Abstract
Background
Overactive adenosine triphosphate signaling via P2X3 homotrimeric receptors is implicated in multiple conditions. To fully understand the metabolism and elimination pathways of eliapixant, a study was conducted to assess the pharmacokinetics, mass balance, and routes of excretion of a single oral dose of the selective P2X3 receptor antagonist eliapixant, in addition to an in vitro characterization.
Methods
In this single-center open-label non-randomized non-placebo-controlled phase I study, healthy male subjects (n = 6) received a single dose of 50 mg eliapixant blended with 3.7 MBq [14C]eliapixant as a PEG 400-based oral solution. Total radioactivity and metabolites excreted in urine and feces, and pharmacokinetics of total radioactivity, eliapixant, and metabolites in plasma were assessed via liquid scintillation counting and high-performance liquid chromatography-based methods coupled to radiometric and mass spectrometric detection. Metabolite profiles of eliapixant in human in vitro systems and metabolizing enzymes were also investigated.
Results
After administration as an oral solution, eliapixant was rapidly absorbed, reaching maximum plasma concentrations within 2 h. Eliapixant was eliminated from plasma with a mean terminal half-life of 48.3 h. Unchanged eliapixant was the predominant component in plasma (72.6% of total radioactivity area under the curve). The remaining percentage of drug-related components in plasma probably represented the sum of many metabolites, detected in trace amounts. Mean recovery of total radioactivity was 97.9% of the administered dose (94.3–99.4%) within 14 days, with 86.3% (84.8–88.1%) excreted via feces and 11.6% (9.5–13.1%) via urine. Excretion of parent drug was minimal in feces (0.7% of dose) and urine (≈ 0.5%). In feces, metabolites formed by oxidation represented > 90% of excreted total radioactivity. The metabolites detected in the in vitro experiments were similar to those identified in vivo.
Conclusion
Complete recovery of administered eliapixant-related radioactivity was observed in healthy male subjects with predominant excretion via feces. Eliapixant was almost exclusively cleared by oxidative biotransformation (> 90% of dose), with major involvement of cytochrome P450 3A4. Excretion of parent drug was of minor importance (~ 1% of dose).
Clinical trial registration
ClinicalTrials.gov: NCT04487431 (registered 27 July 2020)/EudraCT number: 2020-000519-54 (registered 3 February 2020), NCT02817100 (registered 26 June 2016), NCT03310645 (registered 16 October 2017).
Plain Language Summary
Eliapixant is a drug that acts on structures in the body called P2X3 receptors that are involved in several conditions, including chronic cough, overactive bladder, and endometriosis-related pain. When evaluating a new drug, it is important to know how it is being removed from the body by natural mechanisms. We performed a study in which six healthy male volunteers took a single dose of eliapixant, and we investigated what happened to the drug after it was taken. We measured the amount of eliapixant in the volunteers’ blood, urine, and feces, and also measured the compounds formed when eliapixant was broken down naturally by the body (“metabolites”). We also used human cells in the laboratory to investigate how the different metabolites of eliapixant are formed. Almost three-quarters of eliapixant in the blood had not been broken down at all, while the remaining one-quarter had been converted into many different metabolites. A total of 2 weeks after taking eliapixant, almost all of it had been converted to metabolites and eliminated from the body (mostly in feces, but also a small amount in urine). The most important organ for breaking down eliapixant is the liver. The information from this study will help doctors determine whether eliapixant is likely to interfere with other drugs taken simultaneously, and whether patients with liver or kidney problems might take longer than healthy people to remove it from their bodies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In healthy male subjects, pharmacokinetic analysis of total radioactivity and eliapixant in plasma showed rapid absorption and a long terminal plasma elimination half-life. |
Almost complete recovery of the administered eliapixant dose was observed with predominant excretion via feces and, to a much lesser extent, via urine. |
In vitro studies with human liver microsomes and hepatocytes and clinical metabolic profiling in plasma, feces, and urine showed that eliapixant is primarily metabolized by phase I metabolism (oxidation), with CYP3A4 making the predominant contribution. |
1 Introduction
Overactive adenosine triphosphate signaling via P2X3 homotrimeric receptors has been implicated in many disorders including neurogenic inflammation, refractory chronic cough (RCC), overactive bladder (OAB), and endometriosis-related pain [1,2,3,4,5,6,7]. Eliapixant is a potent and highly selective P2X3 receptor antagonist that has been in clinical development for RCC [8], OAB (ClinicalTrials.gov: NCT04545580), and pain associated with endometriosis (ClinicalTrials.gov: NCT04614246) [9]. In a phase IIa study, eliapixant significantly reduced cough frequency and severity in patients with RCC with fewer taste-related side effects at therapeutic doses than reported with another P2X3 receptor antagonist, gefapixant [8]. Additionally, in the recently published phase IIb PAGANINI study, eliapixant reduced cough count versus baseline and placebo in patients with RCC with a favorable taste tolerability profile [10]. While adverse events (AEs) were mainly mild or moderate, one case of a moderate drug-induced liver injury in a participant receiving 150-mg twice-daily eliapixant contributed to intensified liver monitoring in eliapixant clinical trials and subsequently to discontinuation of the clinical development of eliapixant by Bayer AG [10].
To assess potential risks relating to drug–drug interactions or those that might affect patients with impaired elimination organ function relevant to the intended target population, characterization of the metabolism and elimination pathways of eliapixant was warranted. The pharmacokinetic profile of eliapixant after oral administration with a standard immediate-release formulation showed a long half-life, limited oral bioavailability, and less than dose-proportional exposure with single ascending doses of 10–800 mg [11]. A high-fat high-calorie breakfast was associated with a four-fold increase in maximum plasma concentration (Cmax) and a three-fold increase in area under the concentration–time curve (AUC) [11, 12]. With multiple dosing, peak plasma concentrations of eliapixant were reached 3–4 h after administration of the first and subsequent doses, steady-state plasma concentrations were reached after approximately 6 days, and plasma concentrations predicted to achieve ≥ 80% P2X3 receptor occupancy were reached at 200 and 750 mg [13]. In view of the limitations of tablet formulation, there was a need to investigate the oral bioavailability of an eliapixant liquid service formulation in the mass balance study. Here we report a two-part single-center open-label non-randomized non-placebo-controlled study in healthy male subjects. After an initial feasibility study to assess the pharmacokinetics of a single oral dose of eliapixant as an oral solution, the mass balance and route of excretion of radio-labeled material were determined following a single oral dose of [14C]eliapixant given as a solution, and total radioactivity in blood and plasma and unchanged eliapixant in plasma were quantified. We also report metabolite profiling data from in vitro studies and two early clinical trials.
2 Methods
2.1 In Vitro Studies
2.1.1 Biotransformation of Eliapixant in Human Liver Microsomes, Cytosol, and Hepatocytes
[14C]eliapixant was incubated with human liver microsomes, human liver cytosol, and hepatocyte suspensions to evaluate the metabolism of eliapixant (Supplementary Material, Sect. 1.1). The incubations were analyzed by high-performance liquid chromatography (HPLC) with tandem mass spectroscopy (MS/MS) followed by off-line radioactivity detection to generate metabolite profiles and elucidate or confirm the structures of the metabolites formed.
2.1.2 CYP Phenotyping Studies in Human Hepatocytes, Liver Microsomes, and Recombinant Human CYP Enzymes
The overall turnover of [14C]eliapixant and formation of individual metabolites was investigated using incubations with human liver microsomes and hepatocytes, and recombinant human cytochrome P450 (CYP) isoforms [CYP1A1, 1A2, 1B1, 2A6, 2B6, 2C8, 2C9, 2C18, 2C19, 2D6, 2E1, 2J2, 3A4, 3A5, 3A7, 4A11, 4F2, 4F3A, 4F3B, 4F12, and 19A1 (aromatase)]. The effect of CYP isoform-selective inhibitors on unlabeled eliapixant and metabolite formation was assessed using incubations with human liver microsomes and hepatocytes (Supplementary Material, Sect. 1.2). The incubations were analyzed after fractionated collection by HPLC and posterior radioactivity detection for [14C]eliapixant and its metabolites. When unlabeled eliapixant was used, the incubation samples were analyzed by HPLC–MS/MS.
2.2 Human Absorption, Distribution, Metabolism, and Excretion Study
2.2.1 Study Drugs
[14C]eliapixant was manufactured by Bayer AG (Wuppertal, Germany) and was formulated into a PEG 400-based oral solution containing 2.5 mg/mL eliapixant in 20 mL by ICON plc. (Groningen, the Netherlands). [14C]eliapixant had a radiochemical purity of 99.9%, an ultraviolet (UV) purity of 98.4%, and a specific radioactivity of 2.39 MBq/mg. [14C]eliapixant in the formulation for administration had a specific radioactivity of 0.079 MBq/mg, giving ≈ 3.8 MBq for the anticipated 50-mg dose. Chemicals and reagents were obtained from commercial suppliers.
2.2.2 Subjects
Subjects were included if they were male, aged 18–54 years (inclusive) with a body mass index (BMI) ≥ 18 kg/m2 and ≤ 30 kg/m2. The use of CYP3A4 inducers, CYP3A4 inhibitors, organic anion transporting polypeptide (OATP)/breast cancer resistance protein (BCRP) substrates, and permeability glycoprotein (P-gp) substrates and inducers was not permitted from 2 weeks before the study drug administration. Subjects who participated in part 1 of the study were not eligible for part 2 (Supplementary Material, Sects. 1.3.4 and 1.3.5 for full inclusion and exclusion criteria, respectively).
2.2.3 Study Design and Procedures
This was a two-part single-center open-label non-randomized non-placebo-controlled single-dose phase I study. The first part investigated the pharmacokinetics of eliapixant oral solution to confirm the feasibility of the liquid service formulation to be used in the second part (Supplementary Material, Sect. 1.3.1). In the second part, the pharmacokinetics, metabolic disposition, and mass balance of eliapixant oral solution were investigated (ClinicalTrials.gov: NCT04487431; EudraCT number: 2020-000519-54). The study was conducted in a single center at the ICON Clinical Research Unit (Groningen, the Netherlands) between 5 August and 30 October 2020.
Following a 27-day screening period, subjects were admitted to the study unit the day before study drug administration (day −1). A single oral dose of 50 mg eliapixant blended with 3.7 MBq [14C]eliapixant was administered after a high-fat high-calorie meal [containing 59 g fat (equivalent to 527 kcal) and a total of 918 kcal] on day 1, as a high-fat meal had previously been shown to increase the bioavailability of eliapixant from immediate-release tablets [14]. The composition of the meal is shown in the Supplementary Material, Table S1. Subjects then underwent blood sampling for pharmacokinetics, metabolite profiling, and radioanalysis of urine and feces for metabolite profiling, and radioanalysis until the fixed day of discharge from the unit (day 15). Subjects could be readmitted for further sampling based on the “excretion criteria” (see below). The total duration of the study for each subject was approximately 10 weeks.
2.2.4 Study Objectives and Outcome Measures
The primary objectives were: to determine the mass balance and routes of excretion following a single oral dose of [14C]eliapixant given as a solution assessed via measurement of the cumulative amount and time course of drug-related radiolabeled material (eliapixant and its metabolites) excreted in urine and feces as a percentage of the dose; to quantify the total radioactivity in blood and plasma assessed by means of AUC and Cmax of total radioactivity and the calculation of whole blood to plasma ratio by using AUC and Cmax of total radioactivity; and to quantify unchanged eliapixant in plasma assessed via AUC and Cmax of eliapixant in plasma. Other prespecified objectives included metabolic profiling in the plasma, urine, and feces. Secondary objectives were to assess the safety and tolerability of a single oral dose of eliapixant or [14C]eliapixant, respectively, by assessing the frequency and severity of AEs.
2.2.5 Sample Collection and Assessments
Blood samples for pharmacokinetics, metabolite profiling, and analysis of radioactivity were taken predose and 0.5, 1, 2, 4, 6, 8, and 12 h post-dose, and then daily on days 2–10, 12, and 15. For plasma pharmacokinetics and metabolite profiling, a minimum of 2.7 mL and 10 mL of blood, respectively, was taken and transferred to potassium ethylenediaminetetraacetic acid plasma. For metabolite profiling and analysis of radioactivity, urine samples were taken predose and over 12-h periods post-dose for day 1 (0–12 h and 12–24 h) and then over 24-h periods for days 2–15; fecal samples were taken predose and then combined in 24-h periods post-dose until day 15. All blood, plasma, urine, and feces samples were stored at < –20 °C. On day 15, the excretion of total radioactivity was checked according to the excretion criteria whereby the cumulative recovery of radioactivity should have exceeded 90% of the administered dose, and the sum of radioactivity in urine and feces should have been < 1% of the administered dose over a 24-h period on two consecutive sample collection days as determined by quick counts. Subjects not fulfilling these excretion criteria on day 15 were asked to return 7 days later for readmission to the unit and a 24-h overnight visit to collect further blood, urine, and feces samples to recheck the excretion criteria.
2.2.6 Pharmacokinetic Analysis
Plasma concentrations of eliapixant were determined by HPLC–MS/MS. For further details on assays and analyses please see the Supplementary Material, Sects. 1.3.6–1.3.8.
Pharmacokinetic parameters for mass balance data were calculated using the model-independent (compartment-free) method and the pharmacokinetics software Phoenix 8.1 (Certara, Princeton, NJ, USA) in conjunction with non-compartmental analysis Tool plugin. For individual subjects, the observed Cmax, time to Cmax (tmax), AUC from time zero to the last quantifiable concentration [AUC(0–tlast)], AUC from time zero to infinity (AUC), and the apparent terminal elimination half-life (t1/2) were determined. The AUC(0–tlast) was calculated as the sum of partial areas, calculated with the linear (if Ci ≤ Ci+1) and the logarithmic trapezoidal rule (if Ci > Ci+1). The AUC from time zero to infinity was calculated as AUC(0–tlast) + computed Ctlast/λZ, where Ctlast was the computed concentration value at tlast by regression of the terminal phase, and λZ was the terminal rate constant estimated by log-linear regression analysis. AUC was acceptable if the extrapolated area was < 20% of AUC. Values of apparent terminal elimination t1/2 were acceptable if the time range was more than twice the calculated t1/2. Pharmacokinetic parameters for biotransformation were calculated from the individual plasma concentrations by non-compartmental analysis using the software WinNonLin 5.3 (Certara, Princeton, NJ, USA) in conjunction with Automation Extension (version 2.90; Bayer AG, Germany).
2.2.7 Safety Assessments
Safety assessments including physical examination, vital signs, electrocardiogram, and laboratory assessments were performed on day –1 and periodically until discharge from the study unit. AEs were monitored from signing of the informed consent form until last study visit, including any readmission visits. An AE was defined as any untoward medical occurrence, after subjects provided informed consent, whether or not considered related to the study intervention. A serious AE (SAE) was defined as any untoward medical occurrence that, at any dose, (a) resulted in death, (b) was life-threatening, (c) required inpatient hospitalization or prolongation of existing hospitalization, (d) resulted in persistent disability/incapacity, (e) was a congenital anomaly/birth defect, or (f) other specified situations. Full definitions of AEs and SAEs are provided in Supplementary Material, Sect. 1.3.2.
2.2.8 Statistical Analysis
No formal statistical sample size estimation was performed but six subjects were planned to be assigned to the study drug. Sample size assumptions were based on previous experience with mass balance studies. All subjects without any validity findings that could influence the pharmacokinetic evaluation were included in the evaluation of pharmacokinetics and total radioactivity assessment. Safety was assessed in all subjects who took the study drug. Statistical evaluation was performed by using the software package SAS release 9.4 (SAS Institute Inc., Cary, NC, USA). All data were reported using descriptive statistics.
2.2.9 Total Radioactivity Analysis
Concentrations of total radioactivity in whole blood, plasma, urine, and feces were determined by liquid scintillation counting. For further details please see the Supplementary Material, Sects. 1.3.7 and 1.4.
2.2.10 Metabolite Profiling
Metabolite profiling was performed with plasma, urine, and fecal samples using HPLC with subsequent fractionation and off-line liquid scintillation counting. Structural elucidation by HPLC–MS/MS was performed for selected samples. As metabolites could only be detected in trace amounts via radiochromatographic methods in the mass balance study, metabolite pharmacokinetics were assessed from pooled plasma samples from two previous studies where eliapixant was administered to healthy volunteers as a single dose under fasted and non-fasted conditions, using data from the 400-mg dose group [14] and as multiple 200-mg twice-daily doses (non-fasted) [13]. This explorative non-validated analysis was performed using HPLC–MS and HPLC–MS/MS to identify and quantify unchanged eliapixant and its metabolites. Pharmacokinetic parameters were calculated from the pooled plasma concentration–time profiles using the software Toxkin version 4.1.1.1 (Entimo, Berlin, Germany). For further details please see the Supplementary Material. Pharmacokinetic parameters for eliapixant calculated in this analysis are shown in the Supplementary Material, Table S2.
3 Results
3.1 In Vitro Metabolite Profiling
3.1.1 Biotransformation of Eliapixant in Human Liver Microsomes, Cytosol, and Hepatocytes
The profiling and phenotyping study was completed according to the protocol. The principal metabolites following in vitro incubation of [14C]eliapixant in human liver microsomes, cytosol, and hepatocytes are shown in Table 1.
The turnover of [14C]eliapixant in human liver microsomes after 1 h of incubation with NADPH was 60%, and the most significant NADPH-dependent biotransformation pathways were cleavage of the tetrahydrofuran moiety by O-dealkylation of the phenol group, producing M6 (which is further oxidized to M11), oxidation of the tetrahydrofuran moiety to M1 and M2, oxidation of the thiazole ring to M3 and M11, and oxidation and cleavage of the tetrahydrofuran ring to M4, M5, and M8. Several other metabolites, produced mainly by oxidation, glucuronidation, or amide hydrolysis of eliapixant, and some of unclear structure, were detected in small amounts.
In liver cytosol, low turnover (19.3%) was observed after incubation of [14C]eliapixant over 24 h, with formation of an oxidation product at the pyrimidine ring M23 (subsequently converted to M30). M6 and M8 were detected in smaller amounts. Formation of M23 was independent of NADPH, indicating a non-CYP contribution which was confirmed by incubations with recombinant aldehyde oxidase (data not shown).
In hepatocytes, metabolic turnover was 30–95% after 4 h incubation. The predominant metabolites were M2, M4, M5, and M8 (see above), M10 (produced by glucuronidation of M6), and M9, produced by oxidation of the thiazole moiety of M3. M1, M6, M15, and the additional oxidation products M14, M16, M18, and M19 were detected in small amounts.
3.1.2 CYP Phenotyping Studies in Human Liver Microsomes and Hepatocytes, and Recombinant Human CYP Enzymes
Measurement of radioactivity in metabolite patterns from a panel of 21 recombinant CYP isoforms indicated that the oxidative biotransformation of eliapixant was mainly catalyzed by CYP2J2, CYP3A4, to a lesser extent by CYP1A1, and to a minor extent by CYP3A5, CYP1A2, and CYP2D6 (Table 2).
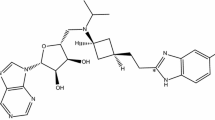
In human liver microsomes, unlabeled eliapixant depletion was inhibited by the pan-CYP inhibitor aminobenzotriazole (ABT) and the irreversible CYP3A4 inhibitors azamulin and mibefradil. Depletion was partly reduced with the CYP1A inhibitor 7-hydroxyflavone, the CYP2J2 inhibitor danazol, the CYP2C8 inhibitor montelukast, the CYP2C9 inhibitor sulfaphenazole, the CYP2C19 inhibitor benzylphenobarbital, and the CYP2D6 inhibitor quinidine (Supplementary Material, Fig. S1). Only ABT, azamulin, and mibefradil markedly inhibited metabolite formation in human liver microsomes, with ABT almost completely abolishing the formation of all metabolites, and turnover inhibited by 95% and 97% with azamulin and mibefradil, respectively. The other CYP inhibitors had no inhibitory effect on metabolite formation (Supplementary Material, Fig. S2). Similarly, in human hepatocytes from one donor, ABT completely inhibited eliapixant depletion, and metabolic clearance was inhibited by 92% and 96% with azamulin and mibefradil, respectively, whereas inhibition was not seen in the presence of danazol or telmisartan, which are also CYP2J2 inhibitors (Supplementary Material, Fig. S3). The proposed metabolic pathways involved in the metabolism of eliapixant are shown in Fig. 1.
3.2 Clinical Study
Both parts of the clinical study were completed according to the protocol. The results of Part 1 of the study are summarized in the Supplementary Material, Sect. 2.1.
3.2.1 Subjects
Of 17 subjects enrolled in part 2, 7 were screening failures, 1 decided not to complete screening, and 3 met the eligibility criteria but were not needed for the study. Consequently, six subjects received study treatment. All six subjects who received study treatment were included in the pharmacokinetic, total radioactivity, and safety assessments (Fig. 2). Due to a positive coronavirus disease 2019 (COVID-19) test, one subject did not undergo readmission assessments, but his pharmacokinetic and radioactivity data were available and he was therefore included in the analyses. His individual results were not markedly different from those of the other subjects. The majority of subjects were white (83%) and never smokers (83%), with a mean BMI of 24.2 kg/m2 (Table 3). The mean [standard deviation (SD)] age of subjects was 36.7 (14.0) years.
3.2.2 Eliapixant Pharmacokinetics in Plasma
Pharmacokinetic parameters for eliapixant are shown in Table 4. A single oral 50-mg dose of [14C]eliapixant administered with a high-fat high-calorie meal was rapidly absorbed (Fig. 3a) with a median tmax of 2.0 h, and thereafter, plasma concentrations declined in a biphasic manner. Eliapixant was eliminated from plasma with a mean apparent terminal t1/2 of 48.3 h. Geometric mean [% coefficient of variation (%CV)] Cmax was 131 µg/L (17.5%) and AUC was 2280 µg·h/L (30.1%). The concentration vs time course of eliapixant and associated total radioactivity in plasma followed a similar pattern (Fig. 3a).
a Geometric mean and geometric SD concentrations of total radioactivity and eliapixant in plasma following single oral administration of 50 mg [14C]eliapixant (semi-logarithmic scale) (n = 6). b Geometric mean and geometric SD concentrations of total radioactivity in whole blood following single oral administration of 50 mg [14C]eliapixant (semi-logarithmic scale) (n = 6). LLOQ eliapixant: 1 µg/L; LLOQ total radioactivity in plasma: 6.4 µgEq/L; LLOQ total radioactivity in whole blood: 10.6 µgEq/L. LLOQ lower limit of quantification, SD standard deviation
3.2.3 Pharmacokinetics of Total Radioactivity in Whole Blood and Plasma
After a single oral 50-mg dose of [14C]eliapixant, a similar concentration–time profile as seen in plasma was determined in whole blood (Fig. 3b). The geometric mean blood to plasma concentration ratio of total radioactivity appeared constant during the first 8 h after administration of a single 50-mg dose of [14C]eliapixant, ranging between 0.74 (at 0.5 h) and 0.76 (at 1 h), and remained stable thereafter with geometric mean values of 0.72 at 12 h and 0.68 at 24 h. The distribution of total radioactivity was mainly restricted to the plasma, with a geometric mean blood to plasma ratio of total radioactivity of 0.57 for AUC and 0.76 for Cmax.
The maximum geometric mean concentration (%CV) of total radioactivity in both whole blood [158 µgEq/L (21.6%)] and plasma [208 µgEq/L (19.5%)] was measured after a median tmax of 1.0 h. The geometric mean AUC (%CV) of total radioactivity was 1780 µgEq·h/L (26.8%) in whole blood and 3140 µgEq·h/L (34.8%) in plasma with geometric mean t1/2 of 12.8 h in whole blood and 28.0 h in plasma. The shorter t1/2 of total radioactivity in blood versus plasma is likely due to differences in the observation periods (tlast 24 hours and 72 hours, respectively).
3.2.4 Total Radioactivity in Urine and Feces
Almost complete mean recovery of drug-derived radioactivity was observed with arithmetic mean ± SD of %AE,ur+fec(0–tlast) of 97.9% ± 2.1% (94.3–99.4%) of the administered dose within 336 h (14 days). The mean cumulated excretion of radioactivity in urine and feces up to 14 days post-dose is shown in Fig. 4.
Total radioactivity was mainly excreted via feces with %AE,fec(0–tlast) of 86.3% ± 1.2% (84.8–88.1%). By the end of day 6, 89.7% of the administered radioactivity was already excreted in feces plus urine in all subjects. About half (51.9%) of the administered total radioactivity was recovered in feces after 3 days and 81.2% after 8 days. For one subject, further excretion of total radioactivity was quantified on day 22 and day 29. The excreted amount was very low and had no impact on mean AE,ur+fec value on the respective days. Of the 11.6% ± 1.3% (9.5–13.1%) of administered total radioactivity excreted in urine, 9.7% had been excreted 3 days after dosing. No loss of total radioactivity dose due to vomiting was documented in any of the subjects within the first 12 h after [14C]eliapixant administration.
3.2.5 Metabolite Profiling in Plasma
In the mass balance study, eliapixant was the most prominent component detected in plasma (72.6% of total radioactivity AUC) with trace amounts of M4, M5, M8, M10, and M25 (produced by oxidation of M5) detected via radiochromatographic and HPLC–MS methods, and M2, M3, M6, M23, and the hydrolysis product M24, only detected by the more sensitive HPLC–MS methods, probably contributing to the remaining percentage of drug-related components (data not shown). Figure 5 shows a representative radiochromatogram from plasma at 4 h. As they were only detected in trace amounts, no meaningful pharmacokinetic parameters could be calculated for the metabolites. Pharmacokinetic parameters for eliapixant based on bioanalytical analyses (HPLC–MS/MS) are shown in the Supplementary Material, Table S3.
In the exploratory metabolite analyses of pooled plasma data from phase I studies, eliapixant was the major component after a single 400-mg dose [14] (84% of the sum of AUC of all drug-related components whether fasting or non-fasting) or multiple 200-mg twice-daily doses [13] (85% and 88% of the sum of AUC of all drug-related components on day 1 and day 13, respectively). No major metabolites were detected, defined as having an AUC > 10% of the total drug-related AUC, following repeated eliapixant administration. M8 was the main metabolite in human plasma, representing 6.0% and 3.7% of the sum of AUC of all drug-related components on day 1 and day 13, respectively, after doses of eliapixant 200 mg twice daily. M2, M4, M5, M6, M8, and M10 were each circulating at exposures of < 10% of the sum of AUC of all drug-related components (Table 5). Additionally, a small amount of M3 (< 1% of the sum of AUC of all drug-related components) was detected. As concentrations of M3 were below the lower limit of quantification (LLOQ), no pharmacokinetic parameters were calculated for this metabolite.
3.2.6 Metabolite Profiling in Urine and Feces
In urine samples, excretion of unchanged eliapixant into urine amounted to 0.5% of excreted total radioactivity of the administered dose. Metabolites M4 and M8 were the predominant components of excreted total radioactivity accounting for 4.4% and 2.6% of the administered dose, respectively, while M10 represented 1.5% of the dose. M5 and the oxidation products M7, M9, M14/M16/M17, M18, M19, M23, M25, and M29 were present in low amounts, each representing < 0.8% of the administered dose (in total accounting for 1.4% of the administered dose). Figure 6 shows a representative radiochromatogram from urine over 0–12 h.
Excretion of unchanged eliapixant into feces only accounted for 0.7% of excreted total radioactivity of the administered dose. M4 and M9 represented the majority of excreted total radioactivity (30.5% and 23.1% of dose, respectively) in fecal samples. Metabolites M23 and M8 represented 9.7% and 8.3% of the dose, respectively. M5, M6, and the additional oxidized metabolites M7, M14/M16/M17, M18, M25/M30, M26, M29, and M31 each accounted for less than 2.7% of the dose (in total representing 11.6% of the dose). Figure 7 shows a representative radiochromatogram from feces over 24–48 h.
Figure 8 shows mass balances of eliapixant and metabolites in fecal and urine samples following a 50-mg dose of [14C]eliapixant.
Mass balances (other categories include metabolites with percentages < 1% and not balanced percentage of dose. Hashed segments refer to recovered from urine, solid segments refer to recovered from feces) of eliapixant and metabolites in fecal and urine samples following a 50-mg dose of [14C]eliapixant. The values shown are percentages of the dose administered. F feces, U urine
3.2.7 Safety
Five subjects (83.3%) reported AEs, all of mild intensity. The AEs reported were fatigue and headache, each in two subjects (33.3%) and abnormal gastrointestinal sounds, asthenia, non-cardiac chest pain, dizziness, insomnia, and pollakiuria, each in one subject (16.7%). None of the AEs were considered related to [14C]eliapixant by the investigator. No procedure-related AEs, AEs leading to discontinuation of the study drug, SAEs, or deaths were reported. The estimated mean total effective radiation dose was 0.09 mSv per subject after oral administration of 3.83 MBq [14C]eliapixant. This was slightly lower than the radiation burden estimation made before the study (0.11 mSv).
4 Discussion
This characterization of metabolism and elimination pathways of eliapixant, a highly potent and selective P2X3 receptor antagonist, included both in vitro and clinical investigations. The phase I study reported here was conducted to investigate the plasma pharmacokinetics, mass balance, and biotransformation of eliapixant given as an oral solution in healthy male subjects. Pharmacokinetic analysis of eliapixant and total radioactivity showed rapid absorption of eliapixant and a long t1/2, in line with previous eliapixant pharmacokinetics reports [13, 14]. The difference in t1/2 between eliapixant in plasma (48.3 h) and that determined for total radioactivity in plasma (28.0 h) and blood (12.8 h) in the current study may be related to the shorter observation period for the lower sensitivity radioactivity measurement, which did not allow for adequate monitoring of the terminal elimination phase as compared with the longer observation period with the higher sensitivity HPLC–MS method. Of interest, the almost unchanged geometric mean of the whole blood to plasma concentration ratio of total radioactivity during the first 24 h after dosing indicates that the majority of total radioactivity representing parent eliapixant and metabolites was distributed in plasma and not notably distributed into cellular components such as erythrocytes. Almost complete recovery of administered total radioactivity was observed via combined excretion in urine and feces (97.9%) within 14 days after dosing, with the main excretion pathway being via feces and to a much lesser extent via urine.
Metabolite profiling in plasma, feces, and urine showed that unchanged eliapixant was the predominant component in plasma with only trace amounts of metabolites M4, M5, M8, M10, and M25 detected by radiochromatographic methods and further metabolites were only detected in non-quantifiable amounts by HPLC–MS methods. These results were in good agreement with the exploratory analysis of samples from previous phase I studies [13, 14]. Of the 86.3% of the radioactive dose excreted in feces, more than 70% was in the form of metabolites M4, M8, M9, and M23, with only 0.7% of the dose attributed to unchanged eliapixant. The presence of metabolite M8 in feces may partly be due to hydrolytic cleavage of the glucuronide M28 in the intestinal milieu (e.g., by microbial flora). Similarly, of the 11.6% of the radioactive dose excreted in urine, the predominant components M4 and M8 accounted for 7% of the dose, with eliapixant only detected in negligible amounts. These results indicate that eliapixant is primarily metabolized by phase I metabolism at the tetrahydrofuran moiety as well as at the methyl thiazole group. The mass balance study confirmed the biotransformation pathways seen in vitro in human liver microsomes and hepatocytes (oxidation, ring opening, and cleavage of the tetrahydrofuran moiety, and oxidation of the methyl thiazole moiety), indicating hepatic biotransformation of eliapixant as the main elimination pathway. The metabolites identified in the hepatocytes and cytosol were also detected in excreta.
Further in vitro studies identified CYP3A4 as the major enzyme responsible for catalyzing the hepatic phase I biotransformation of eliapixant. Although recombinant CYP2J2 catalyzed oxidative metabolism of eliapixant, CYP2J2-selective inhibitors showed no impact on turnover of eliapixant in human hepatocytes, which may be explained by the very low relative abundance of CYP2J2 in the liver. The individual contribution of the pathways mediated by CYP1A1, CYP1A2, and CYP2D6 to the oxidative hepatic metabolism of eliapixant were very minor. The results suggest that there may be a risk for clinically relevant drug–drug interactions when coadministering strong CYP3A4 inhibitors with eliapixant. In a clinical study evaluating the effect of coadministering the strong CYP3A4 inhibitor itraconazole with eliapixant, only a mild-to-moderate effect (with approximately a two-fold increase in total exposure) was observed [14]. These data suggest a fraction metabolized via CYP3A4 of ~ 0.5, while results from the current mass balance study, in line with the in vitro results, indicate a fraction metabolized of ~ 0.8. The cause of this discrepancy between the studies is currently unknown. Since the study cited above was performed, a novel tablet formulation of eliapixant has been introduced, providing approximately threefold greater AUC than the previous formulation and absolute bioavailability of 50% [12]. Further investigations would have been warranted with the current clinical formulation and at the proposed therapeutic dose.
In this two-part clinical study, an oral eliapixant solution was evaluated in combination with a high-fat high-calorie meal because the bioavailability of eliapixant with a standard immediate-release tablet is known to be poor and prone to relevant food effects [12, 14]. Conducting an initial small pharmacokinetic study to allow a comparison of key eliapixant pharmacokinetic parameters with historic data successfully minimized the risk of failure of the mass balance study due to inappropriate selection of dose and formulation.
As usual for studies of this type, this study was performed in healthy men and its results may not be fully generalizable to other populations. Limitations of the current study included the younger mean age of subjects than the targeted patient population, which could slightly alter the metabolism and excretion characteristics of eliapixant.
5 Conclusion
In summary, the data indicate an almost complete recovery of the administered eliapixant dose with predominant excretion via feces. Eliapixant is mainly excreted metabolically with CYP3A4 as the predominant enzyme involved.
References
Burnstock G. Purinergic mechanosensory transduction and visceral pain. Mol Pain. 2009;5:69.
Bernier LP, Ase AR, Seguela P. P2X receptor channels in chronic pain pathways. Br J Pharmacol. 2018;175(12):2219–30.
Cockayne DA, Dunn PM, Zhong Y, Rong W, Hamilton SG, Knight GE, Ruan HZ, Ma B, Yip P, Nunn P, McMahon SB, Burnstock G, Ford AP. P2X2 knockout mice and P2X2/P2X3 double knockout mice reveal a role for the P2X2 receptor subunit in mediating multiple sensory effects of ATP. J Physiol. 2005;567(Pt 2):621–39.
Ding S, Yu Q, Wang J, Zhu L, Li T, Guo X, Zhang X. Activation of ATF3/AP-1 signaling pathway is required for P2X3-induced endometriosis pain. Hum Reprod. 2020;35(5):1130–44.
Fabbretti E. ATP P2X3 receptors and neuronal sensitization. Front Cell Neurosci. 2013;7:236.
Ford AP. In pursuit of P2X3 antagonists: novel therapeutics for chronic pain and afferent sensitization. Purinergic Signal. 2012;8(Suppl 1):3–26.
Song WJ, Morice AH. Cough hypersensitivity syndrome: a few more steps forward. Allergy Asthma Immunol Res. 2017;9(5):394–402.
Morice A, Smith JA, McGarvey L, Birring SS, Parker SM, Turner A, Hummel T, Gashaw I, Fels L, Klein S, Francke K, Friedrich C. Eliapixant (BAY 1817080), a P2X3 receptor antagonist, in refractory chronic cough: a randomised, placebo-controlled, crossover phase 2a study. Eur Respir J. 2021;58(5):2004240.
Fletcher MC. Selectivity of the P2X3 receptor antagonist eliapixant, and its potential use in the treatment of endometriosis. Purinergic Signal. 2022;18(1):1–3.
Dicpinigaitis PV, Morice AH, Smith JA, Sher MR, Vaezi M, Guilleminault L, Niimi A, Gude K, Krahn U, Saarinen R, Pires PV, Wosnitza M, McGarvey L, on behalf of the PAGANINI Investigators. Efficacy and safety of eliapixant in refractory chronic cough: the randomized, placebo-controlled phase 2b PAGANINI study. Lung. 2023;1–12.
Klein S, Gashaw I, Baumanna S, Chang X, Hummel T, Thuss U, Friedrich C. First-in-human study of eliapixant (BAY 1817080), a highly selective P2X3 receptor antagonist, in healthy volunteers: tolerability, safety and pharmacokinetics. Br J Clin Pharmacol. 2022;88(10):4552–64.
Francke K, Chattopadhyay N, Klein S, Rottmann A, Krickau D, van de Wetering J, Friedrich C. Preclinical and clinical pharmacokinetics and bioavailability in healthy volunteers of a novel formulation of the selective P2X3 receptor antagonist eliapixant. Eur J Drug Metab Pharmacokinet. 2023;48(1):75–87.
Friedrich C, Francke K, Gashaw I, Scheerans C, Klein S, Fels L, Smith JA, Hummel T, Morice A. Safety, pharmacodynamics, and pharmacokinetics of P2X3 receptor antagonist eliapixant (BAY 1817080) in healthy subjects: double-blind randomized study. Clin Pharmacokinet. 2022;61(8):1143–56.
Klein S, Gashaw I, Baumann S, Chang X, Hummel T, Thuß U, Friedrich C. First-in-human study of eliapixant (BAY 1817080), a highly selective P2X3 receptor antagonist: tolerability, safety and pharmacokinetics. Br J Clin Pharmacol. 2022;88(10):4552–64.
Acknowledgments
The authors thank all the volunteers who participated in the study and the investigator team at PRA Health Science (now ICON), Groningen, for their assistance in conducting the study. Thanks are also due to the following (all employees of Bayer AG): Detlef Obst and Sabine Backhus for conducting in vitro experiments and exploratory analyses; Alexandra Neumann and Daniela Schaefer for conducting in vitro experiments; Martina Blombach and Dirk Gäfke for technical support in analyzing the mass balance study samples; Klaudia Grunenberg for analysis of human in vivo samples; and Ercan Sükür for pharmacokinetic evaluation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Bayer AG.
Conflicts of interest
Antje Rottmann, Isabel Piel, Karsten Denner, Marcus-Hillert Schultze-Mosgau, Klaus Francke, Stefanie Reif, and Stefan Klein are employees of Bayer AG. Anna Engelen was an employee of Bayer AG at the time the study was designed and conducted and is now an employee of Boehringer Ingelheim, Drug Discovery Sciences, Germany. Renger Tiessen and Ad Roffel are employees of ICON plc., Groningen, the Netherlands, formerly PRA Health Sciences, Groningen, the Netherlands. PRA Health Sciences were contracted by Bayer AG to perform the study.
Ethics approval
Both parts of the mass balance study were approved by the Medical Research Ethics Committee of the Beoordeling Ethiek Biomedisch Onderzoek (BEBO) Foundation, Assen, the Netherlands and conducted in accordance with the ethical principles that have their origins in the Declaration of Helsinki and the International Council for Harmonisation guidelines on Good Clinical Practice. The Central Committee on Research Involving Human Subjects [Centrale Commissie Mensgebonden Onderzoek (CCMO)] number was NL7431.056.20, and the EudraCT number was 2020-000519-54. The study was approved by the accredited ethics committee on 27 July 2020.
Consent to participate
All subjects in both study parts provided written informed consent.
Consent for publication
Not applicable.
Code availability
Not applicable.
Data availability
Availability of the data underlying this publication will be determined according to Bayer’s commitment to the European Federation of Pharmaceutical Industries and Associations and Pharmaceutical Research and Manufacturers of America principles for responsible clinical trial data sharing, pertaining to scope, timepoint, and process of data access. Bayer commits to sharing, upon request from qualified scientific and medical researchers, patient-level clinical trial data, study-level clinical trial data, and protocols from clinical trials in patients for medicines and indications approved in the USA and European Union as necessary for performing legitimate research. This commitment applies to data on new medicines and indications that have been approved by the European Union and US regulatory agencies on or after 1 January 2014. Interested researchers can use https://www.clinicalstudydatarequest.com to request access to anonymized patient-level data and supporting documents from clinical studies to perform further research that can help advance medical science or improve patient care. Information on the Bayer criteria for listing studies and other relevant information is provided in the study sponsors’ section of the portal. Access will be granted to anonymized patient-level data, protocols, and clinical study reports after approval by an independent scientific review panel. Bayer is not involved in the decisions made by the independent review panel. Bayer will take all necessary measures to ensure that patient privacy is safeguarded.
Author contributions
Antje Rottmann, Isabel Piel, Anna Engelen, Karsten Denner, and Klaus Francke made substantial contributions to the conception or design of the work and the acquisition, analysis, and interpretation of the data. Marcus-Hillert Schultze-Mosgau and Stefanie Reif made significant contributions to the conception or design of the work, and analysis and interpretation of data. Stefan Klein made significant contributions to conception of the work and analysis of data. Ad Roffel and Renger Tiessen made significant contributions to the conception of the work and the acquisition and analysis of data. All authors drafted the manuscript or revised it critically for important intellectual content. All authors read and approved the final version of the manuscript and agreed that it should be published. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Medical writing support
Medical writing services were provided by Richard Murphy, PhD of Adelphi Communications Ltd, Macclesfield, UK and funded by Bayer AG, Berlin, Germany in accordance with the Good Publication Practice guidelines, 2022.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reif, S., Schultze-Mosgau, MH., Engelen, A. et al. Mass Balance and Metabolic Pathways of Eliapixant, a P2X3 Receptor Antagonist, in Healthy Male Volunteers. Eur J Drug Metab Pharmacokinet 49, 71–85 (2024). https://doi.org/10.1007/s13318-023-00866-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-023-00866-0