Abstract
Aims
We aimed to verify the usefulness of targeted next-generation sequencing (NGS) technology for diagnosing monogenic diabetes in a single center.
Methods
We designed an amplicon-based NGS panel targeting 34 genes associated with known monogenic diabetes and performed resequencing in 56 patients with autoantibody-negative diabetes mellitus diagnosed at < 50 years who had not been highly obese. By bioinformatic analysis, we filtered significant variants based on allele frequency (< 0.005 in East Asians) and functional prediction. We estimated the pathogenicity of each variant upon considering the family history.
Results
Overall, 16 candidate causative variants were identified in 16 patients. Among them, two previously known heterozygous nonsynonymous single-nucleotide variants associated with monogenic diabetes were confirmed as causative variants: one each in the GCK and WFS1 genes. The former was found in two independent diabetes-affected families. Two novel putatively deleterious heterozygous variants were also assumed to be causative from the family history: one frameshift and one nonsynonymous single-nucleotide variant in the HNF4A gene. Twelve variants remained as candidates associated with the development of diabetes.
Conclusion
Targeted NGS panel testing was useful to diagnose various forms of monogenic diabetes in combination with familial analysis, but additional ingenuity would be needed for practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monogenic diabetes is an uncommon form of diabetes mellitus caused by one or more defects in a single gene. It consists of many diseases that vary depending on the responsible gene, which have been classified into certain disease groups such as maturity-onset diabetes of the young (MODY), transient or permanent neonatal diabetes (TNDM or PNDM), and diabetes-associated syndromes [1, 2]. Many genes causative of monogenic diabetes have been identified so far; however, monogenic diabetes is not diagnosed in many cases because genetic testing for diabetes has not been commonly performed. Genetic analysis may help understand the pathological basis and provide prognostic or therapeutic suggestion based on previous findings on patients with monogenic diabetes.
To detect causative gene variants of monogenic diseases, Sanger sequencing has conventionally been used. However, this approach has the weakness of limited throughput capacity, besides being time-consuming and laborious for sequencing a large number of targets. In recent years, massively parallel DNA sequencing has become possible via the development of next-generation sequencing (NGS). Among the NGS methods, targeted resequencing as a multigene panel testing is the most cost-effective tool for simultaneous and rapid analyses of multiple target genes of interest. These advantages of multigene panel testing make it an efficient option for comprehensive DNA sequencing for the genetic diagnosis of known monogenic diseases.
To date, a few studies have used a targeted NGS approach as an initial genetic screening for known monogenic diabetes [3,4,5,6,7,8]. In many of those studies, multigene panel tests contributed to diagnosing mainly common types of MODY, including MODY3 and MODY2. Meanwhile, the other rare types of MODY, PNDM, or monogenic syndromic diabetes were hardly targeted and rarely diagnosed by methods relying on in silico analysis. In addition, the age of onset of monogenic diabetes varies from the neonatal period to middle age, so diagnostic tests may be valuable for both childhood-onset and adult-onset patients with diabetes. However, most of the previous studies did not document the age of onset about patients who had been diagnosed as any monogenic diabetes and the usefulness of the testing for each age group remains unclear. Against this background, this study was established to use an NGS panel in practice and verify its clinical usefulness for diagnosing various monogenic diabetes in a single center.
Materials and methods
Patients
In this study, 56 unrelated patients with diabetes mellitus who visited Yamagata University Hospital between June 6th, 2017, and March 31st, 2020, were enrolled based on the following criteria: diagnosed with diabetes at < 50 years, and adults with body mass index (BMI) < 28 kg/m2 or non-obese children. Patients with type 1 diabetes, pregnant women with diabetes, patients previously diagnosed with any form of monogenic diabetes, and patients with secondary diabetes whose cause was assumed not to be a specific genetic factor were excluded. Patients lacking a family history were included in this study because monogenic diabetes could be caused by de novo mutation or biallelic recessive variants.
The following clinical data were obtained from each patient: age at diagnosis of diabetes, age at genetic testing and diabetes duration, sex, BMI, treatment, symptoms, and diabetic microvascular and macrovascular complications. Biochemical parameters at genetic testing were measured in patients, such as fasting or postprandial plasma glucose, glycated hemoglobin (HbA1c), fasting serum C-peptide, and 24-h urinary C-peptide excretion. Oral glucose tolerance test or glucagon test was also performed on patients, if available.
Panel design and sequencing
The targeted NGS approach was performed using Ion AmpliSeq™ technology (Thermo Fisher Scientific, Cleveland, OH, USA) via amplicon-based sequencing. Pools of primer pairs as an NGS panel targeting 34 genes known to cause monogenic diabetes were created using the Ion AmpliSeq™ Custom DNA Panel (Thermo Fisher Scientific). Primers for all exons of the target genes and their flanking regions were designed using the Ion AmpliSeq™ Designer (Thermo Fisher Scientific). The target genes were as follows: 15 MODY genes (HNF4A, GCK, HNF1A, PDX1, HNF1B, NEUROD1, KLF11, CEL, PAX4, INS, BLK, ABCC8, KCNJ11, APPL1, RFX6), 14 non-MODY genes causing neonatal diabetes (EIF2AK3, FOXP3, GATA4, GATA6, GLIS3, IER3IP1, MNX1, NEUROG3, NKX2-2, PAX6, PLAGL1, PTF1A, SLC19A2, ZFP57), the PCBD1 gene causing recessively inherited diabetes with HNF1A-like phenotypes, and 4 genes associated with some genetic syndromes with diabetes (WFS1, INSR, TRMT10A, PPP1R15B). The target size was 129,265 bases and total amplicon number was 927, theoretically covering 95.0% of the target region (Table 1).
Genomic DNA was isolated from patients’ blood leukocytes. Target enrichment and NGS library construction were performed using Ion AmpliSeq™ Kit for Chef DL8 (Thermo Fisher Scientific), in accordance with the manufacturer’s instructions. Sequencing was performed using the NGS platform of the Ion PGM™ System (Thermo Fisher Scientific).
Bioinformatic analysis
Sequencing reads were run through two independent variant calling pipelines: BWA-SW (http://bio-bwa.sourceforge.net/)–Platypus (https://www.rdm.ox.ac.uk/research/lunter-group/lunter-group/platypus-a-haplotype-based-variant-caller-for-next-generation-sequence-data) and Bowtie 2 (http://bowtie-bio.sourceforge.net/bowtie2/)–GATK UnifiedGenotyper (https://gatk.broadinstitute.org/hc/en-us). In this procedure, reads were aligned to the reference genome GRCh38.p2 (Genome Reference Consortium Human Build 38 patch release 2, https://www.ncbi.nlm.nih.gov/assembly/GCF_000001405.28) and variants such as single-nucleotide variants (SNVs) and insertions and/or deletions (indels) of single or a few nucleotides were called. Then concordant variants detected by the two pipelines were annotated using the ANNOVAR program (http://annovar.openbioinformatics.org/).
Candidate causative variants were selected based on the following criteria: (1) variant allele frequency (VAF) lower than 0.005 in the East Asian population in the 1000 Genomes Database (http://www.internationalgenome.org/) and the Genome Aggregation Database (gnomAD) v2 or v3 (https://gnomad.broadinstitute.org/), and similarly in the Japanese genome reference panel Tohoku University Tohoku Medical Megabank Organization (ToMMo) 14KJPN (https://jmorp.megabank.tohoku.ac.jp/202112/variants); (2) nonsynonymous SNVs predicted to be functionally deleterious by a Combined Annotation Dependent Depletion (CADD, https://cadd.gs.washington.edu/) phred-like score of ≥ 20 or null variants such as nonsense or frameshift variants in a gene where loss of function (LOF) is a known mechanism of disease.
Variant confirmation
Visualized sequence reads were counted using Integrative Genomics Viewer (https://software.broadinstitute.org/software/igv/) and it was confirmed that the variant was in a region with a read depth of at least 20 × . To search for information about genomic variation and its relationship to phenotype/diseases, we referred to databases such as ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/) or the Human Gene Mutation Database (HGMD®, http://www.hgmd.cf.ac.uk/). To confirm domains and important sites of proteins and predict the functional impact of each variant, we referred to databases such as UniProtKB (https://www.uniprot.org/help/uniprotkb) or InterPro (https://www.ebi.ac.uk/interpro/).
For segregation analysis, pedigree information was obtained from the patient’s family, if available. NGS panel testing was also performed on the proband’s relatives who had given informed consent and agreed.
The pathogenicity of each candidate causative variant was estimated in accordance with the American College of Medical Genetics and Genomics (ACMG)/Association for Molecular Pathology (AMP) clinical variant interpretation guidelines [9]. A known variant that had previously been reported to cause monogenic diabetes was determined to be the causative variant. A novel variant classified as “pathogenic” or “likely pathogenic” by ACMG/AMP guidelines was also assumed to be causative if the patient’s clinical manifestations and segregation data were consistent with the LOF of the relevant gene. Sanger sequencing was performed to confirm the causative variants of patients and their relatives.
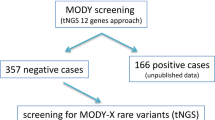
The overall workflow of the study pipeline is shown in supplementary Fig. S1.
Results
Clinical characteristics of the 56 participants are shown in Table 2. The median (range) age at genetic testing was 47 (4–75) years, and the age at the diagnosis of diabetes was 31 (3–49) years. Approximately one-quarter of all patients had been diagnosed with diabetes in their childhood or adolescence. The median BMI at genetic testing was 23 kg/m2. Over 80% of the patients had a family history of diabetes. All patients resided in Yamagata Prefecture, Japan; however, this was not necessarily their birthplace.
Overall, 82 synonymous SNVs, 89 nonsynonymous SNVs, and 1 indel were detected in the target regions for the 56 patients. After filtering by VAF and predicted deleteriousness, 15 nonsynonymous SNVs and 1 frameshift indel were selected as candidate causative variants.
Among these variants, 11 nonsynonymous SNVs identified in 11 patients had already existed in dbSNP (https://www.ncbi.nlm.nih.gov/snp/) regardless of whether they were clinically significant or not (Table 3). Regarding the phenotype–genotype relationships, Yorifuji et al. reported that a heterozygous nonsynonymous variant (NM_000162: c.1142 T > G [p.M381R]) in exon 9 of the GCK gene was supposed to cause MODY2 in Japanese patients based on in silico pathogenicity prediction and family segregation analysis [10]. In addition, Khanim et al. summarized various variants associated with Wolfram syndrome, including a heterozygous nonsynonymous variant (NM_001145853: c.2020G > A [p.G674R]) in exon 8 of the WFS1 gene, based on previous case reports [11]. The other nine known nonsynonymous SNVs were supposed to have the possibility of affecting gene function, but there was no reported evidence of an association with diabetes mellitus.
The remaining four nonsynonymous SNVs and one frameshift indel found in five patients were novel variants (Table 4). None of these variants was found in any databases and their effects on phenotypes were unknown. However, these four nonsynonymous SNVs were in functionally important residues/domains of the proteins, so there was the possibility that the amino acid substitutions affected protein function. A novel heterozygous complex deletion-insertion (delins) variant [NM_000457: c.474_477delinsTGTCCTGCAGGACAGCAGGCTCCT (p.A158Afs)] in exon 4 of the HNF4A gene was identified, in which 4 nucleotides were substituted along with another 24 nucleotides showing modification of the reading frame. This frameshift variant resulted in gross protein rearrangements that might lead to protein dysfunction.
Clinical information of 16 cases with candidate causative variants is shown in supplementary Table S1 and pedigree trees of the cases are shown in supplementary Fig. S2.
After assessing the pathogenicity of each candidate causative variant considering the annotated information, and each patient’s clinical manifestations and family history, four variants in five patients were classified as causative variants. These five patients were consequently diagnosed as having monogenic diabetes (cases 2, 3, 5, 12, and 15), as shown in Table 5.
Case 2 was a 4-year-old boy diagnosed with diabetes at the age of 3, and case 3 was a 14-year-old boy diagnosed with diabetes at the age of 14. Both of these cases were suspected to involve diabetes inherited in an autosomally dominant manner on the paternal side. They similarly showed mild fasting hyperglycemia with slightly low levels of C-peptide, whereas postprandial blood glucose levels were near-normal and C-peptide showed secretory responses in the glucagon test. These findings were consistent with typical clinical features of MODY2. A heterozygous GCK p.M381R variant identically detected in both cases was previously reported to be associated with MODY2, as mentioned above. Therefore, we diagnosed both case 2 and case 3 with MODY2. These two patients resided fairly close to each other, but we could not find any clear familial relationship between them.
Case 5 was a 52-year-old woman who had suffered from diabetes since she was 12 years old, and she had received multiple daily insulin injections for type 1 diabetes mellitus. She had no family history of diabetes. She was referred to the neurology department for evaluation of dysarthria, lightheadedness, cognitive impairment, and nocturia that had occurred around the age of 50. At that time, the previous diagnosis of type 1 diabetes mellitus was negated because the patient was negative for pancreatic autoantibodies. She had suffered from poor vision from the age of 42, the cause of which was found to be bilateral optic nerve atrophy, whereas she had no diabetic retinopathy. She was also diagnosed with sensorineural deafness, ataxia, and dementia associated with atrophy of brainstem and cerebellum, along with neurogenic bladder. Given the significantly reduced C-peptide, she was diagnosed as being insulin-dependent. These various symptoms generally match Wolfram syndrome. A heterozygous WFS1 p.G674R variant was previously reported in several patients and families affected by Wolfram syndrome, in compound heterozygotes combined with another WFS1 gene variant [12,13,14]. We could not find other candidate causative WFS1 gene variants in this case, but the possibility remained that we missed some variants present in a region not covered by the NGS panel. Considering these findings, we diagnosed case 5 with Wolfram syndrome. We needed genetic analysis of the relatives including her parents and children of case 5 to distinguish whether the true genetic cause was any types of compound heterozygous WFS1 mutations or aforesaid heterozygous WFS1 p.G674R alone; however, because her father was dead and the mother and children had few relationships with her, we could not perform genetic testing with them.
Meanwhile, case 12 was a 12-year-old girl diagnosed with diabetes at the age of 12. She had a family history of diabetes on the maternal side over three generations. She showed significant postprandial hyperglycemia, although fasting blood glucose and C-peptide levels were almost normal. These findings resembled typical clinical features of MODY1 due to HNF4A gene mutation. A novel heterozygous HNF4A p.A158Afs variant was identified in this case, the clinical significance of which was unknown. This frameshift variant might disrupt the transcription factor hepatocyte nuclear factor 4 alpha (HNF-4-alpha) over a length of 316 amino acids including a ligand-binding domain, so it was expected to damage protein function. We also performed segregation analysis for case 12 and her parents and confirmed linkage of genotype and phenotype. We consequently diagnosed the proband with MODY1.
Case 15 was a 13-year-old girl diagnosed with diabetes at the age of 13. Her mother had been diagnosed with MODY1 at another facility when she was 18 years old. We could not obtain detailed information on the diagnosis of her mother, including of the HNF4A genotype. In biochemical analysis, plasma glucose and C-peptide levels were like those in case 12. A novel heterozygous HNF4A p.Q131E variant was identified, but predicted to be located in the DNA-binding domain of the nuclear receptor HNF-4-alpha and to change the acidity of the residue. Support for its predicted pathogenicity was also provided by several in silico algorithms based on conservation metrics or protein-level scores, such as Polymorphism Phenotyping v2 (PolyPhen-2, http://genetics.bwh.harvard.edu/pph2/), Sorting Intolerant from Tolerant (SIFT, https://sift.bii.a-star.edu.sg/), and Genomic Evolutionary Rate Profiling (GERP + + , https://bio.tools/gerp). Considering these findings, we diagnosed case 15 as having MODY1 although it was unknown whether she and her mother had the identical HNF4A variant. To verify this problem, we planned to obtain informed consent for the NGS panel testing from the patient’s parents; however, had not accomplished it.
Discussion
According to the American Diabetes Association’s Standards of Medical Care in Diabetes, monogenic diabetes is estimated to account for up to 5% of all patients with diabetes [15]. Identification of each causative gene for patients with monogenic diabetes by genetic testing can provide insights into the pathophysiology of the disease and a reasonable therapeutic approach. Therefore, various in-house genetic testing methods to detect known causative gene variants for monogenic diabetes have been developed worldwide in recent years. However, NGS approaches can pick up massive numbers of variants regardless of their association with disease, and many of those variants generally have no definitive clinical significance. This sometimes makes NGS-based diagnosis of monogenic disorders difficult and may help explain why genetic testing for monogenic diabetes has not become common globally.
In previous studies, cases of monogenic diabetes diagnosed using NGS panel testing accounted for 6–25% of the total patients with non-autoimmune diabetes mellitus whose disease onset had occurred at infancy to young adulthood [3,4,5,6,7,8]. In these studies, targeted NGS panel testing mainly aimed at diagnosing MODYs, and the subjects were usually patients with diabetes with a strong suspicion of having MODY. However, in recent years, late-diagnosed cases such as those of some forms of MODY with middle-age onset [16,17,18] or insulin resistance syndrome of type A [19] were often reported. Although rare, pathogenic variants associated with neonatal diabetes could also be detected in cases with late-onset diabetes [20]. Thus, we anticipated that a certain number of adult-onset cases of monogenic diabetes would be identified from among the study participants. We detected 16 candidate mutations in the gene, but a definitive diagnosis could be reached in only 5 cases. Among most of these five cases, diabetes had developed via a dominant form of inheritance in their close relatives, so genealogical research could easily be conducted. NGS-based genetic diagnosis has an advantage that it enables estimation of the pathogenicity and clinical impact of genetic variants without in vitro/in vivo functional analysis or familial study. In some previous studies related to monogenic diabetes, patients were successfully diagnosed by only in silico functional analysis and information on the clinical features [3, 4]. However, this approach leads to many variants whose association with phenotypes is unclear (variants of uncertain significance, VUSs) remaining and makes variant interpretation difficult. To solve this problem, familial segregation analysis provides additional important information to assess the genotype–phenotype association. In the current study, we were encouraged to examine the clinical presentation and pedigree information of each patient, taking advantage of the small scale and single-center nature of this study. Consequently, we could identify two novel HNF4A gene variants causative of MODY1 with the help of segregation analysis.
In our study, most of the mutations were family-specific or sporadic; in contrast, the GCK p.M381R variant was detected in two unrelated families, all of the members of whom lived in Yamagata. The mutation was identified in the proband by sequencing and confirmed in other family members (Supplementary Fig. S1). All patients had classic clinical parameters of MODY2 with no unusual findings. Interestingly, this mutation was reported several years ago [10] and was found in another family in the same area. Nevertheless, as in other MODY2 studies, almost all patients had a private family mutation. In all of our cases, the patients were from the local region, suggesting a founder effect, although haplotype analysis was not performed. Indeed, several reports of a founder effect in MODY2 have been published. The particular isolation of local communities in our study could have led to a narrow, population-specific spectrum of mutations. MODY2 is characterized by mild, stable, and asymptomatic hyperglycemia due to an elevated threshold for glucose-stimulating insulin secretion. Because patients with MODY2 rarely have microvascular or macrovascular diabetes complications, there is a consensus that medical therapy is unnecessary for them, except during pregnancy, and it is not a major obstacle in terms of offspring preservation [21, 22]. Therefore, if a patient with MODY2 is found, it may be necessary to investigate other individuals in the region to consider whether a founder effect has occurred.
There are certain limitations to this study. First, for many selected candidate causative variants, it was difficult to determine their pathogenicity and they remained as VUSs because of an inability to demonstrate familial segregation. Segregation analysis would help in interpreting the genotype–phenotype correlation; however, particularly for adult participants, it was often difficult to contact the parents, resulting in a lack of family information. To solve this problem, we attempted to obtained missing data on patients and their families. Second, causative variants that were theoretically confirmed by a computational method do not always affect the pathogenesis of diabetes mellitus. The pathogenic effect of each candidate causative variant needs to be substantiated as much as possible by experimental biotechnology. As mentioned in ACMG/AMP clinical variant interpretation guidelines, variants that are well established by in vivo or in vitro functional studies supportive of a damaging effect on the gene are preferred evidence for NGS-based diagnosis. Third, we might miss some true pathogenic variants in undiagnosed patients because of technical limitations of the targeted NGS panel. Because GC-rich regions and repeats are difficult to enrich by PCR, sequencing coverage of our NGS panel could not reach 100% for all targeted regions. In addition, we have not analyzed other types of genomic alterations such as copy number variations or mitochondrial DNA mutations. We consider performing additional extensive genome analyses including whole-genome sequencing, especially for patients highly suspected of having a certain monogenic form of diabetes whose causative variant was negative in this study.
At the beginning of this study, we had expected to detect monogenic diabetes cases with various onset ages. However, contrary to our expectations, all of five diagnosed patients with monogenic diabetes had onset age of < 15 years as a result. Because recent investigations had shown that onset ages of some monogenic diabetes might be older than previously thought, we chose age at diabetes diagnosis < 50 years as inclusion criteria in this study; however, it might lead to lower pretest probability for monogenic diabetes of the participants. We will consider the optimal inclusion and exclusion criteria for participants to maximize diagnostic usefulness of our NGS panel testing.
In conclusion, we distinguished some monogenic diabetes cases from patients with childhood- and adolescent-onset non-autoimmune, non-highly overweight diabetes mellitus by resequencing 34 known causative genes using an NGS panel. Although it was sometimes difficult to confirm the pathogenicity of candidate variants only by computational prediction and database information, it was possible to extract some candidate genes in late-onset diabetes patients under 50 years old; in addition, segregation analyses supported by the interpretation of genotype–phenotype relationships resulted in the diagnosis of monogenic diabetes. Targeted NGS panel testing enabled us to efficiently perform genetic screening for various forms of monogenic diabetes and appeared to be useful to obtain additional genetic information.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Schwitzgebel VM. Many faces of monogenic diabetes. J Diabetes Investig. 2014;5(2):121–33.
Horikawa Y. Maturity-onset diabetes of the young as a model for elucidating the multifactorial origin of type 2 diabetes mellitus. J Diabetes Investig. 2018;9(4):704–12.
Alkorta-Aranburu G, Carmody D, Cheng YW, Nelakuditi V, Ma L, Dickens JT, Das S, Greeley SAW, Del Gaudio D. Phenotypic heterogeneity in monogenic diabetes: the clinical and diagnostic utility of a gene panel-based next-generation sequencing approach. Mol Genet Metab. 2014;113(4):315–20.
Ang SF, Lim SC, Tan CSh, Fong JC, Kon WY, Lian JX, Subramanium T, Sum CF. A preliminary study to evaluate the strategy of combining clinical criteria and next generation sequencing (NGS) for the identification of monogenic diabetes among multi-ethnic Asians. Diabetes Res Clin Pract. 2016;119:13–22.
Ushijima K, Fukami M, Ayabe T, Narumi S, Okuno M, Nakamura A, Takahashi T, Ihara K, Ohkubo K, Tachikawa E, Nakayama S, Arai J, Kikuchi N, Kikuchi T, Kawamura T, Urakami T, Hata K, Nakabayashi K, Matsubara Y, Amemiya S, Ogata T, Yokota I, Sugihara S, Japanese Study Group of Insulin Therapy for Childhood and Adolescent Diabetes. Comprehensive screening for monogenic diabetes in 89 Japanese children with insulin-requiring antibody-negative type 1 diabetes. Pediatr Diabetes. 2018;19(2):243–50.
Donath X, Saint-Martin C, Dubois-Laforgue D, Rajasingham R, Mifsud F, Ciangura C, Timsit J, Bellanné-Chantelot C, Monogenic Diabetes Study Group of the Société Francophone du Diabète. Next-generation sequencing identifies monogenic diabetes in 16% of patients with late adolescence/adult-onset diabetes selected on a clinical basis: a cross-sectional analysis. BMC Med. 2019;17:132.
Tatsi EB, Kanaka-Gantenbein C, Scorilas A, Chrousos GP, Sertedaki A. Next generation sequencing targeted gene panel in Greek MODY patients increases diagnostic accuracy. Pediatr Diabetes. 2020;21(1):28–39.
Ivanoshchuk DE, Shakhtshneider EV, Rymar OD, Ovsyannikova AK, Mikhailova SV, Fishman VS, Valeev ES, Orlov PS, Voevoda MI. The mutation spectrum of maturity onset diabetes of the young (MODY)-associated genes among western siberia patients. J Pers Med. 2021;11(1):57.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, ACMG Laboratory Quality Assurance Committee. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of medical genetics and genomics and the association for molecular pathology. Genet Med. 2015;17(5):405–24.
Yorifuji T, Fujimaru R, Hosokawa Y, Tamagawa N, Shiozaki M, Aizu K, Jinno K, Maruo Y, Nagasaka H, Tajima T, Kobayashi K, Urakami T. Comprehensive molecular analysis of Japanese patients with pediatric-onset MODY-type diabetes mellitus. Pediatr Diabetes. 2012;13(1):26–32.
Khanim F, Kirk J, Latif F, Barrett TG. WFS1/wolframin mutations, wolfram syndrome, and associated diseases. Hum Mutat. 2001;17(5):357–67.
Matsunaga K, Tanabe K, Inoue H, Okuya S, Ohta Y, Akiyama M, Taguchi A, Kora Y, Okayama N, Yamada Y, Wada Y, Amemiya S, Sugihara S, Nakao Y, Oka Y, Tanizawa Y. Wolfram syndrome in the Japanese population; molecular analysis of WFS1 gene and characterization of clinical features. PLoS ONE. 2014;9(9): e106906.
Gómez-Zaera M, Strom TM, Rodríguez B, Estivill X, Meitinger T, Nunes V. Presence of a major WFS1 mutation in Spanish Wolfram syndrome pedigrees. Mol Genet Metab. 2001;72(1):72–81.
Aloi C, Salina A, Pasquali L, Lugani F, Perri K, Russo C, Tallone R, Ghiggeri GM, Lorini R, d’Annunzio G. Wolfram syndrome: new mutations, different phenotype. PLoS ONE. 2012;7(1): e29150.
American Diabetes Association Professional Practice Committee. 2 classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17–38.
Horikawa Y, Enya M, Fushimi N, Fushimi Y, Takeda J. Screening of diabetes of youth for hepatocyte nuclear factor 1 mutations: clinical phenotype of HNF1β-related maturity-onset diabetes of the young and HNF1α-related maturity-onset diabetes of the young in Japanese. Diabet Med. 2014;31(6):721–7.
Horikawa Y, Enya M, Mabe H, Fukushima K, Takubo N, Ohashi M, Ikeda F, Hashimoto KI, Watada H, Takeda J. NEUROD1-deficient diabetes (MODY6): identification of the first cases in Japanese and the clinical features. Pediatr Diabetes. 2018;19(2):236–42.
Uraki S, Furuta H, Miyawaki M, Matsutani N, Shima Y, Iwamoto M, Matsuno S, Morita S, Furuta M, Doi A, Iwakura H, Ariyasu H, Nishi M, Suzuki H, Akamizu T. Neonatal diabetes caused by the heterozygous pro1198leu mutation in the ABCC8 gene in a male infant: 6-year clinical course. J Diabetes Investig. 2020;11(2):502–5.
Takeuchi T, Ishigaki Y, Hirota Y, Hasegawa Y, Yorifuji T, Kadowaki H, Akamizu T, Ogawa W, Katagiri H. Clinical characteristics of insulin resistance syndromes: a nationwide survey in Japan. J Diabetes Investig. 2020;11(3):603–16.
De Franco E, Shaw-Smith C, Flanagan SE, Shepherd MH, Hattersley AT, Ellard S, International NDM Consortium. GATA6 mutations cause a broad phenotypic spectrum of diabetes from pancreatic agenesis to adult-onset diabetes without exocrine insufficiency. Diabetes. 2013;62(3):993–7.
Velho G, Blanché H, Vaxillaire M, Bellanné-Chantelot C, Pardini VC, Timsit J, Passa P, Deschamps I, Robert JJ, Weber IT, Marotta D, Pilkis SJ, Lipkind GM, Bell GI, Froguel P. Identification of 14 new glucokinase mutations and description of the clinical profile of 42 MODY-2 families. Diabetologia. 1997;40:217–24.
Chakera AJ, Steele AM, Gloyn AL, Shepherd MH, Shields B, Ellard S, Hattersley AT. Recognition and management of individuals with hyperglycemia because of a heterozygous glucokinase mutation. Diabetes Care. 2015;38(7):1383–92.
Acknowledgements
The authors thank the patients and their family members who participated in this study. The authors are also grateful to Ms. Tomomi Seino, Mr. Yuki Miyano, and Ms. Ryoko Murakami for technical assistance. The authors gratefully acknowledge Dr. Takashi Daitsu of Mamigasaki Children’s Clinic, Yamagata, Japan for providing us with additional information and helpful discussions about the patients. Finally, the authors also thank Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The idea of the study was conceived by SS. Data collection was performed by YH, KN, NT, SK, WK, and CN. Data analysis was performed by HS. The first draft of the manuscript was written by KT and all authors commented on previous versions of the manuscript. KI supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human rights statement
Name of institutional or national ethical committee on human experimentation. The Ethical Review Committee of Yamagata University Faculty of Medicine.
Date of approval
June 6th, 2017.
Approval number
2017–108
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and/or with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for being included in the study. For patients between the ages of 5 and 18, written informed consent was obtained from each patient or their parents/legal guardians and informed assent was given for themselves.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Takase, K., Susa, S., Sato, H. et al. Identification of causative gene variants for patients with known monogenic diabetes using a targeted next-generation sequencing panel in a single-center study. Diabetol Int 15, 203–211 (2024). https://doi.org/10.1007/s13340-023-00669-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-023-00669-3