Abstract
Background and Objectives
Morbidity and mortality from serious infections are common in intensive care units (ICUs). The appropriateness of the antibiotic treatment is essential to combat sepsis. We aimed to evaluate pharmacokinetic/pharmacodynamic target attainment of meropenem and piperacillin/tazobactam administered at standard total daily dose as continuous infusion in critically ill patients without renal dysfunction and to identify risk factors of non-pharmacokinetic/pharmacodynamic target attainment.
Results
We included 118 patients (149 concentrations), 47% had microorganism isolation. Minimum inhibitory concentration (MIC) [median (interquartile range, IQR) values in isolated pathogens were: meropenem: 0.05 (0.02–0.12) mg/l; piperacillin: 3 (1–4) mg/l]. Pharmacokinetic/pharmacodynamic target attainments (100%fCss≥1xMIC, 100%fCss≥4xMIC and 100%fCss ≥ 8xMIC, respectively) were: 100%, 96.15%, 96.15% (meropenem) and 95.56%, 91.11%, 62.22% (piperacillin) for actual MIC; 98.11%, 71.70%, 47.17% (meropenem, MIC 2 mg/l), 95.83%, 44.79%, 6.25% (piperacillin, MIC 8 mg/l), 83.33%, 6.25%, 1.04% (piperacillin, MIC 16 mg/l) for EUCAST breakpoint of Enterobacteriaceae spp. and Pseudomonas spp. Multivariable linear analysis identified creatinine clearance (CrCL) as a predictive factor of free antibiotic concentrations (fCss) of both therapies (meropenem [β = − 0.01 (95% CI − 0.02 to − 0.0; p = 0.043)] and piperacillin [β = − 0.01 (95% CI − 0.02 to 0.01, p < 0.001)]). Neurocritical status was associated with lower piperacillin fCss [β = − 0.36 (95% CI − 0.61 to − 0.11; p = 0.005)].
Conclusion
Standard total daily dose of meropenem allowed achieving pharmacokinetic/pharmacodynamic target attainments in ICU patients without renal dysfunction. Higher doses of piperacillin/tazobactam would be needed to cover microorganisms with MIC > 8 mg/l. CrCL was the most powerful factor predictive of fCss in both therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Standard doses of meropenem allowed achieving pharmacokinetic/pharmacodynamic target attainments |
Higher doses of piperacillin/tazobactam would be needed to cover microorganisms with MIC > 8 mg/l |
CrCL was predictive of fCss in both therapies |
1 Introduction
Morbidity and mortality due to severe infections are prevalent in intensive care units (ICUs). Antibiotic-resistant infections are expanding [1], and this situation demands several measures, such as (1) to use old antibiotics, (2) to develop new therapies and (3) to optimize existing therapies [2]. Therapeutic interventions and external artifacts may contribute to pharmacokinetic/pharmacodynamic antimicrobial alterations and variability [3, 4]. Antibiotic therapies in the ICU remain challenging since standard dosage guidelines might be unsuitable and fail to achieve pharmacokinetic/pharmacodynamic target attainment [2].
To achieve clinical cure and bacteriologic eradication, it is traditionally believed that it is sufficient to keep plasma concentrations of β-lactams above the minimum inhibitory concentration (MIC) during 40–70% of the time in mild/moderate infections [1, 5, 6]. Nevertheless, longer exposure times (e.g., 100%fT ≥ MIC) might be required for critically ill patients [3, 7, 8]. Besides, clinical data suggest that β-lactam concentration should be between four and eight times above MIC to maximize bacterial killing and to avoid resistances [1, 8,9,10,11].
Previous pharmacokinetic studies showed that continuous infusion of β-lactam provided several advantages compared to intermittent administration: (1) higher percentage of antibiotic concentration values greater than the MIC (100% vs. 22% and 75% vs. 36% for meropenem [MER] and piperacillin/tazobactam [PIP/TAZ], respectively) [12], even with lower daily doses of PIP/TAZ than the standard regimen [13]; (2) higher concentrations of meropenem in both plasma and subcutaneous tissue [14]; (3) similar or higher clinical cure rates [8, 15]. These data support the use of continuous β-lactam infusion in ICU patients and offer an encouraging administration alternative [16].
The primary aim was to explore whether standard total daily dose of MER and PIP/TAZ [17, 18] administered by continuous infusion achieved optimal pharmacokinetic/pharmacodynamic targets in the actual hospital environment. We also wanted to identify risk factors associated with subtherapeutic exposure and failure to attain pharmacokinetic/pharmacodynamics targets.
2 Patients and Methods
2.1 Ethical Issues
The study was approved by the local Ethics Committee (SFB-ATB-2014-01) and conducted following the Declaration of Helsinki. Written informed consent was requested of the patient or the closest relative before inclusion.
2.2 Study Setting
This pharmacokinetic prospective and observational study was carried out over a 3-year period (June 2015–September 2018) in a 34-bed mixed ICU at Hospital Universitari de Bellvitge (Barcelona), a 700-bed teaching hospital in the southern metropolitan area of Barcelona.
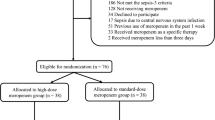
Inclusion criteria were: (1) patient ≥ 18 years old with sepsis according to the Survival Sepsis Campaign Guidelines [19]; (2) under MER or (PIP/TAZ) therapy and (3) creatinine clearance (CrCL) ≥ 60 ml/min/1.73 m2. Exclusion criteria were: (1) pregnancy or (2) impaired renal function (CrCL < 60 ml/min/1.73 m2 or renal replacement therapy).
Patients received a loading dose followed by the total daily dose in continuous infusion, i.e., 4/0.5 g followed by 12/1.5 g q24h of PIP/TAZ (80 mg/ml in 0.9% saline, stability of 24 h at 25 °C, 1 infusion/day) and 1 g followed by 3 g q24h of MER (22 mg/ml in 0.9% saline, stability of 17 h at 25 °C, 2 infusions/day) [20]. Patients who had started antibiotic therapy with intermittent infusion in the previous 24 h did not receive the loading dose, because it was considered they had already achieved the steady state.
2.3 Bioanalytical Assay
Total plasma concentrations were determined through previously validated methods of ultra-performance liquid chromatography-tandem coupled to mass spectrometry (UHPLC-MS/MS) [21]. The mobile phase consisted of a mixture of solution A (0.1% formic acid in water) and solution B (0.1% formic acid in acetonitrile) with an initial composition of 5% solution B. The mobile phase flow rate was maintained at 0.4 ml/min using a gradient mode elution. For chromatography, an Acquity® UPLC® BEHTM C18 reverse-phase column (100 × 2.1 mm id; 1.7 µm) was used. A simple procedure for protein precipitation was used to prepare the samples. Piperacillin-d5 and meropenem-d6 were used as internal standard for PIP and MER, respectively.
Inter-day lower limits of quantification (LLOQ) were 0.50 mg/l for MER (signal-to-noise [S/N] ratio of 5.5) and 0.54 mg/l for PIP (S/N ratio of 5.6). The calibration curve ranged from 0.50 to 175 mg/l for MER (a quadratic regression curve with a weighting scheme of 1/X2) and from 0.54 to 175 mg/l for PIP (a linear regression curve with a weighting scheme of 1/X). For MER, inter-day coefficients of variation (CV) obtained were 10.1%, 7.4% and 4.9% at 3.22, 30.9 and 126 mg/l, respectively; the relative biases (δr) were 7.3%, 3.0% and 4.6% at the same values. For PIP, the CVs were 8.9%, 6.7% and 3.5% at 3.13, 31.5 and 124 mg/l; the δrs were 4.3%, 5.0% and 3.3%.
Blood samples were obtained 24–48 h after the beginning of β-lactam continuous infusion (steady-state condition). Approximately 3 ml of blood was collected in lithium-heparin tubes (Vacuette, Kremsmünster, Austria) and immediately refrigerated at 2–8 °C for a maximum of 30 min. Samples were then centrifuged at 2000g for 10 min at (4 ± 1) °C, aliquoted and stored at (− 75 ± 3) °C until analysis [21].
We calculated free antibiotic concentrations (fCss) considering protein bindings (2% and 30% for MER and piperacillin [PIP], respectively) [22]. As upper limit of the therapeutic window, we adopted PIP Css of 157 mg/l [9, 23] and MER Css of 45 mg/l [14, 24].
2.4 Study Cohort Data
All data were collected from the electronic medical information, and we calculated CrCL from serum creatinine concentrations according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula. We established three groups according to the following CrCL cut-offs: 60–89; 90–119 (female) or 90–129 (male); and ≥ 120/130 (female/male) ml/min/1.73 m2. Finally, we defined augmented renal clearance (ARC) as a CrCL ≥ 120/130 (female/male) ml/min/1.73 m2 [25]. We considered neurocritical care patients as those with traumatic brain injury or subarachnoid haemorrhage.
2.5 Exposure and Pharmacokinetic Parameters
The achieved exposure was given by the free antibiotic concentrations (fCss) and the area under the curve of free concentrations at steady state (fAUCss). We calculated unbound plasma clearance (CLu) and fAUCss according Eqs. 1 and 2, respectively [26]:
2.6 Pharmacokinetic/Pharmacodynamic Endpoints
The pharmacokinetic/pharmacodynamic target was to achieve fCss exceeding the pathogen MIC during 100% of the dosing interval (100%fT). We defined three pharmacokinetic/pharmacodynamic targets: (1) fCss during 100%fT ≥ 1xMIC (fCss/MIC ≥ 1); (2) fCss during 100%fT ≥ 4xMIC (fCss/MIC≥4) and (iii) fCss during 100%fT ≥ 8xMIC (fCss/MIC≥8).
We determined actual MIC values at isolated pathogens by the Etest® method. Otherwise, we inferred the highest MIC in the susceptible range from the European Committee on Antimicrobial Susceptibility Testing (EUCAST) [27]: Pseudomonas spp., 16 mg/l for PIP and 2 mg/l for MER; Enterobacteriaceae, 8 mg/l for PIP and 2 mg/l for MER.
2.7 Evaluation Endpoints
We analysed pharmacokinetic/pharmacodynamic target attainment either as binary (expressed as number or percentage of attainments) or as continuous dependent variables (expressed as fCss/MIC ratio). Similarly, we studied the influence of clinical, physiological and mechanical factors on the antibiotic exposure, given by both fCss and fAUCss.
2.8 Statistical Analysis
We summarized descriptive statistics of continuous variables as median [interquartile range (IQR) or range] or mean [standard deviation (SD)] and the categorical variables as numbers and percentages. We presented fCss, fAUCss and CLu values and fCss/MIC ratios as geometric means with 95% confidence interval (CI). Results of pharmacokinetic/pharmacodynamic target attainment by MIC and breakpoint at the sample level were presented as numbers and percentages.
To examine predictors of final outcomes, considered as continuous variables, we performed univariate and multivariable linear regression analyses. Due to sample size considerations, we only performed statistical evaluation from pharmacokinetic/pharmacodynamic values estimated from surrogate MICs. In univariate analyses, we made comparisons of mean fCss/MIC ratios, fCss, fAUCss and CLu between groups created from different levels within each risk factor. We used a two-way analysis of variance with variables included as fixed factors and patient considered as a random factor nested within these variables.
We included independent factors that showed, in univariate analysis, a significant effect on the outcome, in a multivariable regression model to investigate independent predictors of fCss/MIC ratios. In multivariable regression analysis, we used a mixed model with the patient as a cluster and the logarithmic transformation of the dependent variable.
In all multivariable analyses, we used stepwise procedures based on forward inclusion/backward elimination methods. We performed statistical analyses using R version 3.5.1. and set statistical significance to p < 0.05 in all the cases.
3 Results
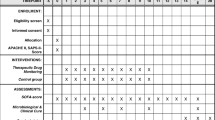
3.1 Population and Samples
During the study period, 118 patients were included, and 149 samples were analysed [96 (64.4%) and 53 (35.6%) for PIP and MER, respectively]. Only 24 (20%) patients had more than one plasma sample. Baseline patient characteristics, clinical, microbiological data and concentrations achieved are shown in Table 1. Most patients (64.4%) had CrCL ≥ 90 ml/min/1.73 m2 and 60.2% had body mass index (BMI) ≥ 25 kg/m2. Median (IQR) MIC value in isolated pathogen was 0.05 (0.02–0.12) mg/l for MER and 3 (1–4) mg/l for PIP. Median fCss was 15.8 (IQR: 7.35–32.3) mg/l and 26.8 (IQR: 17.5–42.6) mg/l for MER and PIP, respectively. Eight meropenem Css values were > 45 mg/l but we did not find any adverse events.
3.2 Pharmacokinetic/Pharmacodynamic Target Attainment
Table 2 shows the results for pharmacokinetic/pharmacodynamic target attainment considering two scenarios (actual or surrogate MIC values). Usually, we observed higher percentages of achievement with actual MIC values. Achievement of MER pharmacokinetic/pharmacodynamic targets using surrogate MIC was similar (fCss/MIC ≥ 1) (98.11% vs. 100%), 25% lower (71.70% vs. 96.15%) (fCss/MIC ≥ 4) and 49% lower (47.17% vs. 96.15%) (fCss/MIC ≥ 8) than those observed considering actual MICs. In the PIP cohort, we observed a similar trend with similar percentages (fCss/MIC ≥ 1) (95.83% vs. 95.56%) or reductions of 46% (44.79 % vs. 91.11%) (fCss/MIC ≥ 4) and 56% (6.25% vs. 62.22%) (fCss/MIC ≥ 8) when surrogate MIC 8 mg/l was evaluated and of 12% (83.33% vs. 95.56%) (fCss/MIC ≥ 1), 84% (6.25% vs. 91.11%) (fCss/MIC ≥ 4) and 61% (1.04% vs. 62.22%) (fCss/MIC ≥ 8) when surrogate MIC 16 mg/l was considered.
3.3 Influence of Clinical Factors on Exposure, Pharmacokinetic Parameters and Pharmacokinetic/Pharmacodynamic Target Values
Results of the effect of the tested clinical factors on exposure (fCss, fCss/MIC, fAUCss) and pharmacokinetic parameters (CLU) are shown in Table 3. Univariate comparisons evidenced that, for MER, a trend to lower fCss values occurred in patients with CrCL ≥ 90 ml/min/1.73 m2 with respect to those with CrCL of 60–89 ml/min/1.73 m2 (fCss: 12.5 vs. 22.8 mg/l, p = 0.072). Similarly, overweight patients (BMI ≥ 25 kg/m2) presented almost half the exposure of those with BMI ≤ 24.9 kg/m2 (fCss: 11.6 vs. 20.0 mg/l, p = 0.118). Although these were the most influential covariates, no statistical significance was reached in any case. Patients under mechanical ventilation (fCss 12.6 vs. 17.8 mg/l, p = 0.34) and post-surgical drainage (fCss: 10 vs. 17.9 mg/l, p = 0.219) also tended to lower fCss values than the others, but statistical significance was not achieved. The trend shown in fCss values of patients treated with vasoactive drugs with respect to those that did not receive this treatment (fCss: 16.5 vs. 14.2 mg/l, p = 0.058) could be attributed to the high variability observed. One patient of the group that received the treatment showed much higher exposure (fCss = 96 mg/l) than the others, this contributing to these results.
In patients under PIP treatment, CrCL was the most influential covariate (p = 0.005) followed by neurocritical status (fCss 22.2 vs. 30.3 mg/l, p = 0.008) and mechanical ventilation (fCss 23 vs. 32.6 mg/L, p = 0.024). Patients with CrCL values ≥ 90 ml/min/1.73 m2 had lower exposures than the others (fCss 23 vs. 36.6 mg/l, p = 0.001) (Table 3, Fig. 1 and Supplementary file: Fig. 1S). Figure 2 displays the statistically significant correlation between fCss/MIC values and CrCL when surrogate MIC values (8 and 16 mg/l) were considered. An inversely proportional linear relationship is observed so that it is showed that 15.2% of the variation of the fCss/MIC value is due to the progressive increase of the CrCL.
Boxplot of piperacillin fCss/MIC ratio distributions, according to surrogate MIC values, sorted by each category within each variable. Footnote: The fCss/MIC distributions based on surrogate MIC values of 8 and 16 mg/l were the same, so only the boxplots for MIC 8 mg/l are represented. The bottom and top extremes of the box represent the first (Q1) and the third quartile (Q3) range of the data, respectively (Q3–Q1: interquartile range). The dark horizontal line in the box is the median and dots are the observed values. The bottom and top whiskers represent the Q1 – 1.5 times the IQR value and Q3 + 1.5 times the IQR values, respectively. fCss free antibiotic concentrations, MIC minimum inhibitory concentration. fCss/MIC ratio of fCss to surrogate MIC values (8 and 16 mg/l for piperacillin), BMI body mass index, CrCL creatinine clearance value (ml/min/1.73m2), calculated with the CKD-EPI equation
Correlation between CrCL and fCss/MIC ratios for piperacillin concentrations. Footnote: MIC values of 8 mg/l (A) and 16 mg/l (B). Creatinine clearance (CrCL) value (ml/min/1.73 m2) was calculated with the CKD-EPI equation. fCss free antibiotic concentrations, MIC minimum inhibitory concentration, fCss/MIC ratio of fCss to surrogate MIC values (8 mg/l or 16 mg/l), R2 coefficient of determination
The multivariable analysis showed the statistically significant effect of CrCL on MER exposure after adjusting by BMI. This finding was probably due to the reduction of variability associated with fCss values after inclusion of BMI in the multivariable analysis. However, its effect was not statistically significant, suggesting that BMI acts as a confounder due to its relationship with both the CrCL and the fCss. Thus, the final multivariable model included CrCL [β = − 0.01 (95% CI − 0.02 to − 0.0; p = 0.043)] as a significant factor that influenced MER exposure.
Regarding PIP, we could not find any statistically significant effect of mechanical ventilation on the fCss/MIC ratio when this covariate was entered on the multivariable model. Of note, in univariate analysis, it was the less influential covariate among those mentioned above. In PIP, the negative predictors of target achievement were CrCL [β = − 0.01 (95% CI − 0.02 to − 0.01, p < 0.001)] and neurocritical status [β=− 0.36 (95% CI − 0.61 to − 0.11, p = 0.005)] (see Supplementary file: Table 1S).
4 Discussion
Considering the actual MIC of isolated microorganisms (55, 47% of patients), our results suggest that standard doses of MER would reach 100%fT ≥ 1xCMI, 100%fT ≥ 4xCMI and 100%fT ≥ 8xCMI in > 96% of occasions. In the case of PIP/TAZ, also 100%fT ≥ 1xCMI and 100%fT ≥ 4xCMI were reached in more than 90% of occasions but higher PIP/TAZ doses would be needed to achieve the most ambitious target (100%fT ≥ 8xCMI).
Isolated pathogens had median MIC values much lower than the EUCAST cut-off [0.05 mg/l vs. 2 mg/l (MER) and 3 mg/l vs. 8 or 16 mg/l (PIP)]. Therefore, we found lower percentages of achievement when we considered the more conservative surrogate MIC values. We considered our results from the MER cohort (71.7% of 100%fT≥4xCMI target attainment) similar to those from Dhaese et al. [28] (75% of 100%fT ≥ 4xCMI target attainment). Compared to our study, they included patients with slightly higher renal function and more estimated CrCL (Cockroft-Gault equation) variability than ours [mean (SD): 117.8 (68.2) vs. 99.2 (22.5)]. However, fCss values from our MER cohort presented higher variability (range 0.7–96.5 mg/l) than their values (range 2–57.7 mg/l). Fifteen of 53 fCss (28.3%) were < 8 mg/l [vs. 10 of 48 (20.8%) in Dhaese’s study], and 7 fCss values were over the upper limit (vs. 2 in Dhaese’s study). In the PIP cohort, our 100%fT ≥ 1xCMI target attainment was in accordance with previous findings (83.3%) [29]. However, our study showed lower 100%fT ≥ 4xMIC target attainment (6.25%) than Dhaese et al. (37.1%) [28] and Richter et al. (55.6%) [30]. A combination of two situations could have contributed to these differences: (1) the administration of different daily doses of PIP (16 g in Dhaese et al. [28] and 12 g in Richter et al. [30]) with respect to our study (3 g); (2) the inclusion of patients with CrCL < 60 ml/min in Dhaese’s and Richter’s studies.
As reported earlier [29, 31,32,33,34,35], our findings suggest that high renal function is an important risk factor for non-target attainment. As expected for renal-excreted drugs, in the present study, drug concentrations were strongly associated with CrCL. For both antibiotics, CrCL was the most influential covariate in the multivariable analysis (MER, p = 0.043; PIP, p < 0.001) but the strongest relationship between concentration and CrCL was found for PIP. On the other hand, Carlier et al. [31] observed a higher impact of CrCL on pharmacokinetic/pharmacodynamic target attainment for MER than ours, i.e., 2.8% less probability to reach 100%fT≥CMI when CrCL increased [β − 0.028; 95% CI for Exp (β): 0.955–0.990; p < 0.002]. This estimation was obtained with multivariate logistic analysis. In our case, in multivariate linear analysis, we observed that for every unit increase in CrCL, fCss/MIC decreased by 1%. They [31] observed a larger range of variation in estimated CrCL, and this could justify the differences from our results. Thus, according to these results, drug monitoring of β-lactams and dose adjustment based on renal function could increase the pharmacokinetic/pharmacodynamic target attainment.
Curiously, in the multivariable analysis, the statistically significant influence of CrCL on MER fCss values (p = 0.043) could only be detected after inclusion in the BMI in the model. This suggested that BMI ≥ 25 kg/m2 could act as a confounding factor because of its association with both fCss and creatinine clearance.
In line with this, patients with BMI ≥ 25 kg/m2 showed lower MER fCss/MIC values (5.8 vs. 10, p = 0.118) compared to patients with BMI < 25 kg/m2. This could be explained by the effects of overweight on either drug clearance or volume of distribution (Vd), as previously reported [36, 37]. No data about Vd values were available in our study, but obese patients showed higher MER clearance than non-obese (10.8 vs. 6.2 l/h, p = 0.118) resulting in lower exposures. Increased kidney size and renal flow could be some of the physiological changes causing higher clearance [36]. Similar results were found by Hites et al. [38], with higher CL values in obese patients and 35% vs. 0% of non-target attainment in obese vs. non-obese patients (p = 0.02). Other authors [39] described a significant relationship between BMI and Vd without affecting pharmacokinetic/pharmacodynamic target attainment. Although post-surgical drainage has been postulated to produce antimicrobial loss because of augmented clearance [40, 41] and a false Vd increase [4, 42, 43], we did not find any significant influence of this covariate on the pharmacokinetic/pharmacodynamic target attainment.
To the best of our knowledge, this is the first study attempting to address the effect of MV on PIP pharmacokinetic/pharmacodynamic target attainment. We identified neurocritical status as an influential covariate for PIP fCss/MIC (p = 0.008). These results were in agreement with recent reports where brain-damaged patients failed to achieve pharmacokinetic/pharmacodynamic targets as they were at particular ARC risk [44,45,46,47]. Moreover, in univariant analysis, the influence of MV was statistically significant (p = 0.024), even though this effect was not retained in the final multivariable model. The lower target attainment in patients with MV could be associated to the effect of positive end-expiratory pressure (PEEP) on Vd [48,49,50,51]. Nevertheless, no data from our study could prove this hypothesis. Although vasoactive drugs could probably increase renal blood flow and thereby drug clearance, this effect could not be shown in the present study.
In the present study, the effect of several factors that had never been previously investigated [28, 30] such as diagnosis, MV, vasoactive drug use, neurocritical status and post-surgical drainage was analysed. We confirmed the lack of independent influence of body weight on target attainment as we analysed the effect of renal function estimated using CKDEPI formula that is independent of body weight. Rather than novelty one of the features of our study is that it was carried out by means of statistical analysis methods compliant with longitudinal data. Moreover, multivariable statistical analyses were performed on the basis of continuous variables rather than categorized or discrete data, this leading to a more powerful and robust analysis. The identification of the predictive capability of the investigated factors on target attainment is crucial for dose individualization during therapeutic drug monitoring in clinical practice.
Some limitations of our study are, first, the small sample size that led to the lack of statistical significance in the MER CL values between ARC and normal renal function. Second, direct urinary creatinine measurement, the most adequate method to assess CrCL, was not routinely available in our centre. Third, pathogens were only grown in 47% of patients and, to obtain robust results, we needed MIC assumptions. Moreover, the use of susceptibility breakpoints could inflate the frequency of sub-threshold levels when drug concentrations were instead adequate because the ‘true’ MIC was substantially lower. Fourth, tazobactam Css was not measured, since its analytical determination was not routinely available in our centre. Finally, this study includes a purely kinetic analysis; thus, we do not presume to draw any conclusions for the clinical outcome.
5 Conclusions
Standard total daily dose of MER (3g q24h) and PIP/TAZ (12/1.5g q24h) administered as a continuous infusion is usually adequate. However, in patients with CrCL ≥ 90 ml/min/1.73m2 (MER and PIP/TAZ), neurocritical status and infections caused by microorganisms with MIC > 8 mg/ (PIP/TAZ) caution is warranted to avoid underdosing. Therapeutic drug monitoring and dose adjustment are highly recommended in these specific situations.
References
Roberts JA, Abdul-Aziz MH, Lipman J, Mouton JW, Vinks AA, Felton TW, et al. Individualised antibiotic dosing for patients who are critically ill: challenges and potential solutions. Lancet Infect Dis. 2014;14(6):498–509. https://doi.org/10.1016/S1473-3099(14)70036-2.
Vardakas KZ, Voulgaris GL, Maliaros A, Samonis G, Falagas ME. Prolonged versus short-term intravenous infusion of antipseudomonal β-lactams for patients with sepsis: a systematic review and meta-analysis of randomised trials. Lancet Infect Dis. 2018;18(1):108–20. https://doi.org/10.1016/S1473-3099(17)30615-1.
Gonçalves-Pereira J, Póvoa P. Antibiotics in critically ill patients: a systematic review of the pharmacokinetics of β-lactams. Crit Care. 2011;15(5):R206. https://doi.org/10.1186/cc10441.
Pea F, Viale P, Furlanut M. Antimicrobial therapy in critically ill patients a review of pathophysiological conditions responsible for altered disposition and pharmacokinetic variability. Clin Pharmacokinet. 2005;44(10):1009–34. https://doi.org/10.2165/00003088-200544100-00002.
De Waele JJ, Carrette S, Carlier M, Stove V, Boelens J, Claeys G, et al. Therapeutic drug monitoring-based dose optimisation of piperacillin and meropenem: a randomised controlled trial. Intensive Care Med. 2014;40(3):380–7. https://doi.org/10.1007/s00134-013-3187-2.
Turnidge JD. The pharmacodynamics of beta-lactams. Clin Infect Dis. 1998;27(1):10–22. https://doi.org/10.1086/514622.
Roberts JA, Kirkpatrick CMJ, Roberts MS, Dalley AJ, Lipman J. First-dose and steady-state population pharmacokinetics and pharmacodynamics of piperacillin by continuous or intermittent dosing in critically ill patients with sepsis. Int J Antimicrob Agents. 2010;35(2):156–63. https://doi.org/10.1016/j.ijantimicag.2009.10.008.
Chytra I, Stepan M, Benes J, Pelnar P, Zidkova A, Bergerova T, et al. Clinical and microbiological efficacy of continuous versus intermittent application of meropenem in critically ill patients: a randomized open-label controlled trial. Crit Care. 2012;16(3):R113. https://doi.org/10.1186/cc11405.
Guilhaumou R, Benaboud S, Bennis Y, Dahyot-Fizelier C, Dailly E, Gandia P, et al. Optimization of the treatment with beta-lactam antibiotics in critically ill patients—guidelines from the French Society of Pharmacology and Therapeutics (Société Française de Pharmacologie et Thérapeutique—SFPT) and the French Society of Anaesthesia and Intensive Care Medicine (Société Française d’Anesthésie et Réanimation—SFAR). Crit Care. 2019;23(1):104. https://doi.org/10.1186/s13054-019-2378-9.
Moriyama B, Henning SA, Neuhauser MM, Danner RL, Walsh TJ. Continuous-infusion β-lactam antibiotics during continuous venovenous hemofiltration for the treatment of resistant gram-negative bacteria. Ann Pharmacother. 2009;43:1324–37. https://doi.org/10.1345/aph.1L638.
Tam VH, Schilling AN, Neshat S, Poole K, Melnick DA, Coyle EA. Optimization of meropenem minimum concentration/MIC ratio to suppress in vitro resistance of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2005;49(12):4920–7. https://doi.org/10.1128/AAC.49.12.4920-4927.2005.
Dulhunty JM, Roberts JA, Davis JS, Webb SAR, Bellomo R, Gomersall C, et al. Continuous infusion of beta-Lactam antibiotics in severe sepsis: a multicenter double-blind, randomized controlled trial. Clin Infect Dis. 2013;56(2):236–44. https://doi.org/10.1093/cid/cis856.
Rafati MR, Rouini MR, Mojtahedzadeh M, Najafi A, Tavakoli H, Gholami K, et al. Clinical efficacy of continuous infusion of piperacillin compared with intermittent dosing in septic critically ill patients. Int J Antimicrob Agents. 2006;28(2):122–7. https://doi.org/10.1016/j.ijantimicag.2006.02.020.
Roberts JA, Kirkpatrick CMJ, Roberts MS, Robertson TA, Dalley AJ, Lipman J. Meropenem dosing in critically ill patients with sepsis and without renal dysfunction: intermittent bolus versus continuous administration? Monte Carlo dosing simulations and subcutaneous tissue distribution. J Antimicrob Chemother. 2009;64(1):142–50. https://doi.org/10.1093/jac/dkp139.
Abdul-Aziz MH, Sulaiman H, Mat-Nor M-B, Rai V, Wong KK, Hasan MS, et al. Beta-Lactam Infusion in Severe Sepsis (BLISS): a prospective, two-centre, open-labelled randomised controlled trial of continuous versus intermittent beta-lactam infusion in critically ill patients with severe sepsis. Intensive Care Med. 2016;42(10):1535–45. https://doi.org/10.1007/s00134-015-4188-0.
Taccone FS, Laupland KB, Montravers P. Continuous infusion of β-lactam antibiotics for all critically ill patients? Intensive Care Med. 2016;42(10):1604–6. https://doi.org/10.1007/s00134-016-4241-7.
European Medicines Agency (EMA). Meropenem Product Information. 2015. https://www.ema.europa.eu/en/medicines/human/referrals/meronem. Accessed 15 May 2015.
European Medicines Agency (EMA). Piperacillin/tazobactam Product Information. 2015. https://www.ema.europa.eu/en/medicines/human/referrals/tazocin. Accessed 15 May 2015.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign. Crit Care Med. 2017;45(3):486–552. https://doi.org/10.1097/CCM.0000000000002255.
IBM Watson Health. IBM Micromedex® web applications access. Greenwood Village, Colorado, USA. 1970. https://www.micromedexsolutions.com. Accessed 1 June 2015.
Rigo-Bonnin R, Ribera A, Arbiol-Roca A, Cobo-Sacristán S, Padullés A, Murillo O, et al. Development and validation of a measurement procedure based on ultra-high performance liquid chromatography-tandem mass spectrometry for simultaneous measurement of β-lactam antibiotic concentration in human plasma. Clin Chim Acta. 2017;468:215–24. https://doi.org/10.1016/j.cca.2017.03.009.
Ulldemolins M, Roberts JA, Rello J, Paterson DL, Lipman J. The effects of hypoalbuminaemia on optimizing antibacterial dosing in critically ill patients. Clin Pharmacokinet. 2011;50(2):99–110. https://doi.org/10.2165/11539220-000000000-00000.
Quinton MC, Bodeau S, Kontar L, Zerbib Y, Maizel J, Slama M, et al. Neurotoxic concentration of piperacillin during continuous infusion in critically ill patients. Antimicrob Agents Chemother. 2017;61(9):e00654-e717. https://doi.org/10.1128/AAC.00654-17.
Imani S, Buscher H, Marriott D, Gentili S, Sandaradura I. Too much of a good thing: a retrospective study of β-lactam concentration-toxicity relationships. J Antimicrob Chemother. 2017;72(10):2891–7. https://doi.org/10.1093/jac/dkx209.
Udy AA, Roberts JA, Boots RJ, Paterson DL, Lipman J. Augmented renal clearance: implications for antibacterial dosing in the critically ill. Clin Pharmacokinet. 2010;49(1):1–16. https://doi.org/10.2165/11318140-000000000-00000.
Dhillon S, Kostrzewski AJ. Basic pharmacokinetics. In: Clinical pharmacokinetics. London: Pharmaceutical Press; 2006. p. 1–44.
European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters, version 11.0, 2020. http://www.eucast.org/clinical_breakpoints. Accessed 24 Dec 2020.
Dhaese SAM, Thooft ADJ, Farkas A, Lipman J, Verstraete AG, Stove V, et al. Early target attainment of continuous infusion piperacillin/tazobactam and meropenem in critically ill patients: a prospective observational study. J Crit Care. 2019;52:75–9. https://doi.org/10.1016/j.jcrc.2019.04.013.
Aardema H, Nannan Panday P, Wessels M, van Hateren K, Dieperink W, Kosterink JGW, et al. Target attainment with continuous dosing of piperacillin/tazobactam in critical illness: a prospective observational study. Int J Antimicrob Agents. 2017;50(1):68–73. https://doi.org/10.1016/j.ijantimicag.2017.02.020.
Richter DC, Frey O, Röhr A, Roberts JA, Köberer A, Funchs T, et al. Therapeutic drug monitoring-guided continuous infusion of piperacillin/tazobactam significantly improves pharmacokinetic target attainment in critically ill patients : a retrospective analysis of four years of clinical experience. Infection. 2019;47:1001–11. https://doi.org/10.1007/s15010-019-01352-z.
Carlier M, Carrette S, Roberts JA, Stove V, Verstraete A, Hoste E, et al. Meropenem and piperacillin/tazobactam prescribing in critically ill patients: does augmented renal clearance affect pharmacokinetic/pharmacodynamic target attainment when extended infusions are used? Crit Care. 2013;17(3):R84. https://doi.org/10.1186/cc12705.
Conil JM, Georges B, Mimoz O, Dieye E, Ruiz S, Cougot P, et al. Influence of renal function on trough serum concentrations of piperacillin in intensive care unit patients. Intensive Care Med. 2006;32(12):2063–6. https://doi.org/10.1007/s00134-006-0421-1.
Udy AA, Varghese JM, Altukroni M, Briscoe S, McWhinney BC, Ungerer J, et al. Subtherapeutic initial b-lactam concentrations in select critically ill patients. Chest. 2012;142(1):30–9. https://doi.org/10.1378/chest.11-1671.
Udy AA, Lipman J, Jarrett P, Klein K, Wallis SC, Patel K, et al. Are standard doses of piperacillin sufficient for critically ill patients with augmented creatinine clearance? Crit Care. 2015;19(1):28. https://doi.org/10.1186/s13054-015-0750-y.
Carrié C, Legeron R, Petit L, Ollivier J, Cottenceau V, d’Houdain N, et al. Higher than standard dosing regimen are needed to achieve optimal antibiotic exposure in critically ill patients with augmented renal clearance receiving piperacillin-tazobactam administered by continuous infusion. J Crit Care. 2018;48:66–71. https://doi.org/10.1016/j.jcrc.2018.08.026.
Alobaid AS, Hites M, Lipman J, Taccone FS, Roberts JA. Effect of obesity on the pharmacokinetics of antimicrobials in critically ill patients: a structured review. Int J Antimicrob Agents. 2016;47(4):256–68. https://doi.org/10.1016/j.ijantimicag.2016.01.009.
Alobaid AS, Wallis SC, Jarrett P, Starr T, Stuart J, Lassig-Smith M, et al. Effect of obesity on the population pharmacokinetics of meropenem in critically ill patients. Antimicrob Agents Chemother. 2016;60(8):4577–84. https://doi.org/10.1128/AAC.00531-16.
Hites M, Taccone FS, Wolff F, Cotton F, Beumier M, De Bacher D, et al. Case-control study of drug monitoring of β-lactams in obese critically ill patients. Antimicrob Agents Chemother. 2013;57(2):708–15. https://doi.org/10.1128/AAC.01083-12.
Cheatham SC, Fleming MR, Healy DP, Chung EK, Shea KM, Humphrey ML, et al. Steady-state pharmacokinetics and pharmacodynamics of meropenem in morbidly obese patients hospitalized in an intensive care unit. J Clin Pharmacol. 2014;54(3):324–30. https://doi.org/10.1002/jcph.196.
Adnan S, Li JX, Wallis SC, Rudd M, Jarrett P, Paterson DL, et al. Pharmacokinetics of meropenem and piperacillin in critically ill patients with indwelling surgical drains. Int J Antimicrob Agents. 2013;42(1):90–3. https://doi.org/10.1016/j.ijantimicag.2013.02.023.
Fujii M, Karumai T, Yamamoto R, Kobayashi E, Ogawa K, Tounai M, et al. Pharmacokinetic and pharmacodynamic considerations in antimicrobial therapy for sepsis. Expert Opin Drug Metab Toxicol. 2020;16(5):415–30. https://doi.org/10.1080/17425255.2020.1750597.
Roberts JA, Lipman J. Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med. 2009;37(3):840–51. https://doi.org/10.1097/CCM.0b013e3181961bff.
Blot SI, Pea F, Lipman J. The effect of pathophysiology on pharmacokinetics in the critically ill patient: concepts appraised by the example of antimicrobial agents. Adv Drug Deliv Rev. 2014;77:3–11. https://doi.org/10.1016/j.addr.2014.07.006.
May CC, Arora S, Parli SE, Frase JF, Thompson M, Cook AM. Augmented renal clearance in patients with subarachnoid hemorrhage. Neurocrit Care. 2015;23(3):374–9. https://doi.org/10.1007/s12028-015-0127-8.
Udy AA, Jarrett P, Lassig-Smith M, Stuart J, Starr T, Dunlop R, et al. Augmented renal clearance in traumatic brain injury: a single-center observational study of atrial natriuretic peptide, cardiac output, and creatinine clearance. J Neurotrauma. 2017;34(1):137–44. https://doi.org/10.1089/neu.2015.4328.
Damen C, Dhaese S, Verstraete AG, Stove V, De Waele JJ. Subtherapeutic piperacillin concentrations in neurocritical patients. J Crit Care. 2019;54:48–51. https://doi.org/10.1016/j.jcrc.2019.07.007.
Ullah S, Beer R, Fuhr U, Taubert M, Zeitlinger M, Kratzer A, et al. Brain exposure to piperacillin in acute hemorrhagic stroke patients assessed by cerebral microdialysis and population pharmacokinetics. Neurocrit Care. 2020;33(3):740–8. https://doi.org/10.1007/s12028-020-00947-x.
Triginer C, Izquierdo I, Fernández R, Torrent J, Benito S, Net A, et al. Changes in gentamicin pharmacokinetic profiles induced by mechanical ventilation. Eur J Clin Pharmacol. 1991;40(3):297–302. https://doi.org/10.1007/BF00315213.
Cawley MJ. Mechanical ventilation: a tutorial for pharmacists. Pharmacotherapy. 2007;27(2):250–66. https://doi.org/10.1592/phco.27.2.250.
Van der Merwe FV, Wallis S, Udy A. Understanding the impact of critical illness on drug pharmacokinetics: scientifically robust study design. J Clin Toxicol. 2011;S4:002. https://doi.org/10.4172/2161-0495.S4-002.
Georges B, Conil JM, Seguin T, Ruiz S, Minville V, Cougot P, Decun JF, et al. Population pharmacokinetics of ceftazidime in intensive care unit patients: Influence of glomerular filtration rate, mechanical ventilation, and reason for admission. Antimicrob Agents Chemother. 2009;53(10):4483–9. https://doi.org/10.1128/AAC.00430-09.
Acknowledgements
We thank the joint dedication of staff members of the departments of intensive care, infectious disease, microbiology, biochemistry and nursing staff of the Hospital Universitari de Bellvitge. Without the teamwork, it would not have been possible to carry out this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Part of this study has been financed thanks to the aid for research projects granted to us by the Sociedad Española de Farmacia Hospitalaria (Convocatoria de Ayudas a Proyectos de Investigación de la SEFH 2013/2014. EPA056/14 ATB-2014-01).
Conflict of Interest
The authors declare that they have no competing interests.
Ethical Approval
The study was approved by the local Ethics Committee (SFB-ATB-2014-01) and conducted following the Declaration of Helsinki.
Consent to Participate
Written informed consent was requested from the patient or the closest relative before inclusion.
Consent for Publication
Not applicable.
Availability of Data and Materials
Main data will be made available on request to the corresponding author.
Code Availability
Not applicable.
Author Contributions
Conception and design: EEP, VGS, SCS, ESP, KMS, JSR, XPF, RRB, FTQ, HCC, APZ. Data collection: EEP, VGS, KMS. Analysis and interpretation: EEP, HCC, APZ. Drafting the manuscript for important intellectual content: EEP, HCC, APZ. Revision and final approval: EEP, VGS, SCS, ESP, KMS, JSR, XPF, RRB, FTQ, JC, HCC, APZ.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Esteve-Pitarch, E., Gumucio-Sanguino, V.D., Cobo-Sacristán, S. et al. Continuous Infusion of Piperacillin/Tazobactam and Meropenem in ICU Patients Without Renal Dysfunction: Are Patients at Risk of Underexposure?. Eur J Drug Metab Pharmacokinet 46, 527–538 (2021). https://doi.org/10.1007/s13318-021-00694-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-021-00694-0