Abstract
The aim of this study is to evaluate the cost-effectiveness of different modifications of the trans-abdominal pre-peritoneal (TAPP) repair of groin hernia. Data were collected prospectively for all consecutive patients who underwent TAPP unilateral inguinal hernia repair between November 2017 and March 2019, and who completed a minimum of 1 year of follow-up. Costs and quality adjusted life year (QALY) gained were collected. Three TAPP variations were assessed: mesh fixation and peritoneal closure with staples (group 1); mesh fixation with fibrin glue and peritoneal closure with sutures (group 2); and mesh fixation and peritoneal closure with fibrin glue (group 3). A matched group of open repairs was established. The incremental cost-effectiveness ratio (ICER) and main intra-operative and post-operative outcomes were assessed. Overall 120 patients were included (group 1 n = 31; group 2 n = 27; group 3 n = 33; open group: 29). Operative time was shorter for groups 2 and 3, and the main post-operative outcomes were similar. The overall mean total cost of the open group (1185.95€) was lower compared with the laparoscopic group (group 1: 1682.39; group 2: 1538.54€; group 3: 1510.1€) (p = 0.026). However, the mean ICERs of groups 2 and 3 were significantly higher compared with group 1 (p = 0.021) and the open group (p = 0.032). At simulations analysis, the probability of cost-effectiveness was 33.32%, 36.26%, and 36.7% in TAPP groups 1, 2, and 3. In the long term, laparoscopic repair of groin hernia is cost-effective compared with open surgery. The use of fibrin glue for mesh fixation and/or for closing the peritoneum is the most cost-effective option and shortens operative times.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last decade, laparoscopic inguinal hernia repair has become very popular worldwide due to several advantages; in particular, faster recovery and reduced post-operative pain [1]. Since the description of the laparoscopic trans-abdominal pre-peritoneal (TAPP) repair, the technique has undergone several modifications, such as mesh type and fixation and method to approximate the peritoneum [1, 2].
Persistent post-operative pain after placement of staples to secure the mesh, along with the discovery of the “triangle of doom” and “triangle of pain”, has led to the recommendation to use few staples or to replace them with glue [1, 3]. This eliminates the risk of lateral cutaneous femoral nerve entrapment, which is the main cause of chronic pain. The same suggestions are extended to the closure of the peritoneum, favouring suture or glue over staples [4]. These modifications might increase the immediate costs of the procedure. However, apart from the clinical advantages, these may result in cost savings in the long term that only adequate cost-effectiveness analyses can detect.
The aim of the study is to compare the cost-effectiveness and outcomes of three TAPP modifications for unilateral groin hernia, including a control group of patients who underwent open repair.
Materials and methods
Study population
Between November 2017 and March 2019, all consecutive cases of elective unilateral inguinal hernia repair were included in a prospective database. Only patients older than 18 years of age and who completed at least 1 year of follow-up were included. Patients with contraindications to general anaesthesia, inguinal hernia recurrence, and previous prostatectomy were excluded. The first 20 procedures performed by each surgeon were excluded, to minimize the learning curve bias. Patients provided written informed consent before undergoing surgery. The procedures were performed by three senior surgeons with expertise and experience in the TAPP technique.
Surgical technique
A single dose of first-generation cephalosporin is given at the induction of the anaesthesia.
The operation is performed under general anaesthesia with the pneumoperitoneum established through a Veress needle placed in the left subcostal space. Three trocars are placed, as shown in Fig. 1. The peritoneum is opened approximately at the level of the lateral trocar, and the opening is extended medially towards the superior margin of the internal inguinal ring, up to the residue of the umbilical artery (Suppl. Material, Video 1). When the Cooper ligament is exposed, the hernia sac is isolated and reduced, freeing the spermatic cord. A polypropylene mesh of 15–10 cm is introduced into the abdominal cavity in the pre-peritoneal space.
Consecutive patients who underwent laparoscopic repair were retrospectively divided into three different groups, according to modifications of the TAPP technique that were developed over time, in an attempt to improve the procedure.
Group 1
The mesh is fixed to the ligament of Cooper with one staple and to the pre-peritoneal space with three or four further titanium staples. The peritoneal flap is then closed, using titanium staples.
Group 2
The mesh is secured with approximately 2 ml of fibrin glue, applied at almost 1 cm distance from the mesh, using a specific laparoscopic tool (Suppl. Material, Video 2). The peritoneum is closed with a running barbed suture.
Group 3
The mesh is secured in the same fashion of group 2, but the peritoneum is closed with fibrin glue (Suppl. Material, Video 2).
Control group (open repair)
A control group was established, including patients who underwent unilateral inguinal hernia repair during the same period of time, (“open group”). A case-matched study design was used to extract patients with similar pre-operative characteristics of the laparoscopic group. Patients were matched by age, body mass index (BMI), American Society of Anesthesiologists’ (ASA) score, and size of the hernia, according to the European Hernia Society classification (Grade I: 1.5 cm, Grade II: 1.5–3 cm, Grade III: > 3 cm) [5].
The procedures of the open group were performed by three senior surgeons who do not perform laparoscopic inguinal hernia repair.
Surgery is performed under epidural anaesthesia with the same antibiotic prophylaxis used in the TAPP approach. The standard Lichtenstein open tension-free technique is used, as described by Amid, and the same mesh as the TAPP groups is placed [2].
Postoperative management
All patients stay overnight at our center.
A standard analgesia regimen was used for all patients post-operatively for up to 7 days, which included paracetamol and metamizole.
Chronic pain was defined as pain lasting at least 3 months after the hernia repair.
The duration of surgery was recorded. The length of post-operative stay, as well as post-operative complications, were prospectively collected. In the case of suspicion of a recurrence, an ultrasound scan was performed to confirm it.
Cost-effectiveness study
Quality adjusted life year (QALY) scores were estimated at 1 year following the procedure for each patient using the medical outcomes study Short Form-36 (SF-36) questionnaire (Spanish version), sent by mail to each patient one and six months after surgery [6].
The Health Utilities Index 2 (HUI2) score was calculated from the eight subscales of the SF-36 using the Nichol method.
A model-based cost–utility analysis estimating mean costs and QALYs per patient was performed with a one-year time horizon.
The Institute for Validation of Clinical Efficacy (IVEC) of HM Hospitales group was responsible for capturing costs ascribed to each patient’s treatment. The total direct hospital costs of care were recorded under the patient’s unique medical record number and were included from the time of patient admission to discharge.
Materials and medications used during surgery were standardized, and thus, the same equipment and resources were used for all patients undergoing surgery, regardless of the technique used. Operative costs included the cost of the operating room in relation to the operative time (according to the analysis from Raft et al. [7], who calculated the cost per minute at 10 Euros), and all required supplies (including all laparoscopic devices, sutures, drapes, and instruments), anaesthesia, laboratory, and related blood transfusion costs, when required. Hospitalization costs included costs associated with room and board, the length of hospital stay (including medications, blood transfusion, parenteral nutrition, and radiology charge), and costs for surgical visits (programmed and emergency), as well as readmission costs up to 90 days from surgery. The direct costs of the professionals involved have not been calculated as they did not vary between the groups. A discount rate of 3% per year is used in the estimation of the costs and QALYs, as recommended by health economic guidelines. All costs are presented in Euros (exchange rate 2020).
Stochastic cost–utility analysis was undertaken, whereby the incremental cost-effectiveness ratio (ICER) was estimated using overall costs of the three groups’ laparoscopic procedures and QALYs derived from patient interviews compared with the standard open group to find the incremental cost per QALYs gained.
Net monetary benefits (NMBs) were calculated to estimate the maximum willingness-to-pay (WTP) of decision makers for a QALY gained. The NMB was calculated as the mean QALYs per patient multiplied by WTP threshold minus the mean cost per patient for the treatment. The decision rule was to adopt the treatment if the NMB > 0, and the alternative with the highest NMB representing the best value for money. No discounting of cost or QALYs was performed given the 11-year time horizon.
Sensitivity analysis
A sensitivity analysis was carried out to propagate the uncertainty of the estimations to the results of the model. A multivariate and stochastic sensitivity analysis performed by 5000 Monte Carlo simulations was used. The cost-effectiveness plane was used to represent all pairs of solutions of the model.
The results of the one-way sensitivity analysis are shown in the tornado diagram which graphically depicts how variations in each input affect the outcome. The 95% confidence intervals around the base-case values were derived using the 2.5 and 97.5 percentiles calculated from the sensitivity analysis.
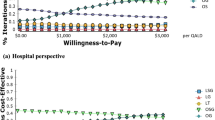
Acceptability curve
We also computed cost-effectiveness acceptability curves (which plot the probability that the three groups), which were cost-effective relative to the open approach over a reasonable range of levels of willingness-to-pay.
Since, in Spain, there is no specific WTP threshold in healthcare, we used a WTP of 20,000 € and 30,000 € per QALY as a threshold to recognize which treatment was most cost-effective, according to the National Institute for Health Care Excellence (NICE).
Statistical analysis
Data have been recorded in a SPSS Statistics Version 20.0 database and are expressed as median values (interquartile range—IQR 25–75). Categorical data are presented as numbers (%). To compare the means of the quantitative variables when the variables followed a normal distribution, a variance analysis and a Student’s t test were used. For the rest of the variables, both Mann–Whitney and Kruskal–Wallis tests were performed. Cost, QALYs, and incremental results are presented in a 95% Confidence Interval. A p value < 0.05 was considered significant. Only data of patients who completed 1-year follow-up are described.
Results
A total of 91 patients who underwent TAPP procedures in the study period were included in the study, which were matched with a total of 29 open inguinal hernia repairs. The baseline clinical characteristics of the four groups are summarized in Table 1.
As shown in Table 2, the mean operative time was longer in group 1 (79.4 min) compared to group 2 (93.1 min) and group 3 (81.1) (p = 0.03). The operative time of the open approach, compared with the laparoscopy, was always shorter (mean, 59.5 min, p = 0.03). No conversion occurred in the laparoscopic groups. The overall mean hospital stay of the laparoscopic groups was 1.03 days (range 1–2) without differences between the groups and compared with the open approach (Table 2).
Post-operative morbidity is shown in Table 2, being lower in the laparoscopic groups (group 1: 6.45%; group 2: 7.4%; group 3: 6%) compared to the open approach (17.24%) (p = 0.035). No recurrences occurred at a mean follow-up of 19.3 months (range 12–26 months). Table 3 summarizes the costs of each specific laparoscopic device or suture used for laparoscopic inguinal hernia repair.
All data related to cost analysis are depicted in Table 3. The mean overall operative costs of materials used in the operating room were higher in the laparoscopic groups (group 1 = 1139.10 €, group 2 = 1.041.74 €, group 3 = 101,644 €), compared with the open group (637.38 €; p = 0.001).
The total overall mean open group cost (1185.95 €) was found to be lower compared with that of all laparoscopic groups (p = 0.003). The incremental cost, which is the measure of the increased cost of a new technique (laparoscopic groups 1, 2, and 3) compared with the cost of the standard approach (open technique), was higher for group 1 (496.44 €), compared with that of group 2 (352.59 €) and group 3 (324.15 €) (p = 0.038).
The highest estimated ICER value in favour of TAPP was found in groups 2 and 3 (0.813 and 0.829, respectively), compared to group 1 (0.666) (Table 3). In the Monte Carlo simulations analysis, there was a 33.32%, 36.26%, and 36.7% probability that laparoscopic groups 1, 2, and 3, respectively, are both less costly and more effective (Fig. 2). The acceptability curves, showing the probability that laparoscopy is cost-effective at the willingness-to-pay threshold of 20,000€ and 30,000€ per QALY gained, are depicted in Fig. 3. This shows that group 3 has the highest probability of cost-effectiveness over the open approach of 96.78% and 98.02% at a WTP thresholds of 20,000 €/QALY and 30,000 € QALY, respectively (Fig. 3). Furthermore, at the lower incremental cost per QALY thresholds of 5,000 €, it is likely that laparoscopic groups 3 and group 2 are 86.3% and 85.04% cost-effective, respectively, while laparoscopic group 1 is 78.58% cost-effective.
Discussion
Currently, minimally invasive repair of inguinal hernia, including TAPP and total extraperitoneal endoscopic hernioplasty (TEP), represents an alternative procedure to the standard open approach, as its advantages are well-established [2, 8, 9]. The type of mesh used, its fixation, and the peritoneal closure for the TAPP technique are still under discussion, as several modifications of the procedure have been proposed [4, 10,11,12].
Several randomized studies showed that using staples for mesh fixation might cause high, early post-operative pain, and chronic pain [11, 13]. Therefore, it is suggested to minimize their use by applying only one staple to the Cooper ligament or using self-fixating meshes [11] or glue [13,14,15,16,17].
Mesh fixation with fibrin glue was proven to be safe and effective in the prospective randomized trial of Lovisetto et al. [16], and it was associated with a lower incidence of post-operative neuralgia compared with staples. Under the light of these results, we modified our TAPP technique from that of group 1 where staples were used for both mesh and peritoneal closure, to that of group 2, replacing staples with fibrin glue to fix the mesh.
Another important modification of the TAPP technique is the peritoneal closure. The original TAPP technique, performed in group 1, adopted the fastest and easiest peritoneum closure method using staples, but at the price of a higher risk of nerve injury and bleeding [12]. Currently, the most frequently used modification is the running suture that we adopted in group 2. However, suturing the peritoneum requires specific surgical skills to avoid tears or rupture that may expose the mesh to the intestine. The development of barbed sutures has decreased the difficulty of this procedure. However, peritoneal ruptures still occur, especially in cases when the hernia sac reduction manoeuvre has been particularly challenging. Additionally, this increased mean operative time from 79.4 min of group 1 to 93.1 min of group 2 (Table 2), and it does not avoid the risk of nerve entrapment.
For these reasons, we have further modified the technique to that of group 3, replacing the running suture with fibrin glue to approximate the peritoneum, which is particularly useful for those cases where the peritoneum is at a higher risk of tear or rupture during closure.
The latest modification of group 3 decreased the mean operative time from 93.1 min of group 2 to 81.1 min of group 3, proving that using glue was the simpler and less time-consuming technique for closing the peritoneum [18]. The most frequently studied glue product is N-2-butyl cyanoacrylate, showing excellent capacity for both mesh and peritoneal closure, achieved after only a few seconds [15]. However, being a non-biological glue, one of the main criticisms is that when this product is in contact with the intestine, potential adhesions may develop. Wilson et al. [15] reported excellent results with no long-term complications, but considerable precautions are required to avoid dropping any material into the intestine.
An alternative to cyanoacrylate is the biological human fibrin used in study group 3, which has the concomitant function of glue and haemostatic agent. Different from the cyanoacrylate, more evidence is available to show that fibrin glue may prevent peritoneal adhesions, potentially representing the optimal and safest tool for this manoeuvre [19].
Previous studies reported only on short-term outcomes of biological human fibrin glue use for mesh fixation and peritoneum closure, without any cost analysis [14, 20]. We only included patients who have completed 1 year of follow-up, to detect long-term complications related to the peritoneal closure, such as small bowel obstructions. Peritoneal closure with fibrin glue is simple and it is also effective for cases with a weighty “fatty” peritoneum that entails increased tension on the peritoneal closure (as shown in the second case of the Suppl. Material, Video S2).
Our study confirmed that laparoscopic repair is more expensive than the standard open approach, with an extra cost of approximately 500 € (Table 3). When examining intra-operative costs of the three groups, we found a significant decrease of mean overall total costs from group 1 (1682.39 €) compared with group 2 (1538.54 €) and group 3 (1510.10 €) (p = 0.046) (Table 3).
The reason for higher cost of the original TAPP technique group 1 is justified by the use of the staple device (380 €), which is not used in groups 2 and 3, being replaced with fibrin glue that is 140 € less expensive (Table 3).
The overall cost of an operation provides limited information about the benefit of the modifications of a technique. A cost-effectiveness analysis of the modifications of the technique represents the ideal method to provide objective evidence of an improvement—this was not yet available in the literature regarding the herein described variations.
The study showed that laparoscopic groups are always the more cost-effective option than the open approach groups, as it has been demonstrated in bilateral inguinal hernias repair [21].
Study limitations
Despite these promising data, we acknowledge some limitations. This study is not randomized, even if the groups are homogenous: therefore, the results may not have been greatly affected. It can be speculated that the mean QALY of this study increased from group 1 to groups 2 and 3 because of accumulated experience. Nevertheless, as stated in the Methods section, this series includes operations performed only after a proper learning curve had been completed.
Conclusion
Unilateral laparoscopic inguinal hernia repair with TAPP is cost-effective compared with open approach. The more recent modifications described in groups 2 and 3 are more cost-effective compared with the original technique described in group 1. Using fibrin glue for both mesh fixation and peritoneal closure (group 3), decreases operative time.
The findings of this study may help to guide clinicians and stakeholders towards adoption of practices that enhance the cost-effectiveness of different modifications of the TAPP technique.
References
Patterson TJ, Beck J, Currie PJ, Spence RAJ, Spence G (2019) Meta-analysis of patient-reported outcomes after laparoscopic versus open inguinal hernia repair. Br J Surg 106(7):824–836. https://doi.org/10.1002/bjs.11139
HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22(1):1–165
Chen LS, Chen WC, Kang YN, Wu CC, Tsai LW, Liu MZ (2019) Effects of transabdominal pre-peritoneal and totally extraperitoneal inguinal hernia repair: an update systematic review and meta-analysis of randomized controlled trials. Surg Endosc 33(2):418–428. https://doi.org/10.1007/s00464-018-6314-x
Shi Z, Fan X, Zhai S, Zhong X, Huang D (2017) Fibrin glue versus staple for mesh fixation in laparoscopic transabdominal pre-peritoneal repair of inguinal hernia: a meta-analysis and systematic review. Surg Endosc 31(2):527–537. https://doi.org/10.1007/s00464-016-5039-y
Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, Hoeferlin A, Kingsnorth AN, Mandala V, Palot JP, Schumpelick V, Simmermacher RK, Stoppa R, Flament JB (2007) The European hernia society groin hernia classification: simple and easy to remember. Hernia 11(2):113–116
Vilaguta G, Ferrera M, Rajmilb L et al (2005) El Cuestionario de Salud SF-36 español: una década de experiencia y nuevos desarrollos, vol 19. Gac Sanit, Barcelona
Raft J, Millet F, Meistelman C et al (2015) Example of cost calculations for an operating room and a post-anaesthesia care unit. Anaesth Crit Care Pain Med 34:211–215
Scheuermann U, Niebisch S, Lyros O, Jansen-Winkeln B, Gockel I (2017) Transabdominal Preperitoneal (TAPP) versus Lichtenstein operation for primary inguinal hernia repair—a systematic review and meta-analysis of randomized controlled trials. BMC Surg 17(1):55. https://doi.org/10.1186/s12893-017-0253-7
Gravidilis P, Davies RJ, Wheeler J, de’Angelis N, Di Saverio S (2019) Total extraperitoneal endoscopic hernioplasty (TEP) versus Lichtenstein hernioplasty: a systematic review by updated traditional and cumulative meta-analysis of randomised-controlled trials. Hernia 23(6):1093–1103. https://doi.org/10.1007/s10029-019-02049-w (Epub 2019 Oct 10)
Kaul A, Hutfless S, Le H, Hamed SA, Tymitz K, Nguyen H, Marohn MR (2012) Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc 26(5):1269–1278
Andresen K, Fenger AQ, Burcharth J, Pommergaard HC, Rosenberg J (2017) Mesh fixation methods and chronic pain after transabdominal pre-peritoneal (TAPP) inguinal hernia surgery: a comparison between fibrin sealant and tacks. Surg Endoscm 31(10):4077–4084
Antoniou SA, Köhler G, Antoniou GA, Muysoms FE, Pointner R, Granderath FA (2016) Meta-analysis of randomized trials comparing nonpenetrating vs mechanical mesh fixation in laparoscopic inguinal hernia repair. Am J Surg 211(1):239-249.e2. https://doi.org/10.1016/j.amjsurg.2015.06.008
Harsløf S, Krum-Møller P, Sommer T, Zinther N, Wara P, Friis-Andersen H (2018) Effect of fixation devices on post-operative pain after laparoscopic ventral hernia repair: a randomized clinical trial of permanent tacks, absorbable tacks, and synthetic glue. Langenbecks Arch Surg 403(4):529–537
Phillips AW, Viswanath YKS, Burns JK, Hall CEJ, Horgan AF (2014) Use of fibrin glue for fixation of mesh and approximation of peritoneum in transabdominal pre-peritoneal (TAPP) inguinal hernia repair: technical feasibility and early surgical outcomes. Surg Laparosc Endosc Percutan Tech 24(2):e43–e45
Wilson P, Hickey L (2019) Laparoscopic transabdominal pre-peritoneal (TAPP) groin hernia repair using n-butyl-2-cyanoacrylate (Liquiband®Fix8TM) for mesh fixation and peritoneal closure: learning experience during introduction into clinical practice. Hernia 23(3):601–661
Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, Faillace G, Longoni M (2007) Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal pre-peritoneal hernioplasty: a prospective, randomized study. Ann Surg 245(2):222–231
Canonico S, Benevento R, Perna G et al (2013) Sutureless fixation with fibrin glue of lightweight mesh in open inguinal hernia repair: effect on post-operative pain: a double-blind, randomized trial versus standard heavyweight mesh. Surgery 153:126–130
Oguz H, Karagulle E, Turk E, Moray G (2015) Comparison of peritoneal closure techniques in laparoscopic transabdominal pre-peritoneal inguinal hernia repair: a prospective randomized study. Hernia 19(6):879–885
Tavares K, Mayo J, Bogenberger K, Davis SS Jr, Yheulon C (2019) Fibrin versus cyanoacrylate glue for fixation in laparoscopic inguinal hernia repair: a network meta-analysis and indirect comparison. Hernia. https://doi.org/10.1007/s10029-019-02072-x.10.1007/s10029-019-02072-x
Ielpo B, Ferri SJ et al (2020) Laparoscopic transabdominal pre-peritoneal (TAPP) inguinal hernia repair using fibrin glue for fixation of the mesh and peritoneum closure. Surg Laparosc Endosc Percutan. https://doi.org/10.1097/SLE.0000000000000797
Ielpo B, Nuñez-Alfonsel J, Duran H, Diaz E, Fabra I, Caruso R, Malavé L, Ferri V, Barzola E, Quijano Y, Vicente E (2018) Cost-effectiveness of randomized study of laparoscopic versus open bilateral inguinal hernia repair. Ann Surg 268(5):725–730
Funding
All authors have no source of funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study. The study was in agreement with the Good Clinical Practice.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary Video 2: Use of fibrin glue to close the peritoneum (MP4 81089 KB)
Supplementary Video 1: Laparoscopic hernia repair, using fibrin glue for mesh fixation (MP4 30622 KB)
Rights and permissions
About this article
Cite this article
Ielpo, B., Nuñez, J., Ferri, V. et al. Laparoscopic inguinal hernia repair: cost-effectiveness analysis of trend modifications of the technique. Updates Surg 73, 1945–1953 (2021). https://doi.org/10.1007/s13304-021-01005-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-021-01005-7