Abstract
Background and Objectives
The selection of suitable functional excipients with low toxicity index and having P-glycoprotein inhibitory characteristics represents a major innovative step in designing a promising formulation for oral chemotherapy. This study was aimed at investigating the chemosensitizing effect of selected pharmaceutical excipients to improve the in vivo pharmacokinetic performance of VP-16.
Methods
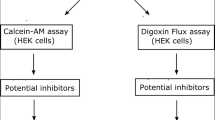
The pharmaceutical excipients having P-glycoprotein inhibitory activity were screened by shake flask method for their VP-16 solubilization capacity. The cumulative amount of VP-16 was determined with or without the selected pharmaceutical excipients at three different concentrations (0.1 % w/v, 0.5 % w/v and 1 % w/v) by an everted gut sac technique. Moreover, pharmacokinetic studies were also performed to determine the oral bioavailability assessment of VP-16 in albino male Wistar rats.
Results
The absorptive transport from mucosal-to-serosal (M → S) and secretory transport from serosal-to-mucosal (S → M) for VP-16 solution over 90 min were found to be (3.58 ± 0.32) × 10−6 and (14.63 ± 3.11) × 10−6 cm/s, respectively, with a net efflux of 4.08. Addition of verapamil (200 µM), a P-glycoprotein inhibitor, elevated the transport from M → S [Papp from (3.58 ± 0.32) to (9.66 ± 1.55) × 10–6 cm/s, p < 0.05] and lowered the S → M [Papp from (14.63 ± 3.11) to (13.35 ± 2.01) × 10–6 cm/s, p < 0.01], with a net efflux of 1.38. The relative bioavailability of VP-16 following oral administration (4.5 mg/kg) in rats was increased significantly (p < 0.01) in presence of Labrasol micellar solution at a concentration of 5 % (w/v) when compared with VP-16 solution alone.
Conclusion
The findings suggest that pharmaceutical excipients may be employed in the development of drug delivery systems to improve the oral bioavailability of drugs having low solubility and/or less permeability as a result of substantial P-glycoprotein mediated efflux.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Research showed that the pharmaceutical excipients could be used as a chemosensitizer for P-gp substrate agents with the advantages of increasing the intestinal absorption of drugs secreted by a P-gp-mediated efflux consequently enhancing oral bioavailability. |
The relative bioavailability of VP-16 following oral administration in rats was significantly increased in the presence of Labrasol micellar solution. |
Our findings suggest that pharmaceutical excipients may be employed in the development of drug delivery systems to improve the oral bioavailability of drugs having low solubility and/or less permeability as a result of substantial P-gp mediated efflux. |
1 Introduction
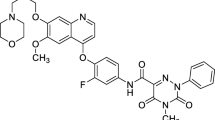
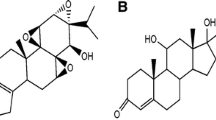
The oral delivery of anticancer drugs presents a major challenge in terms of advancement of cancer therapy because they are both metabolized and actively expelled from the intestine. Furthermore, insufficient aqueous solubility of these drugs makes their oral delivery extremely challenging. One important chemotherapeutic drug, etoposide (VP-16) is poorly absorbed from the gastrointestinal tract (GI) following oral administration, leading to a reduction in clinical outcomes [1]. This drug is dynamically pumped out from the intestinal wall by a transmembrane permeability glycoprotein (P-gp) and metabolized by cytochrome P450, mainly cytochrome P450 3A4 that affects its pharmacokinetic parameters [2]. The unfavorable physicochemical properties of VP-16 along with adverse physiological barrier of the GI tract constitute major challenges for successful oral delivery. The design of effective formulation for P-gp substrate drugs has long been a major challenge, because drug efficacy can be severely limited by instability or insufficient solubility in the vehicle. Consequently, more attention is now being paid to pharmaceutical excipients as efflux pump inhibitors in improving oral drug delivery [3–5]. Several pharmaceutical excipients are emerging as different classes of P-gp inhibitors owing to many advantages including that they are safe, not being absorbed from the gut and pharmaceutically acceptable [6, 7]. The chemosensitizing effects of such excipients were first proved when combined with the active P-gp substrate molecule [8]. This was followed by studies from Woodcock et al. [9] and since then several pharmaceutical excipients [Tweens (20 & 80), Spans, Cremophors (EL & RH 40), Labrasol, Transcutol-P, vitamin-E TPGS, Solutol HS 15, and Gelucire] have been investigated to inhibit P-gp-mediated efflux for different chemotherapeutic agents [4, 5, 10]. The mechanisms by which excipient inhibits P-gp activity varies with the excipient types and their clinical implications are currently unclear [11–15]. There are various mechanisms that can be responsible for P-gp efflux pump inhibition including fluidization of the lipid membranes, inhibition of ATPase activity resulting in ATP depletion and down regulating P-gp expression [4, 5, 10]. Surfactants and solubilizing excipients such as Labrasol, Tween 20, Tween 80, Solutol HS-15, TPGS, enclose themselves between the lipophilic tails of the bilayer membrane thereafter modifying the hydrogen bonding and ionic forces of cell membranes which may lead to improving the intestinal absorption of P-gp substrates via both a paracellular and a transcellular pathway [16]. Some surfactants such as pluronic and polymers can further decrease the P-gp ATPase activity and some of them act concurrently by both the mechanisms. It was also observed that Lipid excipients such as Gelucire and Peceol inhibit Protein kinase C activity, reducing phosphorylation of P-gp due to their capability of down regulating the MDR1 gene expression [12]. Micellar solubilization with pharmaceutical excipients is used as a potential alternative for solubilising hydrophobic drugs in aqueous environments and therefore improving their bioavailability. Mixed micelles have been reported to bypass P-gp drug efflux since the drug accumulation was not influenced by verapamil, a well-known P-gp inhibitor [17]. Two important parameters that also govern P-gp inhibitory activity include hydrophilic–lipophilic balance (HLB) and surfactant concentration. Concentrations that are non-toxic to the intestinal mucosa are most commonly used to inhibit P-gp. Non-ionic surfactants usually are better solubilizing agents than ionic surfactants for hydrophobic drugs, because of their lower critical micelle concentration (CMC) values. It would be advantageous if such surfactants were more active above the CMC, since they would provide dual action of solubilizing hydrophobic substrates as well as inhibiting efflux [14]. In certain cases, there is loss of the inhibitory effect due to P-gp substrate entrapment in the micelles and this effect increases until CMC is reached. In another scenario, inhibitory effect increases even beyond CMC and this could be attributed to the fact that drug could be entrapped in micelles bypass P-gp-mediated efflux [18]. The selection of a suitable functional excipient with low toxicity index and having P-gp inhibitory characteristics represents a major innovative step in designing a promising formulation for oral chemotherapy. In the light of above discussion, the present work aimed to investigate the chemosensitizing effect of pharmaceutical excipients on feasibility of oral absorption of VP-16 through in vitro and in vivo investigation.
2 Materials and methods
2.1 Materials
VP-16, received as a gift sample from Dabur Pharma Limited (Ghaziabad, UP, India). Verapamil was purchased from Sigma Aldrich (St. Louis, MO, USA). Solutol HS 15 was received from BASF (Mumbai, India). Gelucire 44/14, Peceol, Transcutol-P and Labrasol were gifted (Gattefosse, France) through Colorcon Asia (Mumbai, India). Solutol HS 15, Cremophor EL were received from BASF (Mumbai, India). Tween 80, Poly ethylene glycol 400 (PEG-400) and propylene glycol were procured from S.D. Fine Chemicals Ltd. (Mumbai, India). Kreb’s ringer solution (KRB): NaCl (7.0 g), KCl (0.35 g), CaCl2 (0.28 g), MgSO4 (0.28 g), NaHCO3 (2.10 g), KH2PO4 (0.16 g) and d-glucose (5.05 g) is dissolved in 1 L of distilled water. Other chemicals used were of HPLC or, analytical reagent grades.
2.2 Animals
All animal studies were conducted according to the guidelines of the Institutional Animal Ethics Committee (IAEC) of the Jamia Hamdard (Hamdard University), New Delhi. Wistar male albino rats (200–300 g) were obtained from animal house of Jamia Hamdard and kept under standard laboratory conditions, temperature at 25 ± 2 °C, relative humidity (55 ± 5 %); were housed in polypropylene cages with free access to standard laboratory diet (Lipton feed, Mumbai, India) and water ad libitum. Rats were fasted overnight prior to the experiment except free access to water.
2.3 Solubility studies
A number of pharmaceutical excipients were screened by shake flask method for their drug solubilization capacity. For this, an excess amount of VP-16 was added to 2 mL of pharmaceutical excipients namely Peceol, Labrasol, Solutol HS 15, Gelucire, Cremophor EL, Tween 20, Tween 80, polyethylene glycol 400 (PEG 400), Transcutol-P and Propylene glycol and the mixture was stirred using a vortex mixer (Nirmal International, Delhi, India). The mixtures were kept at 25 ± 50 °C in an automatic shaking incubator (Shel Lab, Ave Cornelius, Oregon, USA) for 48 h. The samples were centrifuged at 3000 rpm for 15 min (REMI International, Mumbai, India). The supernatant was separated and filtered using 0.22 µm filter (Millipore USA). The aliquots of the supernatant were diluted with methanol and solubility was determined using RP-HPLC method [19].
2.4 Bidirectional Transport Studies
VP-16 transport across rat ileum tissue was investigated by method reported previously [20]. Briefly, ileum segment was immediately removed, washed with cold KRB and then gently mounted intact in modified Ussing chambers. Ileum segment was then suspended in 50 mL of pre oxygenated KRB and 3 mL of KRB was placed in the serosal compartment, pH 7.4 at 37 °C, under continuous supply. After an incubation period of 30 min, for investigation of the absorptive transport i.e., mucosal-to-serosal (M → S), KRB was replaced by VP-16 solution (100 µg/mL) on mucosal side in 50 mL gassed with CO2/O2, 5/95 % at 37 ± 2 °C. The transport of VP-16 in presence and absence of selected excipients at three different concentrations (0.1, 0.5 and 1 %) was investigated. For investigation of serosal-to-mucosal (S → M) transport, the test solutions were placed on the serosal side i.e., without inversion of ileum. The transport of VP-16 solution from, M → S and S → M transport was also investigated in the presence of a known P glycoprotein inhibitor, verapamil (200 µM). The aliquots (0.5 mL) of samples were collected at 30 min intervals up to 120 min and replaced by the same volume of KRB solution. The samples collected from each time point were stored at −20 °C until analyzed by HPLC method for the estimation of apparent permeability coefficient (Papp). The cumulative amount of VP-16 permeated was plotted as a function of time for VP-16 solution alone and in the presence of pharmaceutical excipients.
The transepithelial Papp was calculated from the linear slope of the plot using the following equation (Eq. 1):
where, Papp: transepithelial apparent permeability coefficient (cm/s), dQ/dT: the cumulative amount of drug (Q) appearing in the acceptor side as a function of time, and was obtained from the slope of the linear portion of the amount transported-versus-time plot.
Co: the initial concentration of substrate in the donor chamber (µg/mL)
A surface area of the intestine in (cm2)
The efflux ratio (ER) was used to evaluate the function of P-gp, using the following equation (Eq. 2):
where, Papp S → M is the intestinal apparent permeability coefficient from serosal-to-mucosal side and Papp M → S is the intestinal apparent permeability coefficient from mucosal-to-serosal side.
2.5 Pharmacokinetic studies
Adult wistar male albino rats (200–250 g) were fasted overnight prior to the experiment except for free access to water. Twenty-four rats were allocated into four groups (n = 6) at random before the experiments. In group I, animals were orally administered VP-16 suspension in 0.25 % w/v sodium carboxymethyl cellulose, while animals in groups II, III &IV received VP-16 solution dissolved in Labrasol at 1, 5 and 10 % w/v concentrations, respectively. Dose for the rats was calculated based on the body weight of rats according to the surface area ratio. To convert the dose used in humans to a dose based on surface area for rats, multiply by the Km factor [21]. Oral dose is equivalent to 50 mg for adult human being (70 kg) and rat dose equivalent can be more appropriately calculated using the following equation (Eq. 3):
where, Km is factor for converting mg/kg dose to mg/m2dose. The Km factor is not constant for any species, but increases as body weight increases. For example, the Km value in rats varies from 5.2 for a 100 g rat to 7.0 for 250 g rats [22]. Therefore, the dose of VP-16 4.5 mg/kg which is equivalent to VP-16 50 mg for adult human being was administered to rats (Eq. 3). Average weight of each rat in this group was 230 g, therefore, dose of VP-16 for each rat will be 1.035 mg (4.5 mg/kg weight of rat). 5 mg of VP-16 was exactly weighed and mixed with 3 mL of double distilled water (1.67 mg/mL). Thus, each rat in this group was given 620 µL (1.035 mg in 620 µL) using oral feeding gavage. The rats were anesthetized using ether and blood samples (approximately 0.5 mL) were withdrawn from the retro-orbital plexus of rat at 0 (pre-dose), 25, 50, 75, 100, 125, 150, 175, 200, 225, 250 min and collected in eppendorf tube containing saturated solution of disodium ethylenediaminetetraacetic acid as an anticoagulant. The blood samples were mixed thoroughly with anticoagulant solution to prevent blood clotting and centrifuged at 4000 rpm for 15 min. The supernatant plasma was separated and stored at −20 °C until HPLC analysis was carried out.
2.6 HPLC Analysis
The analysis of VP-16 samples were carried out in a Waters Alliance e 2695 separating module (Waters Co., Milford, MA, USA) using photo diode array detector (waters 2998) fitted with an autosampler as described previously [19]. The instrument was controlled by the use of empower software installed with equipment for data collection and acquisition. Separation of VP-16 was carried out using LiChrospher 100 C18 reverse-phase column (250 mm × 4.6 mm i.d., 5 μm particle size) at an ambient temperature (25 ± 2 °C). The mobile phase containing a mixture of acetonitrile and phosphate buffer saline (55:45), was pumped at a flow rate of 1.0 mL/min. The mobile phase was filtered through a 0.22 μm nylon filter prior to use. The regression equation for the calibration plot was y = 20903x + 739.47 (n = 3; detection at 283 nm). The intra-day precision was found to be ≤1.581 % (n = 6) and inter-day precision over three different days was calculated as ≤2.113 % (n = 6). Intra-day and inter-day accuracy were found to be 98.00–100.07 and 97.00–100.12 %, respectively. The limits of detection (LOD) and quantitation (LOQ) were calculated by the method based on the standard deviation (σ) of the responses for blank samples in triplicate and the slope (S) of the calibration plot, by use of the formulae LOD = 3.3σ/S and LOQ = 10 σ/S. The LOD and LOQ were found to be 4.7 and 11.6 ng mL−1, respectively.
2.7 Calculations and Statistical Analysis
Pharmacokinetic parameters were determined using pharmacokinetic software (PK solver function for Microsoft Excel, Pharsight Corporation Mountain View, CA, USA). Pharmacokinetic parameters such as maximum plasma concentration (C max), time of peak concentration (T max), and area under the concentration time curve until last observation (AUC0→250min) were calculated individually for each subject in the group and the values were expressed as mean ± SD. Pharmacokinetic data among different test formulations were compared for statistical significance by the one-way ANOVA followed by Tukey–Kramer multiple comparisons test using GraphPad Instat software (GraphPad Software Inc., CA, USA). The relative bioavailability was calculated using the following equation (Eq. 4):
A p value < 0.05 was considered statistically significant. All data are presented as mean value ± SD
3 Results
3.1 Effect of Pharmaceutical Excipients on Solubility
The solubility of VP-16 was found to be 136.5 ± 2.67 and 126.7 ± 2.87 mg/mL in Solutol HS 15 and in Labrasol, respectively. The lowest solubility of VP-16 was found in Peceol and Gelucire was 7.4 ± 2.87 and 10.6 mg/mL, respectively (Fig. 1).
3.2 Bidirectional Transport Studies
The absorptive (M → S) and secretory (S → M) transport of VP-16 in the presence of three different concentrations (0.1, 0.5 and 1 %) of the P-gp modulating excipients i.e., Solutol HS-15, Labrasol and Transcutol-P are shown in Table 1. The absorptive permeability from (M → S) and secretory (S → M) for VP-16 drug solution transport over 90 min were found to be (3.58 ± 0.32) × 10−6 and (14.63 ± 3.11) × 10−6 cm/s, respectively, giving a net ER of 4.08 (Eqs. 1, 2). The absorptive permeability of VP-16 solution was significantly (Dunnett test: p < 0.05) increased from (3.58 ± 0.32) × 10−6 to (9.66 ± 1.55) × 10−6 cm/s while the secretory permeability was decreased from (14.63 ± 3.11) × 10−6 to (13.35 ± 2.01) × 10−6 cm/s, p < 0.01, in the presence 200 µM of verapamil.
Similarly, the Papp value (M → S) of VP-16 in the form of micellar solution with Solutol HS-15 transport at 0.1, 0.5 and 1 % concentration was found to be (5.12 ± 1.55) × 10−6, (5.85 ± 2.34) × 10−6 and (6.48 ± 3.22) × 10−6, respectively. The Papp value (S → M) of VP-16 in the form of micellar solution with Solutol HS-15 transport at 0.1, 0.5 and 1 % concentration was found to be (13.87 ± 2.34) × 10−6, (13.72 ± 1.52) × 10−6 and (13.54 ± 3.15) × 10−6, respectively.
In the same fashion, the Papp value (M → S) of VP-16 in the form of micellar solution with Labrasol transport at 0.1, 0.5 and 1 % concentration was found to be (8.44 ± 0.42) × 10−6, (8.59 ± 2.02) × 10−6 and (9.15 ± 1.66) × 10−6, respectively. The Papp value (S → M) of VP-16 in the form of micellar solution with Solutol HS-15 transport at 0.1, 0.5 and 1 % concentration was found to be (12.80 ± 1.22) × 10−6, (12.11 ± 2.54) × 10−6 and (11.75 ± 3.11) × 10−6, respectively. VP-16 micellar solution with Transcutol-P, the Papp value (M → S) at 0.1, 0.5 and 1 % concentration was found to be (7.11 ± 3.70) × 10−6, (7.76 ± 2.98) × 10−6 and (8.43 ± 3.88) × 10−6, respectively. The Papp value (S → M) of VP-16 in the form of micellar solution with Transcutol-P transport at 0.1, 0.5 and 1 % concentration was found to be (12.58 ± 1.82) × 10−6, (12.19 ± 2.06) × 10−6 and (12.03 ± 3.19) × 10−6, respectively.
3.3 In vivo Pharmacokinetics
Plasma concentration profile after oral administration of VP-16 alone, and in presence of Labrasol (1 % w/v, 5 % w/v and 10 % w/v) in Wistar rats are depicted in Fig. 2. Table 2 shows the pharmacokinetic parameters (C max, T max, AUC0→250min and relative bioavailability) after oral administration of VP-16 alone, and in presence of Labrasol at different concentration (1 % w/v, 5 % w/v and 10 % w/v). The C max value of VP-16 alone and in presence of Labrasol at different concentration (1 % w/v, 5 % w/v and 10 % w/v) resulted, 143.86 ± 6.35, and 674.34 ± 8.16, 1024.21 ± 15.84, 897.10 ± 21.09 ng/mL, respectively. The difference in C max with Labrasol at 5 % (w/v) concentration was significantly different (p < 0.01) when compared with VP-16 solution alone (Table 2). The T max value of VP-16 alone is 125 ± 6.45 min and in presence of Labrasol at different concentration (1 % w/v, 5 % w/v and 10 % w/v) found to be and 110 ± 4.19, 77 ± 5.22, 105 ± 7.15 min, respectively. Statistically, the difference in T max of VP-16 in presence of Labrasol (5 % w/v) was significant (p < 0.01) when compared to T max of VP-16 solution alone whereas the difference was insignificant (p > 0.05) when compared within Labrasol samples 1 % w/v & 10 % w/v. It was observed that AUC0→250min value of control VP-16 solution was found to be 622.12 ± 14.77 ng × min/mL where as AUC0→250min values in presence of Labrasol were found to be 1121.02 ± 55.09, 1934.32 ± 116.65, and 1011.51 ± 216.84 ng × min/mL, at 1, 5 and 10 % (w/v) concentration, respectively. All the values of VP-16 when co-administered with Labrasol were significant (p < 0.01) as compared to VP-16 alone. The relative bioavailability of VP-16 in presence of Labrasol solution was found to be 180.19, 310.92 (p < 0.01) and 162.59 % at three different tested concentration (1, 5 and 10 %, w/v), respectively, compared to that of VP-16 alone (Eq. 4).
4 Discussion
Intestinal drug efflux by P-gp is widely recognized as a major determinant for the low or variable oral absorption of several structurally unrelated drugs. The P-gp substrate drugs are challenging with regard to their solubility and permeability and in particular the need to enhance their bioavailability. The poor solubility of such drugs does not only give low oral bioavailability, but also leads to inter- and intra-subject variability and lack of dose proportionality [23]. The selected excipients used in this study were reported as solubilizing agents for lipophilic candidates as well as permeation enhancers in emulsifying formulations [3–5, 10]. The solubility of VP-16 was improved in the presence of selected pharmaceutical excipients and the maximum solubility was found to be in Solutol HS 15, Transcutol-P and Labrasol. These three excipients having excellent P-gp inhibitory properties were further selected for in vitro and in vivo studies. The permeability of VP-16 was investigated by bidirectional transport studies across rat ileum. The Papp value for VP-16 drug solution from S → M was higher than that of the M → S value, which indicates that VP-16 is a substrate of P-gp. The results suggested that P-gp efflux mechanisms are involved in limiting VP-16 absorption. The functional P-gp transporters in the apical membrane of the intestine secrete intracellular VP-16 back into the mucosal chamber, which retards the drug permeation in the absorptive direction but facilitates drug transport in the secretory direction, with the consequence that VP-16 exhibits an ER of 4.08. In contrast to this, verapamil, a positive control for P-gp inhibition, suppressed the secretion of VP-16 resulting into increased M → S flux and decreased S → M flux, thereby equalizing the Papp in both directions and maintain the ER 1.38 (≤2). This result indicated that inhibition of P-gp induced by verapamil can markedly enhance the intestinal transportation and permeability of VP-16, and subsequently increase its bioavailability. The apparent permeability coefficients of VP-16 micellar solution with Solutol HS 15, Labrasol and Transcutol-P were compared with that of VP-16 solution across the everted intestinal segment are depicted in Table 1. It was observed, that all selected concentrations of selected excipients might inhibit the function of P-gp in rat ileum, thereby increasing intestinal absorption. Labrasol considerably increased M → S transport and decreased S → M transport of VP-16 solution when compared with Transcutol-P and Solutol HS 15 over the concentration range of (0.1 to 1.0 % w/v). Transcutol-P showed the good inhibitory effect on the function of P-gp, while Solutol HS 15 had found some inhibitory action on this function. Based on our findings, Labrasol was found to have the strongest inhibitory effect on P-gp efflux function among other pharmaceutical excipients used in this study. It was reported basolateral-to-apical efflux inhibition by Labrasol was responsible for permeation enhancement of a poorly permeable drug, ganciclovir [24]. Although multiple mechanisms are undoubtedly responsible for the mechanism of permeability transport of P-gp substrates via excipients, this may partially involve the modulating of the membrane lipid fluidity or passive transport via both a paracellular and a transcellular pathway [25, 26]. This approach of investigating potential P-gp-mediated drug efflux clearly revealed that these excipients have a P-gp inhibitory role as it interacts with P-gp and blocks the efflux transport process. Thus, a thorough understanding of P-gp is important to have an opportunity to improve the bioavailability of drugs restricted by P-gp. A remarkable increase in the plasma concentrations of VP-16 was observed when VP-16 was co-administered with Labrasol at 1-10 % (w/v) concentration. The presence of Labrasol at 5 % (w/v) significantly increased the AUC0→250min, C max and significantly reduced (p < 0.01) the T max of orally administered VP-16. The relative bioavailability after oral administration of VP-16 was enhanced 1.80 fold, 3.10 fold and 1.62 fold, when co-administered with Labrasol at three different concentrations (1, 5 and 10 % w/v), respectively. The C max and AUC0→250min of VP-16 were highest when Labrasol was co-administered at 5 % w/v concentration. The results suggest that enhancements of oral absorption of VP-16 by Labrasol are probably due to inhibition of P-gp-mediated drug efflux. Sha et al. [27] reported that oral bioavailability of gentamycin in rats was significantly enhanced when it was co-administered with Labrasol. The study of Akhtar et al. [3] concluded that the improved oral bioavailability of VP-16 in the presence of surfactant could be explained by the significantly improved solubility of VP-16 by surfactant solubilization which could keep the drug as the soluble form during the gastrointestinal permeation process, and the inhibition of P-gp efflux of VP-16 by solution surfactants. Hence, feasibility of oral administration of VP-16 with P-gp inhibitory excipients was considerably improved. However, more clinical data are necessary to explore feasibility of pharmaceutical excipients and overcome the bioavailability problems of P-gp restricted drugs.
5 Conclusions
The results presented the investigation of chemosensitizing effect of pharmaceutical excipients to attain effective plasma concentrations and to improve in vivo pharmacokinetic profile of VP-16. The challenges associated for anticancer drugs associated with P-gp substrate include the selection of right excipients with consideration of their solubilizing capacity, miscibility, efflux activity and stability in the GI tract. The research showed that the enhanced rate and extent of drug absorption using pharmaceutical excipients, lead to identify suitable vehicles to improve the solubility and permeability of VP-16. The observed data indicated that the pharmaceutical excipients could be used as a chemosensitizer for P-gp substrate agents with the advantages of increasing the intestinal absorption of drugs secreted by a P-gp-mediated efflux resulting in enhanced oral bioavailability. Due to their excellent role in development of drug delivery systems, such chemosensitizers offer a promising approach to improve the oral availability of such clinically important drugs.
References
Toffoli G, Corona G, Basso B, Boiocchi M. Pharmacokinetic optimisation of treatment with oral etoposide. Clin Pharmacokinet. 2004;43(7):441–66.
Lagas JS, Fan L, Wagenaar E, Vlaming ML, van Tellingen O, Beijnen JH, et al. P-glycoprotein (P-gp/Abcb1), Abcc2, and Abcc3 determine the pharmacokinetics of etoposide. Clin Cancer Res. 2010;16(1):130–40.
Akhtar N, Talegaonkar S, Khar RK, Jaggi M. Self-nanoemulsifying lipid carrier system for enhancement of oral bioavailability of etoposide by P-glycoprotein modulation: in vitro cell line and in vivo pharmacokinetic investigation. J Biomed Nanotechnol. 2013;9(7):1216–29.
Bansal T, Akhtar N, Jaggi M, Khar RK, Talegaonkar S. Novel formulation approaches for optimising delivery of anticancer drugs based on P-glycoprotein modulation. Drug Discov Today. 2009;14(21–22):1067–74.
Varma MV, Ashokraj Y, Dey CS, Panchagnula R. P-glycoprotein inhibitors and their screening: a perspective from bioavailability enhancement. Pharmacol Res. 2003;48(4):347–59.
Wempe MF, Wright C, Little JL, Lightner JW, Large SE, Caflisch GB, et al. Inhibiting efflux with novel non-ionic surfactants: rational design based on vitamin E TPGS. Int J Pharm. 2009;370(1–2):93–102.
Chen ML. Lipid excipients and delivery systems for pharmaceutical development: a regulatory perspective. Adv Drug Deliv Rev. 2008;60(6):768–77.
Riehm H, Biedler JL. Potentiation of drug effect by Tween 80 in Chinese hamster cells resistant to actinomycin D and daunomycin. Cancer Res. 1972;32(6):1195–200.
Woodcock DM, Linsenmeyer ME, Chojnowski G, Kriegler AB, Nink V, Webster LK, et al. Reversal of multidrug resistance by surfactants. Br J Cancer. 1992;66(1):62–8.
Akhtar N, Ahad A, Khar RK, Jaggi M, Aqil M, Iqbal Z, et al. The emerging role of P-glycoprotein inhibitors in drug delivery: a patent review. Expert Opin Ther Pat. 2011;21(4):561–76.
Constantinides PP, Wasan KM. Lipid formulation strategies for enhancing intestinal transport and absorption of P-glycoprotein (P-gp) substrate drugs: in vitro/in vivo case studies. J Pharm Sci. 2007;96(2):235–48.
Cornaire G, Woodley J, Hermann P, Cloarec A, Arellano C, Houin G. Impact of excipients on the absorption of P-glycoprotein substrates in vitro and in vivo. Int J Pharm. 2004;278(1):119–31.
Parsa A, Saadati R, Abbasian Z, Azad Aramaki S, Dadashzadeh S. Enhanced permeability of etoposide across everted sacs of rat small intestine by vitamin E-TPGS. Iran. J Pharm Res. 2013;12(Suppl):37–46.
Rege BD, Kao JP, Polli JE. Effects of nonionic surfactants on membrane transporters in Caco-2 cell monolayers. Eur J Pharm Sci. 2002;16(4–5):237–46.
Tayrouz Y, Ding R, Burhenne J, Riedel KD, Weiss J, Hoppe-Tichy T, et al. Pharmacokinetic and pharmaceutic interaction between digoxin and Cremophor RH40. Clin Pharmacol Ther. 2003;73(5):397–405.
Lo YL. Relationships between the hydrophilic-lipophilic balance values of pharmaceutical excipients and their multidrug resistance modulating effect in Caco-2 cells and rat intestines. J Control Releas. 2003;90(1):37–48.
Dabholkar RD, Sawant RM, Mongayt DA, Devarajan PV, Torchilin VP. Polyethylene glycol-phosphatidylethanolamine conjugate (PEG-PE)-based mixed micelles: some properties, loading with paclitaxel, and modulation of P-glycoprotein-mediated efflux. Int J Pharm. 2006;315(1–2):148–57.
Zhu S, Huang R, Hong M, Jiang Y, Hu Z, Liu C, et al. Effects of polyoxyethylene (40) stearate on the activity of P-glycoprotein and cytochrome P450. Eur J Pharm Sci. 2009;37(5):573–80.
Akhtar N, Talegaonkar S, Khar RK, Jaggi M. A validated stability-indicating LC method for estimation of etoposide in bulk and optimized self-nano emulsifying formulation: kinetics and stability effects. Saudi Pharm J. 2013;21(1):103–11.
Akhtar N, Talegaonkar S, Ahad A, Khar RK. Potential of a novel self nanoemulsifying carrier system to overcome P-glycoprotein mediated efflux of etoposide: In vitro and ex vivo investigations. J Drug Deliv Sci Technol. 2015;28:18–27
Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. Faseb J. 2008;22(3):659–61.
Freireich EJ, Gehan EA, Rall DP, Schmidt LH, Skipper HE. Quantitative comparison of toxicity of anticancer agents in mouse, rat, hamster, dog, monkey, and man. Cancer Chemother Rep. 1966;50(4):219–44.
Wacher VJ, Salphati L, Benet LZ. Active secretion and enterocytic drug metabolism barriers to drug absorption. Adv Drug Deliv Rev. 2001;46(1–3):89–102.
Shen Y, Lu Y, Jv M, Hu J, Li Q, Tu J. Enhancing effect of Labrasol on the intestinal absorption of ganciclovir in rats. Drug Dev Ind Pharm. 2011;37(12):1415–21.
Lin Y, Shen Q, Katsumi H, Okada N, Fujita T, Jiang X, et al. Effects of Labrasol and other pharmaceutical excipients on the intestinal transport and absorption of rhodamine123, a P-glycoprotein substrate, in rats. Biol Pharm Bull. 2007;30(7):1301–7.
Reddy LH, Sharma RK, Murthy RR. Enhanced delivery of etoposide to Dalton’s lymphoma in mice through polysorbate 20 micelles. Acta Pharm. 2006;56(2):143–55.
Sha X, Yan G, Wu Y, Li J, Fang X. Effect of self-microemulsifying drug delivery systems containing Labrasol on tight junctions in Caco-2 cells. Eur J Pharm Sci. 2005;24(5):477–86.
Acknowledgments
Author is grateful to the Jamia Hamdard (Hamdard University) for providing facility to carry out this project. Author is also grateful to the Dabur India Limited, Sahibabad, India for providing gift sample of VP-16.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding source
Naseem Akhtar would like to thank University Grants Commission (UGC), New Delhi, India for financial assistance in the form of Senior Research Fellowship (10-13/2006, SA-I).
Conflict of interest
NA, AA, MFK, AA and ST declare no conflict of interest.
Ethical approval
All animal studies were conducted according to the guidelines of the Institutional Animal Ethics Committee, Jamia Hamdard (Hamdard University), New Delhi, India.
Rights and permissions
About this article
Cite this article
Akhtar, N., Ahad, A., Khan, M.F. et al. The Ameliorated Pharmacokinetics of VP-16 in Wistar Rats: A Possible Role of P-Glycoprotein Inhibition by Pharmaceutical Excipients. Eur J Drug Metab Pharmacokinet 42, 191–199 (2017). https://doi.org/10.1007/s13318-016-0332-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-016-0332-7