Abstract
Robotic surgery has been proposed over the last decade as a valid option to treat gastrointestinal malignancies in a minimally invasive method, yielding encouraging results. The authors examine the outcomes of a consecutive series of patients with stromal gastrointestinal neoplasms who were operated on using a totally robotic technique. There were 36 patients in the study, with median age 70 years. Resected tumors were located in the esophagus, stomach, duodenum, small intestine and rectum. Perioperative morbidity was 8% and no mortality occurred. R0 resection was achieved in all cases. At a median follow-up of 25 months, 35 patients were disease free while there was one case of death related to metastatic disease. Robotic surgery is a valid option to resect gastrointestinal stromal tumors anywhere along the gastrointestinal tract in a minimally invasive manner.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The introduction of multimodal therapy, especially neoadjuvant therapy [1,2,3], has considerably improved the outcomes of patients with gastrointestinal stromal tumors (GISTs) during the recent years. Nonetheless, even with the advances achieved in combined modality treatment, surgery remains the cornerstone of curative therapy for GISTs [4,5,6,7].
Over the last decades, a dramatic shift toward managing patients via minimally invasive surgery has been observed and minimally invasive approaches are gaining increasing interest also in surgical oncology for the treatment of a number of abdominal malignancies. Indeed, laparoscopy does have the potential of offering a less invasive approach while ensuring oncological radicality and expected survivals. Due to the rarity of lymph node invasion and their propensity to exophytic growth, gastrointestinal stromal tumors (GISTs) can be safely treated with limited resections without the need for routine lymphadenectomy [4,5,6, 8, 9]. Actually, taken together, these features represent an excellent basis for the application of minimally invasive surgery (MIS) [4, 7, 10]. Indeed, as experience and availability of new technologies increased, the recent years have seen the number of minimally invasive GIST resections growing dramatically worldwide, yielding encouraging results [6, 7, 10,11,12,13,14]. However, despite a general demand for minimally invasive surgery, most GISTs and especially those with extragastric locations, are still resected via conventional open surgery [4, 6, 11, 14, 15]. This is essentially in connection with several technical difficulties that may be encountered in resecting such tumors laparoscopically [4,5,6, 14,15,16,17].
Robotic surgery has some hypothetical advantages over traditional laparoscopy and has been successfully applied to resect GISTs, although infrequently [11, 15, 18]. Herein we present our experience on a consecutive series of patients treated with totally robotic resection of GISTs located along the entire gastrointestinal tract.
Materials and methods
Over a 6-year time frame, all consecutive patients with primary GIST who received totally robotic surgery entered the study. A prospectively maintained database was used, which contained details about patient demographics and general characteristics, surgical procedure, postoperative course, pathologic findings, and oncological outcomes. There were no exclusion criteria or contraindication to the minimally invasive technique apart from patient refusal to provide consent for the technique. A procedure-specific informed consent was obtained from each patient.
Preoperative diagnosis assessment featured contrast-enhanced computed tomography (CT), magnetic resonance imaging (MRI), esophagogastroduodenoscopy, colonoscopy, endoscopic ultrasonography (EUS) and positron emission tomography (PET), as needed. Core-needle biopsy was performed when strictly required, depending on clinical conditions. Those patients who received neoadjuvant treatment stopped imatinib a few days before surgery and it was resumed promptly in the postoperative course.
Surgical procedures
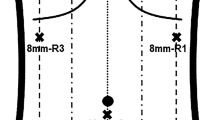
All procedures were performed by surgeons with wide experience in both gastrointestinal and robotic surgery. All surgeries were carried out at two different institutions (two tertiary hospitals). For all interventions, a four-arm Da Vinci Surgical Robot (Intuitive Surgical, Sunnyvale, CA) was employed: a third generation system was used earlier in the series and a fourth generation system later in the series depending on local availability.
Transthoracic subtotal esophagectomy in the case of esophageal location is performed according to Lewis. Briefly, with the patient in the supine position, a gastric conduit is created. The patient is next placed in a left-sided semi-prone position. The esophagus is next divided above the azygos vein, the esophagogastric bloc pulled into the chest and resected. A side-to-side esophagogastric stapled anastomosis is thus performed.
Tumors located at the fundus or at the anterior or posterior gastric wall are resected by wedge resection or fundectomy, depending on cases and tumor size. Antropyloric locations, as well as duodenal neoplasms amenable to local resection are managed with tumor enucleation and direct hand-sewn (robot-sewn) suture of the incisions. The remaining cases of gastric and duodenal tumors are managed with distal gastrectomy (DG) and pancreaticoduodenectomy (PD), respectively. DG and PD are performed according to the technique we described previously, with the exception of lymphadenectomy, which is performed only in the presence of macroscopic evidence of lymphadenopathy [19, 20]. Particularly, following DG the digestive continuity is restored via intracorporeal gastrojejunal anastomosis with antecolically routed Roux-en-Y limb. PD is performed with end-to-side, duct-to-mucosa pancreaticojejunostomy; the pylorus is preserved and gastrojejunal anastomosis performed with an antecolic omega loop in end-to-side fashion [20]. All cases of small bowel tumor are treated with formal bowel resection and stapled side-to-side anastomosis. Rectal locations are managed as for duodenal locations, with local enucleation and direct hand-sewn suture of the incisions. Where needed, for any location robot-integrated ultrasound is employed to extemporaneously control the exact location and to verify tumor margins during resection [21].
Intraoperative blood losses were estimated by visual assessment of graduated suction canisters. Operative time was calculated as the time between skin incision and port-site closure. The same surgical group followed all patients in the postprocedural course and postoperative complications were categorized and recorded using the Clavien–Dindo classification [22]. Major morbidity was defined as the presence of any level III–V complication. Pathologic staging was made according to the criteria proposed by Fletcher et al. [23].
Each patient was followed in a multidisciplinary manner involving surgical, medical, and oncological specialists. Any local or distant recurrence was defined radiologically, with or without pathologic confirmation. Any adjuvant therapy program was established by consensus.
Statistical analysis was performed using the Statistical Package for the Social Sciences, v20.0 (SPSS Inc., Chicago, IL, USA), with results presented in descriptive statistics.
Results
During the period between January 2011 and December 2016, 36 patients of median age 70 years (range 20–81) underwent surgery. Of these, 15 patients (41%) were male.
The distal esophagus was affected in two cases. The stomach was the most frequent site of disease (22 cases). The duodenum was affected in 5 cases, while there were 5 cases of small bowel location and two of rectal location. In total, 5 patients (14%) had neoadjuvant therapy. Patients’ characteristics with relative indications for surgery are given in Table 1. During the same period 5 patients received open surgery because of inability to tolerate pneumoperitoneum or the presence of large mass (> 10 cm) at preoperative assessment. All 5 patients had gastric neoplasm. Of these, 4 patients underwent distal gastrectomy, and one patient underwent gastric fundectomy with distal pancreatectomy.
The main 36 robotic procedures performed consisted of the following: 2 partial esophagectomies, 20 wedge gastric resections, 2 DG, 2 PD, 3 duodenal enucleations, 5 small bowel resections, and 2 rectal enucleations. There was no tumor rupture or spillage and no conversion to open surgery occurred. Three patients received concomitant procedures, including cholecystectomy, liver wedge resection and renal enucleation of a cystic mass. Median estimated blood loss was 20 mL (0–250).
Overall, the median operative time was 125 min (range 70–570). A total of 3 patients (8%) experienced some postoperative complications, whereby one patient (3%) had major medical complication. Of note, one patient who received gastric wedge resection and enucleation of a renal mass had postoperative pneumonia. One other patient had macroscopic hematuria, which cleared spontaneously without sequelae while in the hospital. One further patient required prolonged hospitalization due to postoperative stroke, which resulted in no permanent disability. The median postoperative hospital stay was 4 (range 2–27) days. Surgical procedures and outcomes are summarized in Table 2.
Median tumor size was 4 cm (range 1–8). At histopathology examination, no case of microscopic margin involvement was noticed. According to the Fletcher criteria [23], 9 tumors were categorized as very low risk, 18 low risk and 7 intermediate risk. At histologic assessment, CD117 and CD34 staining results were positive in 31 and 20 patients, respectively. Pathologic findings are summarized in Table 3. Follow-up oncological information was available for all patients. Median duration of follow-up was 25 months, ranging between 1 and 51 months, the overall survival was 97%. Of note, one disease-related death occurred, in a patient who developed metastatic peritoneal disease and succumbed 27 months after resection. Oncological outcomes are given in Table 4.
Discussion
The purpose of this study was to evaluate the feasibility and outcomes of robotic resection of GISTs at any location along the entire digestive tract. To the best of our knowledge, this is the first report on minimally invasive GIST resection ranging from esophagectomy to rectal resection and represents the largest series of patients receiving robotic surgery [11, 15, 18, 24]. The present study suggests that the robot can be employed to resect GISTs in a minimally invasive manner competently, even in the case of unfavorable locations [4,5,6, 13,14,15,16].
Immediate pathological findings reveal an excellent rate of margin-negative resections, which was as high as 100% in our series. Interestingly, the percentage of disease-free patients was 97% at a median follow-up greater than 2 years. This data is consistent with other results concerning standard laparoscopic surgery, and globally compares favorably with that associated with conventional surgery concerning GISTs of the entire gastrointestinal tract [17, 25]. Similarly, overall survival was comparable to that reported after conventional open and laparoscopic procedures in the imatinib era [14, 16, 17].
The significant limitations that are still associated with endoscopic treatment, especially for extirpating large tumors, combined with the morbidity of conventional open surgery render minimally invasive surgery an optimal method to manage GISTs [4,5,6, 11, 17, 26]. Actually, despite the lack of prospective, randomized comparisons upon the matter, growing evidence exists that the application of minimally invasive techniques to GIST surgery may offer better perioperative results compared to conventional open surgery, while maintaining the expected survivals [5, 7]. Koh and colleagues [26] have recently compared conventional minimally invasive versus standard open resection for gastric GISTs on the available data from the literature. In their well-conducted systematic review with meta-analysis, the authors analyzed 11 nonrandomized studies, including a total of 765 patients. Overall, at the analysis of pooled data, laparoscopy showed significantly lower intraoperative blood losses, lower rate of minor postoperative complications and length of hospital stay as compared to conventional surgery. Conversely, no significant difference was found between the two groups in terms of major morbidity, rate of R0 resection, disease-free survival and overall survival, although this difference should be interpreted in the light of a statistically significant higher rate of high-risk tumors and an increased rate of formal gastrectomies in the open compared with the laparoscopic group.
Despite the known advantages on postoperative outcomes of the minimally invasive method, the application of laparoscopy generally encounters a number of technical hindrances when managing extragastric neoplasms [5, 6, 11, 17]. For tumors located at the esophagogastric junction, at the antropyloric area, as well as in the case of duodenal or jejunal locations, wedge stapled resection are generally contraindicated, due to the increased risk of stenosis and/or delayed gastric emptying [5, 16,17,18, 27, 28]. As a consequence, after tumor extirpation, incisions are better hand-sewn than stapled and this makes the procedure highly demanding to be performed laparoscopically [5, 16, 17, 28]. As far as duodenal enucleation is concerned, it is interesting to notice that scarce data currently exist concerning the application of minimally invasive surgery, with few series reporting on robotic surgery [11, 29]. In 2015, Downs-Canners and colleagues [29] published the retrospective analysis of a multi-institutional experience with robotic duodenal resection for benign and borderline duodenal tumors, which included adenomas, neuroendocrine tumors, lipomas and two GISTs. In the same year, Vicente et al. [11] reported on three robotic enucleations of duodenal GISTs within a small series including gastric and duodenal locations. Both experiences reported on hand-sewn duodenal closure and revealed optimal outcomes in terms of surgical and oncological data.
Actually, the intrinsic limitations to the application of laparoscopy are essentially connected to an unstable, bi-dimensional intraoperative view, a limited freedom of movement of surgical tools within narrow spaces and, importantly, poor ergonomics for surgeons [30]. In this respect, over the last decade robotics has represented one of the most promising novelties in surgical practice [11, 15]. A number of technical issues connected with conventional laparoscopy have been overcome, at least partially, by robotic platforms, which permit magnified 3-dimensional intraoperative view and enhanced surgical dexterity on fine anatomical dissections. These features enable not only easier resecting and suturing, thus permitting more accurate anastomoses, but also facilitate the management of possible intraoperative complications such as major bleedings [18, 21]. In this regard, robotic systems represent an alternative option to perform in a minimally invasive manner the same procedures normally achieved in a conventional open fashion, ranging from esophagectomy to PD, to the extirpation of tumors with duodenal or rectal location [20, 30, 31].
The significant cost related to the purchase and maintenance of robotic platforms is still regarded as a crucial issue limiting wide diffusion in clinical practice. However, the actual economic impact of robotic surgery should be evaluated over time. It is worth noting that although only one system has been largely used in clinical setting during the last decade, less expensive platforms are being made available currently. Thus, a growing competition is likely to be observed in the future [21, 30].
Several limitations to the present study are to be acknowledged. First, despite the analysis of an unselected, consecutive series gathered from a prospectively maintained database, it has a retrospective nature and lacks a comparator group. In addition, as the study covered only nearly 6 years, an actual estimation of long-term oncological results cannot be reliably reached. However, the median follow-up, ranging between 1 and 51 months, is likely to reflect appropriately the general trend [1]. Finally, there were predominantly low-risk patients in the series (< 20% ASA III) and this may have influenced positively our general results.
Conclusions
Definitive conclusions cannot be drawn due to the lack of high-level evidence. However, our results suggest that robotics can be considered as a valid option to extirpate neoplasms located anywhere along the entire gastrointestinal tract with a minimally invasive technique.
References
ESMO/European Sarcoma Network Working Group (2014) Gastrointestinal stromal tumors: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25(Suppl 3):21–26
Demetri GD, von Mehren M, Blanke CD et al (2002) Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med 347:472–480
Dematteo RP, Ballman KV, Antonescu CR, American College of Surgeons Oncology Group (ACOSOG) Intergroup Adjuvant GIST Study Team et al (2009) Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumour: a randomised, double-blind, placebo-controlled trial. Lancet 373:1097–1104
MacArthur KM, Baumann BC, Nicholl MB (2017) Laparoscopic versus open resection for gastrointestinal stromal tumors (GISTs). J Gastrointest Cancer 48:20–24
De Vogelaere K, Hoorens A, Haentjens P, Delvaux G (2013) Laparoscopic versus open resection of gastrointestinal stromal tumors of the stomach. Surg Endosc 27:1546–1554
Hsiao CY, Yang CY, Lai IR, Chen CN, Lin MT (2015) Laparoscopic resection for large gastric gastrointestinal stromal tumor (GIST): intermediate follow-up results. Surg Endosc 29:868–873
Sicklick JK, Lopez NE (2013) Optimizing surgical and imatinib therapy for the treatment of gastrointestinal stromal tumors. J Gastrointest Surg 17:1997–2006
Demetri GD, Benjamin RS, Blanke CD, NCCN Task Force et al (2007) NCCN Task Force report: management of patients with gastrointestinal stromal tumor (GIST)–update of the NCCN clinical practice guidelines. J Natl Compr Canc Netw 5(Suppl 2):S1–S29 (quiz S30)
DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF (2000) Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg 231:51–58
Novitsky YW, Kercher KW, Sing RF, Heniford BT (2006) Long-term outcomes of laparoscopic resection of gastric gastrointestinal stromal tumors. Ann Surg 243:738 (discussion 745–737)
Vicente E, Quijano Y, Ielpo B, Duran H, Diaz E, Fabra I, Malave L, Ferri V, Ferronetti A, Caruso R (2016) Robot-assisted resection of gastrointestinal stromal tumors (GIST): a single center case series and literature review. Int J Med Robot 12:718–723
Chung JC, Chu CW, Cho GS, Shin EJ, Lim CW, Kim HC, Song OP (2010) Management and outcome of gastrointestinal stromal tumors of the duodenum. J Gastrointest Surg 14:880–883
Chi JL, Xu M, Zhang MR, Li Y, Zhou ZG (2017) Laparoscopic versus open resection for gastric gastrointestinal stromal tumors (GISTs): a size-location-matched case–control study. World J Surg. https://doi.org/10.1007/s00268-017-4005-8
Pucci MJ, Berger AC, Lim PW, Chojnacki KA, Rosato EL, Palazzo F (2012) Laparoscopic approaches to gastric gastrointestinal stromal tumors: an institutional review of 57 cases. Surg Endosc 26:3509–3514
Buchs NC, Bucher P, Pugin F, Hagen ME, Morel P (2010) Robot-assisted oncologic resection for large gastric gastrointestinal stromal tumor: a preliminary case series. J Laparoendosc Adv Surg Tech 20:411–415
Tanaka E, Kim M, Lim JS, Choi YY, Saklani A, Noh SH, Hyung WJ (2015) Usefulness of laparoscopic side-to-side duodenojejunostomy for gastrointestinal stromal tumors located at the duodenojejunal junction. J Gastrointest Surg 19:313–318
Silberhumer GR, Hufschmid M, Wrba F, Gyoeri G, Schoppmann S, Tribl B, Wenzl E, Prager G, Laengle F, Zacherl J (2009) Surgery for gastrointestinal stromal tumors of the stomach. J Gastrointest Surg 13:1213–1219
Moriyama H, Ishikawa N, Kawaguchi M, Hirose K, Watanabe G (2012) Robot-assisted laparoscopic resection for gastric gastrointestinal stromal tumor. Surg Laparosc Endosc Percutan Tech 22(e155–6):1
Amore Bonapasta S, Guerra F, Linari C, Annecchiarico M, Boffi B, Calistri M, Coratti A (2017) Robot-assisted gastrectomy for cancer. Chirurg 88:12–18
Coratti A, Di Marino M, Coratti F, Baldoni G, Guerra F, Amore Bonapasta S, Bencini L, Farsi M, Annecchiarico M (2016) Initial experience with robotic pancreatic surgery: technical feasibility and oncological implications. Surg Laparosc Endosc Percutan Tech 26:31–37
Guerra F, Amore Bonapasta S, Annecchiarico M, Bongiolatti S, Coratti A (2015) Robot-integrated intraoperative ultrasound: initial experience with hepatic malignancies. Minim Invasive Ther Allied Technol 24:345–349
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Fletcher CD, Berman JJ, Corless C et al (2002) Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol 33:459–465
Al-Thani H, El-Menyar A, Mekkodathil A, Elgohary H, Tabeb AH (2017) Robotic management of gastric stromal tumors (GIST): a single Middle Eastern center experience. Int J Med Robot 13(1):a1729
Conlon KC, Casper ES, Brennan MF (1995) Primary gastrointestinal sarcomas: analysis of prognostic variables. Ann Surg Oncol 2:26–31
Koh YX, Chok AY, Zheng HL, Tan CS, Chow PK, Wong WK, Goh BK (2013) A systematic review and meta-analysis comparing laparoscopic versus open gastric resections for gastrointestinal stromal tumors of the stomach. Ann Surg Oncol 20:3549–3560
Correa-Cote J, Morales-Uribe C, Sanabria A (2014) Laparoscopic management of gastric gastrointestinal stromal tumors. World J Gastrointest Endosc 6:296–303
Kiyozaki H, Saito M, Chiba H, Takata O, Rikiyama T (2014) Laparoscopic wedge resection of the stomach for gastrointestinal stromal tumor (GIST): non-touch lesion lifting method. Gastric Cancer 17:337–340
Downs-Canner S, Van der Vliet WJ et al (2015) Robotic surgery for benign duodenal tumors. J Gastrointest Surg 19:306–312
Guerra F, Pesi B, Amore Bonapasta S, Perna F, Di Marino M, Annecchiarico M, Coratti A (2016) Does robotics improve minimally invasive rectal surgery? Functional and oncological implications. J Dig Dis 17:88–94
Ruurda JP, van der Sluis PC, van der Horst S, van Hilllegersberg R (2015) Robot-assisted minimally invasive esophagectomy for esophageal cancer: a systematic review. J Surg Oncol 112:257–265
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the aforementioned authors declare no competing commercial, personal, political, intellectual, or religious conflict of interests in relation to the present work. No grant or other financial support has been received for the drawing up of the present paper. Dr. Gasperoni has received grants by Novartis, Pfizer e Bayer.
Ethics approval
All procedures were in accordance with the ethical standards of the institutional and national research committee and with the Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
A procedure-specific informed consent has been obtained from each patient.
Rights and permissions
About this article
Cite this article
Guerra, F., Paolini, C., Vegni, A. et al. Feasibility of robotic resection of gastrointestinal stromal tumors along the entire gastrointestinal tract. Updates Surg 71, 695–700 (2019). https://doi.org/10.1007/s13304-018-0568-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0568-7