Abstract
We aimed to identify risk factors for early hypocalcemia after parathyroidectomy in patients with secondary hyperparathyroidism. We retrospectively enrolled 106 of 120 consecutive patients with secondary hyperparathyroidism who underwent parathyroidectomy between January 2019 and July 2021. Perioperative laboratory parameters, preoperative computerized tomography (CT) images, and postoperative histology were evaluated. Parathyroid calcification was defined as hyperdense regions with a density of > 130 Hounsfield Units on CT images of the parathyroid. Subtotal parathyroidectomy, total parathyroidectomy without auto-transplantation, or total parathyroidectomy with auto-transplantation were performed in the present study. Postoperative hypocalcemia was defined as a serum calcium concentration < 2.1 mmol/L within 4 days of surgery. The participants were categorized according to the presence (n = 33) or absence (n = 73) of postoperative hypocalcemia. The demographics, comorbidities, and surgical details were similar in the two groups. Multivariate analysis showed that the preoperative alkaline phosphatase activity, serum intact parathyroid hormone and calcium concentrations, and parathyroid calcification were independent risk factors for postoperative hypocalcemia (all P < 0.05). Receiver operating characteristic analysis generated areas under the curves for preoperative alkaline phosphatase, intact parathyroid hormone, and parathyroid calcification of 0.82, 0.80, and 0.70, respectively (all P < 0.05). Cut-off values for preoperative alkaline phosphatase (> 242.9 IU/L) and intact parathyroid hormone (> 2,104 pg/mL) were found to be predictive of postoperative hypocalcemia. High preoperative alkaline phosphatase activity and serum intact parathyroid hormone concentration and low serum calcium are associated with higher risks of postoperative hypocalcemia. Calcification of the parathyroid may represent a novel radiologic means of predicting postoperative hypocalcemia.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Secondary hyperparathyroidism (SHPT) is a common complication in patients undergoing dialysis because of chronic kidney disease [1, 2]. Clinically, parathyroidectomy (PTX) represents a definitive treatment option for patients with severe SHPT who have not responded to medical therapy. Current evidence shows that PTX can improve quality of life, increase bone mineral density, reduce fracture risk, and prolong survival. Nonetheless, the management of patients with SHPT after PTX is challenging because of the high prevalence of postoperative hypocalcemia [3,4,5], which necessitates intensive monitoring of serum calcium concentration and meticulous adjustment of calcium supplementation.
Several risk factors, including preoperative serum alkaline phosphatase (ALP) activity, serum calcium (Ca) concentration, and serum intact parathyroid hormone (i-PTH) concentration, have been shown to be predictive of postoperative hypocalcemia in patients with SHPT that require PTX [6,7,8,9,10,11,12,13,14,15,16]. However, these findings were made using various definitions of postoperative hypocalcemia, differing methods of perioperative management, and in patients with a variety of clinical characteristics, and therefore do not provide for a robust understanding of the etiology of postoperative hypocalcemia in patients with SHPT. In addition, although laboratory parameters have been considered in many studies, few have focused on the potential predictive value of the status of the parathyroid itself, determined using preoperative imaging techniques. Currently, computerized tomography (CT) is an economical and feasible means of showing the location and extent of the parathyroid prior to surgery. Calcification of the parathyroid in patients with SHPT has been previously identified using CT and its identification has been validated using histologic examination [17, 18]. However, whether this radiologic phenomenon may represent a useful means of identifying patients with SHPT who are at a high risk of postoperative hypocalcemia remains to be determined.
Therefore, in the present study, we aimed to reappraise the risk factors for postoperative hypocalcemia following PTX in patients with SHPT, using laboratory and radiologic data, and to identify appropriate cut-off values for key risk factors to facilitate better identification of high-risk patients.
Material and methods
Recruitment of patients with SHPT
This study was approved by the local ethics committee. Written informed consent was obtained from all the participants. Data from 120 consecutive patients with SHPT who were admitted to the hospital and treated by PTX between January 2019 and July 2021 were retrospectively reviewed. The study is reported according to the STROBE reporting guidelines.
The patients included in the study met the following criteria: (1) PTX was indicated because of SHPT of renal origin (persistent serum i-PTH concentration > 800 pg/mL, lack of response to medical therapy, severe symptoms, severe osteoporosis and skeletal deformity, and more than one enlarged parathyroid gland with a diameter of ≥ 1 cm and rich blood supply on preoperative ultrasonographic examination); (2) preoperative CT examination data available; (3) successful PTX surgery performed, defined as ≥ 3 resected parathyroid glands and a serum i-PTH concentration < 60 pg/mL 1–3 days after surgery [19].
The exclusion criteria were as follows: (1) biliary, pancreatic, or liver disease; (2) use of medications such as cinacalcet to treat SHPT of renal origin within the 6 months preceding surgery; (3) a second PTX, required because of recurrent SHPT following the initial PTX; (4) incomplete medical records; (5) comorbid papillary thyroid carcinoma, diagnosed in patients that were surgically treated for SHPT; (6) incomplete resection of the parathyroid glands (fewer than three resected parathyroid glands) or ineffective PTX surgery (serum i-PTH ≥ 60 pg/mL 1–3 days after surgery); and (7) parathyroid carcinoma, identified on postoperative histologic examination. A flow chart for the patient selection process is shown as Fig. 1.
Collection of data from medical records
The participants’ age, sex, body mass, duration and modality of dialysis, co-morbidities, preoperative drug therapies (including vitamin D analogues and phosphate binders), laboratory data, details of surgery, preoperative CT imaging data, and histologic findings were retrospectively collected.
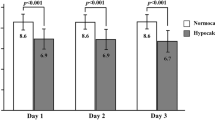
Preoperative laboratory data were obtained that included the following: hemoglobin, serum albumin, ALP activity, blood urea nitrogen (BUN), serum creatinine, serum Ca, serum potassium (K), phosphorus (P), magnesium (Mg), and i-PTH. The serum concentration of Ca was measured every 4–6 h for the first 48–72 h after surgery and then twice daily until stable. The other laboratory data, including ALP, K, P, Mg, and i-PTH were measured on 4 consecutive days during hospitalization. (Table 1).
Surgical procedures
All the surgical procedures were performed by a dedicated endocrine surgeon under general anesthesia. Subtotal parathyroidectomy (s-PTX), total parathyroidectomy without auto-transplantation (TPTX), or total parathyroidectomy with auto-transplantation (TPTX + AT) were performed on the participants in the present study. According to the consensus report of the European Society of Endocrine Surgeons [2], s-PTX is defined as the resection of approximately three-and-a-half parathyroid glands, leaving between 40 and 80 mg of the most normal-appearing, well-vascularized parathyroid gland in situ. For autotransplantation, the most normal-appearing gland was minced into 10–20 1-mm3 pieces for reimplantation in the non-dominant forearm.
All the participants underwent bilateral neck exploration, in an attempt to identify all the parathyroid glands. When four or more glands were identified at the time of surgery, the choice of procedure principally depended upon the preference of the surgeon. If three parathyroid glands were identified, all the identifiable parathyroid glands were removed and autotransplantation was not performed.
Standard supportive treatment
After surgery, all the participants were empirically treated with an intravenous infusion of 50 mL 10% calcium gluconate on both the day of surgery and the first day following surgery. If the serum calcium concentration was < 2.1 mmol/L, an additional volume of 5% calcium gluconate solution was administered intravenously. The transfusion speed of the calcium gluconate solution was adjusted according to the serum calcium concentration during subsequent monitoring. All the participants started to take active vitamin D sterols at a dose of 0.5 µg twice a day and calcium carbonate at a dose of 1200 mg twice a day on the first day following surgery. The intravenous calcium administration was gradually reduced and the participants were discharged when their serum calcium concentrations were stable and within the normal range, without the need for intravenous calcium supplementation, and they showed no symptoms of hypocalcemia or other surgery-related complications.
Definition of postoperative hypocalcemia
Postoperative hypocalcemia was defined as a minimum Ca concentration < 2.1 mmol/L within the 4 days following surgery, despite standard supportive treatment. This cut-off value for serum calcium was the same as that used by Yifei et al., Witteveen et al. and others [4, 5, 8, 16, 19, 20].
Evaluation of parathyroid calcification
All preoperative CT examinations were performed using a multi-detector, 64-row CT scanner (750HD GE Healthcare, Chicago, IL, USA). Due to the condition of chronic renal failure, all patients undergone conventional CT without contrast. The scans began at the hard palate and continued to the manubrium of the sternum. The imaging parameters were: tube voltage, 120 kVp; gantry rotation speed, 0.6 s; and maximum allowable tube current, 500 mA. The CT scan data were collected in the Digital Imaging and Communications in Medicine format and were analyzed using post-processing software (3D slicer, Harvard, Version 4.81 (slicer.org)). Parathyroid calcification was defined as hyperdensity (> 130 Hounsfield Units (HU)) within the region of the parathyroids on CT images. The presence of parathyroid calcification was recorded by surgeon Xinzeng Sun, who has > 10 years’ experience in endocrine surgery. Histologic examination was used to check the intraoperative identification of parathyroid calcification. Figure 2 and the Supplemental Video show the parathyroid calcification on CT and histologically.
Statistical analysis
Continuous data are expressed as mean ± standard deviation and categorical data are expressed as frequency and percentage. Continuous datasets were compared using Student’s t test or the Mann–Whitney U test, as appropriate, and categorical datasets were compared using the chi-square test or Fisher’s exact test. Intra-class correlation coefficients (ICCs) were used to evaluate the repeatability of the detection of calcified parathyroids using CT and histologic examination. ICCs > 0.8 were considered to indicate excellent agreement. All the factors considered were subjected to univariable analysis, and those associated with postoperative hypocalcemia (P < 0.05) on univariable analysis, those shown in the literature to be relevant, and those with a P value of < 0.20 on univariable analysis were included in a multivariable model to identify independent predictors. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to evaluate the strength of the association between each variable and the development of postoperative hypocalcemia. Receiver-operating characteristic (ROC) analysis was used to determine the optimal cut-off values for the significant factors and to evaluate the utility of each of these for the prediction of postoperative hypocalcemia. The value closest to the top-left part of each ROC curve was selected. All the statistical analyses were performed using IBM SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA). All the tests were two-sided and statistical significance was defined as P < 0.05.
Results
Patient demographics
After applying the inclusion and exclusion criteria, data were available for 106 (age 50.00 ± 11.20 years) of 120 patients with SHPT who underwent PTX during the study period. Postoperative hypocalcemia was identified in 33 participants (31.3%). The age, sex, body mass, preoperative symptoms, dialysis modality, preoperative drug therapies and comorbidities were not associated with postoperative hypocalcemia (all P > 0.05). The duration of dialysis in participants who did not experience postoperative hypocalcemia was 92.32 ± 46.02 months, which was not significantly different from that in the participants who did (111.58 ± 70.69 months) (P = 0.10) (Table 1).
Univariate analysis of factors potentially favoring postoperative hypocalcemia
Assessment of the preoperative laboratory test results showed no significant differences in creatinine, BUN, glucose, uric acid, bilirubin, K, or Mg between participants who did or did not experience postoperative hypocalcemia (all P > 0.05). In contrast, hemoglobin, albumin, ALP, i-PTH, and Ca appeared to be predictive of postoperative hypocalcemia. As shown in Table 2, the participants that experienced postoperative hypocalcemia had lower hemoglobin (102.73 ± 14.75 vs. 110.21 ± 17.46 g/L, P = 0.035), lower preoperative serum Ca (2.22 ± 0.18 vs. 2.35 ± 0.20 mmol/L, P < 0.001), higher i-PTH (2,618.33 ± 1,135.41 vs. 1,567.09 ± 648.79 pg/ml, P < 0.001), and higher ALP (552.70 ± 416.50 vs. 223.24 ± 185.61 U/L, P < 0.001) than those who did not.
Twenty-eight participants with calcified parathyroids were initially identified using CT. Histologic examination showed that two of these participants had calcification of other tissues, and were, therefore, excluded from this group, and one additional participant showed parathyroid calcification on histologic examination, and was, therefore, added, yielding a total of 27. The ICC coefficient was 0.944, which implied excellent agreement between the two methods. The prevalence of parathyroid calcification in participants who experienced postoperative hypocalcemia group was 51.5% (17 out of 33 patients), which was significantly higher than that in participants who did not (13.7%, 10 out of 73 patients) (P < 0.001) (Table 1).
Three types of procedure were performed in the present study: s-TPX, TPX, and TPX + AT. Analysis of the prevalence of postoperative hypocalcemia according to the procedure performed showed no significant differences according to the procedure performed of the number of parathyroids dissected (all P > 0.05) (Table 1).
Multivariate analysis of factors potentially favoring postoperative hypocalcemia
The multivariable analysis showed that the following parameters were independent predictors of postoperative hypocalcemia: preoperative ALP activity (OR = 1.003, 95% CI 1.000–1.006; P = 0.025), serum Ca (OR = 0.006, 95% CI 0.0001–0.171; P = 0.003), i-PTH (OR = 1.001, 95% CI 1.000–1.002; P = 0.019), and parathyroid calcification (OR = 8.452, 95% CI 2.317–30.835; P = 0.001) (Table 2).
Subsequently, ROC curves were separately constructed for preoperative ALP, serum Ca, i-PTH, and parathyroid calcification. The areas under curves (AUCs) for these potential risk factors were 0.82 (95% CI 0.738–0.903; P < 0.001), 0.60 (95% CI 0.699–0.900; P = 0.107), 0.80 (95% CI 0.699–0.900; P < 0.001), and 0.70 (95% CI 0.584–0.813; P = 0.001), respectively (Fig. 3). Furthermore, an i-PTH cut-off of ≥ 2,104 pg/mL (sensitivity 72.73% and specificity 82.19%) and an ALP cut-off of ≥ 242.9 U/L (sensitivity 81.82% and specificity 73.24%) were found to predict postoperative hypocalcemia.
Discussion
The management of patients with SHPT after PTX remains challenging because of the requirement to prevent and immediately correct postoperative hypocalcemia. Previous studies have attempted to identify clinical factors that predict the development of postoperative hypocalcemia, but the results have been inconclusive, principally because of differing definitions of postoperative hypocalcemia (serum Ca concentrations of 1.78, 1.87, 2.0, or 2.1 mmol/L, with or without correction for albumin concentration; duration of postoperative hospital stay; or the level of intravenous calcium supplementation); which creates difficulties in their interpretation. In the current study, we favored postoperative hypocalcemia, defined as < 2.1 mmol/L within the first 4 days postoperatively. The two main reasons for this are as follows. First, the threshold value of 2.1 mmol/L was consistent with the reference to normal laboratory calcium levels. In addition, this threshold value was adopted by many previous studies and also recommended by the recently published guidelines of the American Association of Endocrine Surgeons [21]. Secondly, calcium levels always reached their lowest point between 48 and 72 h postoperatively [21]. Therefore, a postoperative observation window of 4 days may be optimal and sufficient to see the corresponding changes in calcium levels.
Three major risk factors have been identified among the typically measured laboratory parameters. First, high ALP activity is widely recognized to be associated with postoperative hypocalcemia because of an imbalance between osteoclast and osteoblast activity. Osteoclast activity significantly decreases after hyperparathyroidism surgery because of a sudden decrease in i-PTH concentration, whereas osteoblast activity is not significantly affected. Therefore, bone metabolism is disrupted, and this may contribute to the development of hypocalcemia after surgery. The results of the univariable and multivariable analyses conducted in the present study are consistent with this. Furthermore, patients with preoperative serum ALP activities > 242.9 IU/L were identified as being at a high risk of postoperative hypocalcemia, with a sensitivity of 81.82% and a specificity of 73.24%. This value is comparable with the cut-off value (208.9 U/L) obtained in the study by Wen et al. [14].
Second, low serum Ca concentration was identified as another independent risk factor for postoperative hypocalcemia in the present study, which is also in accordance with the findings of previous studies [8, 19, 20], 12, 14, 16, 22, 23. This can be explained by the rapid movement of calcium from the circulation into the bone and extensive bone remineralization because of the abrupt decrease in i-PTH. However, the ROC analysis did not identify a serum Ca concentration that should be maintained in patients, and therefore further investigation is required.
Third, in the present study, we have shown that high preoperative i-PTH concentration favors the development of postoperative hypocalcemia, which is consistent with the findings of previous studies [5, 8, 12, 14, 20, 23]. In particular, patients with preoperative serum i-PTH concentrations > 2104 pg/mL may need intensive care to prevent postoperative hypocalcemia. Preoperative i-PTH concentration is generally related to the severity of renal osteodystrophy. Therefore, a positive association between high preoperative serum i-PTH and postoperative hypocalcemia would be expected. However, paradoxically, some other studies did not show that i-PTH concentration is predictive of postoperative hypocalcemia, which might be ascribed to the inclusion of multiple variables that prevented the identification of significant statistical relationships [6, 9, 16, 24].
In contrast to the evidence generated by the laboratory parameters, the image features or morphology performances of the parathyroid glands were evaluated, and a novel association between the calcification of the parathyroid glands and early hypocalcemia following PTX was identified. In the multivariable logistic regression analysis, we found that, compared with participants who did not show parathyroid calcification, those who did were at a substantially higher risk of postoperative hypocalcemia (8.45 times). The biggest advantage of using this factor is the avoidance of the need to assess changes in preoperative laboratory parameters, which can be affected by dialysis, and most of the previous reports did not specify the timing of measurement of these laboratory parameters. Thus, this relatively stable radiologic parameter may represent a more accurate predictor. It is not difficult to differentiate calcified parathyroids, with high CT values, from the surrounding tissue on preoperative CT, and the accuracy of identification of parathyroid calcification by CT is acceptable and shows excellent agreement with the histologic assessment. Although preoperative concurrent single photon emission computed tomography-computerized tomography (SPECT/CT) and ultrasonography were not assessed in the present study, we believe that our findings would also be applicable to these imaging modalities because the calcified lesions can also be easily identified in these ways. Therefore, calcification of the parathyroids represents a radiological predictor of postoperative hypocalcemia following PTX.
Previous studies have shown parathyroid calcification in patients [17, 18], but none have measured the prevalence of this or assessed the use of imaging of the parathyroids for the prediction of postoperative hypocalcemia. In the present study, calcification of the parathyroids was shown to have a relatively high incidence: almost 25% (27 out of 106) of participants with SHPT developed parathyroid calcification. This may be because of long-term dialysis, the severity of SHPT, or a result of ectopic calcification. Interestingly, the number of calcified parathyroids and the location of the calcification in the parathyroids varied among the participants: calcification was found to surround or to occur within the parathyroids. The detailed mechanism of this mineralization requires further analysis.
The present study had several limitations. First, it was subject to the standard limitations of a retrospective study. Several other parameters that might be predictors of postoperative hypocalcemia were not routinely measured. Other factors, such as bone mineral density, serum vitamin D concentration, parathyroid mass, and other parameters of parathyroid morphology should be included in future studies, to reduce confounding. Second, changes in serum calcium levels after hospital discharge were not obtained due to a lack of long-term follow-up. And the sample size was relatively small and potentially important associations between variables may have been obscured. Third, in the present study we used a strict criterion (< 2.1 mmol/L during the first 4 postoperative days), but a consistent method for the evaluation of postoperative hypocalcemia should be established in the future. Furthermore, the empirical use of intravenous Ca support after surgery may have concealed potential hypocalcemia in the participants and may reduce the generalizability of the present findings to other centers. Nevertheless, our findings are comparable to those of previous studies and we have made the novel finding that parathyroid calcification is a predictor of postoperative hypocalcemia.
Conclusion
In this retrospective study conducted at a single center, we have shown that patients with high preoperative ALP activity or i-PTH concentration, low serum Ca, or calcification of the parathyroids are more likely to experience postoperative hypocalcemia. To better identify patients with a high risk of postoperative hypocalcemia, we have identified optimal cut-off values for ALP and i-PTH. Parathyroid calcification was demonstrated to be associated with a high risk of postoperative hypocalcemia for the first time, and this may become a useful radiologic predictor of postoperative hypocalcemia. The early identification of these risk factors should improve patient outcomes and satisfaction.
References
Steinl GK, Kuo JH (2021) Surgical management of secondary hyperparathyroidism. Kidney Int Rep 6(2):254–264
Lorenz K, Bartsch DK, Sancho JJ, Guigard S, Triponez F (2015) Surgical management of secondary hyperparathyroidism in chronic kidney disease—a consensus report of the European Society of Endocrine Surgeons. Langenbecks Arch Surg 400(8):907–927
Goldfarb M, Gondek SS, Lim SM, Farra JC, Nose V, Lew JI (2012) Postoperative hungry bone syndrome in patients with secondary hyperparathyroidism of renal origin. World J Surg 36(6):1314–1319
Witteveen JE, van Thiel S, Romijn JA, Hamdy NA (2013) Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol 168(3):R45-53
Kritmetapak K, Kongpetch S, Chotmongkol W, Raruenrom Y, Sangkhamanon S, Pongchaiyakul C (2020) Incidence of and risk factors for post-parathyroidectomy hungry bone syndrome in patients with secondary hyperparathyroidism. Ren Fail 42(1):1118–1126
Ko WC, Liu CL, Lee JJ, Liu TP, Wu CJ, Cheng SP (2020) Osteocalcin is an independent predictor for hungry bone syndrome after parathyroidectomy. World J Surg 44(3):795–802
Kang BH, Hwang SY, Kim JY, Hong YA, Jung MY, Lee EA et al (2015) Predicting postoperative total calcium requirements after parathyroidectomy in secondary hyperparathyroidism. Korean J Intern Med 30(6):856–864
Wang M, Chen B, Zou X, Wei T, Gong R, Zhu J et al (2020) A nomogram to predict hungry bone syndrome after parathyroidectomy in patients with secondary hyperparathyroidism. J Surg Res 255:33–41
Liu J, Huang Q, Yang M, Huang L, Zhang L (2020) Risk factors predicting severe hypocalcemia after total parathyroidectomy without autotransplantation in patients with secondary hyperparathyroidism. J Int Med Res 48(1):300060519897505
Yang G, Ge Y, Zha X, Mao H, Wang N, Xing C (2019) Peritoneal dialysis can alleviate the clinical course of hungry bone syndrome after parathyroidectomy in dialysis patients with secondary hyperparathyroidism. Int Urol Nephrol 51(3):535–542
Stefanova D, Ullmann TM, Limberg J, Moore M, Beninato T, Zarnegar R et al (2020) Risk factors for prolonged length of stay and readmission after parathyroidectomy for renal secondary hyperparathyroidism. World J Surg 44(11):3751–3760
Tsai WC, Peng YS, Chiu YL, Wu HY, Pai MF, Hsu SP et al (2015) Risk factors for severe hypocalcemia after parathyroidectomy in prevalent dialysis patients with secondary hyperparathyroidism. Int Urol Nephrol 47(7):1203–1207
Ding Y, Wang H, Zou Q, Jin Y, Zhang Z, Huang J (2018) Factors associated with calcium requirements after parathyroidectomy in chronic kidney disease patients. Int Urol Nephrol 50(3):535–540
Wen P, Xu L, Zhao S, Gan W, Hou D, Zhang L et al (2021) Risk factors for severe hypocalcemia in patients with secondary hyperparathyroidism after total parathyroidectomy. Int J Endocrinol 2021:6613659
Ge P, Liu S, Sheng X, Li S, Xu M, Jiang J et al (2018) Serum parathyroid hormone and alkaline phosphatase as predictors of calcium requirements after total parathyroidectomy for hypocalcemia in secondary hyperparathyroidism. Head Neck 40(2):324–329
Ho LY, Wong PN, Sin HK, Wong YY, Lo KC, Chan SF et al (2017) Risk factors and clinical course of hungry bone syndrome after total parathyroidectomy in dialysis patients with secondary hyperparathyroidism. BMC Nephrol 18(1):12
Ford EJ, Chandran PKG, Graefe HH (1991) Parathyroid calcification as a complication of secondary hyperparathyroidism. Nephron 57:498–499
Peces R, RodrõÂguez M, GonzaÂlez F, Ablanedo P (2001) Calcification of all four parathyroid glands in a hemodialysis patient with secondary hyperparathyroidism revealed by computerized tomography. Scand J Urol Nephrol 35:328–329
Ge Y, Yang G, Wang N, Zha X, Yu X, Mao H et al (2019) Bone metabolism markers and hungry bone syndrome after parathyroidectomy in dialysis patients with secondary hyperparathyroidism. Int Urol Nephrol 51(8):1443–1449
Wong J, Fu WH, Lim ELA, Ng CFJ, Choong HL (2020) Hungry bone syndrome after parathyroidectomy in end-stage renal disease patients: review of an alkaline phosphatase-based treatment protocol. Int Urol Nephrol 52(3):557–564
Dream SKL, Kuo JH et al (2022) The American Association of Endocrine Surgeons Guidelines for the definitive surgical management of secondary and tertiary renal hyperparathyroidism. Ann Surg 276(3):e141–e176
Torer N, Torun D, Torer N, Micozkadioglu H, Noyan T, Ozdemir FN et al (2009) Predictors of early postoperative hypocalcemia in hemodialysis patients with secondary hyperparathyroidism. Transpl Proc 41(9):3642–3646
Sun X, Zhang X, Lu Y, Zhang L, Yang M (2018) Risk factors for severe hypocalcemia after parathyroidectomy in dialysis patients with secondary hyperparathyroidism. Sci Rep 8(1):7743
Tan PG, Ab Hadi IS, Zahari Z, Yahya MM, Wan Zain WZ, Wong MP et al (2020) Predictors of early postoperative hypocalcemia after total parathyroidectomy in renal hyperparathyroidism. Ann Surg Treat Res 98(1):1–6
Acknowledgements
We thank Mark Cleasby, PhD from Liwen Bianji (Edanz) (www.liwenbianji.cn) for editing the language of a draft of this manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study conception and design: LC, XS and JB; acquisition of data: TZ, YN and HS; analysis and interpretation of data ZZ and CW; drafting of manuscript LC and XS; critical revision of manuscript JB.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Human participants and/or animals and Informed consent
This study was approved by the local ethics committee. Written informed consent was obtained from all the participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 2886 KB)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, L., Sun, X., Zhang, T. et al. A reappraisal of risk factors for early hypocalcemia after parathyroidectomy in dialysis patients. Updates Surg 74, 1961–1970 (2022). https://doi.org/10.1007/s13304-022-01395-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01395-2