Abstract
Objective
This study assessed whether a structured nurse-led diabetes educational program underpinned by the theories of the health belief model, change in locus of control, and patient empowerment is effective in improving glycemic and metabolic parameters among South Asians with type II diabetes compared to regular outpatient care.
Methods
This was a parallel-group randomized trial in South Asian adult patients with type II diabetes living in Qatar. 460 subjects were randomized to a nurse-led, group-based diabetes educational program (n = 230) or to usual care (n = 230). The primary outcome was the improvement in HbA1c and other metabolic parameters, including lipid profile, albumin/creatinine ratio, blood pressure, and body mass index. Patients in the intervention group were invited to attend four 2-h sessions of self-efficacy improvement education once weekly. Outcomes were assessed at baseline and 12 months later. An intention-to-treat analysis was performed using repeated measures ANOVA (analysis of variance) for each of the clinical outcome variables.
Results
After 12 months, 290 patients completed the study. Subjects in the intervention group had statistically significant improvements in HbA1c (−0.55 %, p = 0.012), fasting blood sugar (−16.6 mg/dl, p = 0.022), albumin/creatinine ratio (−3.09, p < 0.001), and HDL cholesterol (+6.08 mg/dl, p < 0.0001).
Conclusion
The inclusion of South Asian patients with type II diabetes in a structured, theory-based diabetes educational program that is led by nurses improves glycemic and metabolic parameters after 12 months.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes is an increasingly prevalent disease affecting communities worldwide. However, certain ethnicities such as South Asians are more affected than others. Arabian Gulf countries have recently witnessed the emergence of obesity and diabetes mellitus epidemics that are currently presenting a major public health challenge in the region. Recent studies in Arabian Gulf countries, including Qatar, have shown a strong association between obesity and diabetes: more than 56 % of diabetic patients were found to be obese [1]. In parallel, the Arabian Gulf region has witnessed a sharp increase in cardiovascular disease morbidity and mortality over the last three decades due to diabetes and obesity [2, 3]. In general, foreign workers make up 80 % of the population, and the biggest proportion of the population in Qatar are from South Asian countries, mainly India, Bangladesh, and Pakistan, which comprise an estimated 40 % of the population (Qatari nationals represent only 20 % of the population—a minority) [4].
Patient education is an essential component of long-term health care management, although it has not always received the attention it deserves, especially in the Arabian Gulf. Diabetes education, in particular, has become an integral part of diabetes management. Studies have shown that effective diabetes education can lead to improved metabolic control, a reduction in complications, and an overall improvement in the quality of life [5, 6].
However, the concept of improving patients’ behavior merely by improving their knowledge was refuted by a review of twenty studies [7]. Education and knowledge are essential but not enough. Therefore, there are other factors that lead an individual to embrace a certain behavior or not. These include, but are not limited to, the psychological status of the patient, attitude, motivation, the locus of control, therapeutic alliance with the health provider, perception of the disease, perception of the benefit of treatments, comorbid conditions, and the organization of the health system.
As a result, more effective methods to deliver patient education and teach self-management skills are needed. In this regard, it is essential for an educational intervention to be theory-based in order to test its efficacy and to help understand its success or failure [7]. Theory-based educational interventions such as the health belief model [8], change in locus of control [9], patient empowerment [10, 11], counseling [12], and cognitive theory [13] have been utilized in only a few studies worldwide. Additionally, the patient empowerment theory emphasizes a collaborative approach to facilitate a self-directed behavioral change in patients [14], and is probably the most frequently taught model in outreach interventions.
In Qatar, diabetes education is rather fragmented, lacks structure, and is usually delivered by a variety of health professionals, including doctors, nurses, social workers, dieticians, and a few certified diabetes educators. Furthermore, with the introduction of electronic medical files and the excessive number of patients per clinic (which may reach up to 35 patients per session), there is very little time for any effective education to be delivered. It is believed that patients look down on nurses delivering healthcare counseling, viewing their physicians as more capable of looking after their health than nurses. Therefore, we assessed the efficacy of a nurse-led educational intervention underpinned by the theories of the health belief model (HBM), change in locus of control, and patient empowerment in improving glycemic and metabolic parameters among our patient population. This study targeted the South Asian population in Qatar that we feel lacks adequate diabetes education. Furthermore, this study was unique since it assessed the level of knowledge, the influence of structured education, and socioeconomic factors that influenced South Asian patients with type II diabetes who were away from their native culture and habitat, and examined the elements that influence their illness.
Methods
Patient population
Under protocols approved by the Hamad Medical Corporation Research and Ethics Committee 2010, this trial was carried out in 22 primary health care centers across Qatar in addition to 16 endocrinology clinics at Hamad Medical Corporation (HMC), the main hospital in Doha, Qatar. Participants were randomly selected from the primary care registry and from the endocrinology clinics at HMC. The second stage involved sending informed consent letters inviting patients to participate in the trial; this was done in accordance with the guidelines from The International Conference of Harmonization and WHO good clinical practice standards. In the third stage, participants were randomly allocated to either the intervention group or the control group using a random table method [15]. A statistician blinded to the nature or the location of the trial performed the randomization independently at Greenwich University, UK. Patients were excluded if they had type 1 diabetes, a history of alcohol abuse, a history of drug abuse, a mental illness precluding them from participating in the educational sessions, or if they were younger than 18 years of age. Moreover, patients participating in other research studies during the study period were also excluded.
Sample size
The population of Qatar is 1,875,564 as of 31 December 2010 according to the Qatar Statistics Authority, and South Asians represent 40 % of the general population [16]. Since the expected prevalence of diabetes is 16.7 %, the estimated diabetic population is around 125,000. Taking a confidence level of 95 % and a confidence interval of 5 %, the expected sample size was 384 subjects; however, after including the expected drop-out rate of 12 %, the final estimated sample size was 430 subjects.
The subjects in both arms continued to receive standard medical care from their health practitioners (who were were informed of their patients’ participation in the study), both practitioners and the participants were blinded to allocation. For the duration of the 12 months of the study, the subjects’ physicians were requested to abstain from nonessential changes in medication and dosage that might affect the study outcome measures. Essential medication changes were subsequently reported to the principal investigator.
The intervention is an educational program that is 8 h long, divided into four sessions each lasting 2 h, and held once weekly. It was delivered in a community setting at the Qatar Diabetes Association lecture halls, and in small groups of 10 people per group. Males and females were mixed in the different groups for the first time in this part of the world. This was coupled with an educational package (toolkit). The structured, group-based program was designed based on a series of psychological theories including the changing locus of control theory, the health belief model, and the theory of patient empowerment. The education package included pictorial material and was written in layman’s language. It also contained questions at the end of each chapter that were to be discussed in the community setting and to be part of routine daily care. Nurse educators were specifically trained to manage the delivery of the program, and were supported by a group of experts in the field of diabetes and behavioral management who helped them to deliver the program in a uniform and consistent fashion. The goal of education was not just to achieve good long-term control, but also to focus on other factors, including behavioral modifications [17] and psychological adjustment [18], and to target comorbid conditions such as hypertension, dyslipidemia, and microalbuminuria [19]. During the intervention (group-based education), nurses counseled the participants on changing their locus of control from an external to an internal one, such that the patients took the main responsibility for managing their disease. During this session, the patients were made aware of the negative consequences of having an external locus of control, as manifested by hypoglycemic episodes, worsening neuropathy, retinopathy, and nephropathy. Patients were also engaged in empowering exercises, which included self-monitoring of blood glucose, goal-setting skills, and coping skills in stressful situations.
The program was delivered in four sessions, once weekly, and facilitated by two nurse educators. Education was nondidactic and group-based, utilizing individual experiences rather than knowledge of a given health topic. The nurse educators were able to deliver health education by exploring patient experiences and by using the educational package that the patients were given and were referring to during the discussion. After each session, the nurse educators reinforced the attainment of knowledge using the multiple-choice questions in the educational package. The education package was given to the participants to keep and refer to at home.
The curriculum was divided into four sessions. The first one focused on understanding why diabetes happens, and on complications related to uncontrolled diabetes. The second session focused on adopting a healthy lifestyle and encouraging a change in eating practices; in particular, decreasing the consumption of high-carbohydrate portions and adapting the Idaho plate method for a more balanced way of eating. The Idaho method is based on a plate containing 50 % green leafy vegetables and 25 % protein supplemented by a portion of diary products and one fruit. Moreover, one piece of fruit every 2–3 h, half a cup of milk, half a cup of yogurt, or a handful of unsalted nuts were recommended between meals. In addition, we emphasized the idea of roasting food instead of frying it. A high-fiber diet and the use of monosaturated oil instead of saturated fat were encouraged. Participants were asked to keep a prospective weekly diary that also included a blood sugar level series that was to be discussed in the group session. Exercise was discussed in detail, and participants were taught the types of aerobic exercise and their durations as well as meal planning and to measure blood glucose before, during, and after exercise. The third session focused on the health benefits and glycemic improvement attained after carrying out the exercises and goal-setting methods. The fourth session focused on changing the patients’ locus of control from an external one to an internal one via empowerment and attaining a positive attitude. This encouraged the patients to master their own diabetes by following their food diary and correlating it with their blood sugar series in order to see firsthand the extent of their control over the disease. In addition to that, the effects of stress on blood sugar were clarified, and stress-management skills, such as building support systems, were emphasized. Both the intervention and control groups continued to receive regular outpatient care over the 12-month period of the study with their corresponding primary healthcare providers.
Outcome measures
We recorded the outcome measures at the beginning of the study and at 12 months post-intervention. Those included HbA1c, a full lipid profile conforming to methods used in the DCCT trial [20], and blood pressure measurement performed according to accepted methods using an electronic blood pressure monitor [21]. In addition, the subject’s weight was measured, a calibrated electronic stadiometer was utilized to measure their height, and these measures were then used to calculate their body mass index. Venous blood was sent to the main hospital laboratory, which undergoes internal and external auditing on a regular basis.
Statistical analysis
Given the quantitative nature of the clinical outcome variables, the study used repeated measures of analysis of variance (ANOVA) for each of the outcome variables to assess the overall magnitude of the change in the variable over the course of the study, and for the purposes of impact assessment. An intention-to-treat analysis was employed during the statistical analysis. The primary outcome measures were used to test the hypothesis of the study by measuring means, standard deviations, and the standard errors of the means. Mean differences and their equivalent 95 % confidence intervals were calculated for all outcome variables to allow for further statistical comparison between the control and intervention groups, similar to methods employed in previous studies [22]. Stata version 9 (Stata Corp, College Station, TX, USA) and SPP for Windows version 11 (SPSS Inc., Chicago, IL, USA) were used. The Consort statement was adhered to where possible [23].
Results
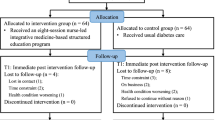
Although a total of 800 patients were invited onto the trial, only 460 participants consented and completed the questionnaires, giving a response rate of 57.4 %. Those were randomized equally into the intervention group (n = 230) and the control group (230). At 12 months, which marked the end of the study, there was a 49 % (n = 112) dropout rate in the intervention group and a 16 % (n = 36) dropout rate in the control group, as shown in Fig. 1. At the end of the study, there were 109 patients in the intervention group (40 males, 69 females) and 181 patients in the control group (50 males, 131 females). There were 42 participants in the intervention arm, and 34 participants in the control arm that dropped out because their employment contracts in Qatar had ended, so they had to leave the country.
Consort diagram of the study design. Of the 800 patients that were approached at the outpatient clinics in Qatar, only 430 gave their consent to be included in the study and completed the questionnaires. Those patients were randomized into an intervention group and a regular outpatient care group. The intervention group received an 8 h long, nurse-led diabetes education program in groups consisting of 10 people over four sessions. Patients in both groups were assessed at baseline and at 12 months. In the intervention group, 106 subjects were lost to follow-up, and 34 subjects were lost to follow-up in the control group. At the end of the study (12 months), the intervention group consisted of 40 males and 69 females, whereas the control group consisted of 50 males and 131 females
Furthermore, 26 patients left the intervention arm because they were relocated outside the capital, and could not commute and attend the educational sessions. Another 38 patients in the intervention arms left the study because several factors discouraged them from attending the educational sessions, including hot weather, traffic jams, family or work responsibilities, and the observance of the holy month of Ramadan, during which Muslims tend to stay indoors and fast. Only 32 of the 38 subjects who dropped out were traced; their attending practitioners were approached and their medical files were examined. However, their files were incomplete due to a lack of biochemical data, so no accurate data could be extrapolated. As shown in Table 1, at baseline there were no statistically significant differences between the two arms of the study in terms of the duration of the disease, educational level, income, blood pressure, fasting blood glucose, HbA1c, HDL cholesterol, and albumin/creatinine ratio. However, the age was slightly lower in the intervention group, averaging 52 years compared to 55 years in the control group (p = 0.04). Although the intervention group had a slightly higher baseline BMI of 32.8 kg/m2, compared to 32.7 kg/m2 in the control group, this difference was statistically nonsignificant, with a p value of 0.65. Interestingly, the intervention group also had a higher baseline lipid profile (total cholesterol, LDL cholesterol, and triglycerides) compared to the control group (p < 0.001). However, at the end of the study there was no statistically significant difference in total cholesterol, LDL cholesterol, or triglycerides between the two groups (Table 2), although, on average, all of the latter were still higher in the intervention group. In addition, there was a significant improvement in the HDL cholesterol in the intervention group, which was on average 6.08 mg/dl higher than in the controls (p < 0.0001), as shown in Table 2.
Both the intervention and the control groups showed improvement in their biochemical profiles after 12 months. However, at the end of the study, there was still no statistically significant difference between the two groups when comparing the systolic blood pressure or diastolic blood pressure. The BMI of the intervention group decreased from 32.8 to 32.4 kg/m2, whereas the BMI of the control group changed from 32.7 to 32.8 kg/m2.
On the other hand, there was a significant improvement in the HbA1c in the intervention group, which was on average 0.55 % (95 % CI of −0.94 to −0.16 %) lower than that of the control group (p value = 0.012). Similarly, the fasting plasma glucose was on average 16.6 mg/dl (95 % CI of −29.9 to −3.2 mg/dl) lower in the intervention arm, indicating a more significant decrease in the intervention arm compared to the controls (p value = 0.022). Furthermore, the albumin/creatinine ratio was on average 3.09 (95 % CI of −2.24 to −3.94) lower in the intervention group compared to the controls (p value < 0.0001) at 12 months, as shown in Table 2.
Discussion
We assessed the hypothesis that a nurse-led, theory-based, structured educational program for patients with type II diabetes would lead to improved glycemic control and metabolic parameters. The primary outcome was glycated hemoglobin after 14 months, and secondary outcomes consisted of the lipid profile, albumin/creatinine ratio, BMI, and blood pressure. Both arms of the trial were well matched for various variables. Although it is well recognized that interventional trials are not pragmatic in primary care settings [24, 25], we have managed to include patients from both primary care and the hospital setting, which adds further strength to the study. The results showed significant improvement in the glycemic parameters in the intervention group compared to the controls. This was evident in the levels of HbA1c, fasting plasma glucose, and the albumin/creatinine ratio. Moreover, there was a significant improvement in the lipid profile, particularly in the HDL cholesterol but also in the other lipid parameters (LDL cholesterol, total cholesterol, triglycerides), which were statistically worse at baseline but were no longer statistically worse in the intervention group after 12 months. The intervention group also showed an improvement in the average BMI, although it was not statistically significant.
Behavioral outcome was assessed based on baseline data showing a high percentage of smoking and little effort to exercise. Post intervention there was a nonsignificant improvement in smoking cessation and exercise levels, as shown in Table 3. This is due to the fact that Qatar has a very hot climate, reaching 53 °C during most months of the year, along with a high level of humidity, which can reach up to 100 %. These unfavorable conditions discourage people from exercising or going outdoors. Furthermore, a smoking cessation program that included nicotine replacement therapy was not part of the intervention. This might explain the nonsignificant improvement in behavioral outcomes. The results of our study compare well to those of another study carried out in the United Kingdom [5], which involved 314 people with established diabetes. At 14 months there was a reduction in HbA1c (−0.6 %, p < 0.001) and other parameters such as total cholesterol, BMI, waist circumference, and reduced requirement for diabetes medication.
Follow-up was similar across the two arms, and a significant effort was made to track adherence among the two arms. Unfortunately, we lacked the resources to track incident diabetes complications. We did have some data on medication compliance, but compliance was uniformly high, which made us question the validity of that data. Another limitation of our study is the attrition rate, which was much higher in the intervention group compared to the control group. This could be due to the fact that the educational program (intervention) was carried out during the summer—a critical time in Qatar that is notorious for its high temperatures and heavy traffic. It also coincided with the holy month of Ramadan, when people tend to stay indoors during the daytime and focus on prayers or family time during the evenings. Interestingly, a large proportion of the dropouts from both arms were attributed to termination of work contracts and departure from the country or the relocation of workers outside the capital. This should not be surprising given that more than 85 % of the inhabitants of Qatar are expatriates who come to Qatar for job opportunities and return to their home countries after their employment is over. The high attrition rate could not have avoided since we had no prior knowledge of which individuals would be departing, and if we had selected individuals with permanent residency, selection bias would have been a potential threat to the validity of the study findings.
To date the major focus of diabetes education in this region of the world has been on a didactic, parent–child interaction, with little involvement of patients and little acknowledgement of the significance of psychological effects that can influence diabetes management. “Parent–child interaction” refers to the flow of information (instructions) from a higher authority (parent) to a lower authority (child). This inevitably leads to the submission of the patient to the instructions of the doctor, thereby neglecting the doctor–patient partnership in decision-making. This type of interaction appears to be the current day-to-day practice in many chronic disease clinics, and it inadvertently encourages an external locus of control among patients. However, a study by Macrodimitis has shown that an internal locus of control, or high perceived patient control, has a beneficial effect on individuals with type 2 diabetes, as measured by decreased HbA1c levels [26]. Moreover, the degree to which patients comply with advice in terms of daily self-care activities is determined, at least partially, by their health belief systems. For instance, perceived benefits and vulnerability were related to diabetes regimen adherence in adults [27], whereas perceived cost and barriers were linked to adherence in younger subjects [28, 29].
Diabetes is a self-managed chronic illness that necessitates a patient-centered approach to care [30]. Individuals suffering from diabetes must make a series of daily decisions involving exercise, diet, medications, blood glucose monitoring, stress management [31], and ongoing preventative measures such as vaccinations, laboratory testing, and visits to various health professionals (podiatrists, ophthalmologists, and so on). Therefore, diabetes educational programs must be culturally competent, taking into account patients’ beliefs and perceptions. They must also be tailored to fit patients’ priorities and goals based on therapeutic alliance, cost-effectiveness, and sustainability over the medium and long terms. This can only be achieved if patients are empowered with the necessary knowledge and skills to attain a positive mental attitude, and change their locus of control from an external to an internal one. On that note, a recent study utilized empowerment as a theoretical basis for a structured diabetes educational program aimed at type 2 diabetic patients in the UK, which led to an improvement in glycemic control and self-management skills [5].
Improvements in glycemic and metabolic parameters in our trial cannot be attributed to a single component, since educational programs are multicomponent interventions where it is often difficult to define the “active ingredient(s)”. However, the holistic nature of the program, including culturally sensitive education, the enthusiasm of the nurses, the facilitation of learning rather than didactic learning, and theory-based intervention coupled with counseling and dietary changes utilizing the Idaho plate method could be reasons for the improvements seen in our trial. The high HDL-C values observed could be due to the fact that physicians were free to prescribe statins to their patients, ultimately resulting in a modest rise in HDL-C.
Our study differs from other studies due to the inclusion of subjects from both hospitals and the community, unlike other studies which have concentrated either on subjects recruited from hospitals [32] or subjects from the Community [32–36]. Secondly, other studies have depended on only one psychological aspect in their interventions; for instance, [12, 15] focused on patient empowerment only whereas [13] focused on counseling alone. Our study was theory-based, and utilized empowerment coupled with a change of the locus of control through nondirective counseling. During the trial, we aimed to change the locus of control of the individuals from an external one to an internal one through brief nondirective group counseling. This is quite important, since the majority of patients in our part of the world (South Asians) believe that the physician always knows best, so patients shift responsibility to the attending physician. This belief results in a negative attitude and a passive approach to managing a serious and chronic disease like diabetes which requires decisions to be made on a daily basis. Thirdly, individuals with diabetes had been receiving education from their attending physicians on a one-to-one basis behind the closed doors of the clinic because diabetes is viewed as a stigma in this part of the world. As a result, the intervention was pragmatically designed for implementation in a primary care setting in Qatar. Fourthly, diabetes educators are quite rare in this part of the world, and Qatar has only a few certified diabetes educators, meaning that an alternative approach is warranted. The idea of open group-based education is new in this part of the world, and proved to be acceptable and efficacious in this study. This is very important, as it allows resources to be saved and individuals to be empowered to take control of their own disease. The program can also be transferred to neighboring countries, since they share the same cultural beliefs and socioeconomic characteristics. Finally, a hallmark of this study is the utilization of local nurses who were vigilantly trained to carry out the structured intervention and deliver adequate diabetes education. This is unprecedented in our region of the world.
Conclusion
In conclusion, the results of this study provide evidence that nurse-led, theory-based, group diabetes education is feasible, generalizable to neighboring Arab countries, and effective at improving diabetes and metabolic parameters of South Asian patients with type 2 diabetes.
References
Bener A, Tewfik I. Prevalence of overweight, obesity, and associated psychological problems in Qatari female population. Obes Rev. 2006;7(2):139–45.
Bener A, Al Suwaidi J, Ghaffar A. Is hypertension a predictor for heart failure? A cross cultural comparison over a 10 year period. Eur J Heart Fail. 2005;7(5):784–6.
Al-Mahroos F. Diabetes mellitus in the Arabian Peninsula. Ann Saudi Med. 2000;20(2):111–2.
Goodman A. The development of the Qatar healthcare system: a review of the literature. Int J Clin Med. 2015;6:177–85. doi:10.4236/ijcm.2015.63023.
UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352(9131):854–65.
Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;2(2):CD003417.
Pendleton D. Knowledge and compliance; not linked after all? Pharm J. 1992;248(6673):186.
Eccles M, Grimshaw J, Walker A, Johnston M, Pitts N. Changing the behavior of healthcare professionals: the use of theory in promoting the uptake of research findings. J Clin Epidemiol. 2005;58(2):107–12.
Rosenstock IM, Stretcher VJ, Becker MH. Social learning theory and health belief model. Health Educ Q. 1988;13:73–92.
Rotter JB. Social learning and clinical psychology. Englewood Cliffs, NJ: Prentice Hall; 1954.
Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26(4):597–604.
Funnell MM, Nwankwo R, Gillard ML, Anderson RM, Tang TS. Implementing an empowerment-based diabetes self-management education program. Diabetes Educ. 2005;31(1):53–61.
Kirk A, Mutrie N, MacIntyre P, Fisher M. Effects of a 12-month physical activity counselling intervention on glycaemic control and on the status of cardiovascular risk factors in people with type 2 diabetes. Diabetologia. 2004;47(5):821–32.
Miller CK, Edwards L, Kissling G, Sanville L. Nutrition education improves metabolic outcomes among older adults with diabetes mellitus: results from a randomized controlled trial. Prev Med. 2002;34(2):252–9.
Funnell MM, Tang TS, Anderson RM. From DSME to DSMS: developing empowerment-based diabetes self-management support. Diabetes Spectr. 2007;20(4):221–6.
Ramsay L, Williams B, Johnston G, MacGregor G, Poston L, Potter J, et al. Guidelines for management of hypertension: report of the Third Working Party of the British Hypertension Society. J Hum Hypertens. 1999;13(9):569–92.
Wylie-Rosett J, Herman WH, Goldberg RB. Lifestyle intervention to prevent diabetes: intensive and cost effective. Curr Opin Lipidol. 2006;17(1):37–44.
Sturt J, Taylor H, Docherty A, Dale J, Louise T. A psychological approach to providing self-management education for people with type 2 diabetes: the diabetes manual. BMC Fam Pract. 2006;7:70.
Gaede P, Vedel P, Parving HH, Pedersen O. Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the Steno type 2 randomised study. Lancet. 1999;353(9153):617–22.
Rohlfing CL, Wiedmeyer HM, Little RR, England JD, Tennill A, Goldstein DE. Defining the relationship between plasma glucose and HbA(1c): analysis of glucose profiles and HbA(1c) in the Diabetes Control and Complications Trial. Diabetes Care. 2002;25(2):275–8.
Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;(2):CD003417.
Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134(8):663–94.
Moher M, Yudkin P, Wright L, Turner R, Fuller A, Schofield T, et al. Cluster randomised controlled trial to compare three methods of promoting secondary prevention of coronary heart disease in primary care. BMJ. 2001;322(7298):1338.
Wilson S, Delaney BC, Roalfe A, Roberts L, Redman V, Wearn AM, et al. Randomised controlled trials in primary care: case study. BMJ. 2000;321(7252):24–6.
Warsy AS, El-Hazmi MA. Diabetes mellitus, hypertension and obesity–common multifactorial disorders in saudis. East Mediterr Health J. 1999;5(6):1236–42.
Macrodimitris SD, Endler NS. Coping, control, and adjustment in type 2 diabetes. Health Psychol. 2001;20(3):208–16.
Brownlee-Duffeck M, Peterson L, Simonds JF, Goldstein D, Kilo C, Hoette S. The role of health beliefs in the regimen adherence and metabolic control of adolescents and adults with diabetes mellitus. J Consult Clin Psychol. 1987;55(2):139–44.
Glasgow RE, McCaul KD, Schafer LC. Barriers to regimen adherence among persons with insulin-dependent diabetes. J Behav Med. 1986;9(1):65–77.
Schafer LC, Glasgow RE, McCaul KD, Dreher M. Adherence to IDDM regimens: Relationship to psychosocial variables and metabolic control. Diabetes Care. 1983;6(5):493–8.
Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment. results of a randomized controlled trial. Diabetes Care. 1995;18(7):943–9.
Anderson RM, Funnell MM. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Couns. 2005;57(2):153–7.
Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the Diabetes Education and Self-management for Ongoing and Newly Diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ Br Med J. 2008;336(7642):491–5. doi:10.1136/bmj.39474.922025.BE.
Gagliardino JJ, Etchegoyen G, PENDID-LA Research Group. A model educational program for people with type 2 diabetes: a cooperative Latin American implementation study (PEDNID-LA). Diabetes Care. 2001;24(6):1001–7.
Wallston KA, Wallston BS, DeVellis R. Development of the multidimensional health locus of control (MHLC) scales. Health Educ Monogr. 1978;6(2):160–70.
Mc Allister M, Dunn G, Payne K, Davies L, Todd C. Patient empowerment: the need to consider it as a measurable patient-reported outcome for chronic conditions.BMC Health Serv Res. 2012;12:157.
Tshiananga JK, Kocher S, Weber C, Erny-Albrecht K, Berndt K, Neeser K. The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Diabetes Educ. 2012;38(1):108–23.
Acknowledgments
We would like to acknowledge the cooperation and the kindness of the Qatar Diabetes Association for providing the venue in which the intervention took place.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors of the manuscript report no conflict of interest.
Informed consent
Informed consent forms were signed by and ethical approval was obtained for the participants after discussing the study with them. The study was approved by the research ethical committee of Hamad Medical Corporation in 2010, Doha, Qatar.
Human rights
This study was carried out in accordance with the Helsinki Declaration 1964.
About this article
Cite this article
Al Lenjawi, B., Mohamed, H., Amuna, P. et al. Nurse-led theory-based educational intervention improves glycemic and metabolic parameters in South Asian patients with type II diabetes: a randomized controlled trial. Diabetol Int 8, 95–103 (2017). https://doi.org/10.1007/s13340-016-0286-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-016-0286-7