Abstract
The incidence of bone metastasis (BM) in colorectal cancer (CRC) patients is low and the prognosis is poor. There is no clear conclusion on the risk factors affecting the survival of CRC patients with BM. The aim of this study was to investigate the factors that may affect the prognosis of CRC patients with BM. The clinical and pathological data of CRC patients with BM were retrospectively analyzed. The overall survival after BM diagnosis was estimated using the Kaplan–Meier method and Log-rank test, and a multivariable cox regression model was used to identify the prognostic factors of overall survival. This study included 178 CRC patients with BM, of whom 151 had left-sided CRC and 27 had right-sided colon cancer. 1124 CRC patients with BM from the SEER database were included to perform a sensitivity analysis of the primary outcome. Multivariate analysis showed that the N staging, site of BM, and primary tumor sidedness (PTS) were independent prognostic factors for CRC with BM. Among them, right-sided colon cancer patients with BM had a poorer prognosis. Sensitivity analyses showed that PTS was an independent prognostic factor in CRC patients with BM. Primary tumor sidedness and N stage may be potential prognostic markers for BM of CRC. The prognosis of N0 stage CRC with BM is better, while the prognosis of right-sided colon cancer is poor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is a common malignant tumor, and the most common metastatic sites of CRC are liver or lung, while bone metastases (BMs) are relatively rare. The vast majority of metastatic bone tumors arise from prostate, breast, kidney, lung, and thyroid cancers, while CRC is less common, accounting for only 3–5% [1].
Patients with BM may develop pathologic fractures, severe bone pain, vertebral compression, and skeleton-related events (SRE) [2], such as hypercalcemia, which can seriously affect the quality of life. The outcomes of CRC patients with BM are worse; the median survival of these patients is less than 1 year [4] and the 5-year survival rate is less than 5% [1]. Despite the inclusion of bisphosphonate therapy, chemotherapy, molecular targeted therapy, immunotherapy, local surgery, radiotherapy, analgesia, and symptomatic support therapy, the prognosis for CRC patients with BM remains unsatisfactory. Understanding the pathological, biochemical, and therapeutic factors related to the prognosis of CRC patients with BM is helpful for early clinical intervention to improve the quality of life and survival rate of patients. However, there is no consensus on the risk factors affecting the survival of CRC patients with BM, and the relevant research remains limited [6].
Therefore, we conducted a retrospective study on the clinical data and follow-up data of 178 CRC patients with BM at Tianjin Union Medical Center. The aims of our study were to analyze the potential prognostic factors related to the survival of CRC patients with BM using clinicopathological, biochemical, and treatment information, which will help optimize clinical treatment strategies.
Materials and methods
Patients and data resources
A total of 202 CRC patients diagnosed with BM between January 2012 and December 2021 in Tianjin Union Medical Center were retrospectively identified. Only patients with CRC and ≥ 1 site of BM during the course of their disease were included in this study. Cases in which CRC directly invaded adjacent bone have been excluded. 13 patients were excluded due to incomplete clinical information, 10 patients were excluded due to BM caused by other types of malignant tumors, and 1 patient was lost to follow-up. The pathological examination confirmed that it was primary CRC. Furthermore, the identification of BM was mainly performed by imaging examinations such as X-rays, computed tomography, emission computed tomography, positron emission tomography–computed tomography, and magnetic resonance imaging. Right-sided colon cancer (RCC) includes cancers of two-thirds of the proximal transverse colon hepatic flexure of colon, ascending colon, and caecum, while left-sided CRC (LCRC) encompasses cancers of third of the distal transverse colon, splenic flexure of colon, descending colon, sigmoid colon, and high and middle rectum [7]. For colon cancer, we performed D3 lymphadenectomy (resection of parenteral, intermediate and central lymph nodes). Lymph node resection for rectal cancer includes intra mesenteric lymphadenectomy, lateral mesenteric lymphadenectomy plus lateral lymph node dissection. For patients who did not receive primary tumor resection, the reported TNM stages of primary tumors were clinically evaluated based on imaging techniques. Extra-osseous metastases were defined as those that occur simultaneously or after the primary tumor. In terms of number of BM, isolated bone involvement was defined as two or fewer adjacent vertebral metastases, while multiple bone involvement was defined as non-adjacent or more than two vertebral metastases.
Follow-up was from diagnosis of CRC until death or March 2022. Cancer-specific survival (CSS) was defined as the time from diagnosis of BM to cancer death or end of follow-up. According to the corresponding guidelines, patients with AJCC stage I were followed up once every 6 months for 5 years. Patients with AJCC stages II–IVwere followed up every 3 months for 3 years, then every 6 months until 5 years after surgery, and then annually after 5 years post-surgery. This study was approved by the Ethics Committee of Tianjin Union Medical Center.
Prognostic factors
Clinical data and survival status of patients were obtained from electronic medical records and follow-ups. Statistical analysis was performed on the collected variables, which included (1) demographic characteristics: age and gender, (2) clinical features: primary tumor location, pathological type, AJCC TNM stage, bone involvement, Tumor metastasis time, site of BM, extra-osseous metastases, (3) laboratory examinations: ALP levels, CEA levels, CA199 levels, and primary tumor resection, and (4) BM-related treatments such as systemic treatment, bisphosphonates, radiotherapy, and surgery.
Sensitivity analysis
Two sets of sensitivity analyses were performed to assess the robustness of the primary outcome. First, considering the impact of different populations on outcomes, we included 1124 patients from the SEER database and screened for age, gender, pathological type of tumor, AJCC TNM stage, T stage, N stage, CEA levels, extra-osseous metastases, liver metastasis, lung metastasis, brain–lung metastasis, chemotherapy, radiotherapy, primary tumor resection, and primary tumor sidedness (PTS) for a total of 15 variables. Then Kaplan–Meier analysis and COX regression analysis were used to re-identify the prognostic factors of BM in CRC (Model 1). Second, considering the influence of clinical treatments such as radiotherapy and tumor pathological information on patient prognosis, we constructed two new prognostic models based on the original prognostic model (Model 0): (1) Model 2.1: Variables contained in the Model 0 and primary tumor site surgery, chemotherapy, radiotherapy, BM site surgery, bisphosphonate therapy, histological type, and T stage; (2) Model 2.2: Variables contained in the Model 0 and primary tumor site surgery, chemotherapy, radiotherapy, BM site surgery, and bisphosphonate therapy; in addition, we removed the variable of lung metastasis (Model 3) from the original prognostic model to assess the changes of independent prognostic factors in CRC patients with BM under different models because of the possible partial overlap between lung metastasis and EM data.
Statistical analysis
Comparing the clinical baseline characteristics of RCC and LCRC patients with BM using Pearson's χ2 test or Fisher's exact test, all variables were analyzed by Kaplan–Meier method and Log-rank test for univariate survival analysis. In the next step, variables whose univariate analysis result was p < 0.05 were included in COX regression model for multivariate prognosis analysis. Finally, hazard ratios and 95% confidence intervals were calculated. p < 0.05 indicates that the difference is statistically significant. Statistical analyses were carried out by IBM SPSS Statistics software (version 26.0).
Results
In this study, 178 colorectal patients diagnosed with BM were included in the final analysis, while 24 cases were excluded. 84.8% of patients (151/178) were identified with LCRC with BM, and 15.2% of patients (27/178) were reported as RCC with BM.
Patient characteristics
The clinical and pathological characteristics of the LCRC and RCC patients with BM are shown in Table 1. The median age in the LCRC group was 62 years (29–84 years), compared with 65 years in the RCC group. Adenocarcinoma was significantly more common in the LCRC group than in the RCC group (77.5% vs. 55.6%, p = 0.04). The AJCC TNM stage (p = 0.088), CEA levels (p = 0.377), CA19-9 levels (p = 0.135), and extra-osseous metastases (p = 0.578) were similar between two groups, when BM was diagnosed.
Patterns of BM and extra-osseous metastasis
There was a statistically significant difference in tumor metastasis time between the LCRC group and RCC group (p = 0.009). Synchronous BMs were more frequent in the RCC group (85.2% vs. 58.3%), while metachronous BMs were significantly more prevalent in the LCRC group (41.7% vs. 14.8%). However, no statistical significance in extra-osseous metastases was observed between the two groups (p = 0.508). Multiple bone lesions were found in 54.3% of patients (82/151) in the LCRC group and 70.4% of patients (19/27) in the RCC group, showing no significant difference (p = 0.143). The spine was the primary site of BM for bone lesions in both groups (35.1% vs. 25.9%), followed by the pelvis (28.5% vs. 22.2%).
Treatments
Primary tumor resection was performed more frequently on RCC patients with BM than LCRC patients with BM (88.9% vs. 66.9%, p = 0.037). Patients in both groups received standardized treatment according to the NCCN guidelines. In addition, no significant difference was found in chemotherapy plus targeted therapy, radiotherapy, bisphosphonates, and metastasectomy for BM between the LCRC and RCC groups (p > 0.05).
Survival
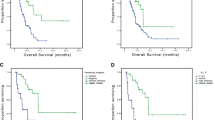
During the follow-up period, 118 CRC patients (66.3%) died of the disease, including 97 in the LCRC group and 21 in the RCC group. The median follow-up time was 7 months (1–39 months). Median CSS was 15 months (95% CI 11.5–18.5 months) in LCRC patients and 6 months (95% CI 0–13.4 months) in RCC patients. The 3-year and 5-year overall survival of LCRC and RCC with BM were 30.9% versus 14.4%, and 21% versus 7.2%, respectively. Figure 1 displays the Kaplan–Meier curves of PTL according to overall CSS. The overall CSS of LCRC was significantly longer than that of RCC (p = 0.22). There was no significant difference in the number of lymph nodes removed between the left and right colons (14.76 ± 4.73 vs. 16.67 ± 9.23, p = 0.560). The results showed that in CRC, the median OS in the group with < 12 lymph nodes dissection was 12 (0.44–23.56) months. The median OS was 15 (12.99–17.01) months in the group with ≥ 12 lymph nodes dissection, and there was no significant difference in OS (p = 0.449).
In this study, compared with LCRC, RCC had a shorter survival time after SBM (15 vs. 5 months). In RCC, the survival time of SBM was significantly shorter (14 vs. 5 months) compared to MBM. This may be due to their different pathologic features and sensitivity to treatment.
We further analyzed the time between the onset of CRC and BM, and the median MBM was 11.5 months. SBM (< 6 months), early MBM (6–12 months), and late MBM (> 12 months) were divided. The median OS of MBM was 14 (7.37–20.63) months, the median OS of early MBM was 16 (0–34.27) months, and the median OS of late SBM was 13 (9.61–16.39) months, and there was no significant difference in prognosis (p = 0.973).
Prognostic Factors
Table 2 shows the p values from the univariate survival analysis for CRC, LCRC, and RCC groups. Variables with p < 0.05 were included in COX regression model for multivariate prognosis analysis. The independent prognostic factors were defined as variables with p < 0.05 in COX regression model. Consequently, primary tumor sidedness (LCRC/RCC) (HR 1.872, p = 0.024), N stage (HR 6.693, p < 0.001), and site of BM (p = 0.026) were identified as independent prognostic factors for CRC with BM patients. N stage (HR 10.523, p = 0.002), lung metastasis (HR 1.529, p = 0.049), and site of BM (p = 0.047) were independent prognostic factors for LCRC with BM patients. In contrast, bisphosphonate therapy (HR 0.007, p = 0.002) and site of BM (p = 0.001) were independent prognostic factors for RCC in BM patients (Fig. 2).
Sensitivity analysis
Prognostic models constructed for 1124 patients in the SEER database showed that pathological type of tumor, T stage, N stage, CEA levels, extra-osseous metastases, liver metastasis, lung metastasis, brain metastasis, primary tumor resection, chemotherapy, radiotherapy, and PTS were independent prognostic factors for CRC patients with BM (Fig. 3). The results of the prognostic models (Model 2, Model 3) that included different variables all indicated that PTS and N stage were independent prognostic factors for CRC patients with BM (Fig. 4).
Discussion
This retrospectively analysis found that primary tumor sidedness, N stage, and site of BM were an independent prognostic factor for CRC with BM. The 5-year OS of LCRC with BM was 21%, while the 5-year OS in the RCC with BM was 7.2% (p = 0.024). The categorization of left-sided CRC and right-sided colon cancer using the layering method may represent the optimal strategy (p = 0.024) (Fig. 1).
There is still no consensus on the prognostic factors of CRC patients with BM. Most studies have shown that the potential risk factors affecting the prognosis of CRC with BM include osteolytic lesions, more than one bone lesion, rib metastasis, CEA elevation, and lung metastasis at BM [5], which is consistent with our study.
Since most of the BM cases are accompanied by metastases to other organs, it suggests that CRC generally may not metastasize to the bone first [10]. Before BM, the most common sites of CRC are the liver, lung, and peritoneum [11]. LCRC is more likely to metastasize to the lungs and liver, whereas RCC metastases to the peritoneum are more common [12]. Studies have shown that CRC with peritoneal metastasis may have a worse prognosis [13]. Thus, patients with LCRC may have a higher risk of BM, while RCC patients with BM may be associated with a worse prognosis. In addition, in our study, there was a higher proportion of synchronous BM (85.3% vs. 58.2%) in RCC, while metachronous BM had a higher prevalence in LCRC (41.7% vs. 14.8%). Previous studies have shown that patients with synchronous BM have a poorer prognosis than patients with metachronous BM [14]. Therefore, this difference may also lead to a poor prognosis in RCC patients with BM.
BM in CRC involves many molecular markers, which may influence the occurrence and development of CRC with BM [15] or predict the occurrence of BM [17]. In this study, CEA and CA19-9 levels were prognostic factors in LCRC patients with BM, and patients with positive levels had shorter OS, which was consistent with previous studies [18]. In addition, several studies have reported that positive ALP level is an independent risk factor for BM in many tumors [20], such as CRC, bladder cancer, and lung cancer, and is associated with poor clinical outcomes [22]. In our study, the univariate analysis demonstrated that ALP was a prognostic factor for LCRC with BM, and positive ALP level patients had significantly shorter OS compared to negative patients (9 vs. 22 months). Therefore, attention should be paid to the changes in the above serological indicators in CRC patients, especially in rectal cancer patients with BM.
Regional lymph node metastasis is the primary route of CRC metastasis, which is closely related to liver, lung, and other distant metastasis [24]. The N stage can predict the occurrence of BM. Furthermore, the N stage was the most significant independent prognostic factor in LCRC patients with BM according to multivariate analysis. Among LCRC and RCC patients, the median survival time of N0 stage patients was higher than that of N1–2 stage patients (Fig. 3A). Therefore, CRC patients with advanced pathological stage and lymph node metastasis should be carefully followed up. CRC usually metastasizes to the liver or lung before bone, but compared with liver metastasis, lung metastasis to bone occurs within a shorter time span, and it can better predict the progression of CRC to bone [10]. Moreover, studies have found that patients with CRC have a poor prognosis after lung metastasis [25]. Lung metastasis was an independent prognostic factor in LCRC patients with BM and not for RCC. Among them, patients without lung metastasis had a better prognosis (MST: 17 vs. 12 months) (Fig. 3B). These findings suggest that LCRC BM via the pulmonary route may lead to poor prognosis. The mode of metastasis may be different, and RCC may spread to the liver via portal circulation, and from there to the lungs. RC metastases directly to the lungs via the rectal venous plexus and Batson venous plexus communicating with it via the inferior vena cava [24]. Therefore, the occurrence of lung metastasis in RCC patients may be related to liver metastasis and other factors, which jointly affect the prognosis of patients. The site and number of BM can affect the outcomes of CRC patients with BM [28]. Our study shows that the site of BM is an independent prognostic factor in both LCRC and RCC. Compared with the pelvis, the OS for CRC metastasis to the spine and ribs was shorter (Fig. 3C). In addition, bone involvement was a prognostic factor for LCRC patients with BM. Univariate analysis of LCRC and RCC patients showed significantly lower OS in multiple BM compared to solitary BM, which is consistent with previous research [4]. Therefore, systematic imaging examination is useful in assessing the prognosis of BM in patients with CRC with risk factors.
Bisphosphonate therapy can inhibit the activity of osteoclasts and reduce bone resorption, thus effectively preventing the occurrence of SREs and improving the quality of life and survival rate of patients [30]. Our findings showed that bisphosphonate therapy had a positive impact on the prognosis and could significantly improve the OS of RCC patients with BM (Fig. 3D). This implies that LCRC and RCC patients with BM might exhibit varying levels of sensitivity to bisphosphonates, and RCC with BM patients were more sensitive to bisphosphonates [31]. In addition, possibly due to the greater number of multiple BM in RCC compared with LCRC (70.4% vs. 54.3%), the clinical benefit and prognosis of patients treated with bisphosphonate are more obvious.
Compared with mucinous adenocarcinoma, the prognosis of adenocarcinoma is significantly better, and the incidence of adenocarcinoma in the LCRC group is significantly higher than that in the RCC group (77.5% vs. 55.6%), which may lead to a better prognosis for LCRC with BM. In addition, due to the different incidence rates, the incidence of LCRC is higher, so there are more patients in the LCRC group, which may lead to bias. Due to the small amount of data included in this retrospective study, bias matching analysis was not performed to reduce bias, but sensitivity analysis was used to further determine the robustness of the conclusions. The results showed that the main results obtained from the data in this paper were almost consistent with the conclusions obtained from the large sample SEER database, which fully demonstrated the robustness of the results.
It is noteworthy that in order to assess the possible impact of risk factors on the prognosis of CRC patients with BM in different populations, we included a subset of such patients from the SEER database for analysis. In addition, to address the possible effects of treatments and pathological factors on the prognosis of CRC patients with BM, we adjusted the independent variables based on the original model and constructed multiple prognostic models for analysis. The results showed that N stage and PTS were potential risk factors for the prognosis of CRC patients with BM. And the prognosis of N0 stage CRC with BM is better, while the prognosis of right-sided colon cancer is poor. Our study had several limitations. First, this was a single-center retrospective study, which could involve selection bias. Second, the incidence of BM in CRC patients has been underestimated because only treated patients were included in our study. Third, moderate sample size and non-randomized design limit conclusions about efficient clinical management. Therefore, it is necessary to conduct further large sample, multivariable randomized prospective studies.
Conclusions
In this study, we compared the clinical and pathological features, treatment options, and outcomes of patients with LCRC and RCC with bone metastases. We found that RCC patients with BM had a poorer prognosis than LCRC patients. In addition, CRC patients with different sites of BM have different outcomes. These results may help doctors make timely clinical decisions and effective treatment strategies.
Data availability
Data analyzed during the current study are not public due to confidentiality and anonymity of participants, but are available on reasonable request from zmq@nankai.edu.cn.
References
Zhenghong, Zihua Z, Guoweijian et al (2017) Retrospective study of predictors of bone metastasis in colorectal cancer patients. J Bone Oncol 9:25–28
Kawamura H, Yamaguchi T, Yano Y et al (2018) Characteristics and prognostic factors of bone metastasis in patients with colorectal cancer. Dis Colon Rectum 61:673–678
Santini D, Tampellini M, Vincenzi B et al (2012) Natural history of bone metastasis in colorectal cancer: final results of a large Italian bone metastases study. Ann Oncol 23:2072–2077
Byttner M, Wedin R, Bauer H et al (2021) Outcome of surgical treatment for bone metastases caused by colorectal cancer. J Gastrointest Oncol 12:2150–2156
Lei S, Ge Y, Tian S et al (2020) Colorectal cancer metastases to brain or bone and the relationship to primary tumor location: a population-based study. J Gastrointest Surg 24:1833–1842
Christensen TD, Jensen SG, Larsen FO et al (2018) Systematic review: Incidence, risk factors, survival and treatment of bone metastases from colorectal cancer. J Bone Oncol 13:97–105
Lee GH, Malietzis G, Askari A et al (2015) Is right-sided colon cancer different to left-sided colorectal cancer?—A systematic review. Eur J Surg Oncol 41:300–308
Guo X, Zhang C, Ma W et al (2019) Patterns of bone metastases in newly diagnosed colorectal cancer: a real-world analysis in the SEER database. Int J Colorectal Dis 34:533–543
Li X, Hu W, Sun H et al (2021) Survival outcome and prognostic factors for colorectal cancer with synchronous bone metastasis: a population-based study. Clin Exp Metastasis 38:89–95
Roth ES, Fetzer DT, Barron BJ et al (2009) Does colon cancer ever metastasize to bone first? A temporal analysis of colorectal cancer progression. BMC Cancer 9:274
Jimi S, Yasui T, Hotokezaka M et al (2013) Clinical features and prognostic factors of bone metastases from colorectal cancer. Surg Today 43:751–756
Boeckx N, Janssens K, Van Camp G et al (2018) The predictive value of primary tumor location in patients with metastatic colorectal cancer: a systematic review. Crit Rev Oncol Hematol 121:1–10
Franko J, Shi Q, Meyers JP et al (2016) Prognosis of patients with peritoneal metastatic colorectal cancer given systemic therapy: an analysis of individual patient data from prospective randomised trials from the Analysis and Research in Cancers of the Digestive System (ARCAD) database. Lancet Oncol 17:1709–1719
Colloca GA, Venturino A, Guarneri D (2020) Different variables predict the outcome of patients with synchronous versus metachronous metastases of colorectal cancer. Clin Transl Oncol 22:1399–1406
Gigante I, Tutino V, De Nunzio V et al (2020) Colorectal cancer and bone tissue: fantastic relations and where to find them. Cancers (Basel) 12:2029
Reynaud C, Ferreras L, Di Mauro P et al (2017) Lysyl oxidase is a strong determinant of tumor cell colonization in bone. Cancer Res 77:268–278
Nunes L, Aasebo K, Mathot L et al (2020) Molecular characterization of a large unselected cohort of metastatic colorectal cancers in relation to primary tumor location, rare metastatic sites and prognosis. Acta Oncol 59:417–426
Liu Z, Xu Y, Xu G et al (2021) Nomogram for predicting overall survival in colorectal cancer with distant metastasis. BMC Gastroenterol 21:103
Kobayashi Y, Shida D, Boku N et al (2022) Prognostic factors of bone metastases from colorectal cancer in the era of targeted therapy. Dis Colon Rectum 66:401–409
Huang P, Lan M, Peng AF et al (2017) Serum calcium, alkaline phosphotase and hemoglobin as risk factors for bone metastases in bladder cancer. PLoS ONE 12:e0183835
Wang N, Liu F, Xi W et al (2021) Development and validation of risk and prognostic nomograms for bone metastases in Chinese advanced colorectal cancer patients. Ann Transl Med 9:875
Mou H, Wang Z, Zhang W et al (2021) Clinical features and serological markers risk model predicts overall survival in patients undergoing breast cancer and bone metastasis surgeries. Front Oncol 11:693689
Park HS, Chun YJ, Kim HS et al (2020) Clinical features and KRAS mutation in colorectal cancer with bone metastasis. Sci Rep 10:21180
Riihimaki M, Hemminki A, Sundquist J et al (2016) Patterns of metastasis in colon and rectal cancer. Sci Rep 6:29765
Ge Y, Lei S, Cai B et al (2020) Incidence and prognosis of pulmonary metastasis in colorectal cancer: a population-based study. Int J Colorectal Dis 35:223–232
Procaccio L, Bergamo F, Manai C et al (2019) An overview on clinical, pathological and molecular features of lung metastases from colorectal cancer. Expert Rev Respir Med 13:635–644
Tamas K, Walenkamp AM, de Vries EG et al (2015) Rectal and colon cancer: not just a different anatomic site. Cancer Treat Rev 41:671–679
Ali A, Hoyle A, Haran AM et al (2021) Association of bone metastatic burden with survival benefit from prostate radiotherapy in patients with newly diagnosed metastatic prostate cancer: a secondary analysis of a randomized clinical trial. JAMA Oncol 7:555–563
Harries M, Taylor A, Holmberg L et al (2014) Incidence of bone metastases and survival after a diagnosis of bone metastases in breast cancer patients. Cancer Epidemiol 38:427–434
Hughes DE, Wright KR, Uy HL et al (1995) Bisphosphonates promote apoptosis in murine osteoclasts in vitro and in vivo. J Bone Miner Res 10:1478–1487
Ma CX, Guan X, Wei R et al (2020) The distinction of clinicopathological characteristics, treatment strategy and outcome in colorectal cancer patients with synchronous vs. metachronous bone metastasis. Front Oncol 10:974
Funding
This study was funded by the foundation of committee on science and technology of Tianjin (Nos. 21JCYBJC01090 and 21JCZDJC00990). This work was funded by Tianjin Key Medical Discipline (Specialty) Construction Project (No. TJYXZDXK-044A). The funding source had no role in study design, data collection, analysis, or interpretation, report writing, or the decision to submit this paper for publication.
Author information
Authors and Affiliations
Contributions
MZ and TS contributed to conceptualization; MZ and YZ were involved in methodology; TL, HJ, and ZC provided software; MZ and HJ performed validation; MZ and LZ did formal analysis; TL, YZ, HJ, and ZC performed investigation; TL and YZ contributed to data curation; TL and HJ were involved in writing—original draft preparation; XZ, MZ, and TS were involved in writing—review and editing; YZ and ZC were responsible for visualization; XZ and MZ did supervision; MZ and TS performed project administration. All the authors have read and agreed to the published version of the manuscript. TL and HJ contributed equally to this work.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
Research involving Human Participants, this study was conducted in accordance with the Declaration of Helsinki, and this study was approved by the Ethics Committee of Tianjin union medical center. Retrospective studies do not require formal consent in accordance with the relevant regulations of Tianjin union medical center.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the Ethics Committee of Tianjin union medical center and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, T., Jing, H., Zhang, Y. et al. Prognostic impact of colorectal cancer patients with bone metastases: a single-center experience. Updates Surg 75, 2245–2256 (2023). https://doi.org/10.1007/s13304-023-01696-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01696-0