Abstract
Aims
Relationship between baseline eGFR and the rate of decline in eGFR was investigated in diabetic kidney disease.
Materials and methods
Patients with type 2 diabetes with microalbuminuria (MI) (n = 124) or macroalbuminuria (MA) (n = 81) received team-based medical care to prevent the development of diabetic kidney disease. The decline in eGFR over 4 years, divided into the first year and subsequent 3 years, was estimated by linear-mixed modeling.
Results
The eGFR showed a rapid decline during the first year, followed by a slower decline. On multiple regression analysis, the baseline eGFR was positively correlated with HbA1c in MI and negatively correlated with carotid plaque in MI and in MA. Subsequent eGFR decline following 1-year intervention was negatively correlated with the baseline eGFR and HbA1c level at 1 year in MI, whereas it was positively correlated with baseline eGFR and negatively correlated with the amount of proteinuria at 1 year in MA. Even in maintained baseline eGFR(≧ 60 ml/min/1.73 m2) at the first year, when HbA1c ≧ 7.5%, eGFR reduction rate and years to ESKD were much faster and shorter, compared to the group of HbA1c < 7.5% [− 3.44 (SE 1.137) vs. − 1.695 (SE 0.431) ml/min/1.73 m2/year, and 19.4 vs. 35.7 years, respectively]. In MA, lower eGFR (< 60 ml/min/1.73 m2) and higher proteinuria (≧ 2.25 g/gCre) had a much faster eGFR decline and shorter time to ESKD, compared to the group of maintained eGFR and lower proteinuria (< 2.25 g/gCre) [− 5.240 (SE 1.537) vs. − 2.67 (SE 0.997) ml/min/1.73 m2/year, and 4.41 vs. 22.8 years, respectively].
Conclusions
In MI, even in maintained eGFR, the continued increase in eGFR in response to hyperglycemia (HbA1c ≧ 7.5%) led to a faster decline in renal function and in MA, lower eGFR, with an increase in proteinuria, contributed to rapid decline of renal function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic kidney disease is the leading cause of end-stage kidney disease (ESKD) worldwide. Diabetic kidney disease is defined by the presence of albuminuria and/or reduced estimated glomerular filtration rate (eGFR), which are also clinically essential in decision-making [1]. Nevertheless, the relationship between baseline eGFR and eGFR decline rates has not been studied in detail [2], as only few studies on GFR decline have been published using an appropriate statistical analysis, such as linear-mixed model (LMM) [3, 4]. Microalbuminuria (MI) is the most important risk factor of progression to overt nephropathy [5, 6], and when this progression occurs, the GFR rapidly decreases, resulting in ESKD development [5, 7,8,9]. Albuminuria is not only an early manifestation of nephropathy but also is associated with an increased risk for cardiovascular disease and death, with increasing nephropathy [6, 8]. Recently, diabetic kidney disease without MI has been reported to have a lower risk for renal disease progression and cardiovascular disease and death, re-emphasizing the importance of MI in disease progression [10].
In a prospective clinical cohort study comprising 15,517 participants over a 26-year period, a LMM analysis revealed that the eGFR decline was almost twofold faster in patients with diabetes than in those without diabetes [4]. However, there is no documentation on the eGFR decline in patients with type 2 diabetes in both stages of diabetic nephropathy (MI and macroalbuminuria [MA]) and its relationship with baseline eGFR [2]. Furthermore, the initiation of antihypertensive treatment induces an initially rapid (but subsequently slower) eGFR decline in diabetic nephropathy [11, 12], without adverse effects on cardiovascular events and death [13]. Improvement in glycemic control can also cause an initial decrease in eGFR [14]; however, the subsequent eGFR decline has not been studied in detail, and there is only one relevant report on patients with type 2 diabetes with hyperfiltration [15].
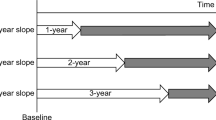
In Japan, diabetes is the leading cause of hemodialysis. Accordingly, a system for diabetes dialysis prevention (DDP) by team-based medical care for patients with albuminuria (> 30 mg/gCre) was introduced in 2012 by the Ministry of Health, Labour and Welfare. The present study investigated the eGFR decline under DDP using LMM and examined the relationship between eGFR decline and baseline eGFR (and other factors). As it is difficult to evaluate the eGFR decline when the initial period is included, we separately examined the eGFR decline in the initial stage, when it is easily affected by metabolic control, and in the subsequent 3-year period, when it is relatively stable and more accurately reflects the eGFR decline.
Materials and methods
Patients
In Japan, medical policies pertaining to DDP have been enforced by the health insurance system of the Ministry of Health, Labour and Welfare since April 2012. Prior to the enactment of DDP, 552 patients among 1,795 outpatients received standard therapy for diabetic nephropathy (in the presence of MI or MA) between January 2004 and March 2014 at the Center of Diabetes and Endocrinology of Shin-koga Hospital. Outpatients were screened for albuminuria and DDP management was started in April 2012. MI was defined as urinary albumin-to-creatinine ratio (UAC) of 30–299 mg/gCre, and MA was defined as UAC > 299 mg/gCre or a urinary protein-to-creatinine excretion rate (UPC) > 0.5 g/gCre in two consecutive urine specimens within 6 months. Among 394 patients with diabetic nephropathy who received team-based medical care for DDP, 40 with advanced chronic renal failure (eGFR < 30 ml/min/1.73 m2) and 149 with less than 4 years of DDP management were excluded. Finally, 205 patients (124 with MI and 81 with MA) with more than 4 years of DDP management were enrolled in this study.
DDP procedures
Team-based medical care by doctors, nurses, and registered dietitians was provided at every monthly visit. Diet therapy and education was performed by dietitians; the Japanese balanced diet comprises 55–60% carbohydrate, 20–25% fat, 12–20% protein, and salt restriction, without excess protein intake (< 1.3 g/body weight). Lifestyle counseling, such as smoking and alcohol intake reduction, and education regarding insulin therapy were provided by nurses.
In the treatment of diabetes, diet therapy alone was 7.3%, oral antidiabetic drugs 59.7%, and insulin treatment 33% and angiotensin II receptor blocker (ARB) was used in patients with hypertension (75.3%). In patients with MA, diet therapy alone was 2.5%, oral antidiabetics 43.2%, and insulin treatment 54.3% and ARB also had been used in most patients with hypertension (77.7%). Dipeptidyl peptidase-4 (DPP4) inhibitors were mainly used in antidiabetic drug in patients with MI (63.7%) and in MA (64.1%), alone, with combination with metformin or with sulfonyl urea. Sodium glucose cotransporter 2 (SGLT2) inhibitors and diuretics did not use in most patients during DDP study.
Assessments
Body weight; blood pressure; HbA1c; serum creatinine; eGFR; serum lipids and UPC in patients with MA were measured monthly. UAC was measured every 3 months in patients with MI. eGFR was calculated using the Modification of Diet in Renal Disease formula, adjusted for ethic Japanese GFR by the Japanese Society of Nephrology: 194 × Cre−1.094 × Age−0.287 for males and 194 × Cre−1.094 × Age−0.287 × 0.739 for females [16]. The mean blood pressure (MBP) was calculated as the diastolic pressure plus one-third of the pulse pressure.
In addition, B-mode ultrasonographic scanning of the carotid artery was performed, Intima-media thickness and plaque were measured (Supplementary Fig. 1), as previously reported [17, 18].
Statistical analysis
Data are presented as means (standard deviations), means [standard errors], median (interquartile range) or numbers (percentages). Clinical factors were compared using the paired t test, with adjustment by Dunnett’s method for multiple comparisons. Pearson’s correlation coefficient (r) was used as the measures of association between baseline eGFR or eGFR reduction rate and clinical factors. The eGFR decline was analyzed using LMM for repeated measures. eGFR regression lines were determined from 12 consecutive eGFRs in the first year and 36 consecutive eGFRs in the subsequent 3 years, as well as from 48 consecutive eGFRs in the entire 4-year period. In this approach, individual-level covariates were allowed to explain the differences across patients. In addition, separate random intercepts and slopes were fitted for each patient; thus, all differences across patients were essentially controlled, and the estimates of the reported associations were effectively free from within-patient differences. The following equation describes the structure of our fitted models:
where Yit is the eGFR in patient i at year, α is the overall intercept, b0 is a random intercept for patienti, β is the slope representing the overall effect of time, b1 is a random slope for patienti, and εit is the within-patient error.
Multivariate regression modeling was applied to evaluate the effects of clinical factors while adjusting for potential confounding factors. Multivariate regression analysis was carried out with the insertion of all variables found to be significant on univariate analysis. We selected the threshold for the factors that were significant in the multiple regression analysis by maximizing the profile partial likelihood among the LMM, with a binary explanatory variable representing the high group or the low group with various thresholds.
Statistical analysis was performed using JMP11, SAS ver. 9.4 (SAS Institute, Inc., Cary, NC, USA), and R version 3.4.4 (http://www.R-project.org). p values < 0.05 were considered statistically significant.
Results
The characteristics of the 205 patients with type 2 diabetes (124 with MI and 81 with MA) are summarized in Table 1. Data on team-based medical care for DDP over the 4-year period following standard therapy are shown in Table 2.
MI under DDP
In patients with MI, the mean HbA1c level and MBP were 7.27 (1.25) % and 94 (11) mmHg, respectively, at baseline, reflecting significant improvements in response to standard therapy (Table 2). Under DDP, the HbA1c level and MBP significantly decreased to 7.01(1.06) % (p < 0.01) and 90.4(8.9) mmHg (p < 0.01), respectively, at 1 year, and remained significantly decreased during the 4-year period. UAC decreased significantly from 76.9 (173.7, 53.2) mg/gCre [median (upper and lower quartile)] at baseline to 55.9 (91.5–35.9) mg/gCre (p < 0.01) at 1 year and 50.6 (93.1, 24.8) mg/gCre (p < 0.01) at 2 years under DDP; it then returned to the initial values at 3 and 4 years and did not significantly increase compared to the baseline value. Remission (UAC < 30 mg/gCre) and regression (> 50% reduction in UAC) in MI were observed in 4 (3.2%) and 21 patients (16.9%), respectively, whereas progression to MA (UAC > 299 mg/gCre) was observed in 2 patients (1.6%). eGFR in MI was significantly decreased from baseline values [66.1(20.7) ml/min/1.73 m2; median, 66.5 ml/min/1.73 m2; interquartile range, 78.8–50.5 ml/min/1.73 m2] to 63.3 (20.7) ml/min/1.73 m2 (p < 0.01) at 1 year under DDP and 58.7 (18.7) ml/min/1.73 m2 (p < 0.01) at the study end. No patients did not show apparent hyperfiltration (eGFR > 125 ml/min/1.73 m2) at 1 year and progressed to ESKD (eGFR < 15 ml/min/1.73 m2) during the 4-year period.
MA under DDP
In patients with MA, HbA1c and MBP were 7.34 (1.10) % and 98.8 (14.6) mmHg, respectively, at baseline, reflecting significant improvements by standard therapy (Table 2). Under DDP, HbA1c levels significantly decreased to 7.06 (0.95) % (p < 0.01) at 1 year and remained significantly decreased during the 4-year observation period. The MBP significantly decreased from 98.8 (14.6) mmHg at baseline to 93.2 (10.7) mmHg (p < 0.05) at 3 years and 93.9 (10.9) mmHg (p < 0.05) at 4 years. The UPC was 0.95(0.54, 2.03) g/gCre; [median (upper, lower quartile)] at baseline and did not significantly change during the first 3 years under DDP but was significantly increased at the study end [1.36(2.25, 0.675), p < 0.05]. eGFR in MA was 59.5 (20.4) ml/min/1.73 m2 (median, 57.2 ml/min/1.73 m2; interquartile range, 70.9–43.9 ml/min/1.73 m2) at baseline and significantly decreased to 54.8 ± 20.6 ml/min/1.73 m2 (p < 0.01) at 1 year under DDP and 46.5 (21.3) ml/min/1.73 m2 (p < 0.01) at the study end. In MA, two patients (2.5%) progressed to ESKD during the 4-year period.
LMM results
The LMM effects for annual eGFR decline are shown in Fig. 1. The slopes of the regression line in the first and subsequent 3 years were analyzed, based on the fixed LMM effects (Fig. 1). In MI, a rapid decline in eGFR occurred in the first year [regression coefficient (standard error), − 2.842 (0.702) ml/min/1.73 m2/year], followed by a slower decrease in eGFR during the subsequent 3-year period [− 1.853 (0.301) ml/min/1.73 m2/year; − 2.9% (0.47%) per annum] and the years to ESKD, calculated from the slope, were 26.19. In MA, a rapid decline in eGFR occurred in the first year [− 4.054 (0.902) ml/min/1.73 m2/year], followed by a slower decrease in eGFR during the subsequent 3-year period [− 3.048 (0.466) ml/min/1.73 m2/year; − 5.6% (0.86%) per annum] and the years to ESKD were 12.89. The rate of eGFR decline in MI and MA during the subsequent 3-year period was 1.3-fold and 2.2-fold faster, respectively, than that reported for the general population (− 1.4 ml/min/1.73 m2/year) [4]. In MA, the eGFR decline rate was 1.6-times faster than that for MI.
Linear mixed-effects models for the annual rate in eGFR decline. Thick straight lines show each regression line from the fixed effect of the linear-mixed model during the first year (a in A, B), subsequent 3-year period (b in A, B), and entire 4-year period (C, D). A and C represent microalbuminuria; B and D represent macroalbuminuria. Thin lines represent the longitudinal eGFR value in each patient over a 4-year period. Values of the slope (SE, standard error) and intercept (SE) of thick regression lines during the first year (a in A, B), subsequent 3-year period (b in A, B), and entire 4-year period (C, D) are shown in the lower panels. The slope denotes the annual eGFR reduction rate (ml/min/1.73 m2/year)
Factors associated with baseline eGFR
Results of the univariate and multivariate regression analyses for baseline eGFR are shown in Table 3. On multiple regression analysis, in MI, baseline eGFR was independently and positively correlated with HbA1c (β = 0.390, p < 0.01) and negatively correlated with the sum of plaque thickness in the carotid artery (β = − 0.319, p < 0.05). In MA, baseline eGFR was independently and negatively correlated with duration of diabetes (β = − 0.258, p < 0.05) and sum of plaque thickness (β = − 0.241, p < 0.05). Similar significant correlations were observed between baseline eGFR and parameters at 1 year under DDP (Supplementary Table1). Notably, in MA, a significant positive correlation between baseline eGFR and HbA1c at 1 year was observed (β = 0.270, p < 0.01).
Factors associated with the decline in eGFR
The results of the univariate and multivariate analyses for the rate of eGFR decline are shown for the entire 4-year period (Supplementary Table 3), the first year under DDP (Supplementary Table 2), and the subsequent 3-year period under DDP (Table 4).
In MI, the multiple regression analysis for eGFR decline rate during the subsequent 3-year period revealed significant, independent, and negative correlations with the HbA1c level (β = − 0.244, p < 0.01) and eGFR (β = − 0.281, p < 0.01) at 1 year under DDP (as the baseline). In the corresponding analysis in MA, there was a significant, independent, and positive correlation with eGFR (β = 0.326, p < 0.05) and a significant, independent, and negative correlation with UPC (β = − 0.372, p < 0.05) at 1 year under DDP (as the baseline) (Table 4).
eGFR decline rate in the combination of risk factors
The thresholds of significant risk factors for eGFR decline in multiple regression analysis (as shown in Table 3) were constructed from Minimum Akaike Information Criterion (AIC). The threshold values were 60 ml/min/1.73 m2 for eGFR and 7.5% for HbA1c in MI, and 60 ml/min/1.73 m2 for eGFR and 2.25 g/gCre for UPE in MA. For MI, in the eGFR > 60 ml/min/1.73 m2 group, when HbA1c ≧ 7.5% at 1 year, the eGFR decline rate and years of ESKD, calculated from slope, were − 3.44 (SE 1.137) ml/min/1.73 m2/year and 19.4 years, respectively; faster and shorter, compared to the group with HbA1c < 7.5% [− 1.695 (SE 0.431) ml/min/1.73 m2/year and 35.7 years, respectively]. In the group of eGFR < 60 ml/min/1.73 m2, when HbA1c < 7.5% after 1 year, the number of years of ESKD were 20.25, comparable to the group of eGFR ≧ 60 ml/min/1.73 m2 and HbA1c ≧ 7.5% (Table 5).
For MA, in the group of eGFR < 60 ml/min/1.73 m2 and UPC ≧ 2.25 g/g Cre, eGFR reduction rate and years of ESKD were − 5.240 (SE 1.537) ml/min/1.73 m2/year and 4.41 years, respectively; faster and shorter than in the group of eGFR ≧ 60 ml/min/1.73 m2 and UPC < 2.25 g/gCre, in which the corresponding values were − 2.67 (SE 0.997) ml/min/1.73 m2/year and 22.82 year, respectively (Table 5).
Discussion
The major findings in the present study were as follows. First, the eGFR showed a rapid decline during the first year, followed by a slower decline. Second, the rate of eGFR decline following the initial drop due to metabolic control was approximately 1.3-fold and 2.2-fold faster in those with incipient diabetic nephropathy and overt nephropathy, respectively, compared to that in the general population [4]. Third, baseline eGFR increased in response to hyperglycemia in both stages of nephropathy, which was limited by the factors of atherosclerosis and age. Forth, the factors contributing to eGFR decline differed between incipient and overt nephropathy; the higher the baseline eGFR with persistent poor glycemic control (HbA1c ≧ 7.5%) in incipient nephropathy, the greater the rate of eGFR decline; in overt nephropathy, the lower the baseline eGFR (eGFR < 60 ml/min/1.73 m2) and the higher the degree of proteinuria (2.25 g/gCre), the greater the rate of eGFR decline.
It is well known that the initiation of treatment for hypertension [11, 12] and the control of hyperglycemia in type 1 and type 2 diabetes [14, 15] causes a temporary decrease in eGFR. The initial drop in eGFR by antihypertensive drugs has been reported to subsequently induce a slow reduction in eGFR [11, 12]. However, subsequent changes in eGFR following glycemic control have not been studied in detail, except in patients with hyperfiltration [15]. Ruggenenti et al. demonstrated that in patients with type 2 diabetes with hyperfiltration and normo- or microalbuminuria, amelioration of hyperfiltration by metabolic control resulted in a slower reduction in eGFR, compared to those with persistent hyperfiltration [15], indicating that persistent hyperfiltration caused a more rapid eGFR decline. Further, we showed evidence that in patients without apparent hyperfiltration (eGFR < 125 ml/min/1.73 m2), a slow decline in eGFR, following the initial rapid decline, occurred in the subsequent 3-year period.
Recently, Warren et al. reported that the eGFR decline was − 2.5 ml/min/1.73 m2/year and − 1.4 ml/min/1.73 m2/year in with and without diabetes, respectively, as determined by LMM [4]. A similar finding was reported by Hemmelgarn et al. [19]. However, few studies have reported the rates of eGFR decline in both MI and MA. Nosadini et al. reported that the GFR decline, as assessed by the Cr57-EDTA decay method, during 4 years of follow-up in patients with type 2 diabetes was − 1.3 ± 9.4 ml/min/1.73 m2/year in MI and − 3.0 ± 13.0 ml/min/1.73 m2/year in MA [20]; these values might not reflect a representative slope when expressed as Mean (SD). In the present study, after exclusion of the period of the initial rapid drop in eGFR by metabolic control (i.e., the first year under DDP), we demonstrated an eGFR decline in diabetic nephropathy of − 1.853 ml/min/1.73 m2/year (− 2.8% per year) in patients with incipient diabetic nephropathy (MI) and − 3.0 ml/min/1.73 m2/year (− 5.6% per year) in patients with overt nephropathy (MA). Hoefield et al. reported similar results, showing that eGFR declined a 1.5% per year in MI and 5.7% per year in MA, in a 3431 patient cohort of type 1 and type 2 diabetes with a median follow-up of 6.5 years, using LMM analysis [3]. Even in the incipient diabetic nephropathy patients, the decline was approximately 1.3-fold faster than that in the general population, as reported by Warren et al. [4], and with the development of overt nephropathy, the decline accelerated to a 2.2-fold faster rate. In addition, the decline in MA was 1.6-fold faster than that in MI.
Baseline eGFR (before DDP)
In the present study, baseline eGFR was independently and negatively correlated with the degree of carotid plaque in both stages (MI and MA). Similarly, Taniwaki et al. reported a significant correlation between GFR (measured by kidney scintigraphy) and intima-media thickness (including plaque) in patients with normo- or MI [21]. In this study, stronger relationships were observed with the measurement of the plaque itself (the sum of plaque thickness), which might more closely reflect systemic atherosclerosis. We demonstrated that atherosclerosis is an important factor in determining baseline eGFR levels not only in incipient nephropathy, but also overt nephropathy. We previously reported that the sum of plaque thickness in the carotid artery is a useful detector of coronary artery disease [17, 18]. Our results also indicated that the plaque score in the carotid artery is an important surrogate marker for reduced kidney function as well as coronary artery disease. Reduced eGFR has been reported prior to the development of MI [22]. Therefore, it is important to measure carotid plaques (a simple laboratory test), as a marker of arteriosclerosis, not only in classical diabetic nephropathy but also in normoalbuminuric renal insufficiency.
In contrast to the negative correlation between baseline eGFR and carotid plaque, we found a positive correlation between baseline eGFR and HbA1c. Acute hyperglycemia is known to increase GFR in normal individuals [23] and in patients with type 1 [24] and type 2 [25] diabetes with normal renal function and type 1 diabetes with overt nephropathy [26]. In the present study, baseline eGFR was significantly positively correlated with baseline HbA1c in MI, with a slightly blunted correlation in MA (β = 0.205, p = 0.065). A similar linear correlation with HbA1c was shown in patients with type 2 diabetes with normoalbuminuria [27] and MI [28, 29]. This may be mediated through the effects of the tubule glomerular feedback system as well as effects on vascular factors, such as the renin–angiotensin–aldosterone [32, 33] and NO systems [34], leading to glomerular hyperfiltration [30, 31].
eGFR decline during the subsequent 3 years
We examined the factors contributing to the eGFR decline during the subsequent 3-year period in MI and MA. In MI, we observed a significant correlation between the eGFR decline and HbA1c, and eGFR, using 1-year values as the baseline.
Such significant negative correlation between eGFR decline and HbA1c [27, 35] or baseline eGFR [27, 36] has been reported in the patients with type 2 diabetes with normoalbuminuria [36] or microalbuminuria [27, 35]. The reason that a high baseline GFR caused a more rapid decline of GFR might be partially explained by glomerular hyperfiltration, as typically found in early stage of type 1 diabetes [37, 38]. However, in our study, none of the patients had obvious hyperfiltration (eGFR > 125 ml/min/1.73 m2). Moreover, the threshold of significant risk factors contributing to the decline of eGFR (Table 4), was 60 ml/min/1.73 m2 in both MI and in MA; the value was equivalent to the definition of chronic kidney disease [39]. The threshold of HbA1c 7.5% in our study was similar to the finding by Brocco et al. that GFR decline was significantly delayed only when HbA1c was controlled below 7.5% in type 2 diabetes with glomerulopathy [40]. Even in the maintained eGFR group (≧ 60 ml/min/1.73 m2), when HbA1c ≧ 7.5 % after 1 year of metabolic control, eGFR decline and years to ESKD, were much faster and shorter, compared to the group with HbA1c < 7.5%. This indicated that the persistent increase of the eGFR in response to hyperglycemia (HbA1c ≧ 7.5%) lead to the decline of renal function. Thus, in clinical practice, patients with maintained eGFR (≧ 60 ml/min/1.73 m2), should also be subjected to metabolic control with HbA1c < 7.5%. Continuous glomerular hyperfiltration in the remaining functional kidney by maximal use of glomerular filtration capacity might induce a reduction in renal function [41].
In contrast, in MA, the eGFR decline was positively correlated with eGFR and negatively correlated with the amount of urinary protein. In the general population, several studies have reported that the eGFR decline is steeper in those with low GFR [9, 42]. The degree of proteinuria was also the important factor contributing to the eGFR decline, confirming previous results showing that, in chronic kidney disease, proteinuria is an independent risk factor for renal disease progression, irrespective of the causing disease [7, 43]. In our study, thresholds of eGFR and UPC for eGFR reduction were 60 ml/min/1.73 m2 and 2.25 g/gCre, respectively. Ruggenenti et al. reported that, threshold of proteinuria for GFR decline was 2 g/day, and patients with proteinuria of ≧ 2 g/day showed faster progressor compared to those of proteinuria < 2 g/day in chronic proteinuric nephropathy [44]. In our study, patients with low eGFR (< 60 ml/min/1.73 m2) and UPC ≧ 2.25 g/gCre had the fastest eGFR decline and the shortest time to ESKD, while patients with maintained eGFR (≧ 60 ml/min/1.73 m2) and UPE < 2.25 g/gCre had a slower progression. It has been reported that in patients with type 2 diabetes with MA, as the eGFR decreases, the risk of renal events such as dialysis or more than 50% decline of eGFR per year, as well as mortality rate, were much increased [9, 45]. Our study indicates that maintaining a baseline eGFR (≧ 60 ml/min/1.73 m2) and not increasing urinary protein excretion (< 2.25 g/gCre) are important factors to prevent the rapid progression of overt nephropathy.
Study limitations
Our study was retrospective study. In addition, our study is a single-center study, but multi-center studies are needed. eGFR decline following the initial drop was examined for 3 years; longer term follow-up is needed to confirm a renoprotection effect. Although our study did not include patients with normoalbuminuria, it is important to examine the reduction in eGFR between patients with normoalbuminuria, MI, and MA.
Change history
27 November 2021
A Correction to this paper has been published: https://doi.org/10.1007/s13340-021-00558-7
Abbreviations
- DDP:
-
Diabetes dialysis prevention
- ESKD:
-
End-stage kidney disease
- LMM:
-
Linear mixed model
- MI:
-
Microalbuminuria
- MA:
-
Macroalbuminuria
- MBP:
-
Mean blood pressure
- UAC:
-
Urinary albumine-to-creatinine ratio
- UPC:
-
Urinary protein-to-creatinine excretion rate
References
American Diabetes Association. Microvascular complications and foot care: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S135–51. https://doi.org/10.2337/dc20-S011 (PMID: 31862754).
Kang YX, Lin XL, Ding Y, Pan XW, He SX, Shan PF. Comment on Warren et al. Diabetes and trajectories of estimated glomerular filtration rate: a prospective cohort analysis of the atherosclerosis risk in communities study. Diabetes Care 2019; 41:1646-1653. Diabetes Care. 2019;42:e51–2. https://doi.org/10.2337/dc18-2288.
Hoefield RA, Kalra PA, Baker PG, Sousa I, Diggle PJ, Gibson MJ, O’Donoghue DJ, Middleton RJ, New JP. The use of eGFR and ACR to predict decline in renal function in people with diabetes. Nephrol Dial Transplant. 2011;26:887–92. https://doi.org/10.1093/ndt/gfq526.
Warren B, Rebholz CM, Sang Y, Lee AK, Coresh J, Selvin E, Grams ME. Diabetes and trajectories of estimated glomerular filtration rate: a prospective cohort analysis of the atherosclerosis risk in communities study. Diabetes Care. 2018;41:1646–53. https://doi.org/10.2337/dc18-0277.
Mogensen CE, Christensen CK. Predicting diabetic nephropathy in insulin-dependent patients. N Engl J Med. 1984;311:89–93. https://doi.org/10.1056/NEJM198407123110204.
Adler AI, Stevens RJ, Manley SE, Bilous RW, Bilous RW, Cull BC, Holman RR. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63:225–32. https://doi.org/10.1046/j.1523-1755.2003.00712.x.
Remuzzi G, Bertani T. Pathophysiology of progressive nephropathies. N Engl J Med. 1998;339:1448–56. https://doi.org/10.1056/NEJM199811123392007.
Yamanouchi M, Furuichi K, Hoshino J, Toyama T, Hara A, Shimizu M, Kinowaki K, Fujii T, Ohashi K, Yuzawa Y, Kitamura H, Suzuki Y, Sato H, Uesugi N, Hisano S, Ueda Y, Nishi S, Yokoyama H, Nishino T, Samejima K, Kohagura K, Shibagaki Y, Mise K, Makino H, Matsuo S, Ubara Y, Wada T, Research Group of Diabetic Nephropathy, the Ministry of Health, Labour and Welfare, and the Japan Agency for Medical Research and Development. Nonproteinuric versus proteinuric phenotypes in diabetic kidney disease: a propensity score-matched analysis of a nationwide, biopsy-based cohort study. Diabetes Care. 2019;42:891–902. https://doi.org/10.2337/dc18-1320.
Shimizu M, Furuichi K, Toyama T, Kitajima S, Hara A, Kitagawa K, Iwata Y, Sakai N, Takamura T, Yoshimura M, Yokoyama H, Kaneko S, Wada T, Kanazawa Study Group for Renal Diseases and Hypertension. Long-term outcomes of Japanese type 2 diabetic patients with biopsy-proven diabetic nephropathy. Diabetes Care. 2013;36:3655–62. https://doi.org/10.2337/dc13-0298.
Yokoyama H, Araki SI, Kawai K, Yamazaki K, Shirabe SI, Sugimoto H, Minami M, Miyazawa I, Maegawa H, JDDM Study Group. The prognosis of patients with type 2 diabetes and nonalbuminuric diabetic kidney disease is not always poor: implication of the effects of coexisting macrovascular complications (JDDM 54). Diabetes Care. 2020;43:1102–10. https://doi.org/10.2337/dc19-2049.
Parving HH, Andersen AR, Smidt UM, Hommel E, Mathiesen ER, Svendsen PA. Effect of antihypertensive treatment on kidney function in diabetic nephropathy. Br Med J (Clin Res Ed). 1987;294:1443–7. https://doi.org/10.1136/bmj.294.6585.1443.
Hansen HP, Rossing P, Tarnow L, Nielsen FS, Jensen BR, Parving HH. Increased glomerular filtration rate after withdrawal of long-term antihypertensive treatment in diabetic nephropathy. Kidney Int. 1995;47:1726–31. https://doi.org/10.1038/ki.1995.238.
Beddhu S, Shen J, Cheung AK, Kimmel PL, Chertow GM, Wei G, Boucher RE, Chochol M, Arman F, Campbell RC, Contreras G, Dwyer JP, Freedman BI, Ix JH, Kirchner K, Papademetriou V, Pisoni R, Rocco MV, Whelton PK, Greene T. Implications of early decline in eGFR due to intensive BP control for cardiovascular outcomes in SPRINT. J Am Soc Nephrol. 2019;30:1523–33. https://doi.org/10.1681/ASN.2018121261.
Vora JP, Dolben J, Williams JD, Peters JR, Owens DR. Impact of initial treatment on renal function in newly-diagnosed type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia. 1993;36:734–40. https://doi.org/10.1007/BF00401144.
Ruggenenti P, Porrini EL, Gaspari F, Motterlini N, Ganntata A, Carrara F, Cella C, Ferrari S, Stucchi N, Parvanova A, Iliev I, Dodesini AR, Trevisan R, Bossi A, Zaletel J, Remuzzi G. Glomerular hyperfiltration and renal disease progression in type 2 diabetes. Diabetes Care. 2012;35:2061–8. https://doi.org/10.2337/dc11-2189.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators Developing the Japanese Equation for Estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92. https://doi.org/10.1053/j.ajkd.2008.12.034.
Akazawa S, Tojikubo M, Nakano Y, Nakamura S, Kawasaki T, Koga N. Usefulness of sum of the thickness of plaque in the carotid artery for predicting the presence and the extent of the coronary artery disease in patients with type 2 diabetes mellitus without known coronary artery disease. Diabetes Res Clin Pract. 2012;96:111–8. https://doi.org/10.1016/j.diabres.2011.11.019.
Akazawa S, Tojikubo M, Nakano Y, Nakamura S, Tamai H, Yonemoto K, Sadasima E, Kawasaki T, Koga N. Usefulness of carotid plaque (sum and maximum of plaque thickness) in combination with intima-media thickness for the detection of coronary artery disease in asymptomatic patients with diabetes. J Diabetes Investig. 2016;7:396–403. https://doi.org/10.1111/jdi.12403.
Hemmelgarn BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, Southern DA, McLaughlin K, Mortis G, Culleton BF. Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int. 2006;69:2155–61. https://doi.org/10.1038/sj.ki.5000270.
Nosadini R, Velussi M, Brocco E, Bruseghin M, Abaterusso C, Saller A, Dalla Vestra M, Carraro A, Bortoloso E, Sambataro M, Barzon I, Frigato F, Muollo B, Chiesura-Corona M, Pacini G, Baggio B, Piarulli F, Sfriso A, Fioretto P. Course of renal function in type 2 diabetic patients with abnormalities of albumin excretion rate. Diabetes. 2000;49:476–84. https://doi.org/10.2337/diabetes.49.3.476.
Taniwaki H, Nishizawa Y, Kawagishi T, Ishimura E, Emoto M, Okamura T, Okuno Y, Morii H. Decrease in glomerular filtration rate in Japanese patients with type 2 diabetes is linked to atherosclerosis. Diabetes Care. 1998;21:1848–55. https://doi.org/10.2337/diacare.21.11.1848.
MacIsaac RJ, Tsalamandris C, Panagiotopoulos S, Smith TJ, McNeil KJ, Jerums G. Nonalbuminuric renal insufficiency in type 2 diabetes. Diabetes Care. 2004;27:195–200. https://doi.org/10.2337/diacare.27.1.195.
Christiansen JS, Frandsen M, Parving HH. Effect of intravenous glucose infusion on renal function in normal man and in insulin-dependent diabetics. Diabetologia. 1981;21:368–73. https://doi.org/10.1007/BF00252683.
Skøtt P, Vaag A, Hother-Nielsen O, Andersen P, Bruun NE, Giese J, Beck-Nielsen H, Parving HH. Effects of hyperglycaemia on kidney function, atrial natriuretic factor and plasma renin in patients with insulin-dependent diabetes mellitus. Scand J Clin Lab Invest. 1991;51:715–27. https://doi.org/10.3109/00365519109104586.
Christensen PK, Lund S, Parving HH. The impact of glycaemic control on autoregulation of glomerular filtration rate in patients with non-insulin dependent diabetes. Scand J Clin Lab Invest. 2001;61:43–50. https://doi.org/10.1080/00365510151067965.
Remuzzi A, Viberti G, Ruggenenti P, Battaglia C, Pagni R, Remuzzi G. Glomerular response to hyperglycemia in human diabetic nephropathy. Am J Physiol. 1990;259:F545-552. https://doi.org/10.1152/ajprenal.1990.259.4.F545.
Yokoyama H, Kanno S, Takahashi S, Yamada D, Itoh H, Saito K, Sone H, Haneda M. Determinants of decline in glomerular filtration rate in nonproteinuric subjects with or without diabetes and hypertension. Clin J Am Soc Nephrol. 2009;4:1432–40. https://doi.org/10.2215/CJN.06511208.
Vedel P, Obel J, Nielsen FS, Bang LE, Svendsen TL, Pedersen OB, Parving HH. Glomerular hyperfiltration in microalbuminuric NIDDM patients. Diabetologia. 1996;39:1584–9. https://doi.org/10.1007/s001250050618.
Moriya T, Tsuchiya A, Okizaki S, Hayashi A, Tanaka K, Shichiri M. Glomerular hyperfiltration and increased glomerular filtration surface are associated with renal function decline in normo- and microalbuminuric type 2 diabetes. Kidney Int. 2012;81:486–93. https://doi.org/10.1038/ki.2011.404.
Fioretto P, Zambon A, Rossato M, Busetto L, Vettor R. SGLT2 inhibitors and the diabetic kidney. Diabetes Care. 2016;39(Suppl 2):S165-171. https://doi.org/10.2337/dcS15-3006.
Cherney DZ, Perkins BA, Soleymanlou N, Maione M, Lai V, Lee A, Fagan NM, Woerle HJ, Johansen OE, Broedl UC, von Eynatten M. Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation. 2014;129:587–97. https://doi.org/10.1161/CIRCULATIONAHA.113.005081.
Miller JA. Impact of hyperglycemia on the renin angiotensin system in early human type 1 diabetes mellitus. J Am Soc Nephrol. 1999;10:1778–85.
Cherney DZ, Reich HN, Scholey JW, Daneman D, Mahmud FH, Har RL, Sochett EB. The effect of aliskiren on urinary cytokine/chemokine responses to clamped hyperglycaemia in type 1 diabetes. Diabetologia. 2013;56:2308–17. https://doi.org/10.1007/s00125-013-3000-3.
Chiarelli F, Cipollone F, Romano F, Tumini S, Costantini F, di Ricco L, Pomilio M, Pierdomenico SD, Marini M, Cuccurullo F, Mezzetti A. Increased circulating nitric oxide in young patients with type 1 diabetes and persistent microalbuminuria: relation to glomerular hyperfiltration. Diabetes. 2000;49:1258–63. https://doi.org/10.2337/diabetes.49.7.1258.
Thomaseth K, Pacini G, Morelli P, Tonolo G, Nosadini R. Importance of glycemic control on the course of glomerular filtration rate in type 2 diabetes with hypertension and microalbuminuria under tight blood pressure control. Nutr Metab Cardiovasc Dis. 2008;18:632–8. https://doi.org/10.1016/j.numecd.2007.05.006.
Silveiro SP, Friedman R, de Azevedo MJ, Canani LH, Gross JL. Five-year prospective study of glomerular filtration rate and albumin excretion rate in normofiltering and hyperfiltering normoalbuminuric NIDDM patients. Diabetes Care. 1996;19:171–4. https://doi.org/10.2337/diacare.19.2.171.
Bjornstad P, Cherney DZ, Snell-Bergeon JK, Pyle L, Rewers M, Johnson RJ, Maahs DM. Rapid GFR decline is associated with renal hyperfiltration and impaired GFR in adults with type 1 diabetes. Nephrol Dial Transplant. 2015;30:1706–11. https://doi.org/10.1093/ndt/gfv121.
Thomson HJ, Ekinci EI, Radcliffe NJ, Seah JM, MacIsaac RJ, Jerums G, Premaratne E. Elevated baseline glomerular filtration rate (GFR) is independently associated with a more rapid decline in renal function of patients with type 1 diabetes. J Diabetes Complicat. 2016;30:256–61. https://doi.org/10.1016/j.jdiacomp.2015.11.003.
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, De Zeeuw D, Hostetter TH, Lameire N, Eknoyan G. Definition and classification of chronic kidney disease: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int. 2005;67:2089–100. https://doi.org/10.1111/j.1523-1755.2005.00365.x.
Brocco E, Velussi M, Cernigoi AM, Abaterusso C, Bruseghin M, Carraro A, Sambataro M, Piarulli F, Sfriso A, Nosadini R. Evidence of a threshold value of glycated hemoglobin to improve the course of renal function in type 2 diabetes with typical diabetic glomerulopathy. J Nephrol. 2001;14:461–71.
Tonneijck L, Muskiet MH, Smits MM, van Bommel EJ, Heerspink HJ, van Raalte DH, Joles JA. Glomerular hyperfiltration in diabetes: mechanisms, clinical significance, and treatment. J Am Soc Nephrol. 2017;28:1023–39. https://doi.org/10.1681/ASN.2016060666.
Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, Kiyohara Y, Makino H, Hishida A, Matsuo S. Slower decline of glomerular filtration rate in the Japanese general population: a longitudinal 10-year follow-up study. Hypertens Res. 2008;31:433–41. https://doi.org/10.1291/hypres.31.433.
Peterson JC, Adler S, Burkart JM, Greene T, Hebert LA, Hunsicker LG, King AJ, Klahr S, Massry SG, Seifter JL. Blood pressure control, proteinuria, and the progression of renal disease. The modification of diet in renal disease study. Ann Intern Med. 1995;123:754–62. https://doi.org/10.7326/0003-4819-123-10-199511150-00003.
Ruggenenti P, Gherardi A, Perna G, Benini R, Remuzzi G. Chronic proteinuric nephropathy: outcomes and response to treatment in a prospective cohort of 352 patients with different patterns of renal injury. Am J Kidney Dis. 2000;35:1155–565. https://doi.org/10.1016/s0272-6386(00)70054-0 (PMID: 10845831).
Bruno G, Merletti F, Bargero G, Novelli G, Melis D, Soddu A, Perotto M, Pagano G, Cavallo-Perin P. Estimated glomerular filtration rate, albuminuria and mortality in type 2 diabetes: the Casale Monferrato Study. Diabetologia. 2007;50:941–8. https://doi.org/10.1007/s00125-007-0616-1.
Acknowledgements
We would like to express our deep gratitude to Dr Eiji Kawasaki, Dr Yuko Nakano, Dr Yoko Sagara, Dr Aira Uchida, Dr Takahiro Fukuyama, Dr Masayuki Tojikubo, and Dr Hidekazu Tamai who involved in the treatment in prevention of diabetes dialysis at the Diabetes Center of Shin-koga Hospital. We thank Mr. Daiki Setoguchi and Mr. Hiroaki Tagawa for his involvement in data organization.
Author information
Authors and Affiliations
Contributions
ES performed statistical analysis and wrote the manuscript. YS and NK contributed to the discussion and reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This study was approved by the Ethical committee at Koseikai Hospital (2020-12, 2020/12/3) and Shin-Koga Hospital (2019/11/13, 2018/11/12).
Informed consent
All informed consent was given before management of Diabetes Dialysis Prevention was initiated. All patients were fully informed about DDP, understood how to do it, and agreed to receive not only treatment by a doctor, but also dietary guidance by a registered dietitian and lifestyle guidance by a nurse.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Akazawa, S., Sadashima, E., Sera, Y. et al. Decline in the estimated glomerular filtration rate (eGFR) following metabolic control and its relationship with baseline eGFR in type 2 diabetes with microalbuminuria or macroalbuminuria. Diabetol Int 13, 148–159 (2022). https://doi.org/10.1007/s13340-021-00517-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00517-2