PEI polyplexes and their in vivo performance. Mol Pharm. 2009;6(4):1246–60.
Tiyaboonchai W, Woiszwillo J, Sims RC, Middaugh CR. Insulin containing polyethylenimine–dextran sulfate nanoparticles. Int J Pharm. 2003;255(1):139–51.
Shahnaz G, Perera G, Sakloetsakun D, Rahmat D, Bernkop-Schnürch A. Synthesis, characterization, mucoadhesion and biocompatibility of thiolated carboxymethyl dextran–cysteine conjugate. J Control Release. 2010;144(1):32–8.
Thakur A, Fitzpatrick S, Zaman A, Kugathasan K, Muirhead B, Hortelano G, et al. Strategies for ocular siRNA delivery: potential and limitations of non-viral nanocarriers. J Biol Eng. 2012;6(1):7.
Nakamura H, Siddiqui SS, Shen X, Malik AB, Pulido JS, Kumar NM, et al. RNA interference targeting transforming growth factor-beta type II receptor suppresses ocular inflammation and fibrosis. Mol Vis. 2004;10(6):703–11.
Sriram S, Robinson P, Pi L, Lewin AS, Schultz G. Triple combination of siRNAs targeting TGFβ1, TGFβR2, and CTGF enhances reduction of collagen I and smooth muscle actin in corneal fibroblaststriple siRNAs reduce scarring gene expression. Invest Ophthalmol Vis Sci. 2013;54(13):8214–23.
Hosseinzadeh H, Atyabi F, Dinarvand R, Ostad SN. Chitosan-pluronic nanoparticles as oral delivery of anticancer gemcitabine: preparation and in vitro study. Int J Nanomedicine. 2012;7(1):1851–63.
Strober W. Trypan blue exclusion test of cell viability. Curr Protoc Immunol. 2001;3(10) https://doi.org/10.1002/0471142735.ima03bs21.
Kahn C, Young E, Lee IH, Rhim J. Human corneal epithelial primary cultures and cell lines with extended life span: in vitro model for ocular studies. Invest Ophthalmol Vis Sci. 1993;34(12):3429–41.
Untergasser G, Gander R, Lilg C, Lepperdinger G, Plas E, Berger P. Profiling molecular targets of TGF-β1 in prostate fibroblast-to-myofibroblast transdifferentiation. Mech Ageing Dev. 2005;126(1):59–69.
Trojanowska M. Role of PDGF in fibrotic diseases and systemic sclerosis. Rheumatology. 2008;47(suppl 5):v2–4.
Netto MV, Mohan RR, Sinha S, Sharma A, Dupps W, Wilson SE. Stromal haze, myofibroblasts, and surface irregularity after PRK. Exp Eye Res. 2006;82(5):788–97.
Jester JV, Budge A, Fisher S, Huang J. Corneal keratocytes: phenotypic and species differences in abundant protein expression and in vitro light-scattering. Invest Ophthalmol Vis Sci. 2005;46(7):2369–78.
Gotzmann J, Fischer A, Zojer M, Mikula M, Proell V, Huber H, et al. A crucial function of PDGF in TGF-β-mediated cancer progression of hepatocytes. Oncogene. 2006;25(22):3170–85.
Araújo F, Rocha M, Mendes J, Andrade S. Atorvastatin inhibits inflammatory angiogenesis in mice through down regulation of VEGF, TNF-α and TGF-β1. Biomed Pharmacother. 2010;64(1):29–34.
Elbashir SM, Harborth J, Lendeckel W, Yalcin A, Weber K, Tuschl T. Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. Nature. 2001;411(6836):494–8.
Rodriguez M, Lapierre J, Ojha CR, Kaushik A, Batrakova E, Kashanchi F, et al. Intranasal drug delivery of small interfering RNA targeting Beclin1 encapsulated with polyethylenimine (PEI) in mouse brain to achieve HIV attenuation. Sci Rep. 2017;7(1):1862.
Grayson ACR, Doody AM, Putnam D. Biophysical and structural characterization of polyethylenimine-mediated siRNA delivery in vitro. Pharm Res. 2006;23(8):1868–76.
Kang J-H, Tachibana Y, Kamata W, Mahara A, Harada-Shiba M, Yamaoka T. Liver-targeted siRNA delivery by polyethylenimine (PEI)-pullulan carrier. Bioorg Med Chem. 2010;18(11):3946–50.
Sharma A, Rodier JT, Tandon A, Klibanov AM, Mohan RR. Attenuation of corneal myofibroblast development through nanoparticle-mediated soluble transforming growth factor-β type II receptor (sTGFβRII) gene transfer. Mol Vis. 2012;18:2598.
Li Z, Duan F, Lin L, Huang Q, Wu K. A new approach of delivering siRNA to the cornea and its application for inhibiting herpes simplex keratitis. Curr Mol Med. 2014;14(9):1215–25.
Donnelly KS, Giuliano EA, Sharma A, Tandon A, Rodier JT, Mohan RR. Decorin-PEI nanoconstruct attenuates equine corneal fibroblast differentiation. Vet Ophthalmol. 2014;17(3):162–9.
Höbel S, Koburger I, John M, Czubayko F, Hadwiger P, Vornlocher HP, et al. Polyethylenimine/small interfering RNA-mediated knockdown of vascular endothelial growth factor in vivo exerts anti-tumor effects synergistically with bevacizumab. J Gene Med. 2010;12(3):287–300.
Werth S, Urban-Klein B, Dai L, Höbel S, Grzelinski M, Bakowsky U, et al. A low molecular weight fraction of polyethylenimine (PEI) displays increased transfection efficiency of DNA and siRNA in fresh or lyophilized complexes. J Control Release. 2006;112(2):257–70.
Helmschrodt C, Höbel S, Schöniger S, Bauer A, Bonicelli J, Gringmuth M, et al. Polyethylenimine nanoparticle-mediated siRNA delivery to reduce α-Synuclein expression in a model of Parkinson’s disease. Mol Therapy-Nucleic Acids. 2017;9:57–68.
Wang F, Gao L, Meng L-Y, Xie J-M, Xiong J-W, Luo Y. A neutralized noncharged polyethylenimine-based system for efficient delivery of siRNA into heart without toxicity. ACS Appl Mater Interfaces. 2016;8(49):33529–38.
Patnaik S, Gupta KC. Novel polyethylenimine-derived nanoparticles for in vivo gene delivery. Expert Opin Drug Deliv. 2013;10(2):215–28.
Sriram S, Gibson DJ, Robinson P, Pi L, Tuli S, Lewin AS, et al. Assessment of anti-scarring therapies in ex vivo organ cultured rabbit corneas. Exp Eye Res. 2014;125:173–82.
Zheng D, Song T, Zhongliu X, Wu M, Liang J, Liu Y. Downregulation of transforming growth factor-β type II receptor prohibit epithelial-to-mesenchymal transition in lens epithelium. Mol Vis. 2012;18:1238–46.
Gallucci RM, Lee EG, Tomasek JJ. IL-6 modulates alpha-smooth muscle actin expression in dermal fibroblasts from IL-6-deficient mice. J Investig Dermatol. 2006;126(3):561–8.
Seong GJ, Hong S, Jung S-A, Lee J-J, Lim E, Kim S-J, et al. TGF-β-induced interleukin-6 participates in transdifferentiation of human Tenon’s fibroblasts to myofibroblasts. Mol Vis. 2009;15:2123.
Ferrari G, Cook BD, Terushkin V, Pintucci G, Mignatti P. Transforming growth factor-beta 1 (TGF-β1) induces angiogenesis through vascular endothelial growth factor (VEGF)-mediated apoptosis. J Cell Physiol. 2009;219(2):449–58.
Viñals F, Pouysségur J. Transforming growth factor β1 (TGF-β1) promotes endothelial cell survival during in vitro angiogenesis via an autocrine mechanism implicating TGF-α signaling. Mol Cell Biol. 2001;21(21):7218–30.
Torricelli AA, Wilson SE. Cellular and extracellular matrix modulation of corneal stromal opacity. Exp Eye Res. 2014;129:151–60.
Chang Y, Wu X-Y. JNK1/2 siRNA inhibits transforming-growth factor-β1-induced connective tissue growth factor expression and fibrotic function in THSFs. Mol Cell Biochem. 2010;335(1–2):83–9.
Kim B, Tang Q, Biswas PS, Xu J, Schiffelers RM, Xie FY, et al. Inhibition of ocular angiogenesis by siRNA targeting vascular endothelial growth factor pathway genes: therapeutic strategy for herpetic stromal keratitis. Am J Pathol. 2004;165(6):2177–85.
Campochiaro P. Potential applications for RNAi to probe pathogenesis and develop new treatments for ocular disorders. Gene Ther. 2006;13(6):559–62.
Tong YC, Chang SF, Liu CY, Kao WWY, Huang CH, Liaw J. Eye drop delivery of nano-polymeric micelle formulated genes with cornea-specific promoters. J Gene Med. 2007;9(11):956–66.
Shihadeh WA, Ritch R, Liebmann JM. Hyphema occurring during selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging Retin. 2006;37(5):432–3.
Najjar DM, Rapuano CJ, Cohen EJ. Descemet membrane detachment with hemorrhage after alkali burn to the cornea. Am J Ophthalmol. 2004;137(1):185–7.
Walker NJ, Foster A, Apel AJ. Traumatic expulsive iridodialysis after small-incision sutureless cataract surgery. J Cataract Refract Surg. 2004;30(10):2223–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zahir-Jouzdani, F., Soleimani, M., Mahbod, M. et al. Corneal chemical burn treatment through a delivery system consisting of TGF-β1 siRNA: in vitro and in vivo. Drug Deliv. and Transl. Res. 8, 1127–1138 (2018). https://doi.org/10.1007/s13346-018-0546-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-018-0546-0