Abstract
Postoperative CA19-9 elevation after pancreatic cancer resection suggests recurrence but can also occur in benign conditions. This study aimed to investigate the interpretation of postoperative CA19-9 elevation after pancreatic cancer surgery in terms of cancer recurrence. A cohort of patients undergoing pancreatectomy for pancreatic cancer at our hospital was included. Among them, 52 patients exhibited postoperative CA19-9 elevation without radiological evidence of recurrence. These patients were evaluated with follow-up CA19-9 measurements. The CA19-9 increase rates were calculated based on the first elevation and the follow-up measurement. The association between the CA19-9 increase rate and tumor recurrence was assessed. Patients with a CA19-9 increase rate of ≥ 30% had a significantly higher frequency of recurrence within 3 months compared to those without such an increase (p = 0.0002). Multivariate analysis demonstrated that a CA19-9 increase rate of ≥ 30% was an independent risk factor for recurrence (odds ratio 8.17, p = 0.0309). The CA19-9 value at the first elevation (p = 0.1794) and at the follow-up measurement (p = 0.1121) were not associated with recurrence. After the first postoperative CA19-9 elevation, the CA19-9 increase rate based on follow-up measurements can serve as a predictive factor for tumor recurrence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the postoperative setting following curative resection for pancreatic cancer, the current guidelines recommend regular follow-up at an interval of 3–6 months because an intense follow-up has not been found to impact patients’ survival rates [1]. However, a recent study has indicated that early detection of tumor recurrence could potentially prolong survival due to advancements in chemotherapy [2]. In this context, several approaches have been explored to identify recurrence at an early stage, with particular attention being drawn to carbohydrate antigen 19-9 (CA19-9) [3].
Although a postoperative elevation of CA19-9 is associated with cancer recurrence, a postoperative elevation of CA19-9 often precedes radiological confirmation of recurrence [4]. Moreover, elevated CA19-9 can also be attributable to benign causes, such as postoperative cholangitis [5] or exacerbated diabetes mellites [6]. Therefore, when a patient shows an elevated postoperative CA19-9 level, the clinical impact of the elevation can be further evaluated by obtaining a follow-up CA19-9 measurement. A markedly increased CA19-9 level at follow-up may indicate that tumor recurrence is likely, while a follow-up level within the normal range might suggest that the CA19-9 elevation was attributable to other causes. There remains a need to further study the impact of the dynamics of postoperative CA19-9 levels, to determine how to optimize the use of this marker to stratify patients according to risk of recurrence.
In the current study, we identified patients who underwent pancreatectomy for pancreatic cancer, exhibited elevated postoperative CA19-9 without radiographic recurrence, and then underwent follow-up measurement of CA19-9. Within this patient group, we calculated the rate of CA19-9 change between the first elevated measurement and the follow-up measurement, and we evaluated the significance of CA19-9 dynamics in association with the risk of tumor recurrence.
Methods
Patient selection
The current study was performed in compliance with the Declaration of Helsinki, and was approved by the ethical committee of our hospital (approval number 22507). CA19-9 was consistently measured in our institution, and an elevated CA19-9 level was defined as over 37 U/mL. With the aim to exclude CA19-9 elevations caused by non-cancerous events such as cholangitis, cases were excluded in which CA19-9 elevation (i.e., > 37 U/mL) accompanies a simultaneous elevation of total bilirubin level of > 3.0 mg/dL. We retrospectively reviewed the cases of 310 consecutive patients who underwent pancreatectomy for pancreatic cancer at our hospital between 2010 and 2020. Pre- and postoperative CA19-9 measurements were retrieved. Figure 1 shows the diagram of patient enrollment. Among the 310 patients reviewed, 50 were excluded from the analysis (Fig. 1, Exclusion criteria #1) for the following reasons: 21 patients did not achieve complete tumor resection due to intraoperatively diagnosed distant metastasis or local invasion, 16 were not followed-up at our hospital, and 13 showed a persistently undetectable CA19-9 level (i.e., Lewis negative population [7]). Among the remaining 260 patients, 137 were excluded (Exclusion criteria #2) because CA19-9 did not normalize within 2 months from surgery (n = 72), or postoperative CA19-9 measurements were persistently within the normal range (n = 65). After these exclusions, 123 patients were identified, whose CA19-9 level normalized within 2 months from surgery, and then increased to an abnormal level (> 37 U/mL; defined as the first elevation). Among these patients, 85 were subject to a follow-up CA19-9 measurement within 2 months after the first elevation (Exclusion criteria #3). For these 85 patients, we calculated the CA19-9 increase rate between the first elevation and follow-up measurement, and evaluated the association between this rate and future tumor recurrence. All of the patients included in this analysis underwent routine follow-ups for at least 2 years after surgery.
Scheme of patient enrollment. Exclusion criteria #1 (n = 50) included patients who did not undergo surgery with curative intent (n = 21), who were not followed-up at our hospital (n = 16), and who persistently exhibited an undetectable CA19-9 level (i.e., Lewis negative population; n = 13). Exclusion criteria #2 (n = 137) included patients whose CA19-9 level did not normalize within 2 months from surgery (n = 72), and whose CA19-9 level was persistently within the normal range throughout the surveyed period (n = 65). Exclusion criteria #3 included patients who did not undergo a follow-up CA19-9 measurement within 2 months from the first elevation
Postoperative management and diagnosis of recurrence
The postoperative surveillance of CA19-9 was started before the initiation of adjuvant chemotherapy. Adjuvant chemotherapy was administered using either S-1 or gemcitabine, depending on the patient’s overall health status. Regular monitoring, using laboratory testing or CT scans, was performed at an interval of every 1–3 months regardless of the presence or absence of symptoms suggestive of tumor recurrence. Tumor recurrence was defined as the reappearance of a malignant growth, confirmed by histological or radiological examinations. Radiological assessments included CT scans, magnetic resonance imaging (MRI), and 18F-fluorodeoxyglucose positron emission tomography (FDG-PET). Moreover, the value of postoperative CA19-9 did not affect the diagnosis of recurrence.
Patient characteristics
We analyzed the relationships between tumor recurrence and the selected patients’ demographic information, including sex, age at the time of surgery, body mass index, preoperative therapy, type of surgical procedure, surgical duration, blood loss, postoperative pancreatic fistula grade [8], histological results [9], postoperative therapy, and postoperative CA19-9 levels. The TNM classification of the tumor was determined based on the 8th edition of Union for International Cancer Control (UICC) TNM classification [10].
Statistical analysis
Patient characteristics were evaluated using chi-square statistics and the Mann–Whitney U test. To determine the optimal cut-off levels of each clinical variable for predicting tumor recurrence, we constructed receiver operating characteristic (ROC) curves (Youden index) in univariate and multivariate analyses. Variables with p < 0.05 were incorporated into a logistic regression model to determine independent risk factors for tumor recurrence, which were described with odds ratios. Statistical significance was defined as p < 0.05 derived from two-tailed tests. All statistical analyses were performed using JMP software (JMP, version 13.2.1).
Results
Association between the dynamics of CA19-9 and tumor recurrence
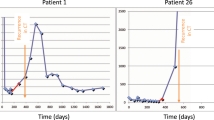
The data obtained from the entire cohort (n = 85) regarding patient characteristics, recurrence free survival (RFS) were presented in Supplementary Fig. 1, and Supplementary Table 1.
The dynamics of postoperative CA19-9 were evaluated in association with tumor recurrence, among the 85 patients whose CA19-9 level normalized after surgery and then increased to an abnormal level, and for whom a follow-up measurement was available within a 2-month interval (Fig. 1). The results are summarized in Fig. 2, which shows that 26 patients developed tumor recurrence before the first elevation of CA19-9, 7 patients developed recurrence between the first elevation and the follow-up measurement of CA19-9, while 52 patients had not developed recurrence at the time of the follow-up measurement.
Dynamics of postoperative CA19-9 and tumor recurrence. Patients who exhibited an elevated CA19-9 level (first elevation) were subject to a follow-up measurement. Tumor recurrence was observed prior to the first elevation in 26 patients, whereas recurrence occurred between the first elevation and the follow-up measurement in 7 patients. f/u follow-up
Predictive value of CA19-9 increase rate for tumor recurrence
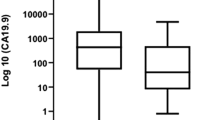
The 52 patients, who had not yet experienced tumor recurrence at the time of the follow-up measurement, were assessed for subsequent recurrence. The gap between surgery and the first measurement of postoperative CA19-9, and the gap between surgery and the first postoperative CT imaging were 44 ± 24.2 and 100.5 ± 36.7 days (median ± SD), respectively. Moreover, the intervals of CA19-9 measurement and CT imaging were 42.5 ± 18.0, and 92 ± 31.8 days (median ± SD), respectively. Next, we calculated the CA19-9 increase rate between the first elevation and follow-up. We further evaluated whether this rate could be used to predict recurrence within 3 months after the follow-up measurement. As shown in Fig. 3a, an elevated level of CA19-9 increase rate was associated with a higher frequency of tumor recurrence. In Fig. 3b, a ROC curve shows the association between the CA19-9 increase rate and tumor recurrence. We determined that a 30% rate of CA19-9 increase was an optimal cut-off value, which yielded 73.9% sensitivity and 79.3% specificity in predicting tumor recurrence within 3 months from the follow-up measurement.
Association between the CA19-9 increase rate and tumor recurrence. a Each patient’s CA19-9 increase rate relative to tumor recurrence. An elevated CA19-9 increase rate was associated with tumor recurrence. b ROC curve showing the association between CA19-9 increase rate and tumor recurrence. The CA19-9 increase rate showed moderate accuracy for predicting tumor recurrence within 2 months after the follow-up measurement (AUC: 0.80). The optimal cut-off value for the CA19-9 increase rate was calculated to be 30% (Youden index), which predicted tumor recurrence with 73.9% sensitivity and 79.3% specificity
Assessment of tumor recurrence risk based on the CA19-9 increase rate
Based on the ROC curve, the 52 patients were classified into three groups according to the CA19-9 increase rate (Fig. 4a). Type A patients exhibited a CA19-9 increase rate of over 30% at the follow-up measurement (n = 23); Type B patients exhibited an abnormal CA19-9 value at the follow-up measurement (> 37 U/mL), but the increase rate was ≤ 30% (n = 16); and Type C patients exhibited a normalized CA19-9 level at the follow-up measurement (n = 13). As presented in Fig. 5, the 3-year RFS in patients of Types A, B, and C was 8.7%, 18.8%, 46.2%, respectively, with a statistical difference between Types A and C (p = 0.0073). The recurrence rate according to the 3 Types was summarized in Fig. 4b. Among the 23 Type A patients, 17 (73.9%) experienced recurrence within 3 months from the follow-up measurement. On the other hand, recurrence within 3 months occurred in 5 of 16 Type B patients (31.3%), and 1 of 13 Type C patients (7.7%). The recurrence rates did not significantly differ between the Type B and Type C groups (p = 0.1834). In contrast, the recurrence rate in the Type A group was significantly higher than in the Type B (p = 0.0112) and Type C (p = 0.0003) groups.
Classification of the dynamics of CA19-9 and recurrence risk. a The dynamics of CA19-9 was categorized into three types based on the cut-off of 30% obtained from the ROC curve. Type A patients exhibited an > 30% increase at the follow-up measurement. Type B patients had an abnormal follow-up measurement, but an increase of ≤ 30%. Type C patients had a normalized follow-up measurement. b The recurrence rate within 3 months after the follow-up measurement is shown according to the three types. Recurrence occurred in 73.0% of Type A patients, which was significantly higher than the recurrence rates among Type B patients (p = 0.012) and Type C patients (p = 0.003). Recurrence occurred in 31.3% of Type B patients, and in 7.7% of Type C patients, and these rates did not significantly differ (p = 0.0184). f/u follow-up
Therefore, the 52 patients were divided into two groups according to recurrence risk. The high-risk group included the Type A patients, in which 73.9% (17/23) of patients experienced recurrence. The low-risk group included the Type B and C patients, in which 20.7% (6/29) of patients experienced recurrence. The recurrence rate was significantly higher in the high-risk group compared to the low-risk group (p = 0.0002).
Patients’ characteristics according to the risk of tumor recurrence
Table 1 summarizes the patients’ characteristics based on their risk of tumor recurrence. Compared to patients in the low-risk group, patients in the high-risk group were significantly younger (p = 0.0483) and had a significantly higher proportion of well-differentiated carcinoma (p = 0.0493). Additionally, patients in the high-risk group underwent adjuvant chemotherapy at a significantly higher rate than patients in the low-risk group (p = 0.0283).
Univariate and multivariate analysis to identify risk factors for tumor recurrence
Table 2 displays the clinical variables that were assessed in association with tumor recurrence within 3 months from the follow-up measurement, using both univariate and multivariate logistic regression models. Univariate analysis revealed four factors that were significantly associated with tumor recurrence: age > 61 years, CA19-9 of > 50 U/mL at the first elevation, CA19-9 of > 77 U/mL at the follow-up measurement, and categorization in the high-risk group. However, in multivariate analysis, only classification in the high-risk group was identified as an independent risk factor for tumor recurrence within 3 months (OR 8.1706, p = 0.0309). Supplementarily, the risk factors for tumor recurrence before the elevation of CA19-9 were assessed in the univariate and multivariate analysis (Supplementary Table 2).
Discussion
The management of patients who exhibit a postoperative elevation of CA19-9 is complicated by recent evidence showing that CA19-9 elevation precedes the radiological appearance of tumor recurrence by 6–18 months [4]. In our current study, the first elevation of CA19-9 preceded radiological confirmation of recurrence by a median of 91 days (IQR: 42-297) in the entire cohort. Moreover, in the patients who experienced recurrence before the first elevation of CA19-9, the median of an interval between the radiological confirmation and the CA19- 9 elevation was 158 days (IQR: 17-381). Since CA19-9 elevation may imply future tumor recurrence, its predictive value must be validated. Here we evaluated the impact of elevated CA19-9 by calculating the CA19-9 increase rate between the first elevation and a follow-up measurement.
Our multivariate analysis results clearly demonstrated the importance of the CA19-9 increase rate, revealing that tumor recurrence was significantly associated with the CA19-9 increase rate (p = 0.0309), but not with the CA19-9 value itself at the first elevation or at the follow-up measurement (Table 2). The predictive value of the CA19-9 increase rate was previously evaluated by Azizian et al., who reported that a single elevation of CA19-9, if it increased by over 2.45-fold, was associated with tumor recurrence with 45% sensitivity and 85% specificity [11]. They proposed that this cut-off might be useful in the selection of patients who would benefit from “CA19-9-orientated” chemotherapy for subclinical recurrence; however, the low sensitivity raises the concern that 45% of patients with subclinical recurrence may be overlooked. In our current study, the CA19-9 increase rate was calculated using the values of the first elevation and the follow-up measurement, and predicated tumor recurrence with 73.9% sensitivity and 79.3% specificity. Together, these results suggest that, although a single CA19-9 elevation can identify patients at risk of subclinical recurrence, the CA19-9 increase rate based on a follow-up measurement can predict subclinical recurrence with greater sensitivity. However, further studies are needed to validate this hypothesis.
In our current study, the Type B group included patients whose CA19-9 level at follow-up showed neither a marked increase nor normalization (Fig. 4). The management of this patient group presents a clinical challenge because an interpretation of this “mildly elevated CA19-9” has never been discussed. Although our analysis revealed that the recurrence risk did not significantly differ between the Type B and Type C groups (p = 0.1834; Fig. 4), this result may have been due to the small number of cases surveyed in this study. Notably, the recurrence rate decreased in the order of Types A, B, and C (Fig. 4). Therefore, the Type B patients may require closer postoperative follow-up than the Type C patients.
Intense postoperative follow-up is not currently recommended for pancreatic cancer patients because it does not improve survival [12]. On the contrary, in other cancers such as colorectal cancer, postoperative follow-up modified according to the recurrence risk is recommended[13]. Therefore, in pancreatic cancer patients, stratification of recurrence risk would be desired if it could improve patients’ survival. Based on our findings that recurrence risk can be stratified by the CA19-9 increase rate, we propose the following strategy as for patient management according to the dynamics of CA19-9. Type A patients, of whom 73.9% experienced recurrence, may warrant further evaluation for subclinical recurrence using other methods, such as ctDNA analysis [14]. Type B patients, of whom 31.3% experienced recurrence, may require close follow-up. Finally, Type C patients, of whom 7.7% experienced recurrence, may require routine follow-ups as recommended in the guidelines (e.g., every 3–6 months) [15]. The modification of postoperative management according to the dynamics of CA19-9 may identify patients who will benefit from intense follow-up and those who can be conventionally managed. However, the clinical impact of this strategy must be evaluated in terms of whether it can prolong patients’ survival. Moreover, further studies are needed to investigate how the dynamics of CA19-9 are influenced by neoadjuvant regimen, postoperative cholangitis, and adjuvant chemotherapy.
The present study has several limitations. First, due to its retrospective nature, we must carefully interpret the impact of the CA19-9 increase rate on tumor recurrence. A prospective study is warranted to further validate the significance of the CA19-9 increase rate. Second, the interval between postoperative follow-ups was heterogenous, which may have given rise to a considerable bias in this study.
Conclusion
In conclusion, after the first elevation of postoperative CA19-9, tumor recurrence could be predicted based on the CA19-9 increase rate calculated using a follow-up CA19-9 measurement. It may be recommended that patient management differ based on the recurrence risk determined by the dynamics of postoperative CA19-9.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Ducreux M, Cuhna AS, Caramella C et al (2015) Cancer of the pancreas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 26(Suppl 5):v56–v68
Daamen LA, Groot VP, Besselink MG et al (2022) Detection, treatment, and survival of pancreatic cancer recurrence in the Netherlands. Ann Surg 275:769–775
Berger AC, Garcia M, Hoffman JP et al (2008) Postresection CA 19–9 predicts overall survival in patients with pancreatic cancer treated with adjuvant chemoradiation: a prospective validation by RTOG 9704. J Clin Oncol 26:5918–5922
Rieser CJ, Zenati M, Hamad A et al (2018) CA19-9 on postoperative surveillance in pancreatic ductal adenocarcinoma: predicting recurrence and changing prognosis over time. Ann Surg Oncol 25:3483–3491
Albert MB, Steinberg WM, Henry JP (1988) Elevated serum levels of tumor marker CA19-9 in acute cholangitis. Dig Dis Sci 33:1223–1225
Murakami M, Nagai Y, Tenjin A et al (2018) Proposed cut-off value of CA19-9 for detecting pancreatic cancer in patients with diabetes: a case-control study. Endocr J 65:639–643
Narimatsu H, Iwasaki H, Nakayama F et al (1998) Lewis and secretor gene dosages affect CA19-9 and DU-PAN-2 serum levels in normal individuals and colorectal cancer patients. Cancer Res 58:512–518
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161:584–591
Society JP, Classification of Pancreatic Carcinoma (Fourth English edition) (1996) Kanehara, Tokyo
James D, Brierley MKG (2017) Christian Wittekind, International Union Against Cancer (UICC): TNM Classification of Malignant Tumours, 8th edn. Wiley-Blackwell, Oxford
Azizian A, Rühlmann F, Krause T et al (2020) CA19–9 for detecting recurrence of pancreatic cancer. Scient Rep. https://doi.org/10.1038/s41598-020-57930-x
Castellanos JA, Merchant NB (2014) Intensity of follow-up after pancreatic cancer resection. Ann Surg Oncol 21:747–751
Godhi S, Godhi A, Bhat R et al (2017) Colorectal cancer: postoperative follow-up and surveillance. Indian J Surg 79:234–237
Guven DC, Sahin TK, Yildirim HC et al (2021) A systematic review and meta-analysis of the association between circulating tumor DNA (ctDNA) and prognosis in pancreatic cancer. Crit Rev Oncol Hematol 168:103528
Tempero MA, Arnoletti JP, Behrman S et al (2010) Pancreatic adenocarcinoma. J Natl Compr Canc Netw 8:972–1017
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by HI, and YT. The first draft of the manuscript was written by HI and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare.
Ethics approval
The current study was performed in compliance with the Declaration of Helsinki, and was approved by the ethical committee of our hospital (approval number 22507).
Informed consent
Informed consent was obtained on a paper basis from each patient enrolled in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Imamura, H., Tomimaru, Y., Kobayashi, S. et al. Diagnostic impact of postoperative CA19-9 dynamics on pancreatic cancer recurrence: a single-institution retrospective study. Updates Surg 76, 479–486 (2024). https://doi.org/10.1007/s13304-024-01758-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-024-01758-x