Abstract
Background and aim
Type 2 diabetes is prone to numerous comorbidities resulting from complex mechanisms involving hyperglycemia, insulin resistance, low-grade inflammation and accelerated atherogenesis. The purpose of the present study was to investigate these disorders and their associated risk factors according to patient sex in a population of type 2 diabetics in North-Eastern Morocco.
Methods
This study was conducted in a medical analysis laboratory over a 1-year period from 01/10/2018 to 01/10/2019. This epidemiological study was carried out on 830 subjects aged 18 and over. Quantitative variables were expressed as means ± standard deviation, and qualitative variables as frequencies and percentages. Hypothesis tests used to compare means and proportions were Student’s t-test and Chi-square test of independence, respectively. Logistic regression was used to predict risk factors for each diabetes.
Results
830 patients were surveyed. 95.66% had diabetes-related comorbidities. Hypertension (23.7%), nephropathy (18.19%), dyslipidemia (14.82%), thyroid dysfunction (10.72%), cataract (10.12%), diabetic foot (7.23%), ketoacidosis (6.27%), retinopathy (3.49%), and skin disorders (2.77%) were observed. Sex was associated with dyslipidemia (p = 0.025), hypertension (p = 0.032) and retinopathy (p = 0.029). Uncontrolled blood sugar, unbalanced lipid profile, age, physical activity, obesity, smoking, and alcohol consumption were risk factors with differential involvement in the occurrence of the mentioned pathologies.
Conclusions
The results of our study showed that a significant proportion of the population suffers from diabetic comorbidities. To meet this challenge, further research is needed to identify the mechanisms of action of these factors, to control them and combat diabetogenic environments by setting up adapted educational programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, the number of people with diabetes has surged from 108 million in 1980 to 422 million in 2014, according to the World Health Organization. This increase has been most pronounced in low- and middle-income countries, and the Eastern Mediterranean region has been disproportionately impacted. In Morocco, diabetes affects 12.4% of adults, and causes over 12,000 deaths annually, with an additional 32,000 deaths attributable to complications of high blood sugar [1].
Multimorbidity, comorbidity, and diabetes complications are medical concepts that relate to different aspects of health and associated medical conditions. Multimorbidity refers to the presence of two or more chronic diseases (or medical conditions) in the same individual. These chronic diseases can be independent of each other and are not necessarily related to a primary disease. Comorbidity refers to the simultaneous presence of two or more diseases or medical conditions in the same individual. However, unlike multimorbidity, comorbidities are often related or associated in some way. For example, type 2 diabetes is frequently associated with obesity and high blood pressure due to common risk factors and similar underlying mechanisms. Diabetes complications are health problems that result from poorly controlled diabetes over time [2, 3].
Type 2 diabetes is managed through weight loss, a balanced diet, and regular physical activity. If these measures are not enough, antidiabetic drugs may be prescribed, starting with tablets and then injections if needed. Treatment aims to reduce the risk of complications by keeping blood sugar levels within the normal range [4]. Without proper management, diabetes can lead to life-threatening complications (nephropathy, neuropathy, retinopathy, coronary heart disease, myocardial infarction, peripheral arterial disease, and stroke), or alternatively, it increases the risk of comorbidities or even multimorbidities (hypertension, obesity, dyslipidemia, kidney disease, eye problems, skin disorders, thyroid dysfunction, ketoacidosis, diabetic foot), which can be expensive, debilitating, and can significantly reduce quality of life [5,6,7].
Sex largely influences the epidemiology, pathophysiology, clinical manifestations, disease progression, and response to treatment of type 2 diabetes (T2DM). Therefore, sex is an important determinant of health that should be considered when planning preventive-curative personalized medicine approaches. Globally, the prevalence of T2DM is increasing, particularly among women [8, 9].
Many health organizations are urging that a sex dimension be integrated into all phases of biomedical research, to improve both the quality and societal relevance of scientific studies [10]. Multiple studies have shown that men with diabetes are more likely to develop microvascular complications (nephropathy, neuropathy, and retinopathy) than women. However, women with diabetes are at higher risk for macrovascular complications (coronary heart disease, myocardial infarction, peripheral arterial disease, and stroke), while the consequences of macrovascular complications may be greater for women [11,12,13,14]. Despite the sex disparities in the occurrence of diabetes-related disorders described earlier, the evidence is incomplete, and studies sometimes contradict each other [15, 16]. This study aims to investigate sex differences in diabetes-related comorbidities and sex-specific correlates of associated risk factors among type 2 diabetics in North-Eastern Morocco. We hypothesize that: (1) Diabetes-related complications/comorbidities differ between men and women. (2) Demographic (age and education), health (alcohol intake, smoking, exercise, depressive symptoms, body mass index, and hypertension), and diabetes (diabetes duration and HbA1c) risk factors are associated with diabetes.
Participants and methods
Study participants
This epidemiological study was conducted in Nador, Morocco, from October 1, 2018, to October 1, 2019, at a private medical laboratory. The study enrolled 830 men and women aged 18 or older. After obtaining approval from the Ministry of Health delegation in Nador to conduct the study in a medical analysis laboratory, we explained the study’s purpose to the laboratory director, a medical biologist. Participants were type 2 diabetic patients who visited the laboratory to monitor their blood glucose levels, and whose blood glucose levels were ≥ 7 mmol/L on two occasions. With the help of a pre-trained team of two nurses and the medical biologist, we explained the study’s purpose to the patients. Those who volunteered signed the consent form and completed a survey. We collected sociodemographic (age, marital status, education level, and employment status) and clinical information. Exclusion criteria were applied, and the following participants were excluded: pregnant or breastfeeding women, children, patients with type 1 diabetes, and patients with gestational diabetes. Appropriate precautions were taken in accordance with the Declaration of Helsinki [17].
Data collection and laboratory measurement
For each fasting participant (12 h of fasting), the laboratory nurse collected two vials of blood from a vein at the elbow using a loose tourniquet and single-use needles. The blood was collected into vacuum-sealed tubes: one dry tube (lithium heparin-glass) for fasting blood glucose and one EDTA tube (ethylene-diamine-tetra-acetic acid) for glycated hemoglobin. Fasting blood glucose was measured 5 min after decantation and 10 min after centrifugation using an automated biochemistry machine. HbA1c was measured in whole blood using a high-performance liquid chromatography machine.
To assess participants’ anthropometry, researchers measured their height, weight, and waist circumference (WC). Participants wore light clothing and removed their shoes while researchers measured their body weight and height to the nearest 0.1 kg and 0.1 cm, respectively. Body mass index (BMI) was calculated by dividing weight in kilograms by the square of height in meters. Researchers collected coexisting conditions according to patient’s clinical history and past medical records (including systemic hypertension, cataract, dyslipidemia, diabetic foot, ketoacidosis, diabetic retinopathy, diabetic kidney disease, skin damage, thyroid dysfunction).
Operational definitions
Hypertension
We defined hypertension as blood pressure exceeding 140/90 mmHg, consistent with World Health Organization guidelines [18]. In our study, participants were classified as hypertensive if they reported a prior diagnosis, had a documented systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg, or were taking prescribed antihypertensive medication.
Dyslipidemia
Dyslipidemia refers to abnormal levels of lipids in the blood, such as cholesterol and triglycerides. The main types include hypercholesterolemia (total cholesterol exceeding 2 g/L (5 mmol/L) or LDL cholesterol exceeding 1.60 g/L (4.1 mmol/L)), hypertriglyceridemia (triglycerides exceeding 1.50 g/L (1.7 mmol/L)), and low HDL cholesterol (below 0.40 g/L (1.7 mmol/L), often called “good cholesterol”) [19]. In our study, we classified individuals as dyslipidemic if they met WHO criteria for at least one of these lipid disorders and had a documented diagnosis with medication prescribed for the condition.
Diabetic kidney disease
Diabetic nephropathy is a serious complication of diabetes that damages the kidneys over time due to high blood sugar [20, 21]. This damage prevents the kidneys from filtering waste and fluids properly, leading to protein leakage and potential kidney failure. The study was based on the medical records of patients, all of whom had been confirmed by their treating physician to have diabetic nephropathy and all stages of diabetic nephropathy have been considered.
Thyroid dysfunction
Refers to any problem that affects the normal functioning of the thyroid gland. This can include excessive or insufficient production of thyroid hormones, which can lead to various symptoms and health issues [22]. A patient with thyroid dysfunction is defined by an abnormal TSH level (normal TSH range is between 0.4 and 4.5 mIU/L) or by taking a thyroid medication.
Cataract
Cataracts are the opacification of the crystalline lens inside the eye, causing a reduction in near and distance vision that cannot be improved by optical correction. The only treatment is surgery. Patients who have undergone cataract surgery after being diagnosed with diabetes have been confirmed as cases.
Diabetic retinopathy
Diabetic retinopathy is a serious complication of diabetes characterized by damage to the blood vessels of the retina, which can lead to vision loss. Symptoms may include blurred vision, dark spots or difficulty seeing at night [23, 24]. Our study was based on patients with confirmed diabetic retinopathy followed regularly by an ophthalmologist.
Skin damage
Up to half of diabetic patients experience skin problems. These can be broadly categorized into three groups: those specific to diabetes (e.g., lipoid necrobiosis), complications arising from the disease itself (like fungal infections), and issues related to diabetes medications [25]. Positive cases for skin lesions focused on patients who reported having skin problems or having consulted a dermatologist about them.
Diabetic ketoacidosis
A serious complication of diabetes characterized by hyperglycemia, hyperketonemia, and metabolic acidosis [26]. It is less common in type 2 diabetes, but may appear in case of infection, physical or emotional stress, poor diabetes management, or lack of insulin. All diabetic patients with a history of hospitalization for this complication were included.
Obesity
A person is considered obese if his or her BMI exceeds 25 kg/m2, so we have merged overweight and obesity.
Regular physical activity
A person was regularly physically active if he or she exercised at least twice a week at a physical activity that increased heart and breathing rates.
Controlled blood glucose
A person was in regular control of his/her blood glucose if he/she measures his/her blood glucose themselves or in a dedicated health center at least twice a month.
Statistical analysis
SPSS version 26 and WHO Anthroplus version 1.04 software were used to analyze the data. Continuous variables were presented as means and standard deviations, while categorical variables were summarized as frequencies and percentages. The independent Student’s t -test was used for continuous variables and Chi-square tests were used to assess significant differences between categorical variables. Multivariate backward regression model was used to determine significant risk factors associated with hypertension. We report crude odds ratios (COR), adjusted odds ratios (AOR), and their respective 95% confidence intervals (CI) as the measure of association.
Results
Characteristics of participants
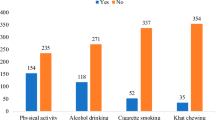
Researchers recruited 830 participants for the study, consisting of 27.2% men and 72.8% women. The average age of the participants was 59.06 ± 14.51 years, with the age group 55–70 years being the most prevalent at 44%. In terms of educational level, 64.94% were illiterate, with 62.8% of them being women. Among the participants, 90.2% were unemployed, with 68% of them being women. Additionally, 86.4% of the sample were married. Regarding anthropometric measurements, the mean weight for men was 81.25 ± 13.68 kg, while for women, it was 79.8 ± 15.45 kg. The average height for women was 162.85 ± 11.05 cm, and for men, it was 167.7 ± 10.67 cm. Body mass index calculations revealed a prevalence of obesity among type 2 diabetics at 47.9%, with 36.9% of them being women. Underweight was estimated at 5.4%, with a predominance of women at 2.4%. Concerning diabetes characteristics, the population had a mean fasting blood glucose of 2.32 ± 0.78 g/L, with a minimum blood glucose of 0.46 g/L and a maximum blood glucose of 5.55 g/L. The mean blood glucose level was 2.25 ± 0.708 g/L in men and 2.34 ± 0.81 g/L in women. The mean glycosylated hemoglobin was 9.43 ± 2.14 in women and 9.25 ± 2.38 in men. The duration of diabetes was 7.51 ± 3.95 years for women and 7.55 ± 4.07 years for men. Concerning self-medication habits, 4.45% of women used traditional self-medication, while only 1.08% of men used traditional medicines to treat diabetes. In terms of toxic habits, 7.7% of diabetics were smokers, including 6.86% of men and 0.81% of women. Additionally, 2.28% were regular alcohol consumers, with 1.92% being men and 0.36% being women. The results are summarized in Table 1.
Association between diabetes comorbidities and patient sex
The study revealed that only 4.34% (n = 36) of patients had no comorbidities related to diabetes. Hypertension was the most prevalent, affecting 23.37% of patients (n = 194), including 153 women and 41 men. Diabetic nephropathy had a prevalence of 18.19% (n = 151), with 107 cases in women and 44 in men. Dyslipidemia was present in 14.82% of the sample (n = 118), with 76 cases in women and 42 in men. Thyroid dysfunction affected 10.72% (n = 89) of patients, including 68 women and 21 men. Cataracts were diagnosed in 10.12% (n = 84) of the patients, with 59 women and 25 men affected. Diabetic foot was found in 7.23% (n = 60) of the cases, including 45 women and 15 men. Ketoacidosis was present in 6.27% (n = 52) of patients, with 39 women and 13 men affected. Diabetic retinopathy concerned 3.49% (n = 29) of the patients, including 18 women and 11 men. Skin involvement was diagnosed in 2.77% (n = 23), including 16 women and 7 men.
The Chi-square test revealed a significant association between patient sex and three diseases: dyslipidemia (p = 0.025), arterial hypertension (p = 0.032), and diabetic retinopathy (p = 0.029) Table 2.
Factors associated with diabetes comorbidities by sex
A multivariate logistic regression analysis was conducted to identify predictors of pathologies previously linked to sex. To enhance the results of the logistic regression, categorical variables were converted into dummy variables (dichotomized). Outliers were examined and it was determined that all residual values were randomly distributed within the range of − 3 to 3 z-scores.
The exploration of risk factors associated with diabetic multimorbidity revealed several findings. Table 3 illustrates the risk factors associated with dyslipidemia. The probability of dyslipidemia increased with advancing age for both sexes. Men above 71 years were approximately three times AOR = 2.8, (95% CI, 1.1–3.2) more at risk of dyslipidemia compared to participants aged 18–25 years, for women the risk is less pronounced AOR = 2.09, (95% CI, 1.55–4.59). The study found that both single and divorced men were more likely to have dyslipidemia compared to married men. Specifically, single men had a roughly two-fold greater risk (2.06 times higher), while divorced men had a 1.5-fold increased risk. Interestingly, marital status was not a risk factor for dyslipidemia in women. High levels of total cholesterol were positively associated with dyslipidemia, the odds ratio in males was AOR = 1.85, (95% CI: 0.24–3.82) and in females AOR = 1.28, (95% CI: 0.44–6.7). The adjusted odds ratio showed that people with high LDL-C level were 1.59 times for men AOR = 1.28, (95% CI: 0.44–6.7) and 1.75 times for women AOR = 1.28, (95% CI: 0.44–6.7) more likely to suffer a dyslipidemia than those who had a normal LDL-C level. However, the high level of triglyceride and low level of HDL-C showed no association with dyslipidemia. Body mass index above 25 kg/m2 was associated with dyslipidemia for both sexes. Being overweight or obese increased the odds of dyslipidemia by AOR = 1.96, (95% CI: 0.8–6.18) for men and AOR = 1.97, (95% CI: 0.86–4.51) in women compared to having normal BMI. Regular physical activity appears to be a protecting factor against dyslipidemia in both men AOR = 0.41, (95% CI: 0.06–1.2) and women AOR = 0.68, (95% CI: 0.56–1.83). In the adjusted model, current alcohol consumption was significantly associated with dyslipidemia for men only. Indeed, regular drinkers were approximately two times AOR = 1.96, (95% CI, 0.78–5.26) more at risk of dyslipidemia compared to non-alcohol drinkers.
Increasing age is associated with a significantly higher likelihood of developing hypertension. Compared to young adults (aged 18–25), the odds of hypertension were nearly doubled (AOR = 1.91, 95% CI: 0.23–3.50) for those aged 56–70. This risk further increased for individuals aged 71 and above, who were four times more likely to develop hypertension (AOR = 8.23, 95% CI: 4.09–16.55). Similar trends were observed in women, with a slight increase in risk compared to men. Women aged 56–70 had an odds ratio of 2.50 (95% CI: 1.02–4.10), while those aged 71 and above had an even higher risk (AOR = 4.50, 95% CI: 2.50–6.30). Having high total cholesterol levels was associated with an increased likelihood of hypertension in both men and women. Compared to those with normal cholesterol, men with high cholesterol had an odds ratio of 1.21 (95% CI: 0.85–1.73) for hypertension. Similarly, women with high cholesterol had an odds ratio of 1.13 (95% CI: 0.63–1.91). Men with high triglycerides had a one-and-a-half times greater risk of hypertension (AOR = 1.59, 95% CI: 1.15–2.58) compared to men with normal triglyceride levels. Similarly, women with high triglycerides were also at increased risk, with an odds ratio of 1.36 (95% CI: 0.74–2.01) compared to their counterparts. Obese men were found to have a three-fold increased risk of hypertension (AOR = 3.18, 95% CI: 0.83–6.91) compared to non-obese men. Similarly, obese women exhibited a nearly three-fold greater likelihood of hypertension (AOR = 2.61, 95% CI: 1.3–4.4) compared to their non-obese counterparts. Regular blood glucose control was associated with a significant reduction in hypertension risk. Men with regular blood glucose control had a 61% lower risk (AOR = 0.27, 95% CI: 0.08–1.35) compared to those without regular control. Similarly, women with regular blood glucose control experienced a 67% reduction in risk (AOR = 0.33, 95% CI: 0.14–1.11). Regular physical activity was associated with a significant reduction in hypertension risk. Engaging in physical activity lowered the odds of hypertension by 56% (AOR = 0.27, 95% CI: 0.06–1.46) for men. Similarly, women who regularly participated in sports experienced a 68% reduction in hypertension risk (AOR = 0.32, 95% CI: 0.18–1.43). Alcohol consumption and smoking were found to be significant risk factors for dyslipidemia, but only among men. Men who were both regular drinkers and regular smokers had roughly double the risk of dyslipidemia (AOR = 2.04, 95% CI: 1.7–5.02) and (AOR = 1.89, 95% CI: 0.78–5.26) respectively, compared to those who did not drink or smoke regularly. Table 4.
Table 5 presents the association between various risk factors and diabetic retinopathy, analyzed using multiple logistic regression. When controlling for other variables, high total cholesterol emerged as a significant risk factor for both men and women. Men with high total cholesterol had an odds ratio (AOR) of 2.0 (95% CI: 1.46–2.65) for developing diabetic retinopathy, while the AOR for women was 1.6 (95% CI: 1.12–2.15). Another factor is obesity. Men with obesity have an adjusted odds ratio (AOR) of 3.07 (95% CI: 0.72–9.93) for developing diabetic retinopathy, while women with obesity have an AOR of 2.50 (95% CI: 0.26–5.33). Uncontrolled blood sugar is a further risk factor for diabetic retinopathy. Men with uncontrolled blood sugar had an AOR of 0.69 (95% CI: 0.37–2.24), while women with uncontrolled blood sugar had an even higher AOR of 0.22 (95% CI: 0.03–1.07). Sedentary behavior also increases the risk of diabetic retinopathy. Men with sedentary lifestyles have an AOR of 0.61 (95% CI: 0.25–0.95), and women with sedentary lifestyles have an AOR of 0.55 (95% CI: 0.22–1.92). A risk factor that concerns men only is alcohol consumption, as alcoholics are twice 1.95 (95% CI: 0.67–4.25) as likely to develop diabetic retinopathy.
Discussion
The present study was conducted in patients with non-insulin-dependent type 2 diabetes. A total of 830 patients were enrolled, comprising 27.2% men and 72.8% women. The predominance of women in our study (72.8% of the cases) can be attributed to the higher utilization of healthcare services by women with diabetes in comparison to men. This, in turn, reflects their tendency to monitor and manage their blood glucose levels more consistently [27]. Another study by El Alami et al. revealed a high prevalence of type 2 diabetes among Moroccan women highlighting specific risk factors that contribute to this high prevalence. These include obesity, a sedentary lifestyle, and socio-economic factors such as low levels of education and precarious socio-economic status [28]. A staggering 64.94% of the study participants were illiterate, with women disproportionately affected (nearly 63% of illiterate participants were women). This lack of education translated into high unemployment, with 90.2% of participants jobless. Women again faced greater challenges, making up almost 68% of the unemployed. This difference can be explained by several factors, including unequal access to education and the persistence of cultural traditions that favor the education of boys [29]. Almost all patients included in the study (96.38%) had T2DM-related multimorbidities. This value considerably exceeds those found internationally. Indeed, among 11,357 people with T2DM from 33 countries followed for three years, Arnold and her team reported in their study that 31.5% of patients had at least one microvascular complication, and 16.6% at least one macrovascular complication [30]. Furthermore, hypertension is the most prevalent comorbidity of T2DM in our population, with a rate of 23.37%. Our results concerning the prevalence of arterial hypertension remain lower than those found regionally and internationally. Oulad Sayad and colleagues reported a prevalence of 45% in Central Morocco [31], in Saudi Arabia Ziyad et al. reported a prevalence of 71.68% [32], in Jordan 75% [33], in the United States 75.4% [34]. The authors of many of these studies stated that blood pressure was not controlled, and the discovery of hypertension was fortuitous. Diabetic kidney disease in our population was estimated at 18.19%, which is lower than the worldwide prevalences of 38.8% in China [35], 34.4% in India [36], 45.7% in Egypt [37], in the USA, prevalence varies from 30 to 40% [38]. Dyslipidemia affects 14.8% of patients. This prevalence of dyslipidemia remains well below international rates, ranging from 81.5% in Ethiopia [39] to 88.9% in Thailand [40]. 10.72% of our patients had thyroid dysfunction, which is similar to studies in the literature [41, 42]. Compared with cataracts, diabetic retinopathy has a low prevalence, at 10.12% and 3.49% respectively. These rates remain relatively similar to the results found on an international scale, for cataracts a study including 42,469 diabetic adults from six countries (China, Ghana, India, Mexico, Russia, South Africa) has reported rates between 1.7% and 13.3% [43]. For diabetic retinopathy, the Global Burden of Disease Study on diabetic retinopathy in 2010 reported a worldwide prevalence of 34% [44], and 27.6% was reported in Japan [45]. It has been reported in the literature that ketoacidosis occurs in 1–29% of cases in type 2 diabetics. Our study is no exception to the general rule, with a prevalence of 6.27% [46, 47]. Diabetic foot ulcers (DFUs) are a common complication of diabetes that develops over time, especially when diabetes is not well controlled. Approximately one in five to three in ten people with diabetes worldwide will develop a DFU at some point in their lives [48, 49]. Concerning diabetic dermopathy, it is observed in 0.2 to 55% of diabetic patients [50]. In our population, the prevalence was estimated at 2.77%, which remains low, and this could be explained by the darker skin color of the residents of the study area, located in Eastern Morocco, which makes dermopathies difficult to discover and to seek treatment from a specialist.
Disparities in prevalences between countries could be explained by inequalities in socioeconomic status (education, income, employment), access to healthcare services (access, affordability, quality), environmental variables (exposure to a toxic environment, diabetogenic environment) [51], or even by the methodology used to identify pathologies. Indeed, some authors use patient medical records or admission records for surgical procedures, while others rely on patient self-reporting.
The Chi-square test revealed a significant difference in the prevalence of dyslipidemia between diabetic men and women (p = 0.025). This finding is confirmed by other studies. In fact, the prevalence of dyslipidemia was higher in women than in men [52, 53]. Investigations in Korea [54], and India [55] have also reported gender differences trends. Mechanisms underlying this gender related trend of prevalence in dyslipidemia between genders are not completely clear. Possible explanations for this trend of increase in females include menopausal transition and loss of estrogen, which might act as a trigger factor and enhance metabolic dysfunction [56, 57]. The factors identified as being significantly associated with dyslipidemia in multivariate logistic regression were older age in both sexes. This result is in line with previous studies. The possible reason, according to these authors, could be age-related degenerative effects. However, the exact mechanism has yet to be elucidated [58,59,60]. Our study also revealed a significant association between marital status and dyslipidemia. However, there is no clear explanation for single men being more likely to have dyslipidemia than married men. Although this may be due to the higher prevalence of unhealthy eating habits (excessive consumption of fat and fast food) that accompany divorce, separation, and widowhood, and which are more common in men than in women [61]. Multivariate analysis reported a significant association between LDL-C and dyslipidemia. Moreover, the t-test revealed a statistically significant difference between LDL-C levels in men and women and given that dyslipidemia is defined by the four components of the lipid profile, including LDL-C. This factor is thought to be involved in the difference in the prevalence of the complication between men and women [62]. In our study, obese men and women seem to be at the same level of risk of developing dyslipidemia, twice as much as normal weight subjects. Obesity is a major risk factor for dyslipidemia, a condition characterized by abnormal levels of fats (lipids) in the blood. Around 60–70% of obese individuals are estimated to have dyslipidemia and there are several ways obesity can contribute to dyslipidemia: increased production of triglycerides and LDL by the liver, Decreased HDL cholesterol levels or even Insulin resistance [63]. Regular physical activity appears to be a protecting factor against dyslipidemia in both men and women. Epidemiological studies provide clear evidence that physical activity can reduce cardiovascular morbidity and mortality by improving lipid profiles [64].
We also found a significant difference in the occurrence of hypertension between the two sexes (p = 0.032). We therefore agree with the earlier findings of Azra et al. in Iran, who reported a higher risk of hypertension in men than in women [65], and those of European clinicians indicating a high risk of hypertension and associated cardiovascular disease in males [66]. The odds of hypertension were nearly doubled for those aged 56–70. This risk further increased for individuals aged 71 and above, who were four times more likely to develop hypertension. Similar trends were observed in women, with a slight increase in risk compared to men. Several studies have attempted to explain this finding. Indeed, after menopause, the risk of hypertension in women increases, rapidly reaching that of men and even surpassing it from the seventh decade of life. The mechanisms by which estrogen deficiency increases the risk of hypertension have been extensively studied. These mechanisms are clearly multifaceted. However, it has not been clearly demonstrated that menopausal hormone treatment reduces blood pressure levels. The factors that cause hypertension to become more prevalent after the seventh decade in women are also certainly of multifactorial origin, notably a lower level of cardiovascular risk in women than in men, all other things being equal, with a higher life expectancy and a survivor effect [67]. Tobacco consumption was associated with hypertension. Several studies have reported tobacco as a risk factor associated with high blood pressure [68, 69]. Tobacco includes nicotine, which causes vasoconstriction of blood vessels [25]. It also activates the sympathetic nervous system, producing an increase in heart rate and blood pressure [70]. While other studies have found a significant association between smoking in women and hypertension [71], our study found no significant association between smoking and the onset of hypertension. Patients with a higher BMI were much more likely to develop hypertension than those with a normal BMI. This result is in line with several previous studies [28, 72, 73]. Research on laboratory animals and humans suggests that altered renal natriuresis due to physical compression of the kidneys by fat in and around them plays an important role in increasing blood pressure [74]. Patients (of both sexes) with high HbA1c levels—the other side of poorly controlled blood sugar levels—are more likely to suffer from hypertension. This result is in line with the findings of numerous other studies [75, 76]. This relationship is attributable to excess glucose in the blood, which traps lipoproteins, leading to atheroma formation and increased blood pressure [77]. Alcohol is also a risk factor for arterial hypertension, which increases blood levels of angiotensin II, known as a powerful vasoconstrictor [78]. The reason why women are exempt from this action could be explained by light or intermittent alcohol consumption, which would have no or even beneficial effects on blood pressure [79].
A significant difference was also observed in the occurrence of diabetic retinopathy (DR). This result is consistent with a study including 12,766 in China and reporting a high risk of DR in women. The mechanisms by which the female sex contributes to the prevalence of DR in T2DM patients are still unknown [80]. An abnormally balanced lipid profile is a risk factor for the development of diabetic retinopathy. Our study revealed a significant association between high total cholesterol levels and diabetic retinopathy. Our results concur with those of Rema et al. which demonstrated that average cholesterol, triglyceride and non-HDL levels were higher in patients with DR than in those without [81]. Obesity has been shown to be a risk factor for DR, in line with the meta-analysis by Zhu et al. who, by analyzing 13 prospective cohort studies on obesity and DR risk, demonstrated the existence of a significant adverse effect on the incidence of DR [82]. Uncontrolled blood sugar is another risk factor for diabetic retinopathy in both sexes. These findings are in line with the findings of Hammoudi and his team [83]. However, regular physical activity in men appears to play a protective role against diabetic retinopathy. Ren and his team examined data from 22 studies and showed that physical activity was found to have a protective association with DR via its hypoglycemic action [84]. Evidence for the involvement of alcohol in the incidence of DR is contradictory. Our study revealed a significant association between alcohol consumption and diabetic retinopathy only in men. This association was explained by the negative action of alcohol on the inflammatory response and oxidative stress could be affected by alcohol and are significantly associated with the risk of diabetic retinopathy [85]. The exclusive effect in men only may be explained by the protective effect of low or moderate alcohol consumption on the incidence of DR [86].
Since no study is exempt from unavoidable limitations. Ours has several limitations. Firstly, it included a higher number of female participants compared to males, this was mainly due to the very high prevalence rate among women, approximately double that of men, achieving a perfect balance might not have been feasible. To mitigate this bias, we conducted sex-stratified analysis to examine the risk factors for males and females separately. However, our findings highlight the importance of future research with a more balanced sex ratio to strengthen the generalizability of the results for both men and women with diabetes. Secondly, throughout the study, we used the notion of “sex” in the biological sense of the term, rather than “gender,” which is a socio-cultural construct. Comparing our results with those of other authors who have used the term “gender” in its socio-cultural dimension could potentially affect the generalizability of our findings. Therefore, in future research, questionnaires should include both “gender” and “sex.” Secondly, the presence of confounding factors alongside the risk factors associated with specific pathologies could introduce bias into the outcomes. For example, the literature suggests a higher risk of cataract occurrence after the age of 60. In future investigations, it may be advisable to focus on younger diabetic populations to address this issue.
Conclusion
The results of our study indicate a significant prevalence of diabetic multimorbidities within the population. To address this issue effectively, it is imperative to implement a combination of preventive and curative strategies. This should include efforts to combat risk factors such as hyperlipidemia, alcohol consumption, obesity, and sedentary lifestyles. Further research is warranted to better understand the mechanisms by which these factors operate and to develop strategies for controlling them, ultimately reducing diabetogenic environments. Achieving this goal can be realized through the establishment of educational programs and adherence to hygienic and dietary measures.
Data availability
The data is available for a reasonable purpose.
References
Diabetes, retrieved from: https://www.paho.org/fr/sujets/diabete#:~:text=Le%20diab%C3%A8te%20est%20une%20maladie,de%20sucre%20dans%20le%20sang. (accessed 27 March 2023)
Gulbech Ording A, Toft SH. Concepts of comorbidities, multiple morbidities, complications, and their clinical epidemiologic analogs. Clin Epidemiol. 2013;5:199.
Cicek M, Buckley J, Pearson-Stuttard J, et al. Characterizing multimorbidity from type 2 diabetes: insights from clustering approaches. Endocrinol Metab Clin North Am. 2021;50:531.
Elsayed NA, Aleppo G, Aroda VR, et al. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023;46:S19-40.
Cho Y, Park HS, Huh BW, et al. Prevalence and risk of diabetic complications in young-onset versus late-onset type 2 diabetes mellitus. Diabetes Metab. 2022;48:101389.
Van Dieren S, Beulens JWJ, Van Der Schouw YT, et al. The global burden of diabetes and its complications: an emerging pandemic. Eur J Cardiovasc Prev Rehabil. 2010;17:3–8.
Suh J, Choi Y, Oh S, et al. Association between early glycemic management and diabetes complications in type 1 diabetes mellitus: a retrospective cohort study. Prim Care Diabetes. 2023;17:60–7.
Mauvais-Jarvis F, Bairey Merz N, Barnes PJ, et al. Sex and gender: modifiers of health, disease, and medicine. Lancet. 2020;396:565–82.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37:278–316.
Heidari S, Babor TF, De Castro P, et al. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev. 2016;1:1–9.
Neugarten J, Golestaneh L, Kolhe NV. Sex differences in acute kidney injury requiring dialysis. BMC Nephrol. 2018;19:1–7.
Kostev K, Rathmann W. Diabetic retinopathy at diagnosis of type 2 diabetes in the UK: a database analysis. Diabetologia. 2013;56:109–11.
Pop-Busui R, Lu J, Lopes N, et al. Prevalence of diabetic peripheral neuropathy and relation to glycemic control therapies at baseline in the BARI 2D cohort. J Peripher Nerv Syst. 2009;14:1–13.
Hotaling JM, Sarma AV, Patel DP, et al. Cardiovascular autonomic neuropathy, sexual dysfunction, and urinary incontinence in women with type 1 diabetes. Diabetes Care. 2016;39:1587–93.
Peters SAE, Huxley RR, Woodward M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia. 2014;57:1542–51.
Regensteiner JG, Golden S, Anton B, et al. Sex differences in the cardiovascular consequences of diabetes mellitus. Circulation. 2015;132:2424–47.
https://www.wma.net/fr/policies-post/declaration-dhelsinki-de-lamm-principes-ethiques-applicables-a-la-recherche-medicale-impliquant-des-etres-humains/. Accessed 13 Aug 2024
Hypertension. https://www.who.int/news-room/fact-sheets/detail/hypertension. Accessed 11 May 2024
Hdia ZB, Abdelaziz AB, Melki S, et al. EPIDEMIOLOGIE DE LA DYSLIPIDEMIE EN TUNISIE.Etude Hammam Sousse Sahloul Heart Study (HSHS 3)*. Tunis Med. 2022;100:323.
Park CW. Diabetic kidney disease: from epidemiology to clinical perspectives. Diabetes Metab J. 2014;38:252.
Fougere É. La néphropathie diabétique. Actual Pharm. 2020;59:55–6.
Benzian Z, Benabadji N, Merad MS, et al. Dysfonctions thyroïdiennes chez les diabétiques type 2 suivis à la consultation externe du service d’endocrinologie du CHU d’Oran. Ann Endocrinol (Paris). 2017;78:263–4.
Schlienger JL. Complications du diabète de type 2. Presse Med. 2013;42:839–48.
Ciulla TA, Amador AG, Zinman B. Diabetic retinopathy and diabetic macular edema: pathophysiology, screening, and novel therapies. Diabetes Care. 2003;26:2653–64.
Senet P, Chosidow O. Manifestations cutanéomuqueuses du diabète. EMC—Endocrinologie—Nutrition. 2010;7:1–7.
Jouini S, Aloui A, Slimani O, et al. Profils épidémiologiques des acidocétoses diabètiques aux urgences. Pan Afr Med J. 2019. https://doi.org/10.11604/PAMJ.2019.33.322.17161.
Shalev V, Chodick G, Heymann AD, et al. Gender differences in healthcare utilization and medical indicators among patients with diabetes. Public Health. 2005;119:45–9.
El Alami H, Haddou I, Benaadi G, et al. Prevalence and risk factors of chronic complications among patients with type 2 diabetes mellitus in Morocco: a cross-sectional study. Pan Afr Med J. 2022. https://doi.org/10.11604/PAMJ.2022.41.182.25532.
Mansuy M, Werquin P. Moroccan youth and employment: gender differences. J Edu Work Moroccan Youth employm: Gend Diff. 2018. https://doi.org/10.1080/13639080.2018.1541504.
Arnold SV, Khunti K, Tang F, et al. Incidence rates and predictors of microvascular and macrovascular complications in patients with type 2 diabetes: results from the longitudinal global discover study. Am Heart J. 2022;243:232–9.
Oulad Sayad N, Ouhdouch F, Diouri A. P108 Profil épidémiologique et clinique des diabétiques de Demnat (région de Marrakech). Diabetes Metab. 2009;35:A53–4.
Almalki ZS, Albassam AA, Alhejji NS, et al. Prevalence, risk factors, and management of uncontrolled hypertension among patients with diabetes: a hospital-based cross-sectional study. Prim Care Diabetes. 2020;14:610–5.
Salameh AB, Hyassat D, Suhail A, et al. The prevalence of hypertension and its progression among patients with type 2 diabetes in Jordan. Annals of Med Surg. 2022. https://doi.org/10.1016/J.AMSU.2021.103162.
Huyser KR, Rockell J, Jernigan VBB, et al. Sex differences in diabetes prevalence, comorbidities, and health care utilization among American Indians living in the Northern Plains. Curr Dev Nutr. 2020;4:42.
Kung K, Chow KM, Hui EM-T, et al. Prevalence of complications among Chinese diabetic patients in urban primary care clinics: a cross-sectional study. BMC Fam Pract. 2014;15:8.
Hussain S, Habib A, Najmi AK. Limited knowledge of chronic kidney disease among Type 2 diabetes mellitus patients in India. Int J of Environ Res Public Health. 2019;16:1443.
Elhefnawy KA, Elsayed AM. Prevalence of diabetic kidney disease in patients with type 2 diabetes mellitus. Egypt J Int Med. 2019;31:149–54.
Gupta S, Dominguez M, Golestaneh L. Diabetic kidney disease: an update. Med Clin North Am. 2023;107:689–705.
Abdissa D, Hirpa D. Dyslipidemia and its associated factors among adult diabetes outpatients in West Shewa zone public hospitals, Ethiopia. BMC Cardiovasc Disord. 2022;22:39.
Narindrarangkura P, Bosl W, Rangsin R, et al. Prevalence of dyslipidemia associated with complications in diabetic patients: a nationwide study in Thailand. Lipids Health Dis. 2019. https://doi.org/10.1186/S12944-019-1034-3.
Palma CC, Pavesi M, Nogueira VG, et al. Prevalence of thyroid dysfunction in patients with diabetes mellitus. Diabetol Metab Syndr. 2013;5:58.
Biondi B, Kahaly GJ, Robertson RP. Thyroid dysfunction and diabetes mellitus: two closely associated disorders. Endocr Rev. 2019;40(3):789–824. https://doi.org/10.1210/er.2018-00163.
Pizzol D, Veronese N, Quaglio G, et al. The association between diabetes and cataract among 42,469 community-dwelling adults in six low- and middle-income countries. Diabetes Res Clin Pract. 2019;147:102–10.
Wong TY, Sun J, Kawasaki R, et al. Guidelines on diabetic eye care: the international council of ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125:1608–22.
Kawasaki R, Kitano S, Sato Y, et al. Factors associated with non-proliferative diabetic retinopathy in patients with type 1 and type 2 diabetes: the Japan diabetes complication and its prevention prospective study (JDCP study 4). Diabetol Int. 2019;10:3–11.
Dabelea D, Rewers A, Stafford JM, et al. Trends in the prevalence of ketoacidosis at diabetes diagnosis: the SEARCH for diabetes in youth study. Pediatrics. 2014;133:e938.
Virdi N, Poon Y, Abaniel R et al. Prevalence, Cost, and Burden of Diabetic Ketoacidosis. https://home.liebertpub.com/dia 2023;25:S75–84.
McDermott K, Fang M, Boulton AJM, et al. Etiology, epidemiology, and disparities in the burden of diabetic foot ulcers. Diabetes Care. 2023;46:209–21.
Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376:2367–75.
George SMC, Walton S. Diabetic dermopathy. Br J Diabet. 2014;14:95–7.
Hill-Briggs F, Adler NE, Berkowitz SA, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. 2021;44:258–79.
Boadu WIO, Anto EO, Frimpong J, et al. Prevalence, knowledge, and lifestyle-associated risk factors of dyslipidemia among Ghanaian type-2 diabetes mellitus patients in rural and urban areas: a multicenter cross-sectional study. Health Sci Rep. 2023;6:e1475.
Abdissa D, Hirpa D. Dyslipidemia and its associated factors among adult diabetes outpatients in West Shewa zone public hospitals. Ethiopia BMC Cardiovasc Disord. 2022;22:1–8.
Boo S, Yoon YJ, Oh H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: a cross-sectional analysis. Medicine. 2018. https://doi.org/10.1097/MD.0000000000013713.
Joshi SR, Anjana RM, Deepa M, et al. Prevalence of dyslipidemia in urban and rural India: the ICMR-INDIAB study. PLoS ONE. 2014. https://doi.org/10.1371/JOURNAL.PONE.0096808.
Lizcano F. Roles of estrogens, estrogen-like compounds, and endocrine disruptors in adipocytes. Front Endocrinol (Lausanne). 2022. https://doi.org/10.3389/FENDO.2022.921504.
Lizcano F, Guzmán G. Estrogen deficiency and the origin of obesity during menopause. Biomed Res Int. 2014. https://doi.org/10.1155/2014/757461.
Bekele S, Yohannes T, Eshete A, et al. Dyslipidemia and associated factors among diabetic patients attending Durame General Hospital in Southern Nations, Nationalities, and People’s Region. Diabetes Metab Syndr Obes. 2017;10:265–71.
Alzaheb RA, Altemani AH. Prevalence and associated factors of dyslipidemia among adults with type 2 diabetes mellitus in Saudi Arabia. Diabetes Metab Syndr Obes. 2020;13:4033–40.
Bayram F, Kocer D, Gundogan K, et al. Prevalence of dyslipidemia and associated risk factors in Turkish adults. J Clin Lipidol. 2014;8:206–16.
Vinther JL, Conklin AI, Wareham NJ, et al. Marital transitions and associated changes in fruit and vegetable intake: findings from the population-based prospective EPIC-Norfolk cohort. UK Soc Sci Med. 2016;157:120.
Russo G, Pintaudi B, Giorda C, et al. Age- and Gender-Related Differences in LDL-Cholesterol Management in Outpatients with Type 2 Diabetes Mellitus. Int J Endocrinol. 2015. https://doi.org/10.1155/2015/957105.
Vekic J, Zeljkovic A, Stefanovic A, et al. Obesity and dyslipidemia. Metabolism. 2018. https://doi.org/10.1016/j.metabol.2018.11.005.
Rhee EJ, Kim HC, Kim JH, et al. 2018 Guidelines for the management of dyslipidemia. Korean J Intern Med. 2019;34:723–71.
Ramezankhani A, Parizadeh D, Azizi F, et al. Sex differences in the association between diabetes and hypertension and the risk of stroke: cohort of the Tehran Lipid and glucose study. Biol Sex Differ. 2022;13:10.
Gerdts E, Sudano I, Brouwers S, et al. Sex differences in arterial hypertension a scientific statement from the ESC Council on Hypertension, the European Association of Preventive Cardiology, Association of cardiovascular nursing and allied professions, the ESC council for cardiology practice, and the ESC working group on cardiovascular pharmacotherapy. Eur Heart J. 2022;43:4777–88.
Connelly PJ, Currie G, Delles C. Sex differences in the prevalence, outcomes and management of hypertension. Curr Hypertens Rep. 2022;24(6):185–92.
Gao N, Liu T, Wang Y, Chen M, Yu L, Fu C, et al. Assessing the association between smoking and hypertension: smoking status, type of tobacco products, and interaction with alcohol consumption. Front Cardiovasc Med. 2023;10:1027988.
Li G, Wang H, Wang K, Wang W, Dong F, Qian Y, et al. The association between smoking and blood pressure in men: a cross-sectional study. BMC Public Health. 2017;17(1):797.
Cigarette smoking and hypertension - PubMed [Internet]. [cité 26 mars 2024]. Disponible sur: https://pubmed.ncbi.nlm.nih.gov/20550499/
Bowman TS, Gaziano JM, Buring JE, Sesso HD. A prospective study of cigarette smoking and risk of incident hypertension in women. J Am Coll Cardiol. 2007;50(21):2085–92.
Asresahegn H, Tadesse F, Beyene E. Prevalence and associated factors of hypertension among adults in Ethiopia: a community based cross-sectional study. BMC Res Notes. 2017. https://doi.org/10.1186/S13104-017-2966-1.
DeMarco VG, Aroor AR, Sowers JR. The pathophysiology of hypertension in patients with obesity. Nat Rev Endocrinol. 2014;10:364–76.
Hall JE, Do Carmo JM, Da Silva AA, et al. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991.
Mariye T, Girmay A, Tasew H, et al. Determinants of hypertension among diabetic patients in public hospitals of the Central Zone, Tigray, Ethiopia 2018: unmatched case-control study. Pan Afr Med J. 2019. https://doi.org/10.11604/PAMJ.2019.33.100.17094.
Heianza Y, Arase Y, Kodama S, et al. Fasting glucose and HbA1c levels as risk factors for the development of hypertension in Japanese individuals: Toranomon hospital health management center study 16 (TOPICS 16). J Hum Hypertens. 2015;29:254–9.
Katakami N. Mechanism of development of atherosclerosis and cardiovascular disease in diabetes mellitus. J Atheroscler Thromb. 2018;25:27–39.
Tsuji S, Kawano S, Michida T, et al. Ethanol stimulates immunoreactive endothelin-1 and -2 release from cultured human umbilical vein endothelial cells. Alcohol Clin Exp Res. 1992;16:347–9.
Mayl JJ, German CA, Bertoni AG, et al. Association of alcohol intake with hypertension in type 2 diabetes mellitus: the ACCORD trial. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2020. https://doi.org/10.1161/JAHA.120.017334.
Li M, Wang Y, Liu Z, et al. Females with type 2 diabetes mellitus are prone to diabetic retinopathy: a twelve-province cross-sectional study in China. J Diabetes Res. 2020. https://doi.org/10.1155/2020/5814296.
Rema M, Srivastava BK, Anitha B, Deepa R, Mohan V. Association of serum lipids with diabetic retinopathy in urban South Indians–the Chennai urban rural epidemiology study (CURES) eye study–2. Diabet Med J Br Diabet Assoc. 2006;23(9):1029–36.
Zhu W, Wu Y, Meng YF, Xing Q, Tao JJ, Lu J. Association of obesity and risk of diabetic retinopathy in diabetes patients. Medicine (Baltimore). 2018;97(32):e11807.
Hammoudi J, Bouanani NEH, Chelqi EH, et al. Diabetic retinopathy in the Eastern Morocco: different stage frequencies and associated risk factors. Saudi J Biol Sci. 2021;28:775–84.
Ren C, Liu W, Li J, et al. Physical activity and risk of diabetic retinopathy: a systematic review and meta-analysis. Acta Diabetol. 2019;56:823–37.
Srikanta AH, Kumar A, Sukhdeo SV, Peddha MS, Govindaswamy V. The antioxidant effect of mulberry and jamun fruit wines by ameliorating oxidative stress in streptozotocin-induced diabetic Wistar rats. Food Funct. 2016;7(10):4422–31.
Association between alcohol consumption and the risk of incident type 2 diabetes: a systematic review and dose-response meta-analysis - PubMed [Internet]. [cité 27 mars 2024]. Disponible sur: https://pubmed.ncbi.nlm.nih.gov/26843157/
Funding
Not available.
Author information
Authors and Affiliations
Contributions
IK: resources, SB: conceptualization, methodology, software, data analysis, writing, review and editing, validation; SD: methodology, writing, review and editing; AB: review and editing; MO: supervision and project administration.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Human rights statement
The study was conducted in accordance with the principles of the Declaration of Helsinki 1964 and later versions. Participants were informed of the purpose of the study, the potential risks and benefits, and their right to withdraw at any time. They gave their informed consent before participating in the study. Those who volunteered signed the consent form and were included in the study. Participants’ anonymity and privacy were respected at all times. Participants’ personal data were anonymized before analysis. The data collected was stored in a secure location and will only be accessible to authorized persons. This research study was conducted retrospectively from data obtained for clinical purposes. We consulted with the Ministry of Health delegation in Nador who determined that our study did not require ethical approval. Official authorization to conduct the study was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kenfaoui, I., Bouchefra, S., Daouchi, S. et al. The comorbidity burden of type 2 diabetes mellitus (T2DM): sex differences and associated factors among 830 cases in North-Eastern Morocco. Diabetol Int (2024). https://doi.org/10.1007/s13340-024-00750-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13340-024-00750-5