Abstract
Laparoscopic cholecystectomy (LC) performed for acute cholecystitis (AC) is usually advised within 72 h of symptom onset. This study aimed to evaluate the outcomes of LC beyond 72 h after presentation. A total of 94 patients underwent LC for AC between January 2012 and February 2015: 70 underwent early LC (ELC, operation within 72 h of symptom onset) and 24 underwent late LC (LLC, beyond 72 h). The outcomes of the groups were compared. Preoperative C-reactive protein (CRP) levels were significantly higher in the LLC group [9.81 (0.41–38.00) mg/dL] compared to the ELC group [1.05 (0.05–24.20) mg/dL; P = 0.001]. Between-group differences were also observed in operative time, blood loss, and postoperative hospital stay [ELC, 76 (37–141) minutes, 10 (1–650) ml and 4 (3–12) days; LLC, 89 (48–234) minutes, 40 (1–3500) ml, and 6 (4–35) days; P = 0.048, 0.007, and <0.001]. The conversion rate of laparoscopic to open cholecystectomy was significantly higher in the LLC group (17%) than the ELC group (1%; P = 0.014). Univariate analysis identified LLC, CRP ≥10 mg/dL, and failure to create a critical view of safety as risk factors for conversion to open surgery, while operative time ≥90 min and blood loss ≥100 ml were risk factors for complications. LLC is associated with longer operation times, greater blood loss, longer hospital stays and higher conversion rates than ELC. Using a high CRP value as a criterion for selecting a surgical procedure, whether open or laparoscopic, would decrease the conversion rate of LLC, which may reduce operation times and blood loss.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
According to the updated Tokyo Guidelines 2013 (TG13), the optimal treatment for acute cholecystitis (AC) is early laparoscopic cholecystectomy (LC), particularly when less than 72 h have passed since the onset of symptoms [1]. However, using this treatment for AC beyond 72 h of symptom onset is controversial. Because the operative difficulty of LC for late AC is greater, elective surgery has been recommended after several weeks or more; alternatively, careful LC may be performed by an expert team [1, 2]. A recent randomized trial showed that immediate LC should become the therapy of choice for AC in operable patients, although the time of symptom onset was not reported [3]. To date, a few reports have compared the surgical results of LC performed within vs. beyond 72 h of symptom onset.
Here, we analyzed the clinical features and surgical outcome of LC for AC both within and beyond 72 h of symptom onset. The aim of this study was to evaluate the outcomes of LC beyond 72 h of presentation and to develop a new criterion for the therapeutic strategy used for AC, especially for late AC.
Methods
Patient selection
We identified 94 patients who underwent LC for AC between January 2012 and February 2015 at the Department of Surgery, Ogaki Municipal Hospital.
Patients with AC were divided into two groups based on the time that had elapsed between symptom onset and surgery: the patients in the early LC (ELC) group were operated on within 72 h of symptom onset, and the patients in the late LC (LLC) group were operated on beyond 72 h after symptom onset [2]. The outcomes of the groups were compared.
AC was diagnosed following current diagnostic criteria [4]. When AC was suspected based on clinical signs (Murphy’s sign, right upper abdominal quadrant pain, and fever) and blood test results [elevated C-reactive protein (CRP) levels or elevated white blood cell (WBC) counts], a definite diagnosis was made through confirmation by diagnostic imaging using ultrasonography and/or computed tomography (CT) scans. The imaging findings for AC include an enlarged gallbladder, wall thickening, subserosal edema, and mucosal enhancement. After diagnosing AC, magnetic resonance cholangiopancreatography (MRCP) was performed to obtain a cholangiogram of sufficient quality to exclude common bile duct stones.
According to our institutional policy, LC was performed for AC for patients without previous upper abdominal laparotomy and without major co-morbidity. For patients with organ dysfunction (i.e., cardiovascular or respiratory dysfunction or coagulation), previous upper abdominal surgery or low-performance status, we performed primary open cholecystectomy; these patients were excluded from the study cohort.
Even for patients with preoperative strict inflammation, our policy was to use LC. In contrast, for patients with perforated AC or Mirizzi syndrome, we typically performed primary open cholecystectomy. Patients with choledocholithiasis, cholangitis or gallbladder tumors were also excluded from this study. For these patients, we typically consider cholecystectomy only after conservative treatment, such as antibiotic therapy or percutaneous transhepatic gallbladder drainage (PTGBD). Disease severity was classified according to the TG13 [4].
Surgical procedure
LC was performed as soon as possible after confirmation of AC. Perioperative intravenous antibiotic therapy was administered to all patients. Residents usually performed LC with a senior doctor who had more than 10 years of surgical experience.
The standard four-trocar operative technique was used for LC. Because the gallbladder was usually distended, it was first aspired and decompressed. To create a critical view of safety, Calot’s triangle was dissected of fat and fibrous tissue and the lower end of the gallbladder was dissected off the liver bed [1, 5]. When dense adhesions were present at Calot’s triangle and it was difficult to create a critical view of safety, either the structures in the lowest part of the gallbladder were carefully ligated or retrograde cholecystectomy was performed to avoid common bile duct injury. However, we readily converted to open surgery when experiencing difficulties performing LC [1]. A drain was routinely left in the gallbladder bed. Follow-up at the outpatient clinic continued until the patients felt fully recovered and had no further postoperative complaints.
Statistical analysis
Measurement values for continuous variables are expressed as the median (range) or the mean ± standard deviation. Case characteristics were compared using the Mann–Whitney U test for continuous variables and the Chi-square test for categorical variables. Fisher’s exact test was also applied when appropriate. Multivariate analysis was performed with a logistic regression test using a forward stepwise selection model. The results were considered statistically significant for P values <0.05. All calculations were performed using the IBM SPSS Statistics 16 software package (IBM Japan Inc., Tokyo, Japan).
Results
Comparison between early and late LC
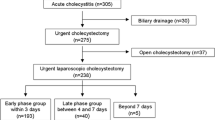
Figure 1 shows the number of cases separated according to the time from symptom onset to operation. A total of 94 patients underwent LC for AC; 70 patients underwent ELC and 24 underwent LLC. The outcomes of the groups were compared (Table 1).
Age, gender, and body mass index distributions were similar between the groups. In total, 33 of the 70 (47%) patients who underwent ELC had known existence of their gallstones preoperatively, whereas only 4 of the 24 (17%) patients who underwent LLC had known their gallstones (P = 0.008). The preoperative laboratory data were relatively comparable between the two groups. However, preoperative CRP levels were significantly higher in the LLC group [9.81 (0.41–38.00) mg/dL] compared to the ELC group [1.05 (0.05–24.20) mg/dL; P = 0.001], and albumin levels in the LLC group were significantly lower [4.2 (3.0–4.6) g/dL] than in the ELC group [4.5 (3.0–5.8) g/dL; P = 0.001]. Tokyo severity grade differed between the groups, because the criteria for grade II AC include symptom persistence for more than 72 h after symptom onset [4].
Between-group differences in operative time and blood loss were also observed [ELC, 76 (37–141) minutes, 10 (1–650) ml; LLC, 89 (48–234) minutes, 40 (1–3500) ml; P = 0.048, 0.007]. Of note, a critical view of safety was created in only 13 of the 24 (54%) LLC cases, while it was achieved in 64 of the 70 (91%) ELC cases (P < 0.001). In addition, the rate of conversion from laparoscopic to open surgery was significantly higher in the LLC group (17%) than the ELC group (1%; P = 0.014). Complications, defined by Clavien–Dindo Grade ≥ II [6], occurred in 7 of the 70 (10%) ELC patients and in 5 of the 24 (21%) LLC patients (P = 0.154), and no mortality was observed. Wound infection, abscess formation, and choledocholithiasis were observed in three cases each and were the most common complications in the cohort. Notably, there were no instances of major bile duct injury. The patients in the LLC group had a significantly longer postoperative hospital stay [6 (4–35) days] than those in the ELC group [4 (3–12) days; P < 0.001].
Risk factors for conversion to open surgery and complications
Sixteen preoperative variables were analyzed as potential risk factors for conversion to open surgery (Table 2). Univariate analysis identified four variables, i.e., surgery beyond 72 h of symptom onset, CRP ≥10 mg/dL, Tokyo severity grade II or III, and failure to create a critical view of safety, as risk factors for conversion to open surgery. However, duration from symptom onset and Tokyo severity grade were apparently correlated because of the criterion associated with the latter [4]. Because the number of patients in the conversion group was small, multivariate analysis could not be adopted.
Among the 19 perioperative variables analyzed, operative time ≥90 min and blood loss ≥100 ml were identified as risk factors for complications in univariate analysis (Table 3). Multivariate logistic regression analysis revealed blood loss ≥100 ml as an independently correlated risk factor for complications (odds ratio 7.2; 95% CI 1.9–26.7; P = 0.003).
Discussion
The present comparison of ELC and LLC showed that LLC was associated with longer operation time, greater blood loss, higher conversion rate and longer hospital stay compared to ELC. However, the 24 patients who underwent LLC had acceptable surgical results. According to the TG13, LC is recommended for patients with AC when less than 72 h have passed since symptom onset [1]. It is well known that LLC is relatively difficult to perform in the presence of severe local inflammation. Generally, for LLC, early gallbladder drainage and elective surgery after several weeks or more are recommended [1]. However, carefully performed LC by a team of experts may be acceptable [2]. Indeed, our data suggested that operative difficulty increased as the delay from symptom onset time increased because of an inability to create a critical view of safety, which occurred in 11 of the 24 (46%) patients who underwent LLC. Nonetheless, no significant between-group differences were observed regarding complications, and no major bile duct injury or mortality occurred. A few studies have reported surgical results for LLC. Zhu et al. reported favorable surgical outcomes for both ELC and LLC in a study of 133 patients who were operated on by two expert surgeons; both operations were deemed safe due to the lack of conversion to open surgery and the absence of complications, except for wound infection [2]. However, the results of the current study are more generalizable, because less experienced surgeons and residents performed 21 of the 24 (87%) LLCs. Thus, careful LC may be an option for AC when more than 72 h have elapsed from symptom onset.
This study demonstrated that symptom duration of longer than 72 h is a significant risk factor for conversion to open surgery, in addition to high CRP levels and failure to create a critical view of safety (Table 2). LC for AC is associated with reduced hospital stay, quick recovery, a few complications, and reduced costs [1, 2, 7, 8]. However, LC is not recommended for all cases of AC due to potential difficulties that can arise during cholecystectomy resulting from severe inflammation [1, 9]. According to the TG13, surgeons should consider conversion to open cholecystectomy when they fail to create a critical view of safety [1]. Therefore, whether laparoscopic or open surgery is performed should be defined preoperatively, especially for patients with AC with a symptom duration of longer than 72 h. Our results indicate that a CRP level higher than 10 mg/dl is also a risk factor for conversion to open surgery. CRP level may be sensitively and specifically influenced by local inflammation and is, therefore, a useful predictor for the need to convert to open surgery [10]. Meanwhile, WBC count, one of the diagnostic criteria for assessing Tokyo severity grade [4], was not associated with conversion to open surgery. Indeed, elevations in WBC count may decrease in subacute or chronic cholecystitis. Some previous reports have also supported using CRP level as a factor for determining conversion [10–13]. Therefore, using high CRP level as a criterion for selecting a surgical procedure should decrease the conversion rate of LLC, which may reduce operation times and blood loss. Re-evaluation of the utility of CRP level in this context is needed with a larger cohort.
Although duration from symptom onset was not associated with postoperative complications, operative time and blood loss were identified as potential predictors of complications in univariate analysis. This means that reduced operative times and blood loss would contribute to patient safety. Because conversion to open surgery wastes time and causes blood loss, the selection of an appropriate therapeutic strategy, i.e., open or laparoscopic surgery, might help decrease the rate of postoperative complications. It has been reported that ELC can decrease the rates of both postoperative complications and conversion [1, 10], while the correlation between LLC and complication rate remains unclear. Because our cohort was not large enough to support multivariate analysis, larger population-based studies are needed to clarify our results.
In conclusion, LLC is associated with longer operation times, greater blood loss, higher conversion rates to open surgery and longer hospital stays than ELC. Adoption of a high CRP level as a criterion for selecting a surgical procedure, whether open or laparoscopic, should decrease the conversion rate of LLC, which may reduce operation times and blood loss. Thus, the therapeutic strategy used for AC beyond 72 h of symptom onset should be carefully considered.
References
Yamashita Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Buchler MW, Gomi H, Dervenis C, Windsor JA, Kim SW, de Santibanes E, Padbury R, Chen XP, Chan AC, Fan ST, Jagannath P, Mayumi T, Yoshida M, Miura F, Tsuyuguchi T, Itoi T, Supe AN, Tokyo Guideline Revision C (2013) TG13 surgical management of acute cholecystitis. J Hepato-Biliary-Pancreat Sci 20(1):89–96. doi:10.1007/s00534-012-0567-x
Zhu B, Zhang Z, Wang Y, Gong K, Lu Y, Zhang N (2012) Comparison of laparoscopic cholecystectomy for acute cholecystitis within and beyond 72 h of symptom onset during emergency admissions. World J Surg 36(11):2654–2658. doi:10.1007/s00268-012-1709-7
Gutt CN, Encke J, Koninger J, Harnoss JC, Weigand K, Kipfmuller K, Schunter O, Gotze T, Golling MT, Menges M, Klar E, Feilhauer K, Zoller WG, Ridwelski K, Ackmann S, Baron A, Schon MR, Seitz HK, Daniel D, Stremmel W, Buchler MW (2013) Acute cholecystitis: early versus delayed cholecystectomy, a multicenter randomized trial (ACDC study, NCT00447304). Ann Surg 258(3):385–393. doi:10.1097/SLA.0b013e3182a1599b
Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, Pitt HA, Garden OJ, Kiriyama S, Hata J, Gabata T, Yoshida M, Miura F, Okamoto K, Tsuyuguchi T, Itoi T, Yamashita Y, Dervenis C, Chan AC, Lau WY, Supe AN, Belli G, Hilvano SC, Liau KH, Kim MH, Kim SW, Ker CG, Tokyo Guidelines Revision C (2013) TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepato-Biliary-Pancreat Sci 20(1):35–46. doi:10.1007/s00534-012-0568-9
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(1):101–125
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196. doi:10.1097/SLA.0b013e3181b13ca2
Zafar SN, Obirieze A, Adesibikan B, Cornwell EE 3rd, Fullum TM, Tran DD (2015) Optimal time for early laparoscopic cholecystectomy for acute cholecystitis. JAMA surgery 150(2):129–136. doi:10.1001/jamasurg.2014.2339
de Mestral C, Rotstein OD, Laupacis A, Hoch JS, Zagorski B, Alali AS, Nathens AB (2014) Comparative operative outcomes of early and delayed cholecystectomy for acute cholecystitis: a population-based propensity score analysis. Ann Surg 259(1):10–15. doi:10.1097/SLA.0b013e3182a5cf36
Borzellino G, Sauerland S, Minicozzi AM, Verlato G, Di Pietrantonj C, de Manzoni G, Cordiano C (2008) Laparoscopic cholecystectomy for severe acute cholecystitis. A meta-analysis of results. Surg Endosc 22(1):8–15. doi:10.1007/s00464-007-9511-6
Asai K, Watanabe M, Kusachi S, Matsukiyo H, Saito T, Kodama H, Kiribayashi T, Enomoto T, Nakamura Y, Okamoto Y, Saida Y, Nagao J (2014) Risk factors for conversion of laparoscopic cholecystectomy to open surgery associated with the severity characteristics according to the Tokyo guidelines. Surg Today 44(12):2300–2304. doi:10.1007/s00595-014-0838-z
Wevers KP, van Westreenen HL, Patijn GA (2013) Laparoscopic cholecystectomy in acute cholecystitis: C-reactive protein level combined with age predicts conversion. Surg Laparos Endos Percutan Tech 23(2):163–166. doi:10.1097/SLE.0b013e31826d7fb0
Teckchandani N, Garg PK, Hadke NS, Jain SK, Kant R, Mandal AK, Bhalla P (2010) Predictive factors for successful early laparoscopic cholecystectomy in acute cholecystitis: a prospective study. Int J Surg 8(8):623–627. doi:10.1016/j.ijsu.2010.05.014
Schafer M, Krahenbuhl L, Buchler MW (2001) Predictive factors for the type of surgery in acute cholecystitis. Am J Surg 182(3):291–297
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
We declare that in the study were respected the ethical standards conformed to the guidelines of the Helsinki Declaration. No study advertising was made and no remuneration was offered.
Research involving human participants and/or animals
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Onoe, S., Kaneoka, Y., Maeda, A. et al. Feasibility of laparoscopic cholecystectomy for acute cholecystitis beyond 72 h of symptom onset. Updates Surg 68, 377–383 (2016). https://doi.org/10.1007/s13304-016-0409-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-016-0409-5