Abstract
Background and Objectives
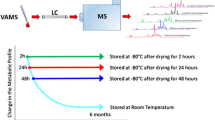
Volumetric absorptive microsampling (VAMS) devices are useful for sampling a smaller volume of blood from rodents in the preclinical setting. In the present study, we evaluated the proof of concept of a VAMS device by comparing the pharmacokinetic data of tacrolimus in rats among dried blood in VAMS, wet blood, and plasma.
Methods
Tacrolimus was administered orally, to rats, at a dose of 10 mg/kg. Only 10 μL aliquots of blood were absorbed by VAMS devices at designated time points. Tacrolimus was extracted with a methanol–water mixture (1:1, v/v) via sonication. Tacrolimus levels in wet blood (10 μL) and plasma (10 μL) were quantified after protein precipitation.
Results
Tacrolimus in VAMS devices was quantifiable from 0.2 ng/mL using high-performance liquid chromatography with tandem mass spectrometer. Accuracy and precision were within the acceptance criteria. Bland–Altman plots showed that tacrolimus concentrations in VAMS devices were similar to those in wet blood, regardless of tacrolimus levels. On the other hand, tacrolimus levels in plasma were different from those in VAMS devices, especially at lower concentrations, likely due to partition of tacrolimus to blood cells. However, pharmacokinetic parameters were comparable among the three matrices.
Conclusions
Collectively, these findings suggest that the VAMS device can be a useful device for pharmacokinetic studies in rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A volumetric absorptive microsampling (VAMS) device was evaluated in rat pharmacokinetic study using tacrolimus and tacrolimus concentrations in dried blood on VAMS devices, wet blood, and plasma were compared. |
Tacrolimus levels in VAMS devices were comparable to those in wet blood, while they were different from those in plasma at lower concentrations in particular due to concentration-dependent blood-to-plasma partition. |
Findings in this study suggest that the VAMS device can be a useful device for pharmacokinetic studies in rats. |
1 Introduction
Microsampling is an attractive sample collection method in both preclinical and clinical settings and has recently been widely applied in pharmacokinetic evaluations. In preclinical situations, microsampling can reduce the number of animals tested by employing serial blood sampling using one animal [1]. This also helps to reduce inter-individual differences in pharmacokinetics. Various types of microsampling devices including capillary tubes, dried blood spots (DBS), and plasma extraction cards have been developed, and their applications for bioanalytical purposes have been reported [2, 3]. Blood-based microsampling is attractive, since it requires a small volume of blood collected from rodents; whereas, plasma-based microsampling, requires a greater volume of blood to achieve a similar sensitivity to that in the blood-based assay regardless of blood-to-plasma partition of drugs (e.g., approximately 50 μL blood is required to develop the plasma-based assay using 20 μL plasma, while only 20 μL blood is required for the blood-based assay to achieve similar sensitivity). There are two major methods for blood-based microsampling, namely DBS and volumetric absorptive microsampling (VAMS). In DBS, the impact of hematocrit (Hct) levels on the assay data can be significant [4]. It may not be a better option in the clinical setting where there are large inter-individual differences in Hct levels. Even in preclinical settings, Hct levels can be variable depending on the condition of animals following dosing of investigational drugs [5]. A VAMS device developed by Neoteryx has overcome the Hct-dependent sampling volume [6], and is thus considered one of the most promising blood-based microsampling devices for overcoming the Hct issue. Previous studies, using E6005 [7] and tacrolimus [8] as model drugs of low and high blood cell partition, respectively, demonstrated that optimization of the extraction procedure, to yield Hct-independent extraction recovery, enabled an accurate sample assay regardless of Hct levels. Application of VAMS, reported for other drugs, further supports application of VAMS to drugs with diverse physicochemical properties [9,10,11,12,13,14,15,16,17]. However, application to pharmacokinetic studies has been limited.
In the present pharmacokinetic study in rats, tacrolimus was used as a model drug to apply the VAMS device to ensure its proof of concept. Tacrolimus was used to represent typical drug candidates in drug discovery and development. In addition, extraction of tacrolimus from VAMS devices was optimized in the previous study [8] and there are many articles reporting tacrolimus results from pharmacokinetic studies in rats [18,19,20,21,22,23]. Although a reproducible assay method of tacrolimus in dried human blood on VAMS devices was developed [8], a more sensitive bioanalytical method for the determination of tacrolimus concentrations in dried rat blood on VAMS devices, with a fivefold lower limit of quantification [lower limit of quantification (LLOQ); 0.2 ng/mL] using only 10 μL blood samples, has been established in this study. The developed analytical method has been qualified to confirm that the developed method is reproducible by assessing the following validation parameters in VAMS devices: linearity, selectivity, accuracy and precision in intra-batch assay, processed sample stability, frozen stability, and bench-top stability. As a previous report suggested that tacrolimus in VAMS devices appeared to be unstable during storage at ambient temperature, possibly due to deteriorated recovery of tacrolimus from the device, we assessed stability in dried rat blood on VAMS devices at − 25 °C, 4 °C, and ambient temperature. In addition to the stability assessment in VAMS devices, we assessed tacrolimus stability in the wet blood and plasma of rats. Tacrolimus assays were also qualified in wet blood and plasma to determine tacrolimus concentrations in these matrices in rats.
2 Methods
2.1 Materials
Tacrolimus (chemical purity: 97.8%) and ascomycin (internal standard, IS) were purchased from Sigma-Aldrich (St Louis, MO, USA) and Focus Biomolecules (Plymouth Meeting, PA, USA), respectively. VAMS devices (10 μL) were purchased from Neoteryx, LLC. (Torrance, CA, USA). Drug-free blank rat blood with heparin sodium as an anticoagulant was collected from three male Sprague–Dawley rats (8-week-old). Heparin sodium was purchased from Mochida Pharmaceutical Co., Ltd (Tokyo, Japan).
2.2 Preparation of Calibration and Quality Control Samples
Stock solutions of tacrolimus in methanol (1000 μg/mL) and IS in acetonitrile (1000 μg/mL) were prepared and then serially diluted to prepare working standard solutions. The stock and working solutions were stored below – 15 °C. In VAMS devices and wet blood assay, calibration samples at 0.2, 0.6, 2, 6, 20, 60, 200, and 250 ng/mL and quality control (QC) samples at 0.2 ng/mL (LLOQ), 0.6 ng/mL (low QC, LQC), 6 ng/mL (mid QC, MQC), and 200 ng/mL (high QC, HQC) were prepared. In plasma assay, calibration samples of 0.1, 0.3, 1, 3, 10, 30, 80, and 100 ng/mL and QC samples of 0.1, 0.3, 3, and 80 ng/mL were prepared.
2.3 Preparation and Extraction of Tacrolimus
2.3.1 VAMS Devices
Blood calibration and QC samples were absorbed by VAMS devices 1 h after fortifying whole blood with tacrolimus. The tip of the device was held in blood samples until it turned red, waiting an additional 2 s before the tip was removed from the blood. The tip was dried at ambient temperature for 2 h and then put into a tube for frozen storage until extraction. The extraction of tacrolimus was performed by adding methanol/water (1:1, v/v, 100 μL; hereafter represented as 50% methanol) followed by sonication for 15 min and vortexing for 10 s as optimized in the previous study [8]. The IS working solution (50 ng/mL, 10 μL) was fortified to the tube, and then centrifuged (15,700×g, 15 min, 4 °C) to obtain supernatant. A 10 μL aliquot was injected to liquid chromatography with tandem mass spectrometer (LC–MS/MS).
2.3.2 Wet Blood
To whole blood samples (10 μL), the IS working solution (50 ng/mL, 10 μL), and 10 μL of calibration standard or methanol was added followed by addition of 2 M zinc sulfate/water/methanol (100 μL, 5:25:70, v/v/v). Samples were then centrifuged (15,700×g, 5 min, 4 °C) for extraction of tacrolimus and IS from whole blood. A 10 μL aliquot of the supernatant was injected into the LC–MS/MS system.
2.3.3 Plasma
The IS working solution (50 ng/mL, 10 μL), 10 μL of calibration standard or methanol, and 50 μL of acetonitrile/methanol (1:1, v/v) were mixed with 10 μL of plasma samples and then centrifuged (15,700×g, 5 min, 4 °C) to obtain the supernatant. A 10 μL aliquot of supernatant was injected into the LC–MS/MS system.
2.4 Chromatographic and Mass Spectrometric Conditions
The assay conditions of tacrolimus were consistent among the three matrices (VAMS devices, wet blood, and plasma). A Nexcera X2 high-performance liquid chromatography system (Shimadzu, Kyoto, Japan) coupled with tandem mass spectrometer, API6500 (Sciex, Redwood City, MA, USA) was used for separation and detection. Although a robust and simple analytical method of tacrolimus has been established in human dried blood on VAMS devices [8], the method has been modified to achieve more sensitivity. The mobile phase consisting of (A) 50 mM ammonium acetate/water (5:95, v/v) and (B) 50 mM ammonium acetate/methanol (5:95, v/v) was used with gradient elution. The mobile phase B (%) was 5% at time = 0 and maintained for 0.2 min. Then, B (%) was increased to 99% at 0.21 min and was kept to 2.50 min. The B (%) was decreased to 5% at 2.51 min and equilibrated to 4.50 min for the next injection. The flow rate of the mobile phase was 0.35 mL/min and the total run time per assay was 4.5 min. Chromatographic analysis was performed on an ACQUITY UPLC HSS T3 column (2.1 × 100 mm, 1.8 µm, Waters, Milford, MA, USA) maintained at 40 °C.
Quantification was achieved with triple quadrupole mass spectrometer in the positive ion electrospray mode. Multiple reaction monitoring of the mass transition pairs, m/z 821 → 769 and m/z 809 → 757, as precursor ion and product ion, for tacrolimus and the IS, respectively, was employed. The collision energy and cone voltage were 27 eV and 40 V, respectively, for both tacrolimus and IS. Ammonium adduct precursor ions were selected for both tacrolimus and the IS due to higher signal compared to protonated ion [24]. In addition, interference in chromatograms did not enable us to select the sodium adduct ion despite comparable signal to the ammonium adduct ion.
2.5 Bioanalytical Method Qualification
To validate the developed method for the determination of tacrolimus concentrations in three matrices (VAMS devices, wet blood, and plasma), linearity, selectivity, intra-batch reproducibility, and stability were evaluated according to bioanalytical guidelines from European Medicines Agency [25] and US Food and Drug Administration [26]. Although matrix effects and extraction recovery are important validation parameters to qualify the assay method in dried blood on VAMS devices, these were not assessed in this study. It is because those parameters were evaluated using human dried blood on VAMS devices with the same extraction procedure in the previous report [8] and comparable data are expected. In the linearity assessment, the peak area ratios of tacrolimus to the IS were plotted against the corresponding nominal concentrations. The calibration curve was constructed by the least square method with 1/(concentration)2 as the weighting factor. Accuracy of each calibration sample was determined to ensure that % inaccuracy at each concentration was within ± 15% (± 20% was allowed at the LLOQ). For selectivity assessment, areas of peaks eluted at the retention times of tacrolimus and the IS should be within 20 and 5% of those of the LLOQ for tacrolimus and the IS, respectively.
Intra-batch accuracy and precision were evaluated using QC samples at four concentrations (LLOQ, LQC, MQC, and HQC) prepared from pooled matrices. Five replicates per concentration were assayed to calculate % inaccuracy and imprecision as % RSD (relative standard deviation) with the exception of the LLOQ samples of VAMS devices due to broken tubes during sonication in sample processing (three replicates at the LLOQ). The acceptance criteria for % inaccuracy and % RSD in intra-batch tests were ± 15 and 15%, respectively (± 20 and 20% at the LLOQ, respectively). As a bioanalytical method for the determination of tacrolimus was validated in human dried blood on VAMS devices [8] and method validation is a partial scope of this study, quantification of tacrolimus was partially validated in rat dried blood on VAMS devices. Thus, inter-batch accuracy and precision were not evaluated in this study. Although anticoagulants used in human and rat dried blood on VAMS devices were different (EDTA in human while heparin in rat), impacts on the assay results are considered minimal [27].
Stability of tacrolimus in VAMS devices, wet blood, and plasma as well as in processed samples was assessed at low and high QC concentrations. Tacrolimus concentrations after storage were compared to initial concentrations and % of initial was calculated. The percentage of initial equal to or more than 85% was considered stable. In the stability assessment in VAMS devices, bench-top stability at ambient temperature was tested for 3 and 24 days, while frozen stability at – 25 °C was evaluated up to 24 days. Stability of tacrolimus in wet blood and plasma was also assessed. Bench-top stability of tacrolimus was evaluated up to 4 h (wet blood) and 5 h (plasma); and, refrigerated stability was evaluated at 4°C in wet blood for 2 days while frozen stability in plasma was evaluated at − 25 °C for 3 days. Stability in processed samples was assessed at 4 °C for 2 days (wet blood) or 3 days (VAMS devices and plasma). Tacrolimus levels in stored processed samples were compared to those in the initial injection and % of initial was calculated.
2.6 Application to a Pharmacokinetic Study in Rats
Sprague–Dawley rats, 6 weeks of age, were purchased from Charles River Laboratories (Kanagawa, Japan) and were acclimatized for 2 weeks prior to the pharmacokinetic study. The body weight on the day of tacrolimus administration ranged from 253 to 273 g in male and from 166 to 177 g in female. Tacrolimus was dissolved in ethanol at 10 mg/mL and then diluted with water to make a 1 mg/mL dosing solution. Tacrolimus was orally administered to three male and three female rats at a dose of 10 mg/kg. At 0.5, 1, 2, 4, 8, and 24 h post-dose, blood samples (approximately 0.15 mL) were drawn from the cervical vein via a heparin-treated syringe with 25G needle and collected in a tube. In the sampling by VAMS devices, blood in a tube was absorbed by VAMS devices until the color of its tip turned red and then the tip was held for an additional two seconds before removal. Subsequently, the VAMS device was put on a bench at ambient temperature for 2 h and then stored below − 15 °C until assay. For the plasma assay, aliquots (50 μL) of blood samples were centrifuged (13,200×g, 4 min, 4 °C) and then plasma samples were prepared and stored below − 15 °C until sample extraction for the assay. For the wet blood assay, 30 μL aliquots were collected and 10 μL aliquots were subjected to extraction described above. In the assay of in-study samples, QC samples at three concentrations were assayed to ensure the validity of the assay. An additional 30 μL blood samples were used for determination of Hct levels at every sampling time by a hematology analyzer, XN-2000V (Sysmex, Hyogo, Japan). Pharmacokinetic parameters of tacrolimus were estimated by non-compartmental analysis using Phoenix WinNonlin® version 6.4 (Certara, Princeton, NJ, USA), and the mean and the standard deviation in three males and three females were calculated. The maximum plasma concentration (Cmax) and time to reach Cmax (Tmax) were observed values. The terminal elimination rate constant (kel) was determined from the last three sampling points (from 4 to 24 h) by the least squares regression analysis of the terminal log-linear portion of the plasma concentration–time profile. The elimination half-life (T1/2) was calculated to be 0.693/kel. The area under plasma concentration–time profile (AUC) was determined by the trapezoidal rule up to the last time points (AUC0–24h). The AUC from time zero to infinity (AUC0-inf) was calculated by the sum of AUC0-24h and C24h/kel. The total clearance (CLtot/F) and the volume of distribution at the steady-state (Vdss/F) after oral administration were calculated from dividing dose by AUC0-inf and CLtot/F × mean residence time, respectively. To compare tacrolimus concentrations among the three matrices (VAMS devices, wet blood, and plasma), Bland–Altman analysis was performed using Graph Pad Prism (La Jolla, CA, USA) by plotting % bias in concentrations and average concentrations. % bias in concentrations between VAMS devices and the other matrices was calculated using the following equation:
where average concentration represents the mean of VAMS devices and the other matrix.
2.7 Blood-to-Plasma Ratio
The in vitro blood-to-plasma concentration ratio of tacrolimus was evaluated. Tacrolimus at 2, 6, 20, 60, 200, 600, and 1000 ng/mL spiked in rat blood was put on a bench at ambient temperature for an hour (triplicates per concentration). Blood samples were centrifuged (15,700×g, 5 min, 4 °C) to obtain plasma samples for the assay of tacrolimus in plasma by LC–MS/MS. Plasma samples were pretreated by the method mentioned above. The blood-to-plasma ratio of tacrolimus was calculated by dividing nominal tacrolimus concentrations in blood by determined tacrolimus concentrations in plasma.
3 Results
3.1 Bioanalytical Method Qualification
3.1.1 VAMS Devices
The developed bioanalytical method for the quantitation of tacrolimus in VAMS devices was qualified by assessing the following parameters: linearity, selectivity, accuracy/precision in intra-assay reproducibility, and stability. Calibration curves of tacrolimus were linear ranging from 0.2 to 250 ng/mL with a correlation coefficient > 0.99. Back-calculated calibration standard concentrations across four batches had average % inaccuracy of ± 6.2% or less and % RSD of 10.0% or less at all the concentrations (Table 1). Typical chromatograms of tacrolimus and the IS are shown in Fig. 1. Although no significant interfering peaks were observed at the retention times of tacrolimus and the IS (2.0 min) in blank samples, areas of interfering peaks in blank from six individual rats were 12.4–29.7% of those of the LLOQ samples. The intra-batch assay reproducibility was assessed by inaccuracy and imprecision using QC samples at the four concentrations (Table 2). The % inaccuracy and % imprecision were within ± 14.2 and 15.6%, respectively, which were within the acceptance criteria [% inaccuracy ≤ ± 15.0%, % RSD ≤ 15%, (for LLOQ: % inaccuracy ≤ ± 20.0%, % RSD ≤ 20%)]. Processed sample stability for 3 days, bench-top stability at ambient temperature for 3 and 24 days and frozen stability at – 25 °C up to 24 days were assessed. The % of initial concentration was within the acceptance criteria (85% or more) except for bench-top storage for 24 days, suggesting that tacrolimus in VAMS devices is stable under those conditions (Table 3).
Representative chromatograms of tacrolimus and the IS in VAMS extracts, wet blood, and plasma. a Blank rat blood in VAMS extracts, b tacrolimus at the low-quality control level (LQC; 0.6 ng/mL) and the IS in VAMS extracts, c blank in rat wet blood, d tacrolimus at the LQC (0.6 ng/mL) and the IS in rat wet blood, e blank rat plasma, f tacrolimus at the LQC (0.3 ng/mL) and the IS in rat plasma. Upper and lower figures show the mass transition of m/z 821 → 769 (tacrolimus) and m/z 809 → 757 (IS), respectively. IS internal standard, LQC low-quality control, VAMS volumetric absorptive microsampling
3.1.2 Wet Blood and Plasma
Tacrolimus was quantified in wet blood at the same quantification range as VAMS devices (0.2–250 ng/mL). In plasma, calibration samples showed acceptable inaccuracy from the LLOQ (0.1 ng/mL) to the upper limit of quantification (100 ng/mL). Inaccuracy and imprecision of calibration samples and typical chromatograms are represented in Table 1 and Fig. 1, respectively. The % inaccuracy and % RSD were within ± 15 and 15%, respectively, in intra-batch reproducibility evaluation (Table 2). The % inaccuracy and % RSD at 0.1 ng/mL in plasma were out of range of the acceptance criteria (> ± 20%). Processed sample stability at 4 °C was ensured up to 2 and 3 days in wet blood and plasma, respectively. Bench-top stability of tacrolimus in wet blood and plasma at ambient temperature was ensured up to 4 and 5 h, respectively. Tacrolimus was stable for at least 3 and 2 days in plasma at – 25 °C and in wet blood at 4 C, respectively. Although % of initial concentration of plasma samples at LQC stored at – 25 °C for 25 days was slightly deviated (117.3%) from the acceptance criteria, possibly due to some fluctuation in the process of extraction of the analyte and/or the analysis by LC–MS/MS, it is highly likely that tacrolimus is stable under this condition since stability in rat blood was ensured for 72 days at – 20 °C [28].
3.2 Pharmacokinetic Study
Figure 2 shows pharmacokinetic profiles of tacrolimus using samples of a VAMS device, wet blood, and plasma. Pharmacokinetic parameters in each matrix are listed in Table 4. Tacrolimus was absorbed rapidly after oral administration and reached maximum levels in systemic circulation at the first sampling time point (0.5 h) and was quantifiable up to the last sampling time point (24 h) in all six rats tested. In VAMS devices, Cmax values were 343 ± 86 and 523 ± 85 ng/mL in male and female rats, respectively, and AUC0–24 h values were 888 ± 349 and 1913 ± 482 ng × h/mL in male and female rats, respectively. The T1/2 was 5.1 ± 0.5 and 4.6 ± 0.6 h in male and female, respectively. The CLtot/F and Vdss/F were 12,034 ± 3937 mL/h/kg and 90.7 ± 34.8 L/kg, respectively, in male, and 5390 ± 1548 mL/h/kg and 36.4 ± 15.0 L/kg, respectively, in female. Similar parameters were obtained in wet blood and plasma as well.
Tacrolimus concentration–time profiles in dried blood on VAMS devices, wet blood, and plasma after a single oral administration of tacrolimus (10 mg/kg) to male (a) and female (b) rats. Tacrolimus (10 mg/kg) was orally administered to Sprague–Dawley male and female rats (n = 3 each) and blood samples were obtained at 0.5, 1, 2, 4, 8, and 24 h post-dose. Tacrolimus concentrations in VAMS (closed circle), wet blood (open circle), and plasma (open triangle) were determined by the qualified LC–MS/MS methods. Data represent the mean ± standard deviation of three rats in each gender. LC–MS/MS liquid chromatography tandem mass spectrometry, VAMS volumetric absorptive microsampling
Tacrolimus levels in wet blood correlated very well with those in VAMS devices, although some samples at higher tacrolimus concentrations showed relatively higher positive bias (Fig. 3a). On the other hand, at lower concentrations (e.g., < 20 ng/mL), tacrolimus concentrations in plasma were different from those in blood-based concentrations (wet blood and VAMS devices), possibly due to partition of tacrolimus into blood cells (Fig. 3b). However, at relatively higher concentrations (e.g, > 100 ng/mL), plasma concentrations were close to blood-based concentrations since the blood-to-plasma concentration ratio in vitro was approximately 0.9 (Fig. 4).
Bland–Altman plots for comparing tacrolimus concentrations between VAMS devices and wet blood (a) and between VAMS devices and plasma (b). Average concentrations of tacrolimus in VAMS devices and wet blood (a) or plasma (b) and % bias between the two matrices were plotted on x- and y-axis, respectively. The % bias was calculated from (VAMS device concentrations—wet blood or plasma concentrations) × 100/average concentrations of VAMS device and the other matrix. VAMS volumetric absorptive microsampling
Relationship between blood concentrations and blood-to-plasma ratio of tacrolimus in rats in vitro. Rat whole blood fortified by tacrolimus (2–1000 ng/mL) was put on a bench for 1 h and then centrifuged to obtain plasma for assay of tacrolimus. Blood-to-plasma ratio was calculated by dividing nominal blood concentrations by the determined corresponding plasma concentrations. Data represent the mean ± standard deviation of three replicates
In this study, impacts of relatively large volume serial blood sampling on Hct levels were also evaluated. The Hct levels ranged from 39.4 to 49.1% at 0.5 h post-dose in six animals. The Hct levels were relatively consistent up to 8 h post-dose in each animal, but decreased by 4.5–57.6% at 24 h compared to the values at 8 h possibly due to excessive volume of collected blood. However, impacts on the assay were considered limited given minimal Hct impacts on the determination of tacrolimus in this assay [8]. QC samples assayed along with in-study samples were within the acceptance criteria for all the matrices, ensuring that the assay of in-study samples was valid.
3.3 Blood-to-Plasma Ratio
Blood-to-plasma ratio of tacrolimus was evaluated from 2 to 1000 ng/mL in blood (three replicates per concentration). Plasma concentrations of tacrolimus were 0.38 ± 0.02, 1.25 ± 0.02, 5.24 ± 0.21, 42.5 ± 0.64, 213.0 ± 2.0, 667.7 ± 13.0, and 1076.7 ± 73.7 ng/mL when nominal blood levels were 2, 6, 20, 60, 200, 600, and 1000 ng/mL, respectively. The calculated blood-to-plasma ratios of tacrolimus were 5.22 ± 0.23, 4.80 ± 0.07, 3.82 ± 0.15, 1.41 ± 0.02, 0.94 ± 0.01, 0.90 ± 0.02, and 0.93 ± 0.06 at 2, 6, 20, 60, 200, 600, and 1000 ng/mL of tacrolimus in blood, respectively, confirming concentration-dependent partition into blood cells (Fig. 4).
4 Discussion
In the method validation study, ascomycin was used as the IS. The use of structural analogue of the analyte as the IS is justified from acceptable validation parameters assessed in this study, although stable isotope labels are gold standard as the IS in assay methods using LC–MS/MS. Although the method validation parameters including accuracy, precision, selectivity, and stability were within the acceptance criteria recommended by bioanalytical guidelines [25, 26], accuracy and precision at the LLOQ did not meet the criteria. However, impacts of failed inaccuracy and imprecision at 0.1 ng/mL in plasma on pharmacokinetic evaluation were negligible since tacrolimus concentrations in plasma was 1.07 ng/mL or above for all the samples, where inaccuracy and imprecision at the QC samples other than 0.1 ng/mL were well within the acceptance criteria. The signal-to-noise ratio of tacrolimus at 0.2 ng/mL may not be sufficient; however, there were no impacts on sample assay of VAMS samples since tacrolimus levels in VAMS devices were 2.04 ng/mL or more, which was tenfold higher than the LLOQ. The acceptable signal-to-noise ratio (S/N) was 2 for the determination of LLOQ in this study. The S/N in this study was 2, 3, and 2, in VAMS, wet blood, and plasma, respectively. The bioanalytical guidelines form US Food and Drug Administration and European Medicines Agency recommended that the S/N should be at least 5 [25, 26]. It is thus suggested that the S/N in this study may not be enough from the regulatory bioanalysis point of view. However, the established method is sufficiently qualified for the purpose of comparing pharmacokinetic data of tacrolimus among the three matrices. In the stability assessment, although freeze–thaw stability has not been assessed in this study, it is likely that it may not give adverse impacts on the integrity of pharmacokinetic data in rats in this study. VAMS devices obtained from a rat pharmacokinetic study were subjected to the assay just after one freeze–thaw cycle. Given that tacrolimus in VAMS devices is stable for at least 3 days at room temperature and for at least 24 days at – 25 °C, it is likely that tacrolimus in VAMS devices is also stable just after one freeze–thaw cycle. In the bench-top stability assessment, tacrolimus in VAMS devices was below 85% of initial only at high concentration after 24 days at room temperature. This “apparent instability” is similar to the finding in our previous study using tacrolimus in human dried blood on VAMS devices. % of initial of tacrolimus was below 85% on days 3 and the apparent instability was more profound at higher concentrations [8]. Reasons to explain this finding remain to be clarified, but apparent instability was reported in the other study [17].
A pharmacokinetic study of tacrolimus was performed in male and female rats by oral administration at 10 mg/kg and tacrolimus concentrations in VAMS devices, wet blood, and plasma were determined using the qualified assay method. Tacrolimus concentrations in female rats were higher than those in male rats. The main clearance pathway of tacrolimus in rats was reported to be via metabolism, since less than 0.4% of dosed activity was excreted as unchanged drug in the excreta in rats [18]. As the unbound fraction of tacrolimus in rat plasma was 0.0131 at 2 mg/mL [21], slight differences in plasma protein binding of tacrolimus between genders lead to differences in pharmacokinetic parameters such as total clearance or volume of distribution. It is possible that the gender differences are attributable to the differences in plasma protein binding and/or metabolic clearance, but further studies are required to clarify the reasons. Pharmacokinetic parameters of tacrolimus in the present study were compared to those in the previous papers. Systemic exposure obtained in this study was slightly higher than the previous paper [18] in which Tmax, Cmax, and AUC0–24 h in blood were 0.5 h, 170 ng/mL, and 776 ng × h/mL, respectively, after oral administration of tacrolimus at a dose of 10 mg/kg to fasted male rats. Although reasons for higher exposure in this study require further evaluation, differences in the assay formats (enzyme immunoassay vs LC–MS/MS) or dosing vehicles which impact the solubility of tacrolimus may contribute to the differences in systemic exposure between the two studies.
Relatively higher concentrations in VAMS devices compared to wet blood were also reported [10, 11, 16]. Concentrations of caffeine and paraxanthine in VAMS devices were higher than those in wet blood and almost all VAMS samples showed positive bias with a maximum bias of approximately 30% [11]. The Cmax of paracetamol in VAMS devices was up to 40% higher than that in wet blood [10]. Although reasons for explaining this bias require further studies, slight differences in extraction recovery between calibration samples and study samples due to potential differences in Hct might be one of contributing factors as suggested [11]. To clarify factors contributing to the differences, further comparison studies between VAMS devices and wet blood are required to see if this bias is consistent among drugs with diverse physiochemical properties.
When pharmacokinetic parameters are compared across studies, differences in blood sampling sites should be also taken into consideration. In this study, blood samples were obtained from cervical vein, while it was drawn from tail vein in the other study using VAMS [17]. Korfmacher et al. compared blood concentrations of five compounds including three proprietary and two non-proprietary compounds (fluoxetine and glipizide) when blood samples were collected from jugular vein and tail vein [29]. Although blood concentration–time profile of glipizide was not statistically different, that of fluoxetine was different between two blood collection sites. The present study has not yet investigated impacts of blood collection sites on tacrolimus blood concentrations, however, it is not an issue as long as blood samples are collected from a consistent site across studies. The findings suggest that pharmacokinetic parameters are different by blood collection site depending on characteristics of drugs and it is important that the site should be consistent across studies.
To explain the differences in tacrolimus levels between blood and plasma, blood-to-plasma ratio was investigated in vitro. Tacrolimus was fortified in whole blood and put on bench for 1 h for equilibrium. It is considered that 1 h incubation is sufficient to determine blood-to-plasma ratio in vitro. In our previous study for determining in vitro blood-to-plasma ratio of tacrolimus in human blood, the time course of blood-to-plasma ratio demonstrated that 1 h incubation was sufficient to reach equilibrium. Given that blood-to-plasma partition in human blood was much higher than that in rat blood, 1 h incubation in rat blood in this study was sufficient. The blood-to-plasma ratio at 2 ng/mL in rats (5.22) was lower than that in humans at 100 ng/mL (51.1, [8]). The calculated blood-to-plasma ratios from the previous report, based on the assumption of a Hct value of 45%, were 3.7, 1.5, and 0.7, respectively, at 5, 50 and 500 ng/mL tacrolimus in the in vitro rat blood [18], which were similar to the values in the present study.
5 Conclusion
The VAMS was applied to a pharmacokinetic study of tacrolimus in rats to demonstrate its proof of concept. The requirement of only 10 μL whole blood per time point enabled the serial collection of whole blood samples to be taken from a single rat, which led to reducing the number of rats used in the study. Tacrolimus concentrations in VAMS devices were comparable to those in wet blood but were different from those in plasma especially at lower concentrations due to high partition of tacrolimus to blood cells. Although more research is needed to see if the VAMS strategy is a viable option as a sole method for PK studies in animals, VAMS is a useful tool for studying tacrolimus PK in rats and can be also useful for other drugs.
References
Chapman K, Chivers S, Gliddon D, Mitchell D, Robinson S, Sangster T, Sparrow S, Spooner N, Wilson A. Overcoming the barriers to the uptake of nonclinical microsampling in regulatory safety studies. Drug Discov Today. 2014;19:528–32.
Kim JH, Woenker T, Adamec J, Regnier FE. Simple, miniaturized blood plasma extraction method. Anal Chem. 2013;85:11501–8.
Ryona I, Henion J. A book-type dried plasma spot card for automated flow-through elution coupled with online SPE-LC-MS/MS bioanalysis of opioids and stimulants in blood. Anal Chem. 2016;88:11229–37.
O’Broin SD, Kelleher BP, Gunter E. Evaluation of factors influencing precision in the analysis of samples taken from blood spots on filter paper. Clin Lab Haematol. 1995;17:185–8.
Roy S, Khanna V, Mittra S, Dhar A, Singh S, Mahajan DC, Priyadarsiny P, Davis JA, Sattigeri J, Saini KS, Bansal VS. Combination of dipeptidylpeptidase IV inhibitor and low dose thiazolidinedione: preclinical efficacy and safety in db/db mice. Life Sci. 2007;81:72–9.
Spooner N, Denniff P, Michielsen L, De Vries R, Ji QC, Arnold ME, Woods K, Woolf EJ, Xu Y, Boutet V, Zane P, Kushon S, Rudge JB. A device for dried blood microsampling in quantitative bioanalysis: overcoming the issues associated blood hematocrit. Bioanalysis. 2015;7:653–9.
Mano Y, Kita K, Kusano K. Hematocrit-independent recovery is a key for bioanalysis using volumetric absorptive microsampling devices, Mitra™. Bioanalysis. 2015;7:1821–9.
Kita K, Mano Y. Application of volumetric absorptive microsampling device for quantification of tacrolimus in human blood as a model drug of high blood cell partition. J Pharm Biomed Anal. 2017;143:168–75.
Barco S, Castagnola E, Moscatelli A, Rudge J, Tripodi G, Cangemi G. Volumetric adsorptive microsampling-liquid chromatography tandem mass spectrometry assay for the simultaneous quantification of four antibiotics in human blood: method development, validation and comparison with dried blood spot. J Pharm Biomed Anal. 2017;145:704–10.
Denniff P, Parry S, Dopson W, Spooner N. Quantitative bioanalysis of paracetamol in rats using volumetric absorptive microsampling (VAMS). J Pharm Biomed Anal. 2015;108:61–9.
De Kesel PM, Lambert WE, Stove CP. Does volumetric absorptive microsampling eliminate the hematocrit bias for caffeine and paraxanthine in dried blood samples? A comparative study. Anal Chim Acta. 2015;881:65–73.
Kip AE, Kiers KC, Rosing H, Schellens JH, Beijnen JH, Dorlo TP. Volumetric absorptive microsampling (VAMS) as an alternative to conventional dried blood spots in the quantification of miltefosine in dried blood samples. J Pharm Biomed Anal. 2017;135:160–6.
Miao Z, Farnham JG, Hanson G, Podoll T, Reid MJ. Bioanalysis of emixustat (ACU-4429) in whole blood collected with volumetric absorptive microsampling by LC–MS/MS. Bioanalysis. 2015;7:2071–83.
Nys G, Gallez A, Kok MGM, Cobraiville G, Servais AC, Piel G, Pequeux C, Fillet M. Whole blood microsampling for the quantitation of estetrol without derivatization by liquid chromatography-tandem mass spectrometry. J Pharm Biomed Anal. 2017;140:258–65.
Protti M, Rudge J, Sberna AE, Gerra G, Mercolini L. Dried haematic microsamples and LC-MS/MS for the analysis of natural and synthetic cannabinoids. J Chromatogr B Anal Technol Biomed Life Sci. 2017;1044–1045:77–86.
Qu Y, Brady K, Apilado R, O’Malley T, Reddy S, Chitkara P, Ibarra C, Alexander RV, Dervieux T. Capillary blood collected on volumetric absorptive microsampling (VAMS) device for monitoring hydroxychloroquine in rheumatoid arthritis patients. J Pharm Biomed Anal. 2017;140:334–41.
Thiry J, Evrard B, Nys G, Fillet GM, Kok MG. Sampling only ten microliters of whole blood for the quantification of poorly soluble drugs: itraconazole as case study. J Chromatogr A. 2017;1479:161–8.
Iwasaki K, Shiraga T, Nagase K, Hirano K, Nozaki K, Noda K. Pharmacokinetic study of FK 506 in the rat. Transpl Proc. 1991;23:2757–9.
Kagayama A, Tanimoto S, Fujisaki J, Kaibara A, Ohara K, Iwasaki K, Hirano Y, Hata T. Oral absorption of FK506 in rats. Pharm Res. 1993;10:1446–50.
Park JS, Cho HR, Kang MJ, Choi YS. A rapid and sensitive method to determine tacrolimus in rat whole blood using liquid-liquid extraction with mild temperature ultrasonication and LC–MS/MS. Arch Pharm Res. 2016;39:73–82.
Takada K, Katayama N, Kiriyama A, Usuda H. Distribution characteristics of immunosuppressants FK506 and cyclosporin A in the blood compartment. Biopharm Drug Dispos. 1993;14:659–71.
Wei H, Tao X, Di P, Yang Y, Li J, Qian J, Feng J, Chen W. Effects of traditional Chinese medicine Wuzhi capsule on pharmacokinetics of tacrolimus in rats. Drug Metab Dispos. 2013;41:1398–403.
Zhou YN, Zhang BK, Li J, Zuo XC, Yuan H, Yang GP, Cheng ZN, Liu Z, Li PJ, Tan HY, Zhou LY, Wang CJ, Yang M. Effect of amlodipine on the pharmacokinetics of tacrolimus in rats. Xenobiotica. 2013;43:699–704.
Taillon MP, Furtado M, Garofolo F. Challenges of developing a bioanalytical method for a macrolide immunosuppressant compound by LC–MS/MS. Bioanalysis. 2011;3:1201–15.
European Medicines Agency. Guideline on bioanalytical method validation. 2011.
U.S. Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research Center for Veterinary Medicine. Bioanalytical Method Validation, Guidance for Industry. 2018.
Alak AM, Moy S, Cook M, Lizak P, Niggebiugge A, Menard S, Chilton A. An HPLC/MS/MS assay for tacrolimus in patient blood samples. Correlation with results of an ELISA assay. J Pharm Biomed Anal. 1997;16:7–13.
Upadhyay V, Trivedi V, Shah G, Yadav M, Shrivastav PS. Rapid and sensitive UPLC-MS-MS determination of tacrolimus in Wistar rats and human blood. J Chromatogr Sci. 2014;52:59–67.
Korfmacher W, Luo Y, Ho S, Sun W, Shen L, Wang J, Wu Z, Guo Y, Snow G, O’Shea T. Utility of capillary microsampling for rat pharmacokinetic studies: comparison of tail-vein bleed to jugular vein cannula sampling. J Pharmacol Toxicol Methods. 2015;76:7–14.
Acknowledgements
This study was funded by Eisai Co., Ltd. The authors acknowledge Kathleen Vanderhoof for providing editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was sponsored by Eisai Co., Ltd.
Conflict of Interest
Kenji Kita and Kenichi Noritake are employees of Sunplanet Co., Ltd., a subsidiary of Eisai Co. Ltd., and Yuji Mano is an employee of Eisai Co., Ltd.
Ethics Approval
Animal care and experimental procedures were performed in the animal facility accredited by the Health Science Center for Accreditation of Laboratory Animal Care and Use of the Japan Health Sciences Foundation. All protocols were approved by the Institutional Animal Care and Use Committee and carried out in accordance with the Animal Experimentation Regulations of Eisai Co., Ltd.
Rights and permissions
About this article
Cite this article
Kita, K., Noritake, K. & Mano, Y. Application of a Volumetric Absorptive Microsampling Device to a Pharmacokinetic Study of Tacrolimus in Rats: Comparison with Wet Blood and Plasma. Eur J Drug Metab Pharmacokinet 44, 91–102 (2019). https://doi.org/10.1007/s13318-018-0493-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-018-0493-7