Abstract
Living donor liver transplantation (LDLT) has emerged as a favorable alternative to deceased donor liver transplantation, significantly reducing waitlist mortality, particularly in Asian countries with very low deceased organ donation rates. Asan Medical Center (AMC) in South Korea has pioneered innovative LDLT surgical techniques and become established as an extremely high-volume center for LDLT. This retrospective study analyzed 6000 consecutive LDLT procedures, including 510 dual-graft procedures, performed at AMC between December 1994 and January 2021. Of these, 312 LDLT procedures were performed in children aged < 18 years. In adult recipients, liver cirrhosis (LC) related to viral hepatitis was the most common indication, occurring in 69.8% of cases. Biliary atresia (46.8%) was the most common indication for pediatric LDLT. This study demonstrated outstanding long-term outcomes, with patient survival rates at 1, 5, 10, and 20 years of 92.7%, 85.9%, 82.1%, and 70.9%, respectively, in LDLT group for adults aged 50 and under at the time of LDLT, and 92.9%, 89.0%, 88.1%, and 81.9%, respectively, in the pediatric group. The in-hospital mortality rate of adult recipients was 3.8% (n = 214/5688). This study demonstrates the importance of refined surgical techniques, selection of grafts tailored to the recipient, and comprehensive multidisciplinary perioperative patient care in expanding the scope of LDLT and improving recipient outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Living donor liver transplantation (LDLT) is now a practical alternative to deceased donor liver transplantation (DDLT) aimed at overcoming organ shortages and consequently reducing the risk of waitlist mortality [1, 2]. The impact of LDLT has been significantly greater in Asia, where access to donor grafts is limited by the extremely low rate of organ donation from deceased donors, and LDLT has made rapid advances in Asia with favorable outcomes for both donors and recipients, and has become the mainstay of liver transplantation (LT) [3,4,5].
The Asan Medical Center (AMC) LT program was launched in August 1992 with DDLT. In 1994, pediatric LDLT was successfully performed at AMC, representing the first LDLT procedure conducted in South Korea. The adult-to-adult LDLT program using right-lobe grafts was initiated in 1997; however, early results were unsatisfactory as severe graft congestion of the anterior sector led to graft dysfunction. To address congestion problems related to middle hepatic vein drainage, the LDLT procedure was altered to include the modification of right-lobe grafts, which involves reconstructing the middle hepatic vein prior to transplantation [6, 7]. This landmark development has substantially improved recipient outcomes in right-lobe LDLT, ensuring donor safety and providing an innovative solution to the severe shortage of deceased donors in Asian countries.
Extensive experience has resulted in a standardized surgical technique and multidisciplinary perioperative patient management, which has established AMC as an extremely high-volume center responsible for one-third of all LDLT procedures in South Korea. The purpose of the current study was to present the long-term outcomes of 6000 consecutive LDLT procedures performed since the start of the LDLT program in 1994 at our institution and describe the strategies used to select grafts according to the requirements of the recipients, based on our accumulated experience.
Methods
Study population and design
A total of 8128 LT procedures (1356 DDLT and 6772 LDLT) have been performed at AMC, University of Ulsan College of Medicine, Seoul, South Korea, from the first DDLT in August 1992 to December 2022. Since 2010, over 300 LDLT procedures per year have been performed at AMC. Remarkably, even during the 3 years of the coronavirus disease 2019 pandemic, the center conducted 400 LDLT procedures each year, including cases requiring highly complex surgical techniques (Fig. 1).
Data collected from the medical records of the 6000 consecutive patients undergoing LDLT between December 1994 and January 2021 were retrospectively analyzed. An adult recipient was defined as one aged 18 years or older. All LDLT procedures were performed after obtaining approval from the Korean Network for Organ Sharing, affiliated with the Korean Ministry of Health. This study was approved by the Institutional Review Board of AMC (Approval Number 2022–1218) and conducted in accordance with the principles outlined in the Declaration of Helsinki.
Preoperative evaluation and donor and recipient surgical procedures
The preoperative evaluation and surgical procedure performed on the living donor have been described previously [1, 8]. Briefly, after an interview to determine their willingness to donate and confirm the absence of any known conditions that significantly increased perioperative risk or contraindicated donation such as significant hepatic steatosis and insufficient remnant liver volume, extensive serological evaluations and imaging tests were performed to confirm their suitability. Imaging tests included mesenteric Doppler ultrasound, volumetric computed tomography (CT), and magnetic resonance (MR) cholangiography to evaluate liver echogenicity, measure liver size, and assess the vasculobiliary anatomy. Percutaneous liver biopsies were selectively performed on candidate donors with a high body mass index (≥ 30 kg/m2), increased levels of AST, ALT, or total bilirubin, any abnormal findings on CT or US indicating hepatic steatosis, or a family history of hereditary liver diseases [8]. Donor hepatectomy was performed using various approaches, including conventional, mini-incision, hand-assisted laparoscopic, and pure laparoscopic techniques, according to the individual donor. The indications for each surgical technique have been described in detail previously [9,10,11].
The preoperative evaluation and surgical procedure performed on the recipient have been described elsewhere [1, 12]. All LT candidates underwent a comprehensive assessment, including imaging using mesenteric Doppler ultrasound, abdominal and chest contrast-enhanced CT, positron emission tomography-CT, and/or MR. An indirect portogram was selectively performed in recipients with portal vein thrombus. If portal vein obliteration was observed on preoperative CT scans, an indirect portogram through the superior mesenteric artery was selectively performed. In addition, all candidates underwent thorough cardiopulmonary and cerebrovascular screening to evaluate perioperative risks. Our standardized LDLT techniques are based on sufficient portal and arterial inflows, good hepatic vein outflow, and secure bile duct anastomosis [1]. All the most hepatic arterial reconstructions were performed by surgeons skilled in reconstructive microsurgery [13]. Hepaticojejunostomy with a Roux limb was the standard procedure for biliary reconstruction until January 2000. From February 2000, duct-to-duct anastomosis became the preferred technique for biliary reconstruction, along with an external biliary drain, unless biliary liver anastomosis was not technically feasible due to the length or vascularity of the recipient bile duct or the recipient had biliary disease.
Immunosuppression
The immunosuppressive regimen comprised a calcineurin inhibitor (CNI), mycophenolate mofetil, and corticosteroids with anti-interleukin 2 induction, with the dose of CNIs and corticosteroids varying depending on the preoperative condition of the recipient. Everolimus, in combination with a CNI, was administered to recipients at a high risk of hepatocellular carcinoma recurrence.
For recipient and donor pairings with incompatible blood types, recipients underwent rituximab treatment and plasma exchange prior to transplantation. No special drugs or induction regimens other than rituximab were used. The frequency and timing of plasma exchange were determined based on the hemagglutination titer, with the aim of achieving an antibody titer of ≤ 1:8 before LT. A detailed description of the desensitization protocol for ABO-incompatible (ABOi) adult LDLT at our institution has been published previously [14,15,16].
Statistical analyses
Quantitative data are expressed as mean ± standard deviation or median with interquartile range (IQR). Qualitative data are expressed as number and percentage (%). The Kruskal–Wallis test by ranks was used to evaluate the differences between several groups. Graft and patient survival rates were determined using Kaplan–Meier survival analysis, and comparisons between different groups were performed using log-rank tests. P < 0.05 was considered statistically significant.
Results
During the study period of December 1994 to January 2021, 7695 LT procedures were performed at AMC, of which 1695 DDLT procedures were excluded, and 6000 LDLT procedures using grafts from 6570 donors were included in this study. Of these, 312 LT procedures were performed in children aged < 18 years. Figure 1 shows the number of LDLT procedures performed at AMC annually.
Recipient and donor baseline characteristics
The indications for LDLT in adult and pediatric patients are shown in Fig. 2a, b, respectively. In adults, LC related to viral hepatitis, including hepatitis B and C viruses, was the most common indication for liver transplantation, occurring in 69.8% of recipients. This was followed by alcoholic LC (15.0%) and cryptogenic LC (5.0%). Hepatocellular carcinoma was present in 2551 recipients (42.5%). Biliary atresia (46.8%) was the most common indication for liver transplantation in pediatric recipients, followed by fulminant hepatic failure (18.3%).
The demographic and clinical data of the recipients and donors of 6000 LDLT procedures are shown in Table 1. In pediatric LDLT, the 312 recipients had a mean age of 4.2 ± 4.8 years (range: 3 months–17 years). The median pediatric end-stage liver disease score was 19 (IQR: 11–27). The donors were mostly the parents of the recipients, with a mean donor age of 34.4 ± 6.4 (range: 30–50) years. Only 1.9% of donors had a blood type incompatible with that of the recipient. In adult LDLT, the 5688 recipients had a mean age of 52.1 ± 9.0 (range: 18–78) years; 4198 were male and 1490 were female. The median model for end-stage liver disease (MELD) score was 14 (IQR: 10–22). Among the 5688 LDLT procedures, 757 (13.3%) were ABOi and 40 (0.7%) were re-transplantation surgeries. Of the total 6256 donors, there were 34 domino donors. The majority of the donors were the children of the recipients (n = 3631; 70.0%) followed by other close relatives, with a mean donor age of 28.3 ± 8.2 (range: 16–65) years. The mean recipient-to-graft weight ratio (GRWR) was 1.09 ± 0.24, and the mean graft volume (GV)/standard liver volume (SLV) ratio was 60.3 ± 11.1%. In adult LDLT, right-lobe grafts were the most commonly procured (n = 4853; 85.3%). In cases of dual grafts (DG), the left lobe/left lobe or left lateral segment graft combination was the most commonly used (n = 332; 58.2%). The demographic and clinical data of the recipients and donors of the 5688 adult LDLT procedures are presented according to graft type in Table 2.
Operative outcomes of adult LDLT according to graft type
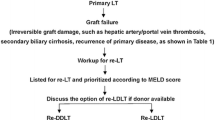
Intraoperative and postoperative data from the 5688 adult LDLT procedures, classified by graft type, are presented in Table 2. The mean red blood cell transfusion requirement was highest in the DG group, with 14 (IQR: 8–26) units needed (P < 0.0001). In addition, the mean operative duration was the longest in the DG group, at 1068 (IQR: 961–1176) min (P < 0.0001). In contrast, the mean postoperative hospital stay was longest in the single left graft group, at 38 (IQR: 28–55) days (P < 0.0001). The incidence of biliary complications including stricture and leak was 19.0% in the single right graft group, 26.1% in the single left graft group, and 30.7% in the DG group (P < 0.0001). Hepatic artery-related complications such as dissection and thrombosis occurred in 3.0% of cases in the single right graft group, 5.1% in the single left graft group, and 3.6% in the DG group (P = 0.057). In the single left graft group, 21 of 253 (8.3%) cases required re-transplantation due to graft failure after transplantation, compared with 242 of 4865 (5.0%) cases in the single right graft group and 29 of 570 (5.1%) cases in the DG group (P = 0.065). In addition, in-hospital mortality was the highest in the DG group at 7.0% and lowest in the right graft group at 3.0% (P < 0.0001).
Patient survival
The patient survival rates at 1, 5, 10, and 20 years of 92.7%, 85.9%, 82.1%, and 70.9%, respectively, for adult recipients aged 50 and under, and 92.8%, 83.2%, 76.7%, and 60.1%, respectively, in adult recipients over 50 years of age. In addition, the patient survival rates at 1, 5, 10, and 20 years were 92.9%, 89.0%, 88.1%, and 81.9%, respectively, for pediatric recipients (P < 0.0001) (Fig. 3a). When patient survival was compared based on the MELD/PELD score, as depicted in Fig. 3b, the group with a MELD score of 31–40 showed the lowest survival rates (P < 0.0001), being 82.9%, 76.8%, 72.7%, and 59.4% at 1, 5, 10, and 20 years, respectively. There were no statistically significant differences between ABOi and ABO-compatible LDLT groups, with 1-, 5-, and 10-year survival rates of 92.5%, 84.5%, and 79.5%, respectively, in the ABO-compatible group, and 94.9%, 84.1%, and 78.8%, respectively, in the ABOi group (P = 0.9958; Fig. 3c). The patient survival rates of the re-transplantation group were significantly lower than those of the primary LDLT group, with 1-, 5-, 10-, and 20 year survival rates of 77.2%, 64.5%, 61.0%, and 40.6%, respectively (Fig. 3d). When patient survival was compared according to graft type (single graft versus DG), as shown in Fig. 3e, the DG group showed lower survival rates of 90.0%, 82.0%, 76.0%, and 64.7% compared with 93.1%, 84.8%, 79.8%, and 66.7% for the single-graft group at 1, 5, 10, and 20 years, respectively (P = 0.0571).
Overall patient survival rates of LDLT recipients according to a Age (adult versus pediatrics) b MELD score, c ABO incompatibility, d LT type (re-transplantation versus primary transplantation) and e graft type (Single versus Dual graft). LDLT living donor liver transplantation, LT liver transplantation, MELD model for end-stage liver disease
Discussion
This study represents the most extensive report of LDLT with the longest follow-up period, conducted at a leading Asian center that has pioneered innovative surgical techniques [7, 17,18,19]. Our study demonstrated outstanding LDLT outcomes, with 10 year overall patient survival rates of 88.1% and 82.1%, and 20-year overall patient survival rates of 81.9% and 70.9% in children and adults aged 50 and under, respectively. The in-hospital mortality rate among adult recipients undergoing LDLT was 3.8% (n = 214/5688), and was even relatively low in patients with increased MELD scores: 0.8% (n = 14/1701) for scores up to 10, 2.2% (n = 51/2340) for scores of 11–20, 7.2% (n = 72/1002) for scores of 21–30, and 11.9% (n = 77/645) for scores of 31–40. These results include the poor outcomes observed in the early stages of the LDLT program; in-hospital mortality has improved over time [7] to 2.3% (27/1163), despite the coronavirus disease 2019 pandemic. In 2017, our institution achieved an extraordinary 0% in-hospital mortality in 361 LDLTs. These findings confirm the effectiveness and safety of LDLT in prolonging the survival of patients with end-stage liver disease without relying on organs from deceased donors.
Over the past 20 years, the success of LDLT has led to an expansion in the eligibility criteria for recipients. Patients previously considered high-risk owing to factors such as advanced age, ultra-high MELD scores, or comorbidities are now considered candidates for LDLT [20]. Furthermore, traditional donor selection criteria are being challenged and broadened, while balancing donor safety with recipient and graft survival [21]. Prioritizing donor safety and selecting the appropriate graft for each recipient are fundamental considerations in LDLT. Several centers have demonstrated the need for careful donor selection for older recipients, who are increasingly undergoing LDLT [22, 23]. We have previously proposed a GV of > 1.0% of the GRWR or > 50% of the GV/SLV from a donor aged ≤ 35 years as the ideal graft for patients aged ≥ 70 years [12]. For severely ill patients with high MELD scores, our center prefers using a graft with a GRWR close to 1.0, young donor age, and simple graft anatomy to provide sufficient volume to meet metabolic requirements and minimize the risk of complications. These strict graft selection criteria have contributed greatly to the excellent results of LDLT observed in our high-risk recipients.
However, as the availability of grafts is frequently limited, even from living donors, it can be challenging to secure an ideal graft in every case. At our institution, dual and ABOi grafts have been actively utilized in adult LDLT to expand the donor pool [7]. DG LDLT, which was first introduced in the form of “two left-lobes” in 2000 [24], has been performed with various graft combinations, as detailed in Table 2, depending on recipient and donor factors. This has allowed the utilization of grafts from older donors and those with severe steatosis, significantly reducing donor risk and minimizing the risk of small-for-size syndrome, a major concern in LDLT, in recipients [25]. In this study, although DG LDLT resulted in lower overall patient survival rates (P = 0.0571) and a higher in-hospital mortality rate (P < 0.0001) than single-graft LDLT, it is essential to consider the higher MELD scores in the DG group while interpreting these findings. A previous study that compared 346 DG LDLT procedures conducted at our institution with propensity-score-matched single-graft LDLT procedures revealed no significant differences in long-term outcomes [26]. With the introduction of rituximab and an improved desensitization protocol, the use of ABOi grafts is gradually increasing, along with its indications. ABOi LDLT now constitutes approximately 25% of all adult LDLT procedures at AMC, with outcomes comparable to those of ABO-compatible LDLT. It has been cautiously implemented in patients with high MELD scores, acute liver failure, and hepatocellular carcinoma, with previous studies showing satisfactory results [16, 17]. However, severe antibody-mediated rejection and biliary and infectious complications still affect outcomes. At our institution, the indications for ABOi LDLT are the same as those for ABO-compatible LDLT; however, we closely monitor cases with an increased risk of biliary complications, such as multiple duct openings. Ongoing efforts are needed to develop a desensitization protocol that can minimize the risk of infection and antibody-mediated rejection, and to develop a rapid and accurate diagnostic method for antibody-mediated rejection.
This study has several limitations. First, this was a single-center retrospective data analysis. More importantly, historical bias may have arisen because of the approximately 27-year study period, over which time significant advances in preoperative evaluation, surgical techniques, and perioperative care have been made. For instance, in the initial phase of LDLT, the left lobe was used preferentially. However, it was found that modifying the right-lobe grafts ensured donor safety and provided satisfactory recipient outcomes, and LDLT using a modified right lobe is now the standard technique at our institution. The inferior surgical outcomes observed in the single left lobe group in this study may therefore be a result of historical biases and should be interpreted with caution.
Conclusion
A surgical technique refined through extensive experience plays a crucial role in achieving successful LDLT outcomes. In recent decades, most technical challenges related to adult and pediatric LDLT donor and recipient procedures have been effectively resolved. Implementing appropriate graft selection strategies tailored to the recipient and employing comprehensive multidisciplinary perioperative patient management involving experienced LT surgeons, anesthesiologists, critical care medicine specialists, interventional radiologists, and pathologists can expand the scope of LDLT and enhance recipient outcomes.
Data availability
The data presented in this study are available upon request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
References
Lee SG (2015) A complete treatment of adult living donor liver transplantation: a review of surgical technique and current challenges to expand indication of patients. Am J Transplant 15:17–38. https://doi.org/10.1111/ajt.12907
Li Z, Rammohan A, Gunasekaran V, Hong S, Chen IC, Kim J, Hervera Marquez KA, Hsu SC, Kirimker EO, Akamatsu N, Shaked O, Finotti M, Yeow M, Genedy L, Dutkowski P, Nadalin S, Boehnert MU, Polak WG, Bonney GK, Mathur A, Samstein B, Emond JC, Testa G, Olthoff KM, Rosen CB, Heimbach JK, Taner T, Wong TC, Lo CM, Hasegawa K, Balci D, Cattral M, Sapisochin G, Selzner N, Bin Jeng L, Broering D, Joh JW, Chen CL, Suk KS, Rela M, Clavien PA (2023) Novel benchmark for adult-to-adult living-donor liver transplantation: integrating eastern and western experiences. Ann Surg 278:798–806. https://doi.org/10.1097/SLA.0000000000006038
Park GC, Song GW, Moon DB, Lee SG (2016) A review of current status of living donor liver transplantation. Hepatobiliary Surg Nutr 5:107–117. https://doi.org/10.3978/j.issn.2304-3881.2015.08.04
Rela M, Reddy MS (2017) Living donor liver transplant (LDLT) is the way forward in Asia. Hepatol Int 11:148–151. https://doi.org/10.1007/s12072-016-9780-z
Kirchner VA, Goldaracena N, Sapisochin G, Alejandro RH, Shah SA (2020) Current status of liver transplantation in North America. Int J Surg 82S:9–13. https://doi.org/10.1016/j.ijsu.2020.05.059
Gyu Lee S, Min Park K, Hwang S, Hun Kim K, Nak Choi D, Hyung Joo S, Soo Anh C, Won Nah Y, Yeong Jeon J, Hoon Park S, Suck Koh K, Hoon Han S, Taek Choi K, Sam Hwang K, Sugawara Y, Makuuchi M, Chul Min P (2002) Modified right liver graft from a living donor to prevent congestion. Transplant 74:54–59. https://doi.org/10.1097/00007890-200207150-00010
Lee SG, Song GW, Yoon YI (2019) An exceptional series: 5000 living donor liver transplantations at Asan Medical Center, Seoul, Korea. Transplant 103:1739–1741. https://doi.org/10.1097/TP.0000000000002708
Yoon YI, Song GW, Lee SG, Park GC, Hwang S, Kim KH, Ahn CS, Moon DB, Ha TY, Jung DH, Kim KW, Shim JH, Tak EY, Kirchner VA, Pruett TL (2021) Safe use of right lobe living donor livers with moderate steatosis in adult-to-adult living donor liver transplantation: a retrospective study. Transpl Int 34:872–881. https://doi.org/10.1111/tri.13859
Park JI, Jung DH, Moon DB, Ahn CS, Yoon YI, Kang WH, Na BG, Ha SM, Kim SH, Kim M, Kim SM, Yang G, Oh RK, Hwang S, Lee SG (2023) Mini-incision right hepatectomy for living donor hepatectomy. Transplant 107:2384–2393. https://doi.org/10.1097/TP.0000000000004594
Ha TY, Hwang S, Ahn CS, Kim KH, Moon DB, Song GW, Jung DH, Park GC, Namgoong JM, Park CS, Park YH, Park HW, Kang SH, Jung BH, Lee SG (2013) Role of hand-assisted laparoscopic surgery in living-donor right liver harvest. Transpl Proc 45:2997–2999. https://doi.org/10.1016/j.transproceed.2013.08.053
Cho HD, Kim KH, Yoon YI, Kang WH, Jung DH, Park GC, Hwang S, Ahn CS, Moon DB, Ha TY, Song GW, Park JI, Lee SG (2021) Comparing purely laparoscopic versus open living donor right hepatectomy: propensity score-matched analysis. Br J Surg 108:e233–e234. https://doi.org/10.1093/bjs/znab090
Kwon JH, Yoon YI, Song GW, Kim KH, Moon DB, Jung DH, Park GC, Tak EY, Kirchner VA, Lee SG (2017) Living donor liver transplantation for patients older than age 70 years: a single-center experience. Am J Transpl 17:2890–2900. https://doi.org/10.1111/ajt.14355
Balci D, Ahn CS (2019) Hepatic artery reconstruction in living donor liver transplantation. Curr Opin Organ Transpl 24:631–636. https://doi.org/10.1097/MOT.0000000000000697
Song GW, Lee SG, Hwang S, Kim KH, Ahn CS, Moon DB, Ha TY, Jung DH, Park GC, Kim WJ, Sin MH, Yoon YI, Kang WH, Kim SH, Tak EY (2016) ABO-incompatible adult living donor liver transplantation under the desensitization protocol with rituximab. Am J Transpl 16:157–170. https://doi.org/10.1111/ajt.13444
Song GW, Lee SG, Hwang S, Kim KH, Ahn CS, Moon DB, Ha TY, Jung DH, Park GC, Kang SH, Jung BH, Yoon YI, Kim N (2014) Biliary stricture is the only concern in ABO-incompatible adult living donor liver transplantation in the rituximab era. J Hepatol 61:575–582. https://doi.org/10.1016/j.jhep.2014.04.039
Yoon YI, Song GW, Lee SG, Hwang S, Kim KH, Kim SH, Kang WH, Cho HD, Jwa EK, Kwon JH, Tak EY, Kirchner VA (2018) Outcome of ABO-incompatible adult living-donor liver transplantation for patients with hepatocellular carcinoma. J Hepatol 68:1153–1162. https://doi.org/10.1016/j.jhep.2018.02.002
Song GW, Lee SG, Moon DB, Ahn CS, Hwang S, Kim KH, Ha TY, Jung DH (2017) Dual-graft adult living donor liver transplantation: an innovative surgical procedure for live liver donor pool expansion. Ann Surg 266:10–18. https://doi.org/10.1097/SLA.0000000000001776
Kim KH, Kang SH, Jung DH, Yoon YI, Kim WJ, Shin MH, Lee SG (2017) Initial outcomes of pure laparoscopic living donor right hepatectomy in an experienced adult living donor liver transplant center. Transplant 101:1106–1110. https://doi.org/10.1097/TP.0000000000001637
Akyol M (2011) Comparison of open and laparoscopic live donor left lateral sectionectomy (Br J Surg 2011; 98: 1302–1308). Br J Surg 98:1308. https://doi.org/10.1002/bjs.7603
Chu KK, Wong KH, Chok KS (2021) Expanding indications for liver transplant: tumor and patient factors. Gut Liver 15:19–30. https://doi.org/10.5009/gnl19265
Moghe A, Ganesh S, Humar A, Molinari M, Jonassaint N (2021) Expanding donor selection and recipient indications for living donor liver transplantation. Clin Liver Dis 25:121–135. https://doi.org/10.1016/j.cld.2020.08.011
Ushigome H, Nakao T, Harada S, Nakamura T, Koshino K, Suzuki T, Ito T, Nobori S, Yoshimura N (2016) Elderly living donor liver transplant recipients over 60 years old at a Japanese single center. Transplant Proc 48:1115–1118. https://doi.org/10.1016/j.transproceed.2015.12.103
Yoshizumi T, Shirabe K, Soejima Y, Taketomi A, Yamashita N, Ikegami T, Uchiyama H, Kayashima H, Ninomiya M, Maehara Y (2010) Living donor liver transplantation in patients older than 60 years. Transplantation 90:433–437. https://doi.org/10.1097/TP.0b013e3181e81b2d
Lee SG, Hwang S, Park KM, Kim KH, Ahn CS, Lee YJ, Cheon JY, Joo SH, Moon DB, Joo CW, Min PC, Koh KS, Han SH, Choi KT, Hwang KS (2001) Seventeen adult-to-adult living donor liver transplantations using dual grafts. Transplant Proc 33:3461–3463. https://doi.org/10.1016/s0041-1345(01)02491-5
Hibi T, Wei Chieh AK, Chi-Yan Chan A, Bhangui P (2020) Current status of liver transplantation in Asia. Int J Surg 82S:4–8. https://doi.org/10.1016/j.ijsu.2020.05.071
Egawa H, Ohdan H, Saito K (2023) Current status of ABO-incompatible liver transplantation. Transplant 107:313–325. https://doi.org/10.1097/TP.0000000000004250
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Patients and data collection was performed by Young-In Yoon, Tae-Yong Ha, Gi-Won Song. Data analysis was performed by Shin Hwang, Chul-Soo Ahn, Deok-Bog Moon. The first draft of the manuscript was written by Young-In Yoon, Ki-Hun Kim, Sung-Gyu Lee. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the Institutional Review Board of Asan Medical Center, University of Ulsan College of Medicine, Seoul, South Korea (approval number 2023–1436) and conducted in accordance with the principles outlined in the Declaration of Helsinki.
Consent to participate
The need for an informed consent was waived due to the retrospective nature of the study.
Research involving human participants and/or animals, and Informed consent
Ethics committee approval and written consent to participate in the study were not required because this was a retrospective review of de-identified patient data from a public database.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoon, YI., Kim, KH., Hwang, S. et al. Outcomes of 6000 living donor liver transplantation procedures: a pioneering experience at ASAN Medical Center. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01807-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01807-5