Abstract
Hepatitis C is a viral infection that has been declared as a global health problem by the World Health Organization. Egypt has the highest prevalence of hepatitis C virus (HCV) which results in a high morbidity and mortality from chronic liver disease, cirrhosis, and even hepatocellular carcinoma. Cities have lower rates of infection than rural areas. Studies about the abnormally high prevalence of HCV in Egypt ascribed that to the governmental campaign to treat Schistosoma. However, these treatment campaigns have stopped more than 35 years ago, which means that some other modes of transmission must have been involved. The objective of this work is to study the main reasons of HCV prevalence in the Egyptian Delta valley. A questionnaire-based study was conducted by members of the HCV Fighters project. Responses were collected from 949 volunteers (451 HCV patients and 498 healthy volunteers as control). The data were analyzed using SPSS version 19.0. The two-sample proportion test was used for statistical comparison between groups. The most probable risk factors of HCV transmission in Egypt included regular visits to dental clinics (55.2%), previous surgical operations (54.4%), former blood transfusion (52%), intrafamilial HCV infection (45.9%) and history of bilharzial infection (44.3%). Increasing public awareness about modes of transmission and risk factors of HCV infection is a must, especially within family members of HCV patients. Strict commitment to proper medical care precautions by health care practitioners is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis C virus (HCV) is a blood-borne viral infection which was declared as a global health problem by the world health organization (WHO) [3]. HCV has a major global apprehension as the persistent infection can be the leading cause of progressive liver diseases, cirrhosis, hepatocellular carcinoma and liver transplantation [21]. HCV species are classified based on genetic differences between the isolates into 7 different genotypes with at least 67 known subtypes [16, 24]. Among these diverse genotypes, genotype 4 is the most predominant form in Egypt (responsible for 93.1% of total cases) [7]. Unfortunately, genotype 4 only accounts for 8.3% to 16.8% of the global cases most of them are in developing countries, which direct less attention towards development of genotype 4 specific antiviral regimens compared to other genotypes. Figure 1 shows the genotype distribution of HCV worldwide [10].
In 2015, viremic prevalence of HCV in Egypt was estimated to be 6.3% (global prevalence was estimated to be 1.0% at the time), which was considered to be the highest prevalence rate in the world [3]. Figure 2 shows the prevalence of HCV infection in countries with the highest burden, based on the number of HCV-infected individuals and the total population in each country [28]. The reported prevalence among Egyptian males applying for visa is up to 32%. About 20% of the blood donors in Egypt have antibodies for HCV which indicates a current or a former infection with the virus [2, 6]. Accordingly, Egypt bears higher burden and shows much higher prevalence rates than surrounding countries in the area and even in countries with comparable socioeconomic conditions [6]. This is particularly important for the Egyptian Delta valley that shows the highest prevalence rate (Fig. 3). The noticeably higher prevalence of HCV in Egyptian Delta valley has been indirectly correlated to parenteral anti-schistosomal therapy (PAT), which was practiced since 1920 with the governmental mass campaigns starting from the late 1950s to 1980s [9]. However, these treatment campaigns have stopped more than 35 years ago which means that some other modes of transmission must have been involved. The aim of our study is to investigate the potential risk factors responsible for HCV clustering in Nile Delta to help better control the viral infection and by applying special protective measures for high risk groups. Literature showed that early diagnosis of HCV increase the opportunity for successful intervention. The incidence of liver decompensation was affected by the time of infection (11% within 1 year, additional 7% within 1–5 years and additional 5% if > 5 years of HCV diagnosis) [18].
Methods
Study design
A cross sectional study was performed using self-administered questionnaires. The influence of various factors on the prevalence of HCV in the Nile Delta was assessed using Yes/No/Do not know questions for 14 items based on common risk factors of HCV in literature [12]. The questions covered statements related to medical procedures (5 items), barber’s precautions (3 items), dentist’s precautions (2 items), bilharzial infection (2 items), family history (1 items), and habits (2 items). Demographic characteristics (age, sex, education level) were collected in the first section of the questionnaire. Table 1 summarizes the demographic data for the studied population.
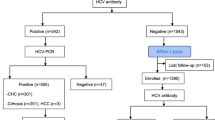
Sample size and data collection
This study was conducted as a survey, and only included voluntary participants from the National Liver Institute in Menoufia University, the Hospital of Tropical Diseases in Tanta and the Hospital of Tanta University. Sample size was calculated by assuming a 6.3% prevalence of HCV, a 99% level of significance, a ± 7 margin of error and a 20% missing-data rate [11]. The study excluded patients with only positive serological tests whose results were not confirmed by PCR.
Data quality assurance
Pretest of the data collection tool was conducted on 25 patients to check for clarity. Based on the result of the pretest, necessary corrections were done.
Data entry, analysis
All data were collected and fed to Microsoft Excel program® then analyzed with SPSS® 19 software (Statistical Package for the Social Sciences, SPSS Inc, and Chicago, USA). A two-sample proportion test was used to test for group differences (Patients vs control).
Result and discussion
Table 2 shows a summary of the questionnaire results and their statistical analysis for test and control groups. The results are arranged according to the z-score from the highest (the most significant) to the lowest (the least significant). According to these results, the most probable risk factors of HCV transmission in Egypt included regular visits to dental clinics (55.2%), previous surgical operations (54.4%), former blood transfusion (52%), intrafamilial HCV infection (45.9%) and history of bilharzial infection (44.3%). The highest z-score was observed in HCV patients co-infected with bilharziasis. Other factors including cupping therapy, renal failure dialysis, accidental needle puncture, tattooing and barbers’ shops were found nonsignificant.
For a long time, PAT campaigns were held responsible for HCV pandemic in Egypt [9, 17]. Our results showed that 44.3% of patients had schistosomal infection compared to 5% of the control group. Only HCV patients who had a bilharzial infection were asked if they were ever injected with the anti-Schistosomal glass syringe. Surprisingly, only 24.5% of the HCV/Schistosoma patients were previously immunized using the non-disposable glass syringe. This means that most of the HCV patients in the studied sample were not subject to PAT campaigns which put a query mark on the alleged strong correlation between the high prevalence of HCV in Egypt and these campaigns. On the other hand, the high z-score observed for the previous Schistosomal infection in HCV patients indicated a strong correlation between bilharziasis and hepatitis C, other than the overestimated PAT campaigns. That was supported by previous reports on the negative effect of Schistosoma infection on the cellular immune responses to core HCV peptides [8], which increased the risk of HCV chronicity, and accelerated the disease progression [27].
Common practices that may cause patient to patient transmission of HCV inside hospitals include surgical operation [15], blood transfusion [25], invasive diagnostics [4] and communal dialysis equipment [20]. Taking into consideration poor infection control and sterilization procedures in the developing countries, high prevalence of nosocomial infections in Egypt may participate to the elevated national HCV levels. The studied HCV patients were asked if they ever had blood transfusion. Significantly higher percentages were observed in the patient group compared with the control group (z score = 7.3). This can be attributed to inadequately screened blood donors [14] and unnecessary blood transfusions [6].
Invasive dental procedures are recently emphasized as possible risk factors for HCV transmission. Our results show a significant difference between percent of patients who regularly visit dental clinics (55.2%) compared to the control group (37.3%). These results highlight the importance of applying universal infection control protocols in the dental operating room. Oral and dental procedures are also a suspect for patient-to-patient transmission of HCV. Lack of proper sterilization protocols and poor infection control in dental clinics can be correlated to transmission of viral hepatitis between patients [13, 26] 41.9% of the patients declared that they do not tell the dentist/the barber that they have an HCV infection. What makes the situation even worse is that dentists/barbers rarely ask if the client has HCV or any other infection (20.4% in the patient group and 12.0% in the control group). These results show that dentists are required to be more strict in following the standard operating procedures and applying the proper infection control measures.
HCV transmission through family member is another interesting and controversial suggestion which has been previously reported in various Egyptian regions [22, 23]. A significant difference is evident between patients and control groups (Table 2) with 45.9% of patients report that at least one of their family members has HCV comparing to 30.7% of control. The risk of intrafamilial transmission can increase by increasing the duration of exposure to the patient, the number of family members suffered from HCV and long term heterosexual contact with the patient [5, 22].
Renal failure and chronic kidney disease are considered primary causes for frequent hemodialysis and/or blood transfusion. A previous report showed that the percentages of anti-HCV reactive patients were correlated with the onset of dialysis (17% if less than 1 year, 43% for 1–5 years and 76% if more than 5 years) [19]. Knowing that HCV is mainly transmitted through invasive procedures, a link maybe established between clustering of HCV and hemodialysis [1, 20]. However, the results showed no significant differences between the patient group and the control group. Similarly, no significant differences were obtained for tattoing, cupping therapy, and being punctured by a syringe needle.
Although barbers’ shops are probable places of infection transmission due to the use of sharp objects and the possibility of sharing tools with others, neither using personal tools nor checking that barbers change the shaving blades between clients was found responsible for the prevalent infection as evidenced by the high p value and the very low z-score. It is ironical that barbers’ shops were found less likely a reason for HCV transmission while dental clinics were. That could be because getting injured during dental procedures is something expected and acceptable. In addition, the high credibility of dentist in the Egyptian society makes it unusual to ask about the sterilization precautions.
The historical exposure to PAT campaigns was considered the major cause for considerably higher prevalence rate of HCV in Egypt, yet the clustering of HCV infection is not well correlated with the distribution of PAT campaign in the past. Other risk factor may have shared responsibility for the high viremic prevalence in Egypt. These factor include intrafamilial transmission, poor sterilization process and inadequate infection control during surgical and dental operation, patient to patient transmission in shared dialysis unit and blood transfusion. Hence, improvements in infection control protocols and strict hygiene practice in hospitals along with increasing awareness among health care providers is expected to reduce risk of HCV infection.
References
Amin Elzorkany K, Zahran A. Hepatitis C virus status in hemodialysis patients in Menoufia Government, Egypt, five years apart: do we have any improvement? Saudi J Kidney Dis Transpl. 2017;28:1126–32.
Arthur RR, Hassan NF, Abdallah MY, El-Sharkawy MS, Saad MD, Hackbart BG, et al. Hepatitis C antibody prevalence in blood donors in different governorates in Egypt. Trans R Soc Trop Med Hyg. 1997;91:271–4.
Blach S, Zeuzem S, Manns M, Altraif I, Duberg AS, Muljono DH, et al. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2:161–76.
Bronowicki J-P, Venard V, Botté C, Monhoven N, Gastin I, Choné L, et al. Patient-to-patient transmission of hepatitis C virus during colonoscopy. N Engl J Med. 1997;337:237–40.
Chang T-T, Liou T-C, Young K-C, Lin X-Z, Lin C-Y, Shin J-S, et al. Intrafamilial transmission of hepatitis C virus: the important role of inapparent transmission. J Med Virol. 1994;42:91–6.
El Ekiaby M, Moftah F, Goubran H, van Drimmelen H, LaPerche S, Kleinman S, et al. Viremia levels in hepatitis C infection among Egyptian blood donors and implications for transmission risk with different screening scenarios. Transfusion. 2015;55:1186–94.
Elbedewy TA, Fouad HM, Mansour FR, Khalifah AD, Ibrahim AA, Mandouh SS, et al. Pretreatment factors predicting sustained virological response to pegylated interferon/ribavirin combination therapy in Egyptian patients with hepatitis C virus genotype 4. Int J Adv Res. 2015;3:982–9.
Farid A, Al-Sherbiny M, Osman A, Mohamed N, Saad A, Shata MT, et al. Schistosoma infection inhibits cellular immune responses to core HCV peptides. Parasite Immunol. 2005;27:189–96.
Frank C, Mohamed MK, Strickland GT, Lavanchy D, Arthur RR, Magder LS, et al. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet. England. 2000;355:887–91.
Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J. Hepatol.; 2014. S45–57.
Kadam P, Bhalerao S. Sample size calculation. Int J Ayurveda Res. Wolters Kluwer – Medknow Publications; 2010;1:55–7.
Kiron S, Premaletha K, Rajagopal P, Saritha M. A study on the job satisfaction levels of pharmacists working in a community pharmacy set-up at northern part of Kerala. IOSR J Pharm. 2012;2:485–90.
Klevens RM, Moorman AC. Hepatitis C virus: an overview for dental health care providers. J Am Dent Assoc. England. 2013;144:1340–7.
Lavanchy D. Evolving epidemiology of hepatitis C virus. Clin Microbiol Infect. 2011;17:107–15.
Massari M, Petrosillo N, Ippolito G, Solforosi L, Bonazzi L, Clementi M. Transmission of hepatitis C virus in a gynecological surgery setting. J Clin Microbiol. 2001;39:2860–3.
Messina JP, Humphreys I, Flaxman A, Brown A, Cooke GS, Pybus OG, et al. Global Distribution and prevalence of hepatitis C virus genotypes. 2014;77–87.
Mohamoud YA, Mumtaz GR, Riome S, Miller D, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Egypt: a systematic review and data synthesis. BMC Infect Dis. BioMed Central; 2013;13:288.
Moorman AC, Xing J, Ko S, Rupp LB, Xu F, Gordon SC, et al. Late diagnosis of hepatitis C virus infection in the Chronic Hepatitis Cohort Study (CHeCS): missed opportunities for intervention. Hepatology. 2015;61:1479–84.
Muller GY, Zabaleta ME, Arminio A, Colmenares CJ, Capriles FI, Bianco NE, et al. Risk factors for dialysis-associated hepatitis C in Venezuela. Kidney Int. 1992;41:1055–8.
Méndez-Sánchez N, Motola-Kuba D, Chavez-Tapia NC, Bahena J, Correa-Rotter R, Uribe M. Prevalence of hepatitis C virus infection among hemodialysis patients at a tertiary-care hospital in Mexico City, Mexico. J Clin Microbiol. 2004;42:4321–2.
Nguyen A. NIH Public Access. 2014;19:292–300.
Nouh ME-D, Mahrous OA, Farg IZ. Intrafamilial transmission of hepatitis C virus in Menoufia Governorate. Menoufia Med J. 2014;27:478–83.
Paez Jimenez A, Sharaf Eldin N, Rimlinger F, El-Daly M, El-Hariri H, El-Hoseiny M, et al. HCV iatrogenic and intrafamilial transmission in Greater Cairo, Egypt. Gut. 2010;59:1554–60.
Petruzziello A, Marigliano S, Loquercio G, Cacciapuoti C. Hepatitis C virus (HCV) genotypes distribution: an epidemiological up-date in Europe. Infect Agent Cancer. Infectious Agents and Cancer; 2016;11:1–9.
Prati D. Transmission of hepatitis C virus by blood transfusions and other medical procedures: a global review. J. Hepatol. 2006. P. 607–16.
Redd JT, Baumbach J, Kohn W, Nainan O, Khristova M, Williams I. Patient-to-patient transmission of hepatitis B virus associated with oral surgery. J Infect Dis. 2007;195:1311–4.
Strickland GT. Liver disease in Egypt: hepatitis C superseded schistosomiasis as a result of iatrogenic and biological factors. Hepatology. 2006;43:915–22.
Thrift AP, El-Serag HB, Kanwal F. Global epidemiology and burden of HCV infection and HCV-related disease. Nat Rev Gastroenterol Hepatol. Nature Publishing Group; 2017;14:122–32.
Acknowledgements
We would like to thank Sara Rabie, Mahmoud Atef Yassen, Abdelrhman Mohamed, Ghada Aboelezz, Donia Hussein, Soad Elkeshk, Haidy Anwar Tayel, Hanan Ragy, Amira Mohamed, Salma Ayman Elsayed, Shimaa Yassen, Amany Sweed, Norhan Dawood, Heba Elsayed, Yassen Hamed, Esraa Ghanem, Amira Mohamed, Hemat Mohamed, Gehad Waheed, Alaa Abdo, Maha Sherief, Salma Mohamed, Basma Farahat, Omnya Fekry, Amira Shibl, Ahmed Gad, Alyaa Hekal, Ghadaa Eldeeb, Marehan Ragab, Gamela Elgendy, Walaa Mohamed, Eman Badr and all other members of HCV Fighters for their help in data collection.
Funding
The authors declare that no fund was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declared no competing interests.
Consent for publication
All the authors gave their consent for the publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mandoh, S.S., Ayman, K., Elbardakheny, A. et al. A cross sectional study of the risk factors of hepatitis C infection in North Egypt. VirusDis. 32, 22–28 (2021). https://doi.org/10.1007/s13337-020-00639-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13337-020-00639-2