Abstract
The employment of laparoscopic gastrectomy (LG) in the management of gastric cancer (GC) is increasing. Despite recent results from randomized trials, its effectiveness and oncological results in different scenarios remain controversial, especially in western centers. The aim of this study was to compare the short-term outcomes and survival of LG with open gastrectomy (OG) for GC. We reviewed all GC patients who underwent curative gastrectomy from a prospective database. Propensity score-matched (PSM) analysis including 10 variables was conducted to reduce patient selection bias using a 1:1 case–control match. A total of 530 GC were eligible for inclusion (438 OG and 92 LG). Older age, lower hemoglobin levels, total gastrectomy, larger tumor size, greater depth of tumor invasion and advanced pTNM stage was more frequent in the OG group. After PMS analysis, 92 patients were matched in each group. All variables assigned in the score were well matched. LG group had a slightly higher number of retrieved lymph nodes (42.3 vs 37.6), however, without reaching statistical significance (p = 0.072). No differences were recorded about the frequency of major postoperative complications (POC) and mortality rates between OG and LG groups (12% vs 15.2%, p = 0.519, respectively). In survival analysis, after matching, there was no difference in survival between the two groups. Multivariate analysis showed that only ASA and pN stage were independent factor associated with survival after PSM. In conclusion, laparoscopic gastrectomy was a safe and effective surgical technique for gastric cancer, with short-term and oncological outcomes comparable to open surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is the third most common cause of cancer-related mortality in the world [1]. Radical gastrectomy associated with lymph node dissection is considered the standard surgical treatment for locally advanced GC, and open gastrectomy (OG) remains the main surgical approach in the management of the disease [2, 3] .
In the last few years, the popularization of minimally invasive laparoscopic techniques has reached a rapid development. For some surgical procedures, laparoscopic method is currently preferred over open surgery, since some surgical short-term outcomes—such as earlier postoperative recovery, shorter hospital stay, alleviated pain, reduced blood loss and shorter time to resumption of oral intake—appear to be potential advantages of a less invasive procedure [4,5,6].
However, when it comes to laparoscopic gastrectomy (LG), a major concern regarding its safety and effectiveness is the achievement of an adequate lymphadenectomy. This part of the procedure is the cornerstone of surgical treatment and demands advanced expertise from surgeons [5, 7]. The non-compliance to D2 lymphadenectomy may favor short-term surgical outcomes, but impairs long-term oncological survival.
Several studies have shown comparable surgical outcomes and survival data between LG and OG for the treatment of GC [8, 9]. However, these studies are predominantly conducted in Asian countries, in large centers, where extensive experience is available [8, 10]. Furthermore, GC in western countries is usually diagnosed at a more advanced stage in patients with a different profile [10, 11]. Accordingly, data on surgical and oncological outcomes of LG that reflect the reality of Western countries, including stages II and III, are still required [8, 12, 13].
Thus, the aim of this study was to evaluate the short-term surgical outcomes and survival of patients who underwent laparoscopic gastrectomy (LG) for GC compared with open gastrectomy (OG) in a single western cancer center.
Methods
All patients who underwent curative surgery for GC from 2009 to 2019 in our Institution were evaluated. Only histologically proven gastric adenocarcinoma and patients who underwent distal or total gastrectomy with lymphadenectomy (D1 or D2) were considered eligible.
The exclusion criteria were as follows: (1) remnant gastric cancer; (2) multivisceral resection; (3) robotic surgery; (4) conversion therapy; (5) emergency surgery; and (6) metastatic patients.
Clinical, surgical and pathological data were retrospectively reviewed from a prospective database maintained at our center. Comorbidities at the time of surgery were classified according to the Charlson Comorbidity Index (CCI), without the inclusion of age and neoplasia in the score, and American Society of Anesthesiologists classification (ASA) [14]. Postoperative morbidity was graded according to the Clavien–Dindo classification, in which grade III to V were defined as major postoperative complications (POC) [15]. Postoperative morbidity and mortality were defined as any event occurring within 30 days after surgery or during the hospital stay. Perioperative or adjuvant treatment was prescribed according to clinical indication (T3/T4 and/or N+) with platinum-based chemotherapy regimens. Tumor staging was performed according to 8th TNM edition [16].
All patients underwent preoperative staging, consisting of computed tomography or magnetic resonance imaging and upper digestive endoscopy with biopsy. Endoscopic ultrasonography was performed in selected cases. Laboratory tests were performed before surgery. Indications for surgery were defined based on pre-operative staging and multidisciplinary team meeting (medical oncologist, surgeon, radiologist and pathologist). The decision to perform laparoscopic was based on the surgeon´s decision during the meeting.
Total or distal gastrectomy was performed according to the location and size of the tumor to achieve a R0 resection. The extent of lymph node dissection (D1 or D2) was defined by the surgeon responsible for the case. All patients underwent gastrectomy with Roux-en-Y reconstruction. All procedures were performed according to the guidelines of Japanese Gastric Cancer Association (JGCA) [2] by an extensively experienced team.
For analysis, patients were divided into two groups according to the surgical approach: laparoscopic gastrectomy (LG) and open gastrectomy (OG). The main outcome of the study was the occurrence of major POC, followed by disease-free survival (DFS) and overall survival (OS). Mortality at 30 and 90 days were additional outcomes assessed as short-term results. To reduce the effect of patient selection bias between the two surgical approaches, we conducted a propensity score matching (PSM) analysis.
Patients were follow-up in the outpatient clinical visits according to a standard protocol, with visits every 3 months during the first year, every 6 months during the second and third years, and once a year thereafter. The study was approved by the institutional review board of our hospital and register (plataformabrasil.saude.gov.br; CAEE 62915516.2.0000.0065).
Statistical analysis
Data were expressed as mean (with standard deviation, SD ±) or median (interquartile ranges, IQR) for continuous variables and as numbers with percentages for categorical data. Continuous and categorical variables were compared between the two groups using the standard t test or Mann–Whitney test and Chi-square test, respectively.
Propensity scores were calculated by bivariate logistic regression, including the following variables that might be considered as potential confounders related to the selection to laparoscopic procedure between groups: age (< 65 vs ≥ 65 years), sex (female vs male), body mass index (BMI < 25 vs 25–30 vs > 30 kg/m2), American Society of Anesthesiologists classification (ASA I/II vs III/IV), comorbidity (CCI 0–1 vs ≥ 2), hemoglobin levels (≤ 11 vs > 11 g/dL, which represents the lower limit between mild and moderate anemia for men and women)[17], type of resection (distal vs total gastrectomy), tumor size (< 5 vs ≥ 5 cm), depth of tumor invasion (pT4 vs pT1–T3) and lymph node metastasis (pN0–N1 vs pN2–N3).
We matched propensity scores 1:1 with a caliper value of 0.01 (one-to-one nearest neighbor matching). The standardized difference (10% or 0.1) was used to compare the distribution of all paired covariates between treatment groups. Plots were built to compare the distribution of risk scores before and after matching.
Survival curves were assessed using the Kaplan–Meier method and compared using the log-rank test. Prognostic factors associated with survival were estimated by univariate and multivariable Cox proportional hazards model. Disease-free survival (DFS) was calculated from surgery to recurrence, death from any cause or last date of follow-up. Overall survival (OS) was the duration between surgical resection to death or last follow-up.
All statistical tests were two-sided and p values < 0.05 were considered significant. Statistical analyses were carried out using SPSS software, version 20 (SPSS, Chicago, IL).
Results
In the analyzed period, 530 GC patients were eligible for inclusion. Mean age was 63.9 years (range 20–94.5 years), with male predominance of 305 cases. The mean BMI of patients at the time of surgery was 24.7 kg/m2 and 40% were classified as stage III. The median length of hospital stay for the entire population was 9 days (mean of 11.9 days, SD 9.1; range 4–63 days).
Among them, 438 (82.6%) patients underwent open gastrectomy (OG) and 92 (17.4%) underwent laparoscopic gastrectomy (LG). The characteristics of the two groups are demonstrated in Table 1. Older age, lower hemoglobin levels, total gastrectomy, larger tumor size, greater depth of tumor invasion and advanced pTNM stage were more frequent in the OG group. The number of lymph nodes retrieved was similar between the two groups. In OG and LG, 13.5% and 6.5% of patients received neoadjuvant chemotherapy, respectively (p = 0.065). Considering the postoperative morbidity, there were no statistical differences between OG and LG groups (p = 0.837). The median hospital stay and mortality rate were also similar between open and laparoscopic approach (Table 2).
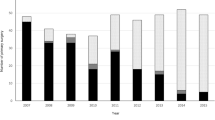
After a propensity score model estimated using the 10 variables previously described, 92 patients were stratified for each group. A flow chart of patient selection scheme is demonstrated in Fig. 1. Histograms of propensity score distribution before and after PSM are presented in Fig. 2.
As a result of the PSM, OG and LG groups were similar for all variables assigned in the score (Table 1). In addition, pN status was perfectly superimposable between the two groups (p = 1.0). Neoadjuvant therapy was administered to 6.5% of patients in both groups (p = 1.0). Only Lauren's diffuse type and poorly differentiated GC were more common in the LG group (p = 0.039 and p = 0.005, respectively). LG group had a slightly higher number of retrieved lymph nodes (42.3 vs 37.6), however, without reaching statistical significance (p = 0.072). TNM stage was comparable between groups.
In relation to the postoperative outcomes, no statistical differences were recorded about the frequency of major POC (p = 0.519). Considering the type of complication, the frequency of clinical and surgical POC was also similar between the groups (Table 2).
The frequency of major POC in the LG group considering the subgroups distal and total gastrectomy was 15.7% and 13.6%, respectively. Regarding the stage of the disease, the frequency of major POC in patients who underwent LG with early gastric cancer (EGC) and advanced gastric cancer (AGC) was 11.4% and 18.8% respectively. Furthermore, the rate of major POC complication was higher in patients with AGC who underwent total gastrectomy (23.1%) (Supplementary Table 2).
The mortality rate at 30 and 90 days was the same in both groups (p = 1.0). The median length of hospital stay was 8 days for both OG and LG group (IQR 6–12 and IQR 5–11.75, respectively) (p = 0.802).
Survival analysis
The median follow-up period for all patients included in the study was 31 months (range 0.1–119.7). Disease recurrence occurred in 105 (19.8%) patients, and 182 (34.3%) patients died. The predicted overall survival for the entire cohort was 57%.
Survival curves before and after PSM are presented in Fig. 3. Patients treated by laparoscopic approach had better OS than OG group (p = 0.033). After matching, there was no difference in DFS and OS between the two groups (p = 0.933 and p = 0.737 respectively).
In the analysis of factors associated with survival after PSM and adjusting for potential confounding variables, ASA category and pN stage were factors significantly associated with DFS and OS in multivariate model (Table 3). ASA category revealed higher hazard of death than pN status, while lymph node status had the higher hazard ratio in DFS analysis.
Discussion
In this retrospective analysis, a cohort of early and advanced GC patients was evaluated to verify if LG can achieve similar short-term surgical and oncological outcomes compared to those who underwent OG. Proximal and distal tumors were included. We applied the propensity score matching to minimize the impact of confounding variables on patient selection and prognosis between the two surgical methods. As result, our findings demonstrated that LG is safe and effective in short-term outcomes for patients with GC, with oncological results comparable to OG.
Currently, there are still debates if the LG is superior, or at least non-inferior, compared to OG for GC patients. Characteristics related to the origin of the studies, as well as the inclusion criteria, contribute to this scenario. Most studies regarding LG are carried out in China, Japan and Korea, in centers with great volume of GC, which provides a faster learning curve and extensive experience in this technique [18,19,20]. As example, in a study including only laparoscopic distal gastrectomy, learning curve was considered to be complete after 60–90 operations, a number that is hardly reached annually for all GC resections in a western center [21].
Randomized clinical trials design usually separate gastric tumors in “EGC vs AGC” and in “proximal vs distal” gastrectomy. Due to greater technical simplicity, mainly related to the proximal anastomosis, most of the actual evidences are related to distal tumors [4, 6, 13, 19]. In this sense, the KLASS-01 trial demonstrated that short-term surgical complication rate were significantly lower for LG group compared OG for distal EGC (13.0% vs 19.9%, p = 0.001) [4]. In our cohort, 14.3% of EGC who underwent distal LG had major POC. Further survival analysis of the trial confirmed the non-inferiority after 5 years establishing LG as the preferred option for distal EGC [19].
Meanwhile, for distal gastrectomy in AGC, trials from South Korea (KLASS-02), China (CLASS-01) and Japan (JLSSG0901) have recently been published. [20, 22, 23] Once again, short-term surgical outcomes and survival were equivalents between groups. The 3-year DFS rate in KLASS-02 trial was 81.3% and 80.3% for open and laparoscopic group [23]. With regard to POC, the rate of early complications in LG compared to OG group from KLASS-02 was 15.7% and 23.4%, respectively (p = 0.027), with a lower frequency of late complications also associated with the LG group (4.7% vs 9.5%, p = 0.0038) [23]. In our analysis, we found a rate of 17.1% of major POC after distal gastrectomy for AGC in the laparoscopic group.
Sustainable data regarding the viability of laparoscopic technique for total gastrectomy are scarcer. Considering only clinical stage I GC and short-term surgical results, the single-arm trial (JCOG1401) [18] evaluated its safety and found that the overall frequency major adverse events were 29% [18]. In the same way, the overall morbidity and mortality rates for stage I GC reported by CLASS-02 trial was 19.1% in the LG group and 20.2% in the OG group, which was not significantly different [24]. Regarding AGC, a multicenter randomized controlled trial (KLASS-06) is being conducted but the results will only be completed in 2027.
As expected, in our study, AGC treated with total LG had the highest morbidity rate compared to the other subgroups. These findings are similar to a previous report conducted in a cohort of Western patients, where minimally invasive surgery demonstrated benefits only for distal gastrectomy, with higher rate of anastomotic leakage for total LG compared to open approach [25]. These results highlight the technical challenge of LG for proximal tumors [26].
Besides surgical volume, another difficulty in extrapolating the results of eastern trials are also related to patients characteristics [12]. In Western countries, GC is usually diagnosed at more advanced stages, which impacts survival [12]. As opposite, Nationwide screening programs in Japan and Korea cause GC to be diagnosed in earlier stages. The incidence of proximal tumors is higher in the west and, consequently, a higher frequency of total gastrectomy is required. Patient characteristics, such as age and body mass index (BMI), are higher in the Western population—all factors that hinder the performance of the laparoscopic technique. [12, 13, 27] In our study, the mean BMI for patients in LG was 24.8 kg/m2, while in Eastern reports, the mean BMI reported for patients who underwent minimally invasive gastrectomy was 22.3 kg/m [12]. To overcome these differences, a randomized controlled trial (LOGICA trial) [28] from the Netherlands is underway. It predicts the inclusion of 210 patients with resectable GC (cT1-4a, N0-3b, M0) to compare LG and OG, but short-term and long term outcomes are still not available.
As expected, in our cohort before the PSM, patients who underwent OG had larger tumor, with more advanced stage, and higher rate of total gastrectomy. Although not significant, patients also had a higher incidence of comorbidities. Such differences are attributed to the selection of more favorable patients for the laparoscopic procedure. However, after PSM, the groups were equivalent for all clinical and pathological variables, in addition to those chosen for the score.
A major issue related to LG refers to the number of lymph nodes retrieved in relation to OG. As previously exposed, the non-compliance to D2 lymphadenectomy may favor short-term surgical outcomes, since dissection along the vascular trunks may cause iatrogenic injuries and local complications, such as fluid collections and pancreatic fistula. However, in a long-term survival analysis it will impair survival. Most trials report no differences in number of retrieved lymph nodes between LG and OP. However, the randomized trials are mostly performed for EGC [29]. Other studies demonstrated a decreased number of harvested lymph nodes for GC patients during LG compared with OG [4, 30]. Although it seems unclear whether compliance to D2 dissection in LG is comparable to that in open surgery, in our study there was no difference of retrieved lymph nodes between LG and OG groups. Interestingly, even after PSM, the mean number of retrieved lymph nodes was similar—being even higher in the LG group. Accordingly, together with clinical, pathological and surgical characteristics, the analysis after the PSM highlighted that both approaches had similar survival rates.
Some limitations of this study must be raised. Although we used PSM, there may still be the influence of selection bias due to its retrospective design rather than a prospective randomized controlled trial. Some patients had insufficient follow-up time, so a complete 5-year OS or 3-year DFS analysis could not be demonstrated. In addition, due to the small number of LG patients, pre-planned statistical analyzes of specific subgroups were not feasible. Even so, we presented these subgroup analysis comparing EGC vs AGC and distal vs proximal tumors as supplementary material. In addition, our cohort included learning curve surgeries, since the number of necessary LG to overcome this phase is difficult to define and achieve. [21]
Nevertheless, as strengths, we included in the propensity score variables that affect both treatment selection and the outcomes in detail. Previous reports indicated that older age, comorbidities, and high BMI contributed to increased morbidity after gastrectomy [27, 31]. The other chosen surgical and pathological variables for PSM are already recognized as prognostic factors [11]. As the proportion of patients in OG group was much higher than LG in our cohort, it was possible to match all patients in the PS analysis. In conformity, this also demonstrated that the cases submitted to LG in our institution more accurately reflect the profile of GC who undergoes surgical treatment. This ensures that the results presented in this reported can be more easily compared to what is evidenced in daily surgical practice outside a clinical trial design. In the end it was possible to include the expressive number of 194 GC patients after PSM in the analysis which comprises 23.9% of total LG and 48.9% of AGC. The fact that it is a single center study guarantees uniformity in perioperative care and standardization of treatment without being dependent on the experience of only one surgeon.
As new results from prospective trials are made available, the use of laparoscopic technique has been confirmed as a safe and effective option in the surgical treatment of GC. Nonetheless, due its technical complexity and heterogeneity of populations, reports of LG results in different scenarios are still required to ensure external validity.
Conclusion
In conclusion, laparoscopic gastrectomy was a safe and effective surgical technique for stage I–III gastric cancer, with short-term outcomes comparable to open surgery. Survival analysis also did not differ between the LG and OG groups.
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Japanese Gastric Cancer A (2017) Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 20(1):1–19. https://doi.org/10.1007/s10120-016-0622-4
Barchi LC, Ramos MFKP, Dias AR, Andreollo NA, Weston AC, Lourenço LG, Malheiros CA, Kassab P, Zilberstein B, Ferraz ÁAB, Charruf AZ, Brandalise A, Silva AMd, Alves B, Marins CAM, Leite CV, Bresciani CJC, Szor D, Mucerino DR, Wohnrath DR, Ilias EJ, Martins Filho ED, Lopasso FP, Coimbra FJF, Felippe FEC, Tomasisch FDS, Takeda FR, Ishak G, Laporte GA, Silva HJT, Cecconello I, Rodrigues JJG, Grande JCD, Motta LMD, Ferraz LR, Moreira LF, Lopes LR, Toneto MG, Mester M, Rodrigues MAG, Carvalho MPd, Franciss MY, Forones NM, Corletta OC, Yagi OK, Castro OAP, Malafaia O, Assumpção PP, Savassi-Rocha PR, Colleoni Neto R, Oliveira RJD, Sallun RAA, Weschenfelder R, Oliveira SCVD, Abreu TBd, Castria TBD, Ribeiro Junior U, Barra W, Costa Júnior WLD, Freitas Júnior WRD (2020) II Brazilian consensus on gastric cancer by the Brazilian gastric cancer association. ABCD Arquivos Brasileiros de Cirurgia Digestiva 33(2):e1514. https://doi.org/10.1590/0102-672020190001e1514
Kim W, Kim HH, Han SU, Kim MC, Hyung WJ, Ryu SW, Cho GS, Kim CY, Yang HK, Park DJ, Song KY, Lee SI, Ryu SY, Lee JH, Lee HJ (2016) Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: short-term outcomes from a multicenter randomized controlled trial (KLASS-01). Ann Surg 263(1):28–35. https://doi.org/10.1097/sla.0000000000001346
Ramos M, Barchi LC, Weston AC, Zilberstein B (2019) Minimally invasive surgery for gastric cancer: paradigm shift. Arquivos Brasileiros de Cirurgia Digestiva ABCD 32(4):e1483. https://doi.org/10.1590/0102-672020190001e1483
Zhang CD, Yamashita H, Zhang S, Seto Y (2018) Reevaluation of laparoscopic versus open distal gastrectomy for early gastric cancer in Asia: a meta-analysis of randomized controlled trials. Int J Surg (Lond, Engl) 56:31–43. https://doi.org/10.1016/j.ijsu.2018.05.733
Dias AR, Jacob CE, Ramos M, Pereira MA, Szor DJ, Yagi OK, Barchi LC, Ribeiro U Jr, Zilberstein B, Cecconello I (2019) Laparoscopic D2 gastrectomy for gastric cancer: mid-term results and current evidence. J Laparoendosc Adv Surg Tech A 29(4):495–502. https://doi.org/10.1089/lap.2018.0474
Zeng F, Chen L, Liao M, Chen B, Long J, Wu W, Deng G (2020) Laparoscopic versus open gastrectomy for gastric cancer. World J Surg Oncol 18(1):20. https://doi.org/10.1186/s12957-020-1795-1
Jiang L, Yang KH, Guan QL, Cao N, Chen Y, Zhao P, Chen YL, Yao L (2013) Laparoscopy-assisted gastrectomy versus open gastrectomy for resectable gastric cancer: an update meta-analysis based on randomized controlled trials. Surg Endosc 27(7):2466–2480. https://doi.org/10.1007/s00464-012-2758-6
Kassab P, da Costa Jr. WL, Jacob CE, Cordts RM, Castro OAP, Barchi LC, Cecconello I, Charruf AZ, Coimbra FJF, Cury AM, Diniz AL, de Farias IC, de Freitas Jr. WR, de Godoy AL, Ilias EJ, Malheiros CA, Ramos M, Ribeiro HSC, Roncon Dias A, Thuler FR, Yagi OK, Lourenco LG, Zilberstein B, Brazilian Gastric Cancer A (2017) Minimally invasive surgery for gastric cancer in Brazil: current status and perspectives-a report from the Brazilian Laparoscopic Oncologic Gastrectomy Group (BLOGG). Transl Gastroenterol Hepatol 2:45. https://doi.org/10.21037/tgh.2017.03.17
Ramos M, Pereira MA, Yagi OK, Dias AR, Charruf AZ, Oliveira RJ, Zaidan EP, Zilberstein B, Ribeiro-Junior U, Cecconello I (2018) Surgical treatment of gastric cancer: a 10-year experience in a high-volume university hospital. Clinics (Sao Paulo, Brazil) 73(suppl 1):e543s. https://doi.org/10.6061/clinics/2018/e543s
van der Wielen N, Straatman J, Cuesta MA, Daams F, van der Peet DL (2018) Short-term outcomes in minimally invasive versus open gastrectomy: the differences between East and West. A systematic review of the literature. Gastric Cancer 21(1):19–30. https://doi.org/10.1007/s10120-017-0747-0
Chevallay M, Jung M, Berlth F, Seung-Hun C, Morel P, Mönig S (2019) Laparoscopic surgery for gastric cancer: the European point of view. J Oncol 2019:8738502–8738502. https://doi.org/10.1155/2019/8738502
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Amin MB, Edge SB and Greene FL et al (eds) (2017) AJCC cancer staging manual, 8th ed. Springer, New York
World Health O (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization, Geneva
Katai H, Mizusawa J, Katayama H, Kunisaki C, Sakuramoto S, Inaki N, Kinoshita T, Iwasaki Y, Misawa K, Takiguchi N, Kaji M, Okitsu H, Yoshikawa T, Terashima M (2019) Single-arm confirmatory trial of laparoscopy-assisted total or proximal gastrectomy with nodal dissection for clinical stage I gastric cancer: Japan Clinical Oncology Group study JCOG1401. Gastric Cancer 22(5):999–1008. https://doi.org/10.1007/s10120-019-00929-9
Kim HH, Han SU, Kim MC, Kim W, Lee HJ, Ryu SW, Cho GS, Kim CY, Yang HK, Park DJ, Song KY, Lee SI, Ryu SY, Lee JH, Hyung WJ (2019) Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage I gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol 5(4):506–513. https://doi.org/10.1001/jamaoncol.2018.6727
Yu J, Huang C, Sun Y, Su X, Cao H, Hu J, Wang K, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Hu Y, Liu H, Zheng C, Li P, Xie J, Liu F, Li Z, Zhao G, Yang K, Liu C, Li H, Chen P, Ji J, Li G (2019) Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: the CLASS-01 randomized clinical trial. JAMA 321(20):1983–1992. https://doi.org/10.1001/jama.2019.5359
Zhang X, Tanigawa N (2009) Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomy-based analysis. Surg Endosc 23(6):1259–1264. https://doi.org/10.1007/s00464-008-0142-3
Inaki N, Etoh T, Ohyama T, Uchiyama K, Katada N, Koeda K, Yoshida K, Takagane A, Kojima K, Sakuramoto S, Shiraishi N, Kitano S (2015) A multi-institutional, prospective, phase II feasibility study of laparoscopy-assisted distal gastrectomy with D2 lymph node dissection for locally advanced gastric cancer (JLSSG0901). World J Surg 39(11):2734–2741. https://doi.org/10.1007/s00268-015-3160-z
Hyung WJ, Yang HK, Park YK, Lee HJ, An JY, Kim W, Kim HI, Kim HH, Ryu SW, Hur H, Kim MC, Kong SH, Cho GS, Kim JJ, Park DJ, Ryu KW, Kim YW, Kim JW, Lee JH, Han SU (2020) Long-term outcomes of laparoscopic distal gastrectomy for locally advanced gastric cancer: the KLASS-02-RCT randomized clinical trial. J Clin Oncol 38(28):3304–3313. https://doi.org/10.1200/jco.20.01210
Liu F, Huang C, Xu Z, Su X, Zhao G, Ye J, Du X, Huang H, Hu J, Li G, Yu P, Li Y, Suo J, Zhao N, Zhang W, Li H, He H, Sun Y, Chinese Laparoscopic Gastrointestinal Surgery Study G (2020) Morbidity and mortality of laparoscopic vs open total gastrectomy for clinical stage I gastric cancer: the CLASS02 multicenter randomized clinical trial. JAMA Oncol 6(10):1590–1597. https://doi.org/10.1001/jamaoncol.2020.3152
Gertsen EC, Brenkman HJF, Seesing MFJ, Goense L, Ruurda JP, van Hillegersberg R (2019) Introduction of minimally invasive surgery for distal and total gastrectomy: a population-based study. Eur J Surg Oncol 45(3):403–409. https://doi.org/10.1016/j.ejso.2018.08.015
Norero E, Vargas C, Achurra P, Ceroni M, Mejia R, Martinez C, Muñoz R, Gonzalez P, Calvo A, Díaz A (2019) Survival and perioperative morbidity of totally laparoscopic versus open gastrectomy for early gastric cancer: analysis from a single Latin American centre. Braz Arch Dig Surg 32(1):e1413. https://doi.org/10.1590/0102-672020180001e1413
Noshiro H, Shimizu S, Nagai E, Ohuchida K, Tanaka M (2003) Laparoscopy-assisted distal gastrectomy for early gastric cancer: is it beneficial for patients of heavier weight? Ann Surg 238(5):680–685. https://doi.org/10.1097/01.sla.0000094302.51616.2a
Haverkamp L, Brenkman HJ, Seesing MF, Gisbertz SS, van Berge Henegouwen MI, Luyer MD, Nieuwenhuijzen GA, Wijnhoven BP, van Lanschot JJ, de Steur WO, Hartgrink HH, Stoot JH, Hulsewé KW, Spillenaar Bilgen EJ, Rütter JE, Kouwenhoven EA, van Det MJ, van der Peet DL, Daams F, Draaisma WA, Broeders IA, van Stel HF, Lacle MM, Ruurda JP, van Hillegersberg R (2015) Laparoscopic versus open gastrectomy for gastric cancer, a multicenter prospectively randomized controlled trial (LOGICA-trial). BMC Cancer 15:556. https://doi.org/10.1186/s12885-015-1551-z
Eshuis WJ, van Berge Henegouwen MI, Draaisma WA, Gisbertz SS (2018) Compliance to D2 lymphadenectomy in laparoscopic gastrectomy. Updat Surg 70(2):197–205. https://doi.org/10.1007/s13304-018-0553-1
Ramagem CAG, Linhares M, Lacerda CF, Bertulucci PA, Wonrath D, Oliveira ATTD (2015) Comparison of laparoscopic total gastrectomy and laparotomic total gastrectomy for gastric cancer. ABCD Arquivos Brasileiros de Cirurgia Digestiva (São Paulo) 28:65–69
Ramos M, Pereira MA, Dias AR, Yagi OK, Zaidan EP, Ribeiro-Junior U, Zilberstein B, Cecconello I (2019) Surgical outcomes of gastrectomy with D1 lymph node dissection performed for patients with unfavorable clinical conditions. Eur J Surg Oncol 45(3):460–465. https://doi.org/10.1016/j.ejso.2018.11.013
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MFKPR and MAP study design, data retrieval, critical analysis, statistical analysis, draft of the manuscript. ARD data retrieval, review of the manuscript. UR Jr, BZ and SCN critical analysis, review of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
The study was approved by the hospital ethics committee and registered online (https://plataformabrasil.saude.gov.br; CAAE: 62915516.2.0000.0065).
Informed consent
Informed consent was waived by the local Ethics Committee in view of the retrospective nature of the study.
Human and animal rights
This study involved human research participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ramos, M.F.K.P., Pereira, M.A., Dias, A.R. et al. Laparoscopic gastrectomy for early and advanced gastric cancer in a western center: a propensity score-matched analysis. Updates Surg 73, 1867–1877 (2021). https://doi.org/10.1007/s13304-021-01097-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-021-01097-1