Abstract
Background and Objective
Tacrolimus, a major immunosuppressant used after transplantation, is associated with large interindividual variation involving genetic polymorphisms in metabolic processes. A common variant of the cytochrome P450 (CYP) 3A5 gene, CYP3A5*3, affects blood concentrations of tacrolimus. However, tacrolimus pharmacokinetics at the early stage of transplantation have not been adequately studied in heart transplantation. We retrospectively examined the impact of the CYP3A5 genotype on tacrolimus pharmacokinetics at the early stage of heart transplantation.
Methods
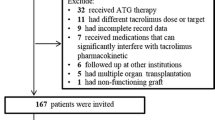
The tacrolimus pharmacokinetic profile was obtained from 65 patients during the first 5 weeks after heart transplantation. Differences in the patients’ characteristics and tacrolimus pharmacokinetic parameters between the CYP3A5 expresser (*1/*1 or *1/*3 genotypes) and non-expresser (*3/*3 genotype) groups were assessed by the Chi-square test, Student’s t test, or Mann–Whitney U test.
Results
The CYP3A5 *1/*1, *1/*3, and *3/*3 genotypes were detected in 5, 22, and 38 patients, respectively. All patients started clotrimazole therapy approximately 1 week after starting tacrolimus. Apparent clearance and dose/weight to reach the target trough concentration (C0) were significantly higher in the expresser group than in the non-expresser group (0.32 vs. 0.19 L/h/kg, p = 0.0003; 0.052 vs. 0.034 mg/kg/day, p = 0.0002); there were no significant differences in the area under the concentration-time curve from 0 to 12 h (AUC0–12) and concentrations at any sampling time point between the two groups.
Conclusion
Similar concentration–time curves for tacrolimus were obtained in the expresser and non-expresser groups by dose adjustment based on therapeutic drug monitoring. These results demonstrate the importance of the CYP3A5 genotype in tacrolimus dose optimization based on therapeutic drug monitoring after heart transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The CYP3A5 expresser group required a higher dose of tacrolimus to reach the target C0 than the non-expresser group. |
Dose adjustment based on therapeutic drug monitoring in heart transplant patients ensured that similar blood concentration–time curves for tacrolimus were seen in CYP3A5 expresser and non-expresser groups. |
Genotype detection prior to transplantation may be beneficial in shortening the time taken to reach the target C0 and allow better control of the blood concentrations in heart transplant patients. |
1 Introduction
Transplant patients are generally treated with multidrug-immunosuppressive agents including calcineurin inhibitors (cyclosporine or tacrolimus), mycophenolate mofetil, and steroids. Recently, tacrolimus has been mainly used, as there is considerable evidence to suggest that it is significantly more effective than cyclosporine in preventing acute rejection in transplant patients, and that it has a superior cardiovascular risk profile [1]. However, the dose adjustment of tacrolimus to maintain appropriate blood concentrations is difficult, since it has a narrow therapeutic range [2]. Moreover, it is necessary to ensure that the concentration of tacrolimus is within the therapeutic range as early as possible after transplantation, since low concentrations of the drug 1–2 weeks after transplantation lead to acute rejection [3]. Therefore, good control of tacrolimus blood concentrations is the primary goal for heart transplant patients at the early stages of transplantation. However, ensuring that the blood concentration of tacrolimus lies within the therapeutic range early after transplantation can be problematic [4, 5] as individual patients have different metabolic characteristics with respect to the drug.
Tacrolimus is primarily metabolized by cytochrome P450 (CYP) 3A isoenzymes, particularly CYP3A4 and CYP3A5, in the liver and intestinal wall [6,7,8]. It is known that the intrinsic clearance of tacrolimus is approximately twofold higher for CYP3A5 than for CYP3A4 [9]. Although the difference in the intestinal clearance of tacrolimus between CYP3A4 and CYP3A5 is unknown, it has been reported that intestinal CYP3A5, as well as hepatic CYP3A5, plays an important role in the first pass effect associated with orally administered tacrolimus [10]. CYP3A5 shows polymorphic expression, which affects the pharmacokinetics of tacrolimus. The wild-type allele, designated CYP3A5*1, produces high levels of full-length CYP3A5 mRNA and expresses high levels of functional CYP3A5 protein. On the contrary, the mutant allele, designated CYP3A5*3, produces very low levels of functional CYP3A5 protein due to an aberrant mRNA that is prematurely degraded [11]. It has been reported that the CYP3A5 genotype affects the pharmacokinetics of tacrolimus mainly in kidney or liver transplant patients [12]. Although the previous studies have shown that the CYP3A5 genotype affects the C0 of tacrolimus in heart transplant patients, other pharmacokinetic parameters have not been adequately studied [13,14,15,16,17]. In addition, there are no reports that have focused on the pharmacokinetics of tacrolimus at the early stages of heart transplantation. The purpose of this study was to investigate the impact of the CYP3A5*1 allele on the pharmacokinetics of tacrolimus at the early stages of heart transplantation. In addition, the difference in the pharmacokinetics of tacrolimus at the early stages of transplantation between CYP3A5 expresser and non-expresser patients was our main concern in this study.
2 Patients and Methods
2.1 Study Design
The retrospective study investigated the effect of CYP3A5 genotype on the pharmacokinetics of tacrolimus at the early stage of heart transplantation. Patients who had undergone heart transplantation at the National Cerebral and Cardiovascular Center in Japan between February 2005 and June 2017 were enrolled in the study. All patients received standard triple-drug immunosuppression therapy that included the regular release formulation of tacrolimus, mycophenolate mofetil, and prednisolone or methylprednisolone as a steroid. Pharmacokinetic profiles were obtained from the patients during the first 5 weeks after heart transplantation. All patients started clotrimazole therapy with troche 10 mg four times daily approximately 1 week after the initiation of treatment with tacrolimus. However, no patient was concomitantly treated with medications that affect the pharmacokinetic parameters of tacrolimus, including macrolides, non-dihydropyridine calcium channel blockers, or everolimus. A previous study found that the tacrolimus C0 of approximately 10 ng/mL was favorable for prevention of acute rejection [18]. In our hospital, tacrolimus was initially administered at a dose of 1 mg/day in two divided doses. Thereafter, the dose was adjusted to achieve a C0 of 9–12 ng/mL, based on the therapeutic drug monitoring of tacrolimus during the first 2 years, approximately. Mycophenolate mofetil was initially administered at a dose of 1.5–2 g in two divided doses. Subsequent doses of these were adjusted based on the leukocyte count and the area under the concentration–time curve (AUC) of mycophenolic acid. A standard steroid taper was carried out in all patients in accordance with the protocol of the National Cerebral and Cardiovascular Center. Genotyping of CYP3A5 (rs776746; CYP3A5*3) was performed after the monitoring and analyses of tacrolimus blood concentrations. Therefore, the dose adjustment of tacrolimus was carried out with no reference to the CYP3A5 genotype for 5 weeks after transplantation.
The study protocol was approved by the National Cerebral and Cardiovascular Center Ethics Committee (reference number M27-067-5) and all patients gave written informed consent regarding the disclosure of clinical data.
2.2 Therapeutic Drug Monitoring and Pharmacokinetic Profiles
The pharmacokinetic profile of tacrolimus during the 5 weeks after transplantation was examined in 65 patients. We collected a blood sample from patients directly prior to tacrolimus administration at 1, 2, and 3 weeks after transplantation. At the 5 weeks after transplantation, we collected a blood sample from patients before administration of tacrolimus and 1, 2, 4, 6, 8, and 12 h after dosing. Approximately 1 mL of venous blood was collected into a disposable syringe and transferred to a vacuum blood collection tube. The samples were centrifuged and harvested blood was frozen at − 30 °C until analysis. The concentration of tacrolimus was measured by an affinity column-mediated immunoassay, using the Dimension Clinical Chemistry System (Siemens Healthineers, Japan) [19]. Of seven sampling points, C0 was obtained directly from the raw data. The dose-adjusted C0 of tacrolimus at 1, 2, 3, and 5 weeks was calculated as the C0 divided by the dose. In addition, the other pharmacokinetic parameters including the C0 were calculated at 5 weeks.
2.3 Pharmacokinetic Analysis
The primary pharmacokinetic variables obtained for tacrolimus were the AUC, mean residence time after oral administration (MRTpo), apparent body clearance after dosing (CL/F), elimination half-life (te1/2), and absorption half-life (ta1/2). With respect to the AUC and area under the moment curve (AUMC), the range from the time before drug administration to the time of the last measurable concentration of drug (AUC0–12 and AUMC0–12) was calculated. In accordance with the non-compartment model, the AUC0–12 and AUMC0–12 were calculated using the linear trapezoidal method. In accordance with the one-compartment model, the elimination rate constant (Ke), absorption rate constant (Ka), te1/2, ta1/2, and CL/F were calculated according to the equations below. The MRTpo,0–∞ of the drug, on single dosing, could be calculated using the basic equation: MRTpo,0–∞ = AUMC0–∞/AUC0–∞. However, in our study, since tacrolimus was administered repeatedly every 12 h, we could not use this equation for calculating MRTpo,0–∞. Pfeffer showed that the equation derived from a basic equation, MRTpo,0–∞ = AUMCpo,0–∞/AUCpo,0–∞, was appropriate for estimation of the equivalent values for MRT on multiple dosing to steady state in accordance with the terminal data point in the dosing interval [20]. Therefore, we calculated MRT po,0–∞ using the equation suggested by Pfeffer. The Ke and Ka were estimated from the slope of the terminal linear portion (6, 8, and 12 sampling points) and the subtraction method based on the regression line, respectively:
2.4 CYP3A5 Genotyping
Genotyping of CYP3A5 (rs776746; CYP3A5*3) was carried out using the newly developed genotyping system, GTS-7000® (Shimadzu, Japan), with 1 μL of the remainder of the whole blood used for laboratory testing. This system can detect single-nucleotide polymorphisms (SNPs) on direct polymerase chain reaction amplification with no requirement for DNA extraction. Prior to the study, genotype results obtained with the GTS-7000® assay were validated using a laboratory-based CYP3A5*3 genotyping assay, namely, a DNA sequence assay using 3130 × L Genetic Analyzers® (Applied Biosystems, USA). The results of SNP detection between two assays were completely consistent. GTS-7000® seems to have the same accuracy as that of the conventional method. Patients were classified into three genotype groups to give CYP3A5 expressers (that is, carriers of *1/*1 or *1/*3), and CYP3A5 non-expressers (*3/*3).
2.5 Statistical Analysis
The characteristics of the heart transplant patients, the pharmacokinetic parameters of tacrolimus, and laboratory test data are expressed as the number, mean ± standard deviation, and median (quartiles 1–3). Categorical data were compared between the expresser and non-expresser groups by performing the Chi-square test. To test the population homogeneity of the subjects, the genotype frequency of the CYP3A5 polymorphism was tested against Hardy–Weinberg equilibrium by performing the Chi-square test. Student’s t test or Mann–Whitney U test was used to assess the difference in continuous values between the expresser and non-expresser groups. Stepwise multiple linear regression analyses for CL/F and AUC0–12 of tacrolimus were performed to determine the effects of all variables examined in the univariate analysis. Backward–forward selection was used to select predictor variables and to quantify the corresponding partial determination coefficient (R2). Bonferroni’s correction was applied to the analyses of characteristics, laboratory test data, and pharmacokinetic parameters of tacrolimus.
Statistical analysis was performed using JMP® version 13.1.0. A p value less than 0.05 was considered statistically significant.
3 Results
3.1 Patient Characteristics
Sixty-five heart transplant patients were enrolled in the study. CYP3A5 *1/*1, *1/*3, and *3/*3 genotypes were detected in 5 (7.7%), 22 (33.8%), and 38 (58.5%) patients, respectively (Table 1). The genotype distribution was in Hardy–Weinberg equilibrium (p = 0.478). Patients with CYP3A5 *1/*1 and *1/*3 were defined as expressers and the patients with CYP3A5 *3/*3 were defined as non-expressers. Consequently, 27 and 38 patients were classified into the expresser and non-expresser groups, respectively. No significant differences were observed in the baseline characteristics between the expresser and non-expresser groups.
3.2 Tacrolimus Pharmacokinetics
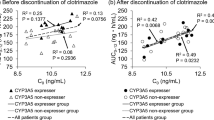
Figure 1 shows the blood concentrations of tacrolimus in the expresser and non-expresser groups at the 5 weeks after transplantation. No significant differences were observed between the two groups. The dose and C0/dose of tacrolimus at the 1, 2, 3, and 5 weeks after transplantation are presented in Table 2, and pharmacokinetic parameters as determined by moment and one compartment model analysis at the 5 week are presented in Table 3. The dose/weight in the expresser group was significantly higher than those in the non-expresser group at the 2, 3, and 5 weeks after transplantation. In addition, C0/dose/weight in the expresser group was significantly lower than in the non-expresser group at the 2, 3, and 5 weeks after transplantation. At the 5 weeks after transplantation, CL/F in the expresser group was significantly higher than in the non-expresser group and AUC0–12/dose/weight in the expresser group was significantly lower than in the non-expresser group. In the multiple linear regression analysis for the CL/F of tacrolimus, CYP3A5 genotype, hematocrit, dose of mycophenolate mofetil, and age were identified as significant explanatory variables (Table 4).
Concentration profile of tacrolimus in 65 heart transplant patients within expresser (CYP3A5 *1/*1 or *1/*3) and non-expresser (CYP3A5 *3/*3) groups at 5 weeks after transplantation when the target C0 was 9–12 ng/mL. The data are represented as the median for each group. No significant differences were observed between the two groups. C0 trough concentration, CYP cytochrome P450
4 Discussion
This study revealed that there was no significant difference in tacrolimus concentrations between the expresser and non-expresser groups at the 5 weeks after heart transplantation (Fig. 1). In addition, moment and one compartment model analyses showed that there were no significant differences in te1/2, ta1/2, MRTpo,0–∞, and AUC0–12 between the two groups. Meanwhile, CL/F and dose/weight at the 5 weeks after transplantation were significantly higher in the expresser group than in the non-expresser group. These findings suggest that similar concentration–time curves for tacrolimus and AUC0–12 were obtained in the expresser and non-expresser groups by dose adjustment based on therapeutic drug monitoring.
In this study, although the CYP3A5 expresser group required higher doses of tacrolimus to reach target C0 compared to the non-expresser group at the early stages of heart transplantation, no significant differences were observed in AUC0–12. In addition, there were no significant differences in te1/2 or MRTpo,0–∞ between the two groups. AUC0–12, te1/2, and MRTpo,0–∞ are calculated based on systemic circulating blood concentrations after the first pass effect. Therefore, since CYP3A5 affected the first pass effect rather than the systemic circulation process, the expresser group may require a higher dose of tacrolimus to reach target C0 than the non-expresser group.
In the study here, the target C0 level (9–12 ng/mL) was not reached at the 1 week after transplantation. In the study, the CYP3A5 genotype was not determined at the early stages of transplantation in all patients. According to our protocol, tacrolimus was initially administered at a dose of 1 mg/day in two divided doses, regardless of genotype and body weight. Meanwhile, dose/weight at the 5 weeks of transplantation was approximately 1.5-times higher in the expresser group compared to the non-expresser group. Therefore, it is desirable that the initial dose of tacrolimus is determined taking the CYP3A5 genotype and body weight into consideration.
Clotrimazole, an azole antifungal drug, is frequently used for the prophylaxis and treatment of oral mucosal candidiasis following solid organ transplantation. Drug interactions via CYP3A between tacrolimus and azole antifungal drugs (that is, clotrimazole, itraconazole, ketoconazole, miconazole, fluconazole, and posaconazole) are well known and represent a major concern when treating patients after transplantation [21,22,23,24,25,26,27,28,29,30]. In our protocol, all patients started treatment with clotrimazole troche for prevention of oral candida approximately 1 week after the initiation of tacrolimus therapy. Our results showed that C0/dose/weight at the 5 weeks in the expresser group was significantly lower than in the non-expresser group (188.1 vs. 317.6 ng/mL/mg/kg/day, p = 0.0002). Meanwhile, Lesche et al. reported that C0/dose/weight in the CYP3A5 expresser group was significantly lower than in the non-expresser group (61.2 vs. 122.2 ng/mL/mg/kg/day, p = 0.001) in heart transplant patients [16], and Díaz-Molina et al. reported that C0/dose/weight in the expresser group was significantly lower than in the non-expresser group (84.7 vs. 205.8 ng/mL/mg/kg/day, p = 0.005) [13]. In these previous studies, it is unclear whether clotrimazole was concomitantly administered. However, C0/dose/weight values in the expresser and non-expresser groups of our study were higher than those presented in the studies outlined above. This finding may suggest that clotrimazole affects tacrolimus concentrations. In the study here, tacrolimus therapy was initiated immediately following heart transplantation, with clotrimazole treatment beginning approximately 1 week after this initiation. Although the impact of clotrimazole on the pharmacokinetics of tacrolimus is not established, the dosing timing and schedules of tacrolimus and clotrimazole may have major effects on the pharmacokinetics of the former drug and the time taken to reach its target C0.
Some potential limitations should be taken into account when interpreting the results obtained from this study. First, this was a single-center study with a retrospective design. Heart transplantation has not been a major treatment for patients with serious heart failure in Japan [31]. Therefore, we were unable to register sufficient cases for this study. However, it is beneficial to know the influence of genetic polymorphisms of CYP3A5 on the pharmacokinetics of tacrolimus in Japanese heart transplant patients. Second, three distinct phenotypes (CYP3A5 *1/*1, *1/*3, and *3/*3 genotypes) were detected in this study. Although a multiple group comparison may be applicable if a sufficient number of patients are included, there were only five (7.7%) patients with CYP3A5*1*1 in this study. Therefore, the patients were classified into the expresser (CYP3A5*1*1 and CYP3A5*1*3) and non-expresser (CYP3A5*3*3) groups. Third, some possible confounding factors should be considered when interpreting the results. In the multiple linear regression analysis for the CL/F of tacrolimus, CYP3A5 genotype, hematocrit, dose of mycophenolate mofetil, and age were identified as significant explanatory variables. Recently, it was reported that the CL/F of tacrolimus decreased when co-administered with mycophenolate mofetil [32]. In addition, the clearance of tacrolimus is affected by hematocrit and protein binding [33]. Moreover, the effect of age on tacrolimus pharmacokinetics has been reported [34]. These reported findings are not inconsistent with our results. There were also no significant differences in these explanatory variables between the CYP3A5 expresser and non-expresser groups. Therefore, these factors may not have affected the difference in CL/F between the CYP3A5 expresser and non-expresser groups in this study. Clotrimazole may affect the pharmacokinetics of tacrolimus. However, we have not directly investigated the effects of clotrimazole on the pharmacokinetics of tacrolimus here. In this study, 40 mg/day of clotrimazole was administered for 5 weeks for all patients. There were no significant differences in percentage of patients who were treated with clotrimazole at individual sampling date (Supplementary Table 1). Therefore, concomitant use of clotrimazole may not have greatly affected the results in the study. In addition, there were no significant differences in the doses of mycophenolate mofetil and steroids between the CYP3A5 expresser and non-expresser groups on individual sampling dates (Supplementary Table 1). Furthermore, other CYP3A4 or CYP3A5 inhibitors and inducers were not used during the observational period in all study patients. Thus, drug–drug interactions were unlikely to have affected the results in the study. Fourth, the CYP3A4 genotype was not determined in this study. CYP3A4 polymorphism, including the CYP3A4*1B genotype, may influence tacrolimus pharmacokinetics [35]. However, it has been reported that the CYP3A4*1B genotype was not detected in Japanese patients [36]. Indeed, no report has shown that CYP3A4 polymorphism had an effect on the pharmacokinetics of tacrolimus in Japanese patients. Therefore, CYP3A4 polymorphisms may not have affected the study results. Fifth, tacrolimus metabolites were not determined in this study. The tacrolimus metabolite-to-tacrolimus ratio may be useful information to confirm the nature of the interaction. This is a major limitation in the study.
The effects of CYP3A5 polymorphism on the pharmacokinetics of tacrolimus have been studied in various solid organ transplant patients, including heart transplant patients. However, the previous studies in heart transplantation have reported the effect of CYP3A5 polymorphism on the blood concentration of tacrolimus, but no other pharmacokinetic parameters except for the C0 have been analyzed [13,14,15,16,17]. In addition, the effects of CYP3A5 genotype on the pharmacokinetics of tacrolimus at the early stage of heart transplantation remain unclear. This is the first study to have focused on the effect of CYP3A5 genotype on the pharmacokinetics of tacrolimus at the early stage of heart transplantation. Since acute rejection frequently occurs at the early stage of transplantation, evaluation of the pharmacokinetics at this stage may be useful to reduce the risk of acute rejection in heart transplant patients.
5 Conclusion
This study revealed that the CYP3A5 expresser group required a higher dose of tacrolimus to reach the target C0 than the non-expresser group. This may be attributable to the higher CL/F observed at the early stages of heart transplantation. In addition, dose adjustment based on therapeutic drug monitoring in heart transplant patients ensured that similar blood concentration–time curves for tacrolimus were seen in CYP3A5 expresser and non-expresser groups. Finally, genotype detection prior to transplantation may be beneficial in shortening the time taken to reach the target C0 and allow better control of the blood concentrations in heart transplant patients.
References
Margreiter R. Efficacy and safety of tacrolimus compared with ciclosporin microemulsion in renal transplantation a randomised multicentre study. Lancet. 2002;359:741–6.
Böttiger Y, Brattström C, Tydén G, Säwe J, Groth C. Tacrolimus whole blood concentrations correlate closely to side-effects in renal transplant recipients. Br J Clin Pharmacol. 1999;48(3):445–8.
Staatz C, Taylor P, Tett S. Low tacrolimus concentrations and increased risk of early acute rejection in adult renal transplantation. Nephrol Dial Transplant. 2001;16(9):1905–9.
Wong S. Therapeutic drug monitoring for immunosuppressants. Clin Chim Acta. 2001;313(1–2):241–53.
Tsuchiya N, Satoh S, Tada H, Li Z, Ohyama C, Sato K, et al. Influence of CYP3A5 and MDR1 (ABCB1) polymorphisms on the pharmacokinetics of tacrolimus in renal transplant recipients. Transplantation. 2004;78(8):1182–7.
Dai Y, Hebert MF, Isoherranen N, Davis CL, Marsh C, Shen DD, et al. Effect of CYP3A5 polymorphism on tacrolimus metabolic clearance in vitro. Drug Metab Dispos Biol Fate Chem. 2006;34(5):836–47.
Sattler M, Guengerich FP, Yun CH, Christians U, Sewing KF. Cytochrome P-450 3A enzymes are responsible for biotransformation of FK506 and rapamycin in man and rat. Drug Metab Dispos Biol Fate Chem. 1992;20(5):753–61.
Iwasaki K. Metabolism of tacrolimus (FK506) and recent topics in clinical pharmacokinetics. Drug Metab Pharmacokinet. 2007;22(5):328–35.
Dai Y, Hebert M, Isoherranen N, Davis C, Marsh C, Shen D, et al. Effect of CYP3A5 polymorphism on tacrolimus metabolic clearance in vitro. Drug Metab Dispos. 2006;34(5):836–47.
Uesugi M, Masuda S, Katsura T, Oike F, Takada Y, Inui K. Effect of intestinal CYP3A5 on postoperative tacrolimus trough levels in living-donor liver transplant recipients. Pharmacogenet Genom. 2006;16(2):119–27.
Kuehl P, Zhang J, Lin Y, Lamba J, Assem M, Schuetz J, et al. Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat Genet. 2001;27(4):383–91.
Staatz C, Goodman L, Tett S. Effect of CYP3A and ABCB1 single nucleotide polymorphisms on the pharmacokinetics and pharmacodynamics of calcineurin inhibitors: part I. Clin Pharmacokinet. 2010;49(3):141–75.
Diaz-Molina B, Tavira B, Lambert JL, Bernardo MJ, Alvarez V, Coto E. Effect of CYP3A5, CYP3A4, and ABCB1 genotypes as determinants of tacrolimus dose and clinical outcomes after heart transplantation. Transplant Proc. 2012;44(9):2635–8.
Gijsen V, Mital S, van Schaik RH, Soldin OP, Soldin SJ, van der Heiden IP, et al. Age and CYP3A5 genotype affect tacrolimus dosing requirements after transplant in pediatric heart recipients. J Heart Lung Transplant. 2011;30(12):1352–9.
Kniepeiss D, Renner W, Trummer O, Wagner D, Wasler A, Khoschsorur GA, et al. The role of CYP3A5 genotypes in dose requirements of tacrolimus and everolimus after heart transplantation. Clin Transplant. 2011;25(1):146–50.
Lesche D, Sigurdardottir V, Setoud R, Oberhänsli M, Carrel T, Fiedler G, et al. CYP3A5*3 and POR*28 genetic variants influence the required dose of tacrolimus in heart transplant recipients. Ther Drug Monit. 2014;36(6):710–5.
Zheng H, Webber S, Zeevi A, Schuetz E, Zhang J, Bowman P, et al. Tacrolimus dosing in pediatric heart transplant patients is related to CYP3A5 and MDR1 gene polymorphisms. Am J Transplant. 2003;3(4):477–83.
Staatz C, Taylor P, Tett S. Low tacrolimus concentrations and increased risk of early acute rejection in adult renal transplantation. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Renal Assoc. 2001;16(9):1905–9.
Cangemi G, Barco S, Bonifazio P, Maffia A, Agazzi A, Melioli G. Comparison of antibody-conjugated magnetic immunoassay and liquid chromatography-tandem mass spectrometry for the measurement of cyclosporine and tacrolimus in whole blood. Int J Immunopathol Pharmacol. 2013;26(2):419–26.
Pfeffer M. Estimation of mean residence time from data obtained when multiple-dosing steady state has been reached. J Pharm Sci. 1984;73(6):854–6.
Choy M. Tacrolimus interaction with clotrimazole: a concise case report and literature review. P T Peer Rev J Formul Manag. 2010;35(10):568–9.
El-Asmar J, Gonzalez R, Bookout R, Mishra A, Kharfan-Dabaja MA. Clotrimazole troches induce supratherapeutic blood levels of sirolimus and tacrolimus in an allogeneic hematopoietic cell-transplant recipient resulting in acute kidney injury. Hematol Oncol Stem Cell Ther. 2016;9(4):157–61.
Gibbs M, Kunze K, Howald W, Thummel K. Effect of inhibitor depletion on inhibitory potency: tight binding inhibition of CYP3A by clotrimazole. Drug Metab Dispos. 1999;27(5):596–9.
Gibbs M, Thummel K, Shen D, Kunze K. Inhibition of cytochrome P-450 3A (CYP3A) in human intestinal and liver microsomes: comparison of Ki values and impact of CYP3A5 expression. Drug Metab Dispos. 1999;27(2):180–7.
Laftavi MR, Pankewycz O, Patel S, Nader N, Kohli R, Feng L, et al. African American renal transplant recipients (RTR) require higher tacrolimus doses to achieve target levels compared to white RTR: does clotrimazole help? Transplant Proc. 2013;45(10):3498–501.
Lalan S, Abdel-Rahman S, Gaedigk A, Leeder JS, Warady BA, Dai H, et al. Effect of CYP3A5 genotype, steroids, and azoles on tacrolimus in a pediatric renal transplant population. Pediatr Nephrol. 2014;29(10):2039–49.
Moody DE, Liu F, Fang WB. Azole antifungal inhibition of buprenorphine, methadone and oxycodone in vitro metabolism. J Anal Toxicol. 2015;39(5):374–86.
Mordvinov VA, Shilov AG, Pakharukova MY. Anthelmintic activity of cytochrome P450 inhibitors miconazole and clotrimazole: in vitro effect on the liver fluke Opisthorchis felineus. Int J Antimicrob Agents. 2017;50(1):97–100.
Saad A, DePestel D, Carver P. Factors influencing the magnitude and clinical significance of drug interactions between azole antifungals and select immunosuppressants. Pharmacotherapy. 2006;26(12):1730–44.
Viesselmann CW, Descourouez JL, Jorgenson MR, Radke NA, Odorico JS. Clinically significant drug interaction between clotrimazole and tacrolimus in pancreas transplant recipients and associated risk of allograft rejection. Pharmacotherapy. 2016;36(3):335–41.
Nakatani T, Fukushima N, Ono M, Saiki Y, Matsuda H, Nunoda S, et al. The registry report of heart transplantation in Japan (1999–2014). Circ J. 2016;80(1):44–50.
Kim JH, Han N, Kim MG, Yun HY, Lee S, Bae E, et al. Increased exposure of tacrolimus by co-administered mycophenolate mofetil: population pharmacokinetic analysis in healthy volunteers. Sci Rep. 2018;8(1):1687.
Undre NA, Schafer A. Factors affecting the pharmacokinetics of tacrolimus in the first year after renal transplantation. European Tacrolimus Multicentre Renal Study Group. Transpl Proc. 1998;30(4):1261–3.
Staatz CE, Tett SE. Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin Pharmacokinet. 2004;43(10):623–53.
Shi WL, Tang HL, Zhai SD. Effects of the CYP3A4*1B Genetic Polymorphism on the Pharmacokinetics of Tacrolimus in Adult Renal Transplant Recipients: a Meta-Analysis. PLoS One. 2015;10(6):e0127995.
Lamba JK, Lin YS, Thummel K, Daly A, Watkins PB, Strom S, et al. Common allelic variants of cytochrome P4503A4 and their prevalence in different populations. Pharmacogenetics. 2002;12(2):121–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No source of funding was used to conduct this study.
Disclosure of potential conflicts of interest
Takaya Uno, Kyoichi Wada, Sachi Matsuda, Yuka Terada, Akira Oita, Atsushi Kawase, and Mitsutaka Takada declare that they have no conflicts of interest.
Ethical approval
The study protocol was approved by the National Cerebral and Cardiovascular Center Ethics Committee (reference number M27-067-5).
Informed consent
Written informed consent regarding the disclosure of clinical data was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Uno, T., Wada, K., Matsuda, S. et al. Impact of the CYP3A5*1 Allele on the Pharmacokinetics of Tacrolimus in Japanese Heart Transplant Patients. Eur J Drug Metab Pharmacokinet 43, 665–673 (2018). https://doi.org/10.1007/s13318-018-0478-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-018-0478-6