Abstract
Despite growing interest in gasless endoscopic unilateral thyroid lobectomy via the axillary approach, there are a lack of sufficient data on its safety and cosmetic outcomes. This retrospective study analysed the clinical outcomes and postoperative complications of 161 patients who underwent this surgery for thyroid cancer and nodules, with particular attention given to complications and patient satisfaction with cosmetic outcomes. All 161 patients (143 females, 18 males) successfully underwent the operation without conversion to open surgery. Temporary vocal cord paralysis occurred in five patients, with no other serious complications observed. The cosmetic outcomes were generally good, with no recurrences or tumour implantations observed during follow-up. For carefully selected patients, gasless endoscopic unilateral thyroid lobectomy via the axillary approach is not only safe but also provides excellent cosmetic results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With continuous advancements in medical diagnostic technologies, the detection rate of thyroid diseases, particularly thyroid cancer, has been increasing [1]. In 2020, thyroid cancer accounted for 3% of all newly diagnosed cancers and 0.4% of all cancer deaths [2], making it the 11th most common cancer and the 5th most common cancer among women, who are three to four times more likely to develop the disease than men are [3]. Papillary thyroid carcinoma is the most common type of thyroid cancer, and surgical intervention remains the preferred treatment method. Although the conventional collar incision is highly effective, the resulting visible scars can significantly impact the psychological and aesthetic well-being of patients [4,5,6]. This issue has driven the medical community to explore new surgical approaches that are both safe and meet patients’ aesthetic needs. In 2006, Chung et al. from Korea first reported the use of a gasless axillary approach for endoscopic unilateral thyroid lobectomy, offering a new perspective in the field. Subsequent enhancements by Tae et al. refined the surgical procedures and technical details. Kang et al. improved the safety and feasibility of surgery by employing a gasless endoscopic technique, effectively reducing complications potentially caused by CO2 insufflation [6,7,8]. Although the da Vinci robotic system® offers a high-tech option for unilateral thyroid lobectomy, its high cost and long operation time limit its widespread use. Therefore, the gasless endoscopic approach without robotic assistance has significant advantages in terms of cost-effectiveness and operation duration [9,10,11,12].
This study was a retrospective analysis of 161 patients who underwent gasless endoscopic unilateral thyroid lobectomy via the axillary approach, aiming to assess the feasibility, safety, and cosmetic outcomes of this surgical method. By meticulously recording various medical metrics and patient feedback during surgery, we strive to provide a comprehensive assessment to guide future clinical practices and optimize surgical techniques. Additionally, by analysing postoperative complications in detail, this study also aimed to explore how to further minimize surgical risks [13], thereby enhancing overall treatment outcomes and patient satisfaction.
Materials and methods
Patient enrolment
This retrospective study included patients who underwent unilateral thyroid lobectomy via the axillary approach at Yancheng First People’s Hospital between March 2021 and December 2023 and patients who were diagnosed with thyroid cancer or nodules exceeding 2 cm in diameter. The inclusion criteria were as follows: patients diagnosed with papillary thyroid carcinoma (PTC) via ultrasound-guided fine needle aspiration (FNA); patients with PTC diagnosed with negative central lymph nodes according to two professional ultrasonographers; patients with unilateral Bethesda category IV nodules exceeding 2 cm (indicating indeterminate cytology); and patients with unilateral Bethesda category III nodules exceeding 4 cm. The exclusion criteria were as follows: patients with benign nodules exceeding 6 cm in diameter, patients requiring total thyroidectomy, and patients unsuitable for endoscopic surgery due to previous neck or chest wall surgeries. A total of 161 patients (72 with PTC and 89 with thyroid adenomas) were included in the study.
Surgical equipment
The equipment consisted of an inverted "L" shaped bracket, a connector, and a "U" shaped hook with a suction tube at the front end bent at 30 degrees (Hangzhou Kangji Medical Instrument Co., China) (Fig. 1-1, 1-2). The arrangement of the instruments used during the surgery is shown in Fig. 2.
Surgical procedure
-
1.
Position and incision
After general anaesthesia, the patient was placed in a supine position with the ipsilateral arm extended to 90 degrees (Fig. 3). A 5-cm incision was made behind the anterior axillary fold, and laparoscopic instruments, including a rigid 30-degree videoscope, were used. Retractors were used to maintain the surgical space. An additional 5-mm auxiliary incision was made vertically above the axillary incision (3–5 cm from the incision) for the placement of a 5-mm trocar.
-
2.
Establishing the surgical space
The area between the sternal and clavicular heads of the sternocleidomastoid muscle was delineated, extending from the cricoid cartilage to the clavicle. The sternal head of the sternocleidomastoid was retracted upwards to expose the omohyoid muscle; the omohyoid and internal jugular veins were dissected laterally, and the retractors were placed under the omohyoid (Fig. 4-1, 4-2).
Key points:
-
a.
The pectoral fascia should be preserved as much as possible during dissection to reduce mechanical friction and postoperative bleeding.
-
b.
The external jugular vein and the supraclavicular nerve were protected, avoiding damage.
-
3.
Unilateral thyroid lobectomy
After the omohyoid muscle was retracted from the ventral side of the thyroid, preliminary lateral dissection of the thyroid was performed. The middle thyroid vein was ligated and severed, exposing the lateral margin of the common carotid artery. The lower parathyroid glands were identified and preserved in situ. Blunt dissection of the tracheoesophageal groove was performed to expose the recurrent laryngeal nerve (Fig. 5). Using nerve monitoring, the nerve was identified, and the inferior thyroid artery and vein were ligated and severed. The thyroid isthmus was cut along the surface of the trachea, thereby freeing the superior medial space between the thyroid and the cricothyroid muscle. After exposing the superior laryngeal nerve and the upper parathyroid glands, the superior thyroid vessels were ligated, and the Berry ligament was removed before complete removal of the thyroid lobe. The thyroid tumours were marked and sent for frozen section analysis.
Key Points:
-
a.
Due to the heat conduction of the harmonic scalpel, ensure that it is kept at least 3 mm from the recurrent laryngeal nerve, and use it for no more than 3 s at a time to minimize thermal damage to the nerve. A nerve monitor was used to assess the condition of the recurrent laryngeal nerve.
-
b.
When the recurrent laryngeal nerve was bluntly exposed, preoperative CT imaging was used to confirm the presence of the brachiocephalic trunk; the nonrecurrent laryngeal nerve was considered if it was absent.
-
c.
If fat, lymph nodes, or parathyroid glands could not be distinguished during surgery, a portion of the tissue was removed for intraoperative frozen section analysis.
-
d.
The Berry ligament is dense, and careful haemostasis is required after its division.
-
4.
Central Neck Dissection (CND)
If frozen section analysis indicated malignancy, central neck dissection was performed. The boundaries for central neck dissection include the cricoid cartilage as the upper boundary, the common carotid artery laterally, the superficial layer of the deep cervical fascia anteriorly, and the superior sternal notch inferiorly. The medial boundary is the outer edge of the contralateral thyroid gland at the trachea. Dissection starts along the superficial layer of the deep cervical fascia, beginning deep to the recurrent laryngeal nerve, followed by lymph nodes lateral or medial to the nerve. Finally, the pretracheal lymph nodes along the surface of the trachea are dissected up to the contralateral border of the sternothyroid muscle at the trachea and eventually separated from the thymus (Fig. 6).
-
5.
Specimen Removal and Wound Closure
The specimen was removed using sterile gloves, a drainage tube was placed at the lowest point, and the wound was closed with intradermal sutures using 4–0 absorbable stitches (Fig. 7), similar to other endoscopic and open surgical methods. The surgical techniques used in this study are consistent with those reported by other surgical teams [14,15,16,17].
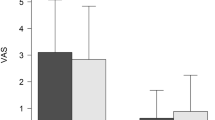
The patients were followed up with a retrospective review of their medical records, with follow-up periods ranging from 3 to 36 months. A specially designed questionnaire focused on cosmetic satisfaction was used to survey the quality of life of the included patients (Supplement Table). To specifically evaluate the cosmetic outcomes of the surgery, the Neck Appearance Score (Patient Satisfaction Score, PSS) was used, with the following scoring criteria: 1 (very satisfied), 2 (satisfied), 3 (dissatisfied), and 4 (very dissatisfied) [13].
Statistical analysis
All continuous variables were represented by mean ± standard deviation (SD) and range. All categorical variables were represented as percentages.
Results
Between March 2021 and December 2023, a total of 161 patients (143 females and 18 males) underwent gasless endoscopic surgery via the axillary approach, all without conversion to open surgery. These patients ranged in age from 17 to 77 years, with an average age of 43.6 years. Eighty-nine of these patients underwent thyroid lobectomy for solitary or cystic thyroid adenomas. Fine needle aspiration cytology (FNAC) revealed malignant nodules in 72 patients who then underwent thyroid lobectomy and prophylactic unilateral central neck dissection. The average diameter of the benign tumours was 37 mm (range 26–49 mm), and the average diameter of malignant tumours was 12.0 mm (range 9–21 mm). The average surgery time for thyroid lobectomy and prophylactic central neck dissection was 86.3 ± 18.1 min, while the average surgery time for unilateral thyroid lobectomy was 70.9 ± 15.1 min. The average blood loss was 29.0 ± 17.8 ml. The average drainage volumes were 35.0 ± 10.4 ml on the first day, 27.6 ± 5.6 ml on the second day, and 12.7 ± 3.2 ml on the third day (Table 1). In all patients, the drainage tubes were removed on the third postoperative day. The average number of prophylactically removed central neck lymph nodes was 3.95 ± 2.2. The recurrent laryngeal nerve was clearly identified and preserved in all patients. Only 5 patients experienced temporary vocal cord paralysis, with no cases of permanent vocal cord paralysis. Additionally, 3 patients experienced temporary hypoparathyroidism postoperatively and received intravenous calcium treatment; 3 patients developed subcutaneous seromas, which were treated by syringe aspiration; and 1 patient experienced postoperative bleeding at the incision site, which was managed with pressure dressing (Table 2). The median hospital stay for patients was 3.1 ± 0.35 days (range 1–7 days). In terms of the incision satisfaction scores, the average score for the 161 patients was 3.6 ± 1.7, for scar awareness, the average score was 2.0 ± 1.3 and for Vancouver scar scale, the average score was 2.5 ± 1.8. The specific scoring details are shown in Table 3.
Discussion
Over the past decade, as endoscopic technology has rapidly evolved, an increasing number of thyroid surgeons have begun exploring the use of endoscopic thyroidectomy to reduce the scarring caused by traditional surgery [18]. In this study, 161 patients successfully underwent gasless endoscopic unilateral thyroid lobectomy via the axillary approach. We observed few complications, with only 5 cases of temporary vocal cord paralysis. Additionally, 3 patients experienced temporary hypoparathyroidism, 3 developed subcutaneous seromas, and 1 experienced postoperative bleeding, but no other serious common postoperative complications occurred. Although the specific number of parathyroid glands was not statistically significant, we believe that with increased experience, the recognition and preservation of parathyroid glands will improve. Studies by Lee et al. have shown that axillary thyroidectomy not only is related to better cosmetic outcomes but also may lead to longer surgery times, voice changes, sensory abnormalities, and altered swallowing functions [19]. Research on robot-assisted gasless axillary thyroidectomy by Piccoli et al. also demonstrated the feasibility and safety of the surgery, with only a very few patients (0.45%) requiring conversion to traditional methods and no reported injuries to the internal jugular vein [13]. Although these studies demonstrate the potential of the technique, a consensus on its clinical application has not yet been reached, mainly due to the variability in complication rates.
In addition to the usual complications, Leonardo Rossi et al. reported that robot-assisted gasless axillary thyroidectomy can also result in unconventional complications such as brachial plexus nerve damage, implant metastasis, seroma, and skin flap perforation [20]. It is generally believed that brachial plexus nerve damage is mainly due to extreme arm extension; thus, special attention is needed during the positioning phase. The patient’s ipsilateral arm was extended at the shoulder, flexed at the elbow, and fixed on an elevated pad to reduce the occurrence of this complication. Considering that all conventional specimen removals follow a "no-touch" principle, the cause of implant metastasis is mainly due to the endoscope being contaminated with shed cells during operation, which mechanically rub against muscles such as the pectoral muscle, and some tumour cells fall off. Additionally, highly vascularized muscle provides a growth-promoting environment for shed cells. Due to extensive subcutaneous dissection from the axilla to the neck, theoretically, there is a higher possibility of forming a seroma. In previous studies, the incidence rate was approximately 2%, while in this study, there were 3 cases of subcutaneous fluid, thus yielding an incidence rate of 1.9%, which is roughly equivalent to the literature rate. Skin flap perforation occurs because the skin near the clavicle is thinner; therefore, more caution is required when dissecting this area to prevent this complication. During the limited follow-up period, we did not observe any recurrence, and patients generally expressed satisfaction or high satisfaction with the cosmetic outcomes of the surgery. Although the axillary approach causes additional trauma, it still has certain application value under appropriate circumstances. However, a clear disadvantage of this technique is the difficulty in locating the contralateral thyroid lobe, thus limiting its use in bilateral total thyroidectomy. The surgical objectives can be achieved by cutting the sternohyoid muscle, which may increase surgery time, neck pain, and swallowing discomfort. Compared to traditional two-dimensional endoscopic surgery, three-dimensional endoscopic surgery has been proven to be an effective, safe, and reliable method due to its superior depth perception and stereoscopic vision, and the surgical outcomes are equally satisfactory [21]. Good postoperative cosmetic results are a major advantage of laparoscopic thyroidectomy. Many studies have reported good cosmetic outcomes for endoscopic thyroidectomy, but most studies have assessed only short-term subjective cosmetic satisfaction. In this study, we used modified scar scores and the Vancouver scar scale, which are known to help reduce scarring. Fine surgical techniques, including aseptic operation, avoiding tension, precise alignment, avoiding rough surfaces, and atraumatic tissue handling (5A principles) [22], are important. Surgeons need to carefully handle the incision edges to minimize trauma. Especially in the axillary and subaxillary areas, forceful pulling should be avoided to prevent the formation of unsightly scars. Although this study Leonardo provides valuable insights, it has some limitations, mainly due to the inherent flaws of retrospective studies. The limitations of this paper mainly include the following. 1. Patients were mainly recruited from Yancheng First People’s Hospital, which prevents the results from being generalised to the entire target population. 2. Retrospective analyses mainly depend on past medical records, and errors in data entry or missing information may affect the results. 3. The validity of the cosmetic questionnaires was unclear.
Previous studies have shown that despite the challenges of learning curves and equipment costs, axillary gasless endoscopic thyroidectomy is of significant clinical importance for reducing neck scarring, improving patient satisfaction, reducing postoperative complications, and accelerating postoperative recovery. Our study revealed that gasless endoscopic thyroidectomy via the axillary approach is a viable surgical option, providing acceptable safety and excellent cosmetic outcomes for strictly selected patients. Future studies need to further investigate and verify the cosmetic effects and oncological outcomes of this surgical technique through prospective clinical research. Additionally, in-depth study of the learning curve for this technique is also necessary. Although gasless endoscopic thyroidectomy via the axillary approach requires a certain amount of equipment, it is more economically valuable than robotic endoscopic thyroidectomy via the axillary approach.
Conclusion
In a carefully selected patient cohort, gasless endoscopic unilateral thyroid lobectomy via the axillary approach not only demonstrated good feasibility but also demonstrated high safety and significant cosmetic advantages. This surgical method offers an effective treatment option for patients with thyroid diseases, as it balances therapeutic effectiveness and aesthetic needs.
Data availability
The data that support the findings of this study are derived from anonymized questionnaires. Due to the sensitive nature of the information and privacy protections, the data are not publicly available.
References
Nabhan F, Ringel MD (2017) Thyroid nodules and cancer management guidelines: comparisons and controversies. Endocr Relat Cancer 24(2):R13-r26. https://doi.org/10.1530/erc-16-0432
Sung H et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
Messina G et al (2023) Experimental study on physical exercise in diabetes: pathophysiology and therapeutic effects. Eur J Transl Myol. https://doi.org/10.4081/ejtm.2023.11560
Chen GZ et al (2012) Systematic comparison of cervical and extra-cervical surgical approaches for endoscopic thyroidectomy. Surg Today 42(9):835–841. https://doi.org/10.1007/s00595-011-0100-x
Mitchem JB, Gillanders WE (2013) Endoscopic and robotic thyroidectomy for cancer. Surg Oncol Clin N Am. 22(1):1–13. https://doi.org/10.1016/j.soc.2012.08.009
Duncan TD et al (2006) Endoscopic transaxillary near total thyroidectomy. Jsls 10(2):206–11
Kang SW et al (2009) Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery 146(6):1048–1055. https://doi.org/10.1016/j.surg.2009.09.007
Tae K et al (2019) Robotic and endoscopic thyroid surgery: evolution and advances. Clin Exp Otorhinolaryngol 12(1):1–11. https://doi.org/10.21053/ceo.2018.00766
Lang BH, Chow MP (2011) A comparison of surgical outcomes between endoscopic and robotically assisted thyroidectomy: the authors’ initial experience. Surg Endosc 25(5):1617–1623. https://doi.org/10.1007/s00464-010-1450-y
Kang SW et al (2009) Gasless endoscopic thyroidectomy using trans-axillary approach; surgical outcome of 581 patients. Endocr J 56(3):361–369. https://doi.org/10.1507/endocrj.k08e-306
Jantharapattana K, Maethasith J (2017) Transaxillary gasless endoscopic thyroidectomy versus conventional open thyroidectomy: a randomized study. Eur Arch Otorhinolaryngol 274(1):495–500. https://doi.org/10.1007/s00405-016-4242-8
Johri G et al (2020) Endoscopic versus conventional thyroid surgery: a comparison of quality of life, cosmetic outcomes and overall patient satisfaction with treatment. World J Surg 44(12):4118–4126. https://doi.org/10.1007/s00268-020-05732-7
Lee DW et al (2020) Comparison of postoperative cosmesis in transaxillary, postauricular facelift, and conventional transcervical thyroidectomy. Surg Endosc 34(8):3388–3397. https://doi.org/10.1007/s00464-019-07113-1
Cong R et al (2022) Gasless, endoscopic trans-axillary thyroid surgery: our series of the first 51 human cases. World J Surg Oncol 20(1):9. https://doi.org/10.1186/s12957-021-02484-z
Dhoomun DK et al (2023) Comparison of health-related quality of life and cosmetic outcome between traditional gasless trans-axillary endoscopic thyroidectomy and modified gasless trans-axillary endoscopic thyroidectomy for patients with papillary thyroid microcarcinoma. Cancer Med 12(15):16604–16614. https://doi.org/10.1002/cam4.6258
Sun B et al (2022) Gasless endoscopic transaxillary thyroid surgery: CUSUM analysis of a single surgeon’s experience from 105 preliminary procedures. Surg Endosc 36(11):8270–8279. https://doi.org/10.1007/s00464-022-09273-z
Xu S et al (2022) Surgical steps of gasless transaxillary endoscopic thyroidectomy: from A to Z. J Oncol 2022:2037400. https://doi.org/10.1155/2022/2037400
Berber E et al (2016) American thyroid association statement on remote-access thyroid surgery. Thyroid 26(3):331–337. https://doi.org/10.1089/thy.2015.0407
Kim SK et al (2016) Routine level 2b dissection may be recommended only in N1b papillary thyroid carcinoma with three- or four-level lateral lymph node metastasis. Ann Surg Oncol 23(Suppl 5):694–700. https://doi.org/10.1245/s10434-016-5521-8
Rossi L et al (2022) Postsurgical complications after robot-assisted transaxillary thyroidectomy: critical analysis of a large cohort of European patients. Updates Surg 74(2):511–517. https://doi.org/10.1007/s13304-022-01244-2
Huang Z et al (2021) Comparison between 3-dimensional and 2-dimensional endoscopic thyroidectomy for benign and malignant lesions: a meta-analysis. World J Surg Oncol 19(1):23. https://doi.org/10.1186/s12957-021-02134-4
Son D, Harijan A (2014) Overview of surgical scar prevention and management. J Korean Med Sci 29(6):751–757. https://doi.org/10.3346/jkms.2014.29.6.751
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no confict of interest.
Ethical approval
This retrospective study was conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Ethical approval was waived by the Institutional Review Board of Yancheng First hospital, due to the non-invasive nature of the study and the use of de-identified patient data.
Informed consent
Informed consent was obtained from all individual participants included in the study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, Y., Zhou, S. & Zhou, G. Safety and cosmesis of gasless endoscopic thyroidectomy: a retrospective study. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01938-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01938-9