Abstract
Recently, somatic mutations in SRSF2 gene have been discovered in a proportion of hematologic malignancies including acute myeloid leukemia (AML). This study was aimed to investigate SRSF2 mutations in Chinese AML patients. High-resolution melting analysis (HRMA) was developed to screen SRSF2 mutations in 249 cases with AML, and then direct DNA sequencing was used to verify the results of HRMA. In this study, 3.6 % (9/249) of Chinese AML patients were found with heterozygous SRSF2 mutations. Patients with SRSF2 mutations were older than those with wild-type SRSF2 (P = 0.014). No differences in the sex, blood parameters, French–American–British classification (FAB) subtypes, and karyotypes were observed between AML patients with and without SRSF2 mutations. Although the overall survival (OS) of SRSF2-mutated patients was inferior to those without mutations in both whole AML patients (median 4 vs. 11 months, respectively; P = 0.006) and cytogenetically normal patients (median 2 vs. 12 months, respectively; P = 0.008), multiple analysis disclosed that SRSF2 mutation was not an independent prognostic factor in AML patients. These results suggest that SRSF2 mutation occurs at a low frequency in aged AML patients and might not be associated with adverse prognosis in Chinese AML patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is the most common type of hematologic neoplasms in adults, which is characterized by an abnormal expansion of hematopoietic stem/progenitor cells with limited differentiation and excessive proliferation. Conventional cytogenetics analysis finds that approximately 55 % of AML patients exhibit chromosome abnormalities, which can be utilized widely to evaluate the risk status of AML [1]. With the fast development of genetic technology, the discoveries of somatic gene mutations involved in tyrosine kinase signaling, transcriptional, and epigenetic regulation have contributed to the improvement in risk stratification and prognosis prediction of AML [2, 3]. For example, the presence of c-KIT mutations in patients with core-binding factor (CBF) in AML confers a higher risk of relapse [4, 5]. FLT3-ITD mutations are considered to confer a significantly poorer outcome in cytogenetically normal patents [6, 7]. Recently, a new category of genes involved in RNA splicing pathway has been found to be mutated in myeloid neoplasms, most frequently (44–85 %) in myelodysplastic syndrome (MDS), less frequent (26 %) in AML transformed from MDS, and rarely (6.6 %) in de novo AML [8].
SRSF2 (also known as SC35), a member of the splicing factors, belongs to the Ser/Arg-Rich (SR) protein family that plays a crucial role in the recognition of the 3′ splice site during RNA splicing pathway [9]. Hotspot mutations in the position codon 95 of SRSF2 gene have been found in patients with MDS, chronic monomyelocytic leukemia (CMML), primary myelofibrosis (PMF), and AML [8, 10–14]. SRSF2 mutation appears to predict adverse prognosis in MDS and PMF [12–15], while it is not associated with the survival of CMML patients [10, 11]. To date, little has been known about the clinical relevance and prognostic implications of SRSF2 mutations in de novo AML patients [8, 16]. In the current study, we analyzed the frequency of SRSF2 mutations and evaluated its clinical relevance in 249 Chinese AML patients.
Materials and methods
Patients and DNA extraction
Two hundred forty-nine patients with de novo AML were diagnosed according to the French–American–British (FAB) Cooperative Group Criteria and the World Health Organization (WHO) classification [17, 18]. Bone marrow samples were collected at the time of initial diagnosis after the informed consent was written. The bone marrow mononuclear cells (BMNCs) were isolated by density-gradient centrifugation using Ficoll, and subsequent genomic DNA extraction from BMNCs was performed according to the manufacturer’s instructions. This study was approved by the Ethics Committee Board of Affiliated People’s Hospital of Jiangsu University.
Primer design and PCR conditions
Primers for PCR were designed with LightScanner primer design software v1.0 (Idaho Technology, Salt Lake City, Utah) and as follows: 5′-TGCAAATGGCGCGCTAC-3′ (Forward); 5′-GGCGGCTGTGGTGTGAG-3′ (Reverse). PCR was carried out in 25-μl volume in the presence of 1× PCR buffer (Invitrogen, Merelbeke, Belgium), 0.2 mmol/l of each dNTP, 0.5 μmol/l of both forward and reverse primers, 0.8 μmol/l of internal oligonucleotide calibrators [19], 1 × LCgreen Plus (Idaho, Salt Lake City, Utah, USA), 0.75 U hot start DNA polymerase (Takara, Tokyo, Japan), and 50 ng genomic DNA. PCR reactions were performed on a 7300 Thermo cycler (Applied Biosystems, Foster City, CA, USA). The PCR conditions were as follows: 98 °C for 10 min, followed by 40 cycles of 98 °C for 10 s, 63 °C for 30 s, and 72 °C for 30 s, followed by a final 7 min extension step at 72 °C.
High resolution melting analysis
PCR products were transferred to the LightScanner (Idaho Technology Inc. Salt Lake City, Utah, USA) for high resolution melting analysis (HRMA). Plates were heated from 55 to 95 °C with a ramp rate of 0.10 °C/s. The melting curve analysis was carried out by the LightScanner software package with CALL-IT® software (Idaho Technology Inc., Salt Lake City, Utah, USA).
Other nine genes recurrent in AML, including C-KIT, CEBPa, NPM1, FLT3-ITD, RAS, IDH1/IDH2, DNMT3A, SF3B1, and U2AF1 mutations, were detected as reported previously [20–24].
DNA sequencing
To verify the results of HRMA, a separate PCR was carried out to generate a larger product (212 bp). Primers used as follows: 5′-TTCGCCTTCGTTCGCTTTCA-3′ (forward) and 5′-CCCCTCAGCCCCGTTTACC-3′ (reverse). PCR conditions were similar with that for HRMA except for the annealing temperature at 60 °C. PCR products were directly sequenced on both strands using an ABI 3730 automatic sequencer.
Statistics
Statistical analysis was performed using the SPSS 17.0 software package (SPSS, Chicago, IL, USA). The difference of discrete variables was compared by Pearson chi-square analysis or Fisher exact test. The difference of continuous variables was compared by Mann-Whitney’s U test. Survival was analyzed according to the Kaplan–Meier method. The individual impacts of prognostic factors on OS were estimated using Cox proportional hazards regression. For all analyses, the P values were two-tailed, and less than 0.05 was considered statistically significant.
Results
SRSF2 mutations in AML patients
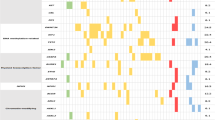
HRMA was performed to screen mutations in SRSF2. About 3.6 % (9/249) of cases were identified with heterozygous SRSF2 mutations in 249 AML patients (Table 1), which showed complex changes of melting curve shapes, compared to smooth and symmetric melting curves in other 240 wild-type SRSF2 patients (Fig. 1). The identical judgment was demonstrated by two blinded investigators. All HRMA results were further verified by direct sequencing which disclosed one heterozygous P95R (c.284C>G), two heterozygous P95L (c.284C>T), and six heterozygous P95H (c.284C>A) (Fig. 2). The clinical characteristics of SRSF2-mutated patients were shown in Table 2.
There was no difference in sex, blood parameters, WHO subtypes, and karyotype classification between cases with and without mutations (P > 0.05, Table 1). However, the patients with SRSF2 mutations were older than those with wild-type SRSF2 (P = 0.014). There was also no significance in SRSF2 mutation between cytogenetically normal (CN) AML (6/114, 5.20 %) and cytogenetically abnormal AML (3/119, 2.52 %) (P = 0.279).
To investigate the prognostic impact of SRSF2 mutation on AML, 173 cases with follow-up data were considered for survival analysis. Although the patients with SRSF2 mutation had the lower rate of complete remission (CR) after induction chemotherapy than those without SRSF2 mutation (28.57 vs. 50.88 %), the difference was not statistically significant (P = 0.249). The median overall survival (OS) of patients with SRSF2 mutations was 4 months (95 % confidence interval = 1.6–6.3 months), obviously shorter than those without SRSF2 mutations (median = 11 months, 95 % confidence interval = 7.4–14.6 months) (P = 0.006, Fig. 3a). Within patients with CN-AML, SRSF2-mutated cases also had a shorter OS than those without SRSF2 mutations (median = 2 vs. 12 months, P = 0.008, Fig. 3b). However, further multivariate analysis including SRSF2 mutation and other six prognostic factors selected by univariate analysis (P < 0.1) showed that significant impact of SRSF2 mutation on OS was lost (P = 0.119, Table 3).
Association of SRSF2 mutations with other mutations
The mutational data of other nine genes recurrent in AML were available (C-KIT, CEBPa, IDH1/IDH2, DNMT3A, NPM1, FLT3-ITD, RAS, SF3B1, and U2AF1) in this cohort of AML. Overall, 44.2 % (110/249) of cases carried at least one gene mutation. Among the nine patients with SRSF2 mutations, three patients simultaneously had the IDH2 mutation, NRAS mutation, and NPM1 mutation, respectively. No association was observed between SRSF2 mutations and other gene mutations (Table 1). It was noted that the most commonly mutated genes in RNA splicing (SF3B1, U2AF1, and SRSF2) were occurred in a mutually exclusive manner.
Discussion
Recurrent somatic mutations involved in RNA splicing machinery have been firstly reported in myelodysplasia by Yoshida et al. [8], suggesting that genetic alternations of the critical splicing components (mainly including SF3B1, U2AF1, and SRSF2 genes) could contribute to the pathogenesis of disease. Later, increasing studies investigated these mutations in MDS and other hematologic diseases. In the present study, we identified a very low frequency of SRSF2 mutations (3.6 %) in Chinese de novo AML patients. The low frequency was not caused by the methodology as the maximal sensitivity of HRMA could reach 10 % in a background of wild-type DNA, which was higher than those of direct DNA sequencing (25 %) and all HRMA results were further confirmed by direct DNA sequencing [25]. Besides, our result was in accordance with another two papers reported (0.7 and 5.6 %, respectively) [8, 16], implicating that SRSF2 mutation is a rare event in AML patients.
All SRSF2 mutations were heterozygous. In the previous studies, we have investigated the mutations in another two critical splicing factors SF3B1 and U2AF1 genes (1.1 and 2.5 %, respectively) [20, 21]. In total, 6.8 % (17/249) of AML patients harbored the three splicing genes mutations and we observed the same results in other studies that the three splicing factors mutated in mutually exclusive manner [8, 11, 14], suggesting that they might not affect RNA splicing and progression of disease cooperatively.
The presence of SRSF2 mutations was significantly correlated with older age in our AML cohorts, which was in accordance with the observations in CMML, PMF, and MDS [10, 13, 15]. However, no correlations in sex, blood parameters, FAB subtypes, and karyotype classification were noted between cases with and without mutations. The prognostic impact of SRSF2 mutations in MDS remains obscure: Makishima et al. reported that SRSF2 mutations had worse survival in low-risk MDS but not in the entire cohort of MDS patients [14]. Thol et al. reported that SRSF2 mutations were correlated with inferior survival and a higher rate of progression to AML [12]. Wu et al. proposed that SRSF2 mutation was associated with shorter OS but not an independent prognostic factor in MDS or in low-risk MDS and not associated with disease progression [15]. Our previous study also confirmed the adverse impact of SRSF2 mutation on survival in MDS [20]. In PMF, SRSF2 mutations predicted inferior OS and leukemia-free survival (LFS) [13]. Although Herold et al. identified SRSF2 mutations in 81 % of AML patients with isolated trisomy 13 (+13) [26], no case with +13 was found in our group. So far, no prognostic relevance has been found in AML. Our data revealed that the presence of SRSF2 mutations was significantly associated with worse OS according to univariate analysis; however, multivariate analysis did not disclose the association of SRSF2 mutation with prognosis. Clonal hematopoiesis with somatic mutations including SRSF2 mutation has been identified as an increasingly common event in aged people and is associated with increased risks of hematologic cancer [27–29]. Furthermore, a recent study has revealed that SRSF2 mutation contributes to myelodysplasia by altering SRSF2’s RNA binding activity and thereby altering the exon recognition to drive abnormal splicing of key hematopoietic regulators [30]. These results suggest that SRSF2 mutation is an early driver mutation involved in leukemogenesis but not a prognosis-associated event.
Previous studies have shown that in CMML SRSF2 mutations are frequently co-occurred with other mutations, such as TET2, IDH1/IDH2, RAS, RUNX1, and ASXL1 mutations whereas mutually exclusive with EZH2 mutation. Besides, patients with RUNX1 mutations overlapped with SRSF2 mutations have a favorable survival [10, 13–15]. Among the nine patients with SRSF2 mutations in our study, three patients simultaneously had IDH2 mutation, NRAS mutation, and NPM1 mutation, respectively. No significant association of SRSF2 mutation with them due to the low frequency in AML.
In summary, SRSF2 mutations are rarely mutated and associated with older age in Chinese AML patients. Furthermore, SRSF2 mutation might not be an independent prognostic event in AML.
References
Byrd JC, Mrózek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, et al. Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood. 2002;100:4325–36.
Marcucci G, Haferlach T, Döhner H. Molecular genetics of adult acute myeloid leukemia: prognostic and therapeutic implications. J Clin Oncol. 2011;29:475–86.
Mardis ER, Ding L, Dooling DJ, Larson DE, McLellan MD, Chen K, et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N Engl J Med. 2009;361:1058–66.
Nanri T, Matsuno N, Kawakita T, Suzushima H, Kawano F, Mitsuya H, et al. Mutations in the receptor tyrosine kinase pathway are associated with clinical outcome in patients with acute myeloblastic leukemia harboring t(8;21)(q22;q22). Leukemia. 2005;19:1361–6.
Schnittger S, Kohl TM, Haferlach T, Kern W, Hiddemann W, Spiekermann K, et al. KIT-D816 mutations in AML1-ETO-positive AML are associated with impaired event-free and overall survival. Blood. 2006;107:1791–9.
Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98:1752–9.
Thiede C, Steudel C, Mohr B, Schaich M, Schäkel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99:4326–35.
Yoshida K, Sanada M, Shiraishi Y, Nowak D, Nagata Y, Yamamoto R, et al. Frequent pathway mutations of splicing machinery in myelodysplasia. Nature. 2011;478:64–9.
Long JC, Caceres JF. The SR protein family of splicing factors: master regulators of gene expression. Biochem J. 2009;417:15–27.
Meggendorfer M, Roller A, Haferlach T, Eder C, Dicker F, Grossmann V, et al. SRSF2 mutations in 275 cases with chronic myelomonocytic leukemia (CMML). Blood. 2012;120:3080–8.
Patnaik MM, Lasho TL, Finke CM, Hanson CA, Hodnefield JM, Knudson RA, et al. Spliceosome mutations involving SRSF2, SF3B1, and U2AF35 in chronic myelomonocytic leukemia: prevalence, clinical correlates, and prognostic relevance. Am J Hematol. 2013;88:201–6.
Thol F, Kade S, Schlarmann C, Löffeld P, Morgan M, Krauter J, et al. Frequency and prognostic impact of mutations in SRSF2, U2AF1, and ZRSR2 in patients with myelodysplastic syndromes. Blood. 2012;119:3578–84.
Lasho TL, Jimma T, Finke CM, Patnaik M, Hanson CA, Ketterling RP, et al. SRSF2 mutations in primary myelofibrosis: significant clustering with IDH mutations and independent association with inferior overall and leukemia-free survival. Blood. 2012;120:4168–71.
Makishima H, Visconte V, Sakaguchi H, Jankowska AM, Abu Kar S, Jerez A, et al. Mutations in the spliceosome machinery, a novel and ubiquitous pathway in leukemogenesis. Blood. 2012;119:3203–10.
Wu SJ, Kuo YY, Hou HA, Li LY, Tseng MH, Huang CF, et al. The clinical implication of SRSF2 mutation in patients with myelodysplastic syndrome and its stability during disease evolution. Blood. 2012;120:3106–11.
Zhang SJ, Rampal R, Manshouri T, Patel J, Mensah N, Kayserian A, et al. Genetic analysis of patients with leukemic transformation of myeloproliferative neoplasms shows recurrent SRSF2 mutations that are associated with adverse outcome. Blood. 2012;119:4480–5.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al., editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: IARC; 2008.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposed revised criteria for the classification of acute myeloid leukaemia. A report of the French–American–British Cooperative Group. Ann Intern Med. 1985;103:620–5.
Qian J, Lin J, Yao DM, Chen Q, Xiao GF, Ji RB, et al. Rapid detection of JAK2 V617F mutation using high-resolution melting analysis with LightScanner platform. Clin Chim Acta. 2010;411:2097–100.
Yang J, Qian J, Yao DM, Qian SX, Qian W, Lin J, et al. SF3B1 mutation is a rare event in Chinese patients with acute and chronic myeloid leukemia. Clin Biochem. 2013;46:701–3.
Qian J, Yao DM, Lin J, Qian W, Wang CZ, Chai HY, et al. U2AF1 mutations in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. PLoS One. 2012;7:e45760.
Lin J, Yao DM, Qian J, Chen Q, Qian W, Li Y, et al. IDH1 and IDH2 mutation analysis in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. Ann Hematol. 2012;91:519–25.
Lin J, Yao DM, Qian J, Chen Q, Qian W, Li Y, et al. Recurrent DNMT3A R882 mutations in Chinese patients with acute myeloid leukemia and myelodysplastic syndrome. PLoS One. 2011;6:e26906.
Szankasi P, Jama M, Bahler DW. A new DNA-based test for detection of nucleophosmin exon 12 mutations by capillary electropheresis. J Mol Diagn. 2008;10:236–41.
Lin J, Yang J, Wen XM, Yang L, Deng ZQ, Qian Z, et al. Detection of SRSF2-P95 mutation by high-resolution melting curve analysis and its effect on prognosis in myelodysplastic syndrome. PLoS One. 2014;9:e115693.
Herold T, Metzeler KH, Vosberg S, Hartmann L, Röllig C, Stölzel F, et al. Isolated trisomy 13 defines a genetically homogenous AML subgroup with high frequency of mutations in spliceosome genes and poor prognosis. Blood. 2014;124:1304–11.
Genovese G, Kähler AK, Handsaker RE, Lindberg J, Rose SA, Bakhoum SF, et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N Engl J Med. 2014;371:2477–87.
Jaiswal S, Fontanillas P, Flannick J, Manning A, Grauman PV, Mar BG, et al. Age-related clonal hematopoiesis associated with adverse outcomes. N Engl J Med. 2014;371:2488–98.
McKerrell T, Park N, Moreno T, Grove CS, Ponstingl H, Stephens J, et al. Leukemia-associated somatic mutations drive distinct patterns of age-related clonal hemopoiesis. Cell Rep. 2015;10:1239–45.
Kim E, Ilagan JO, Liang Y, Daubner GM, Lee SC, Ramakrishnan A, et al. SRSF2 mutations contribute to myelodysplasia by mutant-specific effects on exon recognition. Cancer Cell. 2015;27:617–30.
Acknowledgments
This study was supported by National Natural Science foundation of China (81172592, 81270630), Six major talent summit project in Jiangsu Province (WSN-112), Science and Technology Special Project in Clinical Medicine of Jiangsu Province (BL2012056), 333 Project of Jiangsu Province (BRA2013136), Science and Technology Infrastructure Program of Zhenjiang (SS2012003), Medical Key Talent Project of Zhenjiang, and Social Development Foundation of Zhenjiang (SH2013042, SH2014044, SH2014086).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Yang, J., Yao, Dm., Ma, Jc. et al. The prognostic implication of SRSF2 mutations in Chinese patients with acute myeloid leukemia. Tumor Biol. 37, 10107–10114 (2016). https://doi.org/10.1007/s13277-015-4716-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4716-0