Abstract
More than 10,000 appendectomies are performed every year in Switzerland. The aim of this study was to investigate the treatment strategy for appendicitis among Swiss surgeons with particular interest in laparoscopic technique, method of appendiceal stump closure, and abdominal lavage. We performed an anonymous survey among 540 members of the Swiss Surgical Society. Technical details and differences between the surgical procedures in adults and children as well as in complicated and non-complicated appendicitis were investigated. The overall response rate was 45% (n = 243). 78% of the surgeons perform laparoscopic appendectomies in children and 95% in adult patients. Only 3% use a single incision site technique. Surgeons consider pus or stool in the abdomen (94%), an abscess (86%) or perforation of the appendix (82%), but not an inflamed appendiceal base (16%) as complicated appendicitis. 41% of surgeons use endoloops, 36% a stapling device, and 20% polymeric clips in non-complicated appendicitis for appendiceal stump closure. However, 82% of the surgeons use a stapler in complicated appendicitis. Most (76%) of surgeons do not plunge the appendiceal stump. 24% of surgeons lavage the abdomen with > 1 L of fluid independent of the intraabdominal finding. Most Swiss surgeons perform multiport laparoscopic appendectomies. Endoloops and staplers are mostly used for appendiceal stump closures in uncomplicated appendicitis, and staplers in complicated appendicitis. Only a minor part of surgeons plunge the appendiceal stump or perform routine abdominal lavage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Appendicitis has a lifetime incidence of about 8% with more than 11,000 diagnoses per year in Switzerland, and over 95% of these patients undergoing appendectomy according to federal statistics [1, 2]. Open right lower quadrant incision for appendectomy was first described in 1894 by McBurney [3]. Despite the fact that laparoscopic appendectomy provides multiple benefits over open appendectomy including faster postoperative recovery with less postoperative pain and shorter hospital stay, a lower complication rate, and the possibility to assess the whole abdominal cavity some surgeons still adhere to open appendectomy, particularly in children [4]. Since the first laparoscopic appendectomy performed in 1980 [5, 6], several technical differences performing the procedure have been described, as, e.g., number and placement of trocars. Depending on complicating factors (such as perforation, inflammation of the appendix base, etc.) different techniques of appendiceal stump closure have been described. Frequently used are stapling devices or looped sutures (endoloops) [7, 8]. In addition, the value of intraperitoneal lavage following perforated appendicitis has recently been questioned, especially in children [9,10,11]. The aim of the present study was to assess the commonly applied techniques for appendectomy among surgeons in Switzerland with a special focus on technique of laparoscopy, appendiceal stump closure, and abdominal lavage. Furthermore, definitions of complicated appendicitis by Swiss surgeons were determined.
Methods
Participants
All 540 members of the Swiss Society of Surgeons (Schweizer Gesellschaft für Chirurgie, SGC) representing the majority of Surgeons in Switzerland, were eligible as participants in the present study. Email addresses were obtained from the SGC office and an email with a short introduction and a hyperlink to the online survey was sent directly to the participants. Three email reminders were sent in total.
Questionnaire
We created an anonymous survey by using an online platform (surveymonkey.com, SurveyMonkey Europe UC, Dublin, IRL). The survey was conducted from November to December 2016. Questions covered general information about the participant, their affiliation, and technical details. The participants were also asked regarding a common strategy and the application of postoperative antibiotic treatment and follow-up interval. Anonymous data were then imported and evaluated in Excel (Microsoft Corp., Redmond, WA, USA).
Results
Response rate and distribution of participants
The overall response rate was 45% (n = 243). The majority of participants were experienced surgeons working either as consultants, attending surgeons or head of a department. Only six residents answered the questionnaire. Sixty-five percent of the questionnaire responses came from a cantonal hospital or a primary care hospital, 24% from a private clinic, and 11% from a university hospital. Numbers of performed appendectomies per year at participants’ institution were n 1–100: 43.3%, n 101–200: 37.1%, and n > 200: 19.6% of cases.
Approach: multi-port laparoscopy preferred
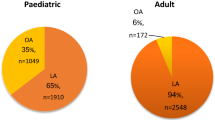
Most of the surgeons prefer a laparoscopic approach for appendectomy: Ninety-five percent in adults, and 78% in children (Fig. 1). Almost all (97%) use a three-trocar laparoscopic approach, with single incision surgeries performed in 3%. Sixty percent of surgeons prefer the following three-port trocar positioning: umbilical, left lower quadrant, above symphysis, and 37% prefer to place the third (above symphysis in the first group) trocar in the right lower quadrant. Seventy-five percent of surgeons mostly use a 10-mm laparoscope while 25% use a 5-mm camera.
Stump closure: endoloops and stapler
The most commonly applied technique for appendiceal stump closure by the surgeon in uncomplicated appendicitis were endoloops (41%), a stapler (36%) or polymeric clips (20%). Metallic clips or ligatures are used only by 2% and 1% of the surgeons, respectively. In complicated appendicitis, surgeons preferred stapler device (82%) far more often than endoloops (12%), polymeric clips (4%) or other methods (2%) (Fig. 2). 76% of the surgeons forego an additional stump coverage after closure and 22% occasionally covering the stump.
Conditions to complicate: pus, perforation, perityphlitic abscess
When asked which condition defines a complicated appendicitis, 94% of the participating surgeons agree with pus or stool in the abdomen, 86% with a perityphlitic abscess, and 83% with perforated appendicitis. 16% of the participants think that an inflamed appendicular base complicates appendicitis. Fluid in the lower pelvis (9%), fibrinous coverings (6%), adhesions (5%), retrocoecal location (4%), or a fecolith (1%) was hardly considered to complicate the disease (Fig. 3).
Lavage
Twenty-four percent use more then 1 L of fluid to lavage the abdomen independent of the intraoperative finding. Among those, most surgeons (74%) use 1–2 L in uncomplicated appendicitis, whereas in complicated cases, only 10% use 1–2 L, 35% use 2–4 L, and 56% of the participants use 4–6 L or even more.
Antibiotics
During postoperative course, 1% of the participants administer antibiotics on a regular base, and 90% only in complicated cases.
Follow-up
After a normal postoperative course and unremarkable histology, patients are normally seen by their general practitioner. However, 16% of the surgeons see their patients regularly following appendectomy as outpatients.
Discussion
The present study assessed the treatment strategy of appendicitis among Swiss surgeons using an online survey. There is no uniform definition of complicated appendicitis among Swiss surgeons. The preferred technique to perform an appendectomy consists of laparoscopy using three ports placed in the umbilicus, the left lower quadrant, and above the symphysis with a 10-mm camera. Endoloops and staplers are most commonly applied for appendiceal stump closure in uncomplicated appendicitis, whereas most surgeons use staplers for complicated appendicitis. Only a minor part of surgeons considers to plunge the appendiceal stump after closure, and only one-fourth performs abdominal lavage independent of the intraoperative finding.
The advantages of the laparoscopic appendectomy compared to an open approach in adults were widely shown in recent literature, consisting of shorter length of hospital stay, less postoperative pain, earlier recovery, and a lower overall complication rate [4, 12]. The World Society of Emergency Surgery Guidelines recommend this approach as first choice, depending on availability of equipment and staff [13], and almost all replying surgeons seem to rely on these advantages when treating adults. However, in children some surgeons prefer an open approach, despite evidence showing a shorter hospital stay and a lower overall morbidity following laparoscopic appendectomy [12, 13]. Hence, some authors recommend that children should be referred to a hospital that offers the laparoscopic approach [14].
Trocar placement and number of used trocars depend on multiple factors, such as patient’s size, size of the abdominal wall, angle of the camera, and surgeon’s preference [15]. In the present survey most surgeons (60%) prefer a triangulated trocar positioning using the belly button, the left lower quadrant, and the area above the symphysis. A triangular trocar position apart from the appendix makes visualization, grasping, and manipulation of the appendix (including application of a stapler/endoloop/clip applier in a 90° angle) ergonomic and easy. Nevertheless, 37% of Swiss surgeons prefer the third trocar to be placed in the right lower quadrant instead of the area above the symphysis. In the authors’ opinion, this latter trocar positioning makes laparoscopic appendectomy technically more demanding, but provides the possibility to increase the right lower trocar site to an open incision if needed. It furthermore avoids the midline above the symphysis where the bladder is located and hence saves from possible bladder injuries with trocar placement. Almost all surgeons prefer a multiport technique with only 3% using single incision surgery. This might be due to the steep learning curve, a higher technical failure rate, and longer operative times following SILS [7, 16], despite evidence showing complication rates, postoperative ileus, length of stay, and postoperative pain not being different when comparing a single incision approach versus multiport appendectomy [17]. Most Swiss surgeons use endoloops (41%) or a stapling device (36%) to close the appendiceal stump in uncomplicated appendicitis, which is in line with reports from other countries [18]. Endoloops are cheaper than staplers and might be operated using a 5-mm port. Nevertheless, as compared to other techniques, endoloops need more tissue manipulation, and the loop might cut through the base of the appendix or slip off if tied too tight or too loose, respectively [8, 17]. Some surgeons consider this technical challenge as a good exercise to improve manual skills especially when teaching residents. Staplers are time efficient, easy to operate, and save especially in complicated appendicitis involving the appendiceal stump or even the coecum [7]. Hence, most surveyed surgeons in Switzerland use a stapler in complicated appendicitis. Polymeric clips (hem-o-lok clips) were described more recently for appendiceal stump closure [19, 20]. They provide a cheap and technically simple alternative to staplers that might be operated via a 10-mm trocar (while a 12-mm trocar is needed for staplers). Whereas the tissue is cut close, but distal to the applied clip or endoloop, leaving a small amount of protruding contaminated mucosa behind, staplers do not leave any mucosa exposed. Whereas some authors argue that this exposed mucosa might be the reason for increased likelihood of postoperative abscess formation following appendectomy using endoloops [8, 21], most trials show no differences concerning the abscess rates when comparing different stump closing techniques [22, 23]. Hem-o-lok clips might seal appendiceal stumps up to a diameter of 1.6 cm, but their reliability decreases when the appendix base measures more than 1 cm [24]. Hence, 21% of Swiss surgeons use polymeric clips to seal the appendiceal stump in uncomplicated appendicitis, but only 5% in complicated cases. In our own cohort of patients we found a reduced abscess rate following appendiceal stump closure using hem-o-lok clips versus endoloops for acute appendicitis [8]. A study comparing the outcomes following appendiceal stump closure with polymeric clips versus staplers for complicated and uncomplicated appendicitis is under perusal. A majority of surgeons in Switzerland forego an additional stump coverage, e.g., with a suture. This is in line with the current literature showing no advantage of stump inversion and coverage neither in the open nor in the laparoscopic approach [13]. A comprehensive definition of ‘complicated appendicitis’ is missing in the literature. Most Swiss surgeons consider pus or stool in the abdomen, a perityphlitic abscess and perforation of the appendix as ‘complicated appendicitis’. Only 16% of participants consider an inflamed appendicular base as ‘complicated appendicitis’. Only 24% of surgeons in Switzerland perform abdominal lavage independent of the intraoperative finding. Various publications, however, have shown no advantages [13, 25] or even a higher postoperative abscess rate following irrigation [10], even in complicated appendicitis.
The overall response rate of the present survey was 45%, which was rather high when comparing to published response rates around 35% from previous surveys among physicians [26]. This especially since male-dominant disciplines (such as general surgery) show typically even lower response rates [26]. Nevertheless, it remains unclear whether the included 45% were representative of all Swiss surgeons or not, especially since our survey was anonymous and hence participants’ factors (such as age, gender, years of experience, etc.) were not compared to the whole population of Swiss surgeons. Furthermore, Pediatric Surgeons (unlike in other countries) are only board certified in Pediatric Surgery, but not in General Surgery. They are hence mostly not part of the Swiss Society of Surgeons and might be underrepresented in the present survey. Finally, only six residents completed the present survey, despite the fact that many chief residents are part of the Swiss Society of Surgeons, indicating that this group might also be underrepresented in the present study.
The response rate of 45% reflects a source of bias, since surgeons answering the questionnaire are likely more interested and up-to-date in the topic than the whole population of Swiss surgeons.
In summary, most Swiss surgeons prefer a multiport laparoscopic approach for appendectomy in adults, but not in children. Endoloops and staplers are commonly used for appendiceal stump closures in uncomplicated appendicitis, and staplers in complicated appendicitis. Only a minor part of surgeons perform routine abdominal lavage or plunge the appendiceal stump. Finally, the definition of ‘complicated appendicitis’ differs among Swiss surgeons.
References
Addiss DG, Shaffer N, Fowler BS, Tauxe RV (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 132(5):910–925 (PubMed PMID: 2239906. Epub 1990/11/01)
BFS BfS. Spitalaufenthalte 2008 Ausgewählte Ergebnisse. CH-2010 Neuchàtel: Bundesamt für Statistik der Schweizerischen Eidgenossenschaft; 2008. http://www.bfs.admin.ch/bfs/portal/de/index/infothek/publ.Document.131717.pdf. Accessed 05 Feb 2018
McBurney C IV (1894) The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg 20(1):38–43 (PubMed PMID: 17860070. Pubmed Central PMCID: PMC1493708. Epub 1894/07/01)
Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X et al (2010) Laparoscopic versus conventional appendectomy—a meta-analysis of randomized controlled trials. BMC Gastroenterol 10:129 (PubMed PMID: 21047410. Pubmed Central PMCID: 2988072)
Semm K (1983) Endoscopic appendectomy. Endoscopy 15(2):59–64 (PubMed PMID: 6221925)
Litynski GS (1998) Kurt Semm and the fight against skepticism: endoscopic hemostasis, laparoscopic appendectomy, and Semm’s impact on the “laparoscopic revolution”. JSLS 2(3):309–313 (PubMed PMID: 9876762. Pubmed Central PMCID: PMC3015306)
Parikh PP, Tashiro J, Wagenaar AE, Curbelo M, Perez EA, Neville HL et al (2018) Looped suture versus stapler device in pediatric laparoscopic appendectomy: a comparative outcomes and intraoperative cost analysis. J Pediatr Surg. 53(4):616–619 (PubMed PMID: 28550935. Epub 2017/05/30)
Soll C, Wyss P, Gelpke H, Raptis DA, Breitenstein S (2016) Appendiceal stump closure using polymeric clips reduces intra-abdominal abscesses. Langenbecks Arch Surg 401(5):661–666 PubMed PMID: 27294658
Akkoyun I, Tuna AT (2012) Advantages of abandoning abdominal cavity irrigation and drainage in operations performed on children with perforated appendicitis. J Pediatr Surg 47(10):1886–1890 (PubMed PMID: 23084202. Epub 2012/10/23)
Hartwich JE, Carter RF, Wolfe L, Goretsky M, Heath K, St Peter SD et al (2013) The effects of irrigation on outcomes in cases of perforated appendicitis in children. J Surg Res 180(2):222–225 (PubMed PMID: 22595016. Epub 2012/05/19)
Snow HA, Choi JM, Cheng MW, Chan ST (2016) Irrigation versus suction alone during laparoscopic appendectomy; a randomized controlled equivalence trial. Int J Surg 28:91–96 (PubMed PMID: 26912015. Epub 2016/02/26)
Agresta F, Ansaloni L, Baiocchi GL, Bergamini C, Campanile FC, Carlucci M et al (2012) Laparoscopic approach to acute abdomen from the Consensus Development Conference of the Societa Italiana di Chirurgia Endoscopica e nuove tecnologie (SICE), Associazione Chirurghi Ospedalieri Italiani (ACOI), Societa Italiana di Chirurgia (SIC), Societa Italiana di Chirurgia d’Urgenza e del Trauma (SICUT), Societa Italiana di Chirurgia nell’Ospedalita Privata (SICOP), and the European Association for Endoscopic Surgery (EAES). Surg Endosc 26(8):2134–2164 (PubMed PMID: 22736283)
Di Saverio S, Birindelli A, Kelly MD, Catena F, Weber DG, Sartelli M et al (2016) WSES Jerusalem guidelines for diagnosis and treatment of acute appendicitis. World J Emerg Surg 11:34 (PubMed PMID: 27437029. Pubmed Central PMCID: PMC4949879. Epub 2016/07/21)
Esposito C, Calvo AI, Castagnetti M, Alicchio F, Suarez C, Giurin I et al (2012) Open versus laparoscopic appendectomy in the pediatric population: a literature review and analysis of complications. J Laparoendosc Adv Surg Tech A 22(8):834–839 (PubMed PMID: 23039707. Epub 2012/10/09)
Ferzli GS, Fingerhut A (2004) Trocar placement for laparoscopic abdominal procedures: a simple standardized method. J Am Coll Surg 198(1):163–173 (PubMed PMID: 14698326. Epub 2003/12/31)
Buckley CE, Kavanagh DO, Gallagher TK, Conroy RM, Traynor OJ, Neary PC (2013) Does aptitude influence the rate at which proficiency is achieved for laparoscopic appendectomy? J Am Coll Surg 217(6):1020–1027 (PubMed PMID: 24051067. Epub 2013/09/21)
Aly OE, Black DH, Rehman H, Ahmed I (2016) Single incision laparoscopic appendicectomy versus conventional three-port laparoscopic appendicectomy: a systematic review and meta-analysis. Int J Surg 35:120–128 (PubMed PMID: 27686264. Epub 2016/10/25)
Clerveus M, Morandeira-Rivas A, Moreno-Sanz C, Herrero-Bogajo ML, Picazo-Yeste JS, Tadeo-Ruiz G (2014) Systematic review and meta-analysis of randomized controlled trials comparing single incision versus conventional laparoscopic appendectomy. World J Surg 38(8):1937–1946 (PubMed PMID: 24682257. Epub 2014/04/01)
Akkoyun I, Akbiyik F (2012) Closing the appendicular stump with a polymeric clip in laparoscopic appendectomy: analysis of 121 pediatric patients. Eur J Pediatr Surg 22(2):133–135 (PubMed PMID: 22517519)
Colak E, Kement M, Ozlem N, Mutlu T, Yildirim K, Gurer A et al (2013) A comparison of nonabsorbable polymeric clips and endoloop ligatures for the closure of the appendicular stump in laparoscopic appendectomy: a prospective, randomized study. Surg Laparosc Endosc Percutan Tech 23(3):255–258 (PubMed PMID: 23751988. Epub 2013/06/12. eng)
Beldi G, Vorburger SA, Bruegger LE, Kocher T, Inderbitzin D, Candinas D (2006) Analysis of stapling versus endoloops in appendiceal stump closure. Br J Surg 93(11):1390–1393 (PubMed PMID: 16862615. Epub 2006/07/25. eng)
Miyano G, Urao M, Lane GJ, Kato Y, Okazaki T, Yamataka A (2011) A prospective analysis of endoloops and endostaples for closing the stump of the appendix in children. J Laparoendosc Adv Surg Tech A 21(2):177–179 (PubMed PMID: 21214418)
Mannu GS, Sudul MK, Bettencourt-Silva JH, Cumber E, Li F, Clark AB et al (2017) Closure methods of the appendix stump for complications during laparoscopic appendectomy. Cochrane Database Syst Rev 11:CD006437 (PubMed PMID: 29190038)
Mayir B, Ensari CO, Bilecik T, Aslaner A, Oruc MT (2015) Methods for closure of appendix stump during laparoscopic appendectomy procedure. Ulus Cerrahi Derg. 31(4):229–231 (PubMed PMID: 26668532. Pubmed Central PMCID: PMC4674045)
St Peter SD, Adibe OO, Iqbal CW, Fike FB, Sharp SW, Juang D et al (2012) Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Ann Surg 256(4):581–585 (PubMed PMID: 22964730. Epub 2012/09/12)
Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E et al (2015) Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 15:32 (PubMed PMID: 25888346. Pubmed Central PMCID: PMC4404667. Epub 2015/04/19)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
The research did not involve human participant or animals.
Informed consent
Not applicable for this type of study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Obrist, N.M., Tschuor, C., Breitenstein, S. et al. Appendectomy in Switzerland: how is it done?. Updates Surg 71, 375–380 (2019). https://doi.org/10.1007/s13304-019-00654-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-019-00654-z