Abstract
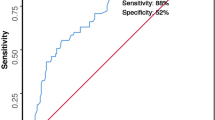
Postoperative peritonitis (PoP), despite their relatively low incidence, are associated with high mortality. Such poor outcomes are also related to the high proportion of aged patients, whose intra-abdominal infections are difficult to manage. The study included 84 consecutive patients with PoP. The aim was the validation of the Mannheim Prognostic Index (MPI) in the context of PoP and the assessment of the prognostic impact of age and other clinical factors in a large series from a tertiary center. PoP had an incidence of 3.9% in all the abdominal surgeries in the study period. Surgical control of POP focus was achieved in 90.5% of cases and a complete abdominal clearance in 58.3%. Complication rate was 75% with a mortality of 26.2%. For MPI score, the ROC curve indicated a cut-off value of 29 with a sensitivity of 72.7% and specificity of 67.7% in predicting death. At univariate analysis, factors significantly related to poorer prognosis included advanced age (p 0.001), site of primary surgery (p 0.05), lack of abdominal clearance (p 0.003), generalized peritonitis (p 0.04) and high MPI score (p < 0.001). Age, MPI score and absence of abdominal clearance resulted in independent prognostic factors at multivariate analysis. MPI showed good efficacy in identifying POP patients at high risk of death. The increased risk of mortality related to advanced age should be considered with MPI score in planning the treatment. An aggressive and early diagnostic-therapeutic approach is required to reduce the MPI score and improve the prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-operative peritonitis (PoP) is typically the result of a dehiscence of an anastomosis or a suture performed during abdominal surgery. PoP complicate the postoperative course in 0.7–7% of abdominal procedures in reported series [1, 2]. Despite the relatively low incidence, PoP represents a major issue because the mortality rate associated with it is high, approaching 30–50% in the literature [3].
PoP occurs in patients who are debilitated by the primary pathology and by the first surgical stress itself. As a consequence, the intra-abdominal infection caused by PoP frequently evolves into sepsis and shock and, eventually, death.
Even though patients with PoP are hospitalized and monitored through standardized post-operative protocols, the diagnosis of these surgical complications is often problematic because the alterations related to the abdominal procedure jeopardize the clinical and laboratory findings. [4].
As a result, a delay in secondary surgical treatment may often occur, thus contributing to the poorer outcomes in PoP patients. Besides timing to reoperation, other factors such as the presence of sepsis or septic shock, the site of origin of PoP, the presence of immunosuppression and older age contribute to determine the final prognosis [5, 6].
The identification of clinical scores that take into account the factors impacting the outcome of PoP and that allow to accurately estimate the prognosis and risk stratification is of primary importance to plan the surgical procedure and intensive post-operative care.
Scores commonly used in critical patients, such as POSSUM or APACHE II, have high efficacy in predicting the outcome and have proved their efficacy in the setting of intra-abdominal infections, but they are complex to calculate and are best suited for the intensive care setting [7,8,9]. Therefore, such clinical tools may not be suitable for use among patients with PoP diagnosis as their application at patient’s bedside is difficult and unpractical.
The Mannheim Peritonitis Index (MPI) (Table 1) is a prognostic score developed in the 1980s for patients with acute abdominal infection. It is based on the evaluation of a few easily recordable clinical and operative parameters [10]. The MPI has been tested in patients with intra-abdominal infections and perforative peritonitis in recent series [11,12,13] where it confirmed its efficacy at stratifying the risk of death successfully. However, PoP is a group of peritonitis that differs significantly from the more common secondary, non-post-surgical, forms, and the applicability and reliability of the MPI in this clinical context has not been proved till present.
The purpose of our cohort prospective study was to evaluate the efficacy of the MPI in a population of patients with PoP. We compared the MPI score to the other clinical and surgical factors impacting on prognosis, and we used these data to individuate those parameters which could allow a reliable risk stratification of PoP patients.
Methods
This paper describes the results of an observational prospective cohort study conducted on a population of patients who developed PoP after primary abdominal surgery at the Unit of General Surgery and Surgical Oncology of the University of Siena. The primary aim of the study was the validation of the MPI as a prognostic tool in the context of PoP. The secondary objective of the study was the assessment of the impact of other clinical and surgical factors on the prognosis of patients with PoP.
The study was approved by the Scientific Committee of the Department of Medicine, Surgery and Neurosciences of the University of Siena. Ethics approval was not required because this was an observational study which did not require any modification of the standard therapeutic protocols.
The study includes patients submitted to abdominal surgery at our institution between January 2014 and December 2019 who developed a PoP.
The onset of PoP was identified by one or more of the following signs or symptoms: absence of intestinal motility, intense abdominal pain not responding to pain drugs, presence of bile or intestinal contents in the abdominal drainages, fever higher than 38.5 °C, hypoxia (pO2 < 65 mmHg), hypotension (systolic blood pressure < 100 mmHg), oliguria (< 500 cc in 24 h) [4]. Clinical suspect of PoP was confirmed by radiological workup which included CT scan as per institutional protocols. Patients with acute diffused peritonitis at primary surgery were excluded from the study.
Data were retrieved from patients’ clinical records undergone to informed consent. Pre-operative and primary surgery data of patients with PoP were prospectively collected with information on the time between the onset of PoP and surgical treatment, type of surgical procedures performed, intraoperative findings, postoperative complications, length of hospital stay and in-hospital mortality.
Correlations between mortality and variables included in the study were first conducted by univariate analysis; their statistical significance was evaluated using the χ2 test for categorical variables and Student t test for continuous variables.
The preoperative patient characteristics that were considered included age, primary pathology and related surgical procedure performed and comorbidities. In the definition of co-morbidities, we included cardiological pathologies such as electrocardiographic or echocardiographic abnormalities or pathologies for which the patient was assuming medications; hypertension was included as a cardiological co-morbidities. Respiratory diseases were assessed as chest X-ray or CT scan abnormalities or pathologies for which the patient was under specific treatment. Diabetes mellitus, hepatic diseases, cerebrovascular diseases, and chronic kidney disease were assessed using informations on patient medications and clinical history.
Presence of active cancer was considered as a comorbidity, but for MPI calculation only abdominal cancers treated at primary surgery were given a score of four points.
For the purpose of statistical analysis, we stratified patients in four age subgroups (\(\le\) 60 years old, 61–70 years old, 71–80 years old, \(\ge\) 80 years old).
Variables related to PoP included white blood cells count (WBC) and serum creatinine level at the time of the onset of PoP, time to reoperation, site and cause of the PoP, an extension of peritonitis and type of exudate, type of secondary procedure, number of blood transfusions, MPI score and success in obtaining a complete abdominal clearance at the end of the procedure. Complete abdominal clearance at the end of the surgery was defined by identification and correction of the focus of PoP (interruption of contamination) and removal of contaminating fluids (purulent material, enteric and biliary secretions) or infected and necrotic tissues.
To identify those factors independently related to an increased risk of mortality, the variables which resulted statistically significant at univariate analysis were entered in a multivariate analysis and a logistic binomial regression model was run. For statistical comparison, a p-value < 0.05 was considered significant.
The Statistical Package for the Social Sciences software (version 25.0) (SPSS™, Chicago, Illinois, USA) was used for statistical analysis.
Results
The study population included 84 patients with PoP (43 males and 41 females), with a mean age of 63.5 years (range 21–97); 33 patients (39.3%) were younger than 60 years and 12 (14.3%) were older than 80 years.
Clinical characteristics of the study population are described in Table 2.
Co-morbidities were present in 70 cases (83.3%) and 13 patients (15.5%) had at least three comorbidities. Most common primary surgeries were colorectal (44.1%) and gastric resections (21.4%) (Table 2). Some 16 primary procedures (19%) were emergency operations, and included 6 cases of intestinal obstruction, 5 cases of acute visceral ischemia, 3 appendicitis and 2 perforated diverticulitis.
Primary surgeries were performed in oncological patients in 41 cases (49%).
The most common procedures were colo-rectal resections with 35 cases (12 right emicolectomies, 10 left emicolectomies, 2 transverse colon resections and 11 rectal resections) followed by gastrectomies (16 cases, 19%) and small-bowel procedures (15 cases, 17.8%).
At diagnosis of PoP, 24 patients (28.6%) had serum creatinine levels higher than 1.2 mg/dL, 26 (30.9%) had systolic blood pressure lower than 100 mmHg and 10 (11.9%) had heart rate higher than 120 bpm. Signs of respiratory distress were present in 20 cases (23.8%). WBCc higher than 12,000 WBC/mm3 was present in 28 patients (33.3%) while 8 patients (9.5%) were leukopenic (WBC < 4000/mm3); anemia with hemoglobin values lower than 9 g/dl was found in 11 cases (13%).
All patients underwent surgery with open approach, within 12 h of onset of symptoms in 26 cases (31%), between 12 and 24 h in 45 cases (53.6%) and after 24 h in 13 cases (15.4%).
The most frequent focus of PoP was the small bowel (34.5%) followed by the left colon (23.8%) and the gastroduodenal tract (21.4%). The overall incidence of anastomotic or gastrointestinal stump dehiscence was 58.3%, while a iatrogenic visceral lesion was responsible of PoP in 25 cases.
There was no correlation between iatrogenic cause of PoP and emergency surgery. Among patients with iatrogenic PoP, we observed a higher percentage of perforations for minimally invasive approach, but these data have no general value as an higher incidence of lesions following laparoscopic surgery was not confirmed when considering all the abdominal primary surgeries in the study series.
In 58 cases (69%) PoP was diffuse. The exudate was biliary in 25 cases (29.8%), purulent in 33 cases (39.3%) and fecaloid in 26 cases (31%).
The focus of the PoP was identified and corrected in 90.5% of patients and a complete abdominal clearance was obtained in 49 cases (58.3%). A visceral resection was performed with immediate anastomosis in 22 (26.2%) of cases and with anastomosis and protective stoma in other 22 patients. A simple suture of visceral perforation was performed in 19 cases (22.6%) and associated with a stoma in further 10 patients (11.9%). Finally, a simple stoma was performed in 11 patients (13.1%). Blood transfusions were required in 44 patients (52.4%).
We recorded 85 postoperative complications in 63 patients, with a morbidity of 75%; the post-reoperation hospital stay was of 14 days (1–64).
According to the classification of surgical complications proposed by Dindo [14], we observed 35 grade II, 17 grade III and 33 grade IV complications (Table 3).
The most frequent medical complication was the development of a septic shock related to PoP (15 cases); cardiac (17 cases) and pulmonary (13 cases) complications had a high incidence too.
Infective complications, either intra-abdominal or wall-located, were the most common surgical complication (21 cases, 24.3%).
Some 22 patients died of PoP with a mortality of 26.2%: the most frequent cause was Multi-Organ Failure Syndrome (14 patients), followed by heart failure (4 cases), pulmonary hembolism (2 cases) and respiratory distress syndrome (2 cases).
We constructed the ROC curves (receiver operating curves) for the MPI score and serum creatinine levels as predictors of mortality. For the MPI score, the ROC curve identified 29 as the best cut-off value, with a sensitivity of 72.6% and a specificity of 67.7% in predicting the risk of death. The AUC (area under the curve) of the ROC curve was 0.759 (Fig. 1). For serum creatinine levels, the cut-off value showed by the ROC curve was 1 mg/dl, with a sensitivity of 68.2% and a specificity of 59.7% (Fig. 2). These cut-off values were then used in the survival analysis.
At univariate analysis, age higher than 80 years, serum creatinine level > 1 mg/dl, diffuse peritonitis, site of the first surgery, the impossibility of surgical correction of the PoP focus, incomplete abdominal clearance and MPI score > 29 resulted significantly associated to increased risk of mortality. (Table 4).
The statistically significant variables were included in a logistic regression model. MPI score, age higher than 80 years and abdominal clearance were identified as independent predictors of mortality in multivariate analysis. (Table 5).
Discussion
PoP includes a heterogeneous group of clinical situations poorly studied in recent literature, characterized by low incidence but also high mortality.
Our series included 84 cases of PoP with an incidence of 3.9% in all the 2154 abdominal surgeries performed at our institutions in 6 years. This value is in line with the 0.7–7% incidence of PoP reported in the literature. Overall, these estimated values may be biased downward because those patients with PoP treated with conservative therapies (e.g. percutaneous drainage) or not reoperated due to extremely poor conditions (e.g. elderly patients with abdominal ischemia) have not been included in the studies’ samples [15, 16].
The age distribution was typical of western industrialized countries with a high percentage of elderly patients. These patients represent a particularly fragile population with multiple comorbidities, in which the onset of a PoP is associated with higher risk of mortality despite adequate surgical and intensive care treatment. The mortality rate of our series (26.2%) was in line with the lower values reported in the literature but still significant [3, 5].
The outcome of PoP is difficult to establish because it is affected by many factors, including the different primary pathologies and surgical procedures performed. However, the severity of the pathology makes it necessary to have a rapid and easily applicable prognostic tool.
MPI was developed specifically for patients with acute abdominal infection and is based on the evaluation of a few readily detectable clinical and surgical parameters (Table 1) but it has not been validated for PoP before.
In our study, we have evaluated for the first time the application of MPI to the clinical setting of PoP and we have demonstrated that this prognostic tool can be useful in stratifying the prognosis of these patients. Nonetheless, the MPI showed some limitations.
Older age is considered in MPI and is a major prognostic factor in this study, with a mortality of only 3% in patients younger than 60 years and of 50% in the population aged 80 years, or older. If we exclude neoplasms, age was significantly related to a higher number of associated pathologies (Table 6) and such interdependence between age and comorbidities on prognosis is confirmed by the 46.2% mortality rate in patients with three or more comorbidities.
We found a significant correlation between prognosis and serum creatinine levels at the diagnosis of PoP. Serum creatinine levels > 1 mg/dL were associated with a more than doubled mortality compared to that of patients with lower values (15.9% for creatinine values < 1 mg/dl vs 37.5% for higher values), indicating that creatinine is a sensible indicator of the development of systemic organ failure since the early stages of PoP [12].
An important aspect to be considered in evaluating organ failure according to MPI is the presence of intestinal obstruction, as a prolonged post-operative intestinal paresis is usually present in the early post-operative period and may persist at the onset of PoP independently from a systemic organ dysfunction. In our series, the seven points of MPI score for organ failure were assigned in 23 cases, but in none of them the presence of an intestinal obstruction was the only parameter to identify the condition. Nonetheless, we stress the importance of an accurate evaluation of the degree and persistence of intestinal obstruction, in particular in the paretic form, in calculating the MPI in this setting of patients.
First surgeries on the upper gastrointestinal tract and small bowel were associated with a mortality of 44.4% and 40%, respectively. These rates are significantly higher than for surgeries on the right and left colon (26.7% and 13.6%, respectively). The same difference was observed when considering the focus of PoP, as the mortality recorded in PoP of colonic origin (17.6%) was much lower than that of PoP originating from the small bowel (27.6%) and the upper gastrointestinal tract (38.1%). These results are probably related to the earlier activation of the systemic inflammatory response due to the rapid spread of large quantities of biliary material which occurs in proximal PoP, and to higher technical difficulties in the surgical treatment of PoP occurring in the supra-mesocolic district [17]. These aspects are well considered in the MPI score, which assigns a high, 4 points score to the peritonitis originating outside the colon.
The timing of the re-operation was associated with an increase in mortality from 23.9% in early redo surgeries to 38% in deferred operations. However, this difference was not statistically significant, in contrast with the results of other studies [2]. This finding could be related to the low number of patients treated with a deferred surgical approach in our series. Furthermore, the identification of the onset of PoP and the associated delay to reoperation remain a highly debated issue and a possible confounding factor in our study and the related literature [3].
The type of peritonitis was significantly correlated with the outcome, with an increase of mortality up to 32.8% in the diffuse forms. Such a result is uniformly reported in the literature [16] and taken into account in the MPI, where the presence of diffuse abdominal infection gives a 6 points score increase. Indeed diffuse peritonitis determines an inflammatory and infectious systemic response that rapidly evolves towards septic shock and multi-organ failure [5]. Furthermore, in patients where septic material has extensively spread through the whole abdomen, adequate control of the focus of PoP and complete clearance of the peritoneal cavity are much more difficult to obtain.
Indeed, the control of the PoP focus and the complete abdominal clearance were major determinants of survival in our series. Patients in whom it was impossible to obtain a detection and correction of the primary focus had a mortality as high as 75%. Similarly, the absence of clearance of the abdomen at the end of the surgery was responsible for a mortality rate of 42.9%. These two factors are interdependent and were considered together in the logistic regression, which confirmed their independent prognostic value with a relative risk of 3.9. This finding has not been reported before in other studies on PoP, even if an adequate abdominal clearance and a complete control of the peritoneal focus are reported as factors associated with a better outcome in other types of peritonitis [18].
The type of exudate did not significantly impact survival, even if a purulent exudate was associated with a worse outcome and a mortality rate of 39.4%. Our study showed that an important limitation of MPI for PoP may be represented by the fact that the presence of biliary exudate is not weighted with a dedicated score. As the primary objective of the present study was to verify the efficacy of MPI in the setting of post-operative peritonitis, we followed the criteria for score calculation adopted both in the original study [10] and in the confirmation study by Billing [16] and we assigned a score of 0 to the presence of biliary exudates. The results of our study demonstrated that biliary exudate is, on the contrary, a marker of increased risk for mortality and its presence should be taken into account in the prognostic assessment of these patients.
In the univariate analysis, the MPI was identified as a significant prognostic factor for PoP mortality, which showed an increase from 14 to 38% in cases where the MPI score is equal or greater than the threshold value of 29 identified by the ROC curve. However, it should be emphasized that some of its components have not shown influence on prognosis in our experience. Similarly to sex, the presence and the stage of cancer at primary abdominal surgery did not significantly impact survival. We note that this result may be influenced by the fact that our data were collected in a general surgery and surgical oncology unit and include a higher percentage of neoplastic patients than the series from general surgery units of other studies [16, 19]. Furthermore, the age cut-off of 50 years used in the MPI did not correspond to the cut-offs for a significant increase of mortality of 60 years and 80 years described in our series. Indeed, our data are consistent with the findings of Salamone who reported a poorer prognosis of patients aged older than 80 in a recent study evaluating the MPI in the elderly affected by peritonitis [13].
However, the study was aimed at assessing the applicability of the MPI in this patient setting, and we have applied the score as originally described.
Despite these limitations, the MPI resulted in an independent prognostic factor at multivariate analysis, with a relative risk of 1185 per score point. The cut-off value of 29 selected with the ROC curve in our study is higher than the cut-off values of 21–27 reported in the literature on cases of patients with non-postoperative diffuse acute peritonitis [13, 16, 19]. These higher values are due to the more aggressive characteristics of PoP, which show overall higher values of MPI, and to the efficacy of the diagnostic and therapeutic protocols adopted at our institution which limited mortality in the less severe situations. At this value, MPI showed a good sensitivity of 70%, even if with low specificity, as about two-thirds of patients with MPI above the cut-off value survived. In the subgroup of patients with MPI equal to or greater than 29, colonic site of primary surgery and PoP focus and early surgical reoperation significantly related to better outcomes.
Strengths and limitations
This is the first study which has evaluated the efficacy of the MPI in PoP.
We conducted an observational prospective cohort study based on a relevant population from a single, high-volume, general and oncological surgery center.
While monocentricity assures the adoption of standardized diagnostic and therapeutic protocols of a tertiary center, on the other hand our results should be validated in a larger multicentric prospective study.
Conclusions
Our study demonstrated a good efficacy of the MPI in identifying PoP patients at high risk of exitus, even if with a suboptimal specificity.
The increase of risk with older age expresses the fragility of aged patients and correlates with the prognostic impact of associated pathologies: mortality increases more than 10 times in the age group between 60 and 80 yo and more than 15 times in the over 80 yo, compared to the under 60 yo group.
An Optimal abdominal clearance at the time of reoperation resulted in primary prognostic importance; therefore we argue that the MPI should be integrated with a score assigned by the surgeon that weights the estimated effectiveness of the intervention practiced, as already reported in the literature [15, 16, 20].
In conclusion, our data underline the importance of an aggressive and early diagnostic-therapeutic approach, particularly when PoP is secondary to upper gastrointestinal tract surgery and when biliary peritonitis is suspected. Advanced age should not be a limitation to reoperation, but on the contrary, a primary indication of an aggressive approach to minimize the MPI score and, therefore, offer patients a better prognosis.
References
Mulier S, Penninckx F, Verwaest C et al (2003) Factors affecting mortality in generalized postoperative peritonitis: multivariate analysis in 96 patients. World J Surg 27:379–384. https://doi.org/10.1007/s00268-002-6705-x
Ruggiero R, Sparavigna L, Docimo G et al (2011) Post-operative peritonitis due to anastomotic dehiscence after colonic resection. Multicentric experience, retrospective analysis of risk factors and review of the literature. Ann Ital Chir 82:369–376
Sartelli M, Chichom-Mefire A, Labricciosa FM et al (2017) The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg 12:29. https://doi.org/10.1186/s13017-017-0141-6
Sartelli M, Griffiths EA, Nestori M (2015) The challenge of post-operative peritonitis after gastrointestinal surgery. Updates Surg 67:373–381. https://doi.org/10.1007/s13304-015-0324-1
Bassetti M, Eckmann C, Giacobbe DR et al (2019) Post-operative abdominal infections: epidemiology, operational definitions, and outcomes. Intensive Care Med 46:163–172
Torer N, Yorganci K, Elker D, Sayek I (2010) Prognostic factors of the mortality of postoperative intraabdominal infections. Infection 38:255–260. https://doi.org/10.1007/s15010-010-0021-4
Copeland GP, Jones D, Walters M (1991) POSSUM: a scoring system for surgical audit. Br J Surg 78:355–360. https://doi.org/10.1002/bjs.1800780327
Kulkarni SV, Naik AS, Subramanian N (2007) APACHE-II scoring system in perforative peritonitis. Am J Surg 194:549–552. https://doi.org/10.1016/j.amjsurg.2007.01.031
Kumar S, Gupta A, Chaudhary S, Agrawal N (2011) Validation of the use of POSSUM score in enteric perforation peritonitis—results of a prospective study. Pan Afr Med J. https://doi.org/10.4314/pamj.v9i1.71197
Wacha H, Linder MM, Feldmann U et al (1987) Mannheim peritonitis index - prediction of risk of death from peritonitis: construction of a statistical and validation of an empirically based index. Theor Surg 1:169–177
Muralidhar VA, Madhu CP, Sudhir S, Srinivasarangan M (2014) Efficacy of Mannheim Peritonitis Index (MPI) score in patients with secondary peritonitis. J Clin Diagnostic Res 8:NC01–NC03. https://doi.org/10.7860/JCDR/2014/8609.5229
Neri A, Marrelli D, Scheiterle M et al (2015) Re-evaluation of mannheim prognostic index in perforative peritonitis: prognostic role of advanced age. A prospective cohort study. Int J Surg 13:54–59. https://doi.org/10.1016/j.ijsu.2014.11.035
Salamone G, Licari L, Falco N et al (2016) Mannheim Peritonitis Index (MPI) and elderly population: prognostic evaluation in acute secondary peritonitis. G Chir 37:243–249. https://doi.org/10.11138/gchir/2016.37.6.243
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Correia MM, Thuler LCS, Velasco E et al (2001) Prediction of death using the Mannheim peritonitis index in oncology patients. Rev Bras Cancerol 47(1):63–68
Billing A, Fröhlich D, Schildberg W (1994) Prediction of outcome using the Mannheim peritonitis index in 2003 patients. Br J Surg 81:209–213. https://doi.org/10.1002/bjs.1800810217
Solomkin Joseph S, Mazuski John E, Bradley John S, Rodvold Keith A, Goldstein Ellie J C, Baron Ellen J, O’Neill Patrick J, Chow Anthony W, Patchen Dellinger E, Eachempati Soumitra R, Gorbach Sherwood, Hilfiker Mary, May Addison K, Nathens Avery B, Robert JGB (2010) Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clin Infect Dis 11:79–109. https://doi.org/10.1086/649554
Malangoni MA (2003) Current concepts in peritonitis. Curr Gastroenterol Rep 5:295–301
Bosscha K, Reijnders K, Hulstaert PF et al (1997) Prognostic scoring systems to predict outcome in peritonitis and intraabdominal sepsis. Br J Surg 84:1532–1534. https://doi.org/10.1002/bjs.1800841110
Mariette C (2006) Principes de prise en charge chirurgicale des péritonites postopératoires. J Chir (Paris) 143:84–87
Funding
This research received no specific grant from any funding agency in the public, commercial or not for- profit sectors.
Author information
Authors and Affiliations
Contributions
AN conceived the study, participated in data collection and analysis, drafted the manuscript. DF conceived the study, participated in statistical analysis and reviewed the manuscript. LM and VS participated in data collection and analysis, provided language help and contributed to the manuscript draft. ABCP and CD participated in data collection and to statistical analysis. FR is the clinical lead and guarantor of the manuscript. DM conceived of the study, participated in its design and coordination and reviewed the final draft. All Authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interest to disclose.
Ethical approval
None required.
Research involving human participants and/or animals
All procedures performed in this study involving patients were in accordance with the ethical standards of the national research commitee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent to consult clinical records was obtained from all patients included in the studies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neri, A., Fusario, D., Marano, L. et al. Clinical evaluation of the Mannheim Prognostic Index in post-operative peritonitis: a prospective cohort study. Updates Surg 72, 1159–1166 (2020). https://doi.org/10.1007/s13304-020-00831-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00831-5