Abstract
Multidrug resistance 1 (MDR1) gene encodes P-glycoprotein (P-gp), which acts as an efflux pump and provides cell protection against various substances, and its single-nucleotide polymorphisms (SNPs) are associated with the development of malignant hematologic diseases. The present study aimed at investigating whether the MDR1 SNPs and haplotype variants were correlated with the susceptibility to multiple myeloma (MM). A total of 115 MM patients and 153 healthy controls from Jiangsu Han population were enrolled and genotyped by polymerase chain reaction–allele-specific primer (PCR-ASP) method or DNA direct sequencing at MDR1 loci of C1236T, G2677T/A, and C3435T. No significance was found in the distribution of alleles and genotypes in MDR1 three loci. Diplotype analysis has also demonstrated no effect in susceptibility to MM. But, in haplotype analysis, the haplotype of T–G–T was significantly more common than healthy controls (12.6 % in MM group vs. 1.7 % in control group, odds ratios (ORs) = 8.7, 95 % confidence interval (CI) 3.3–22.8, Pc < 0.01). Our results pointed out that comparable allele, genotype, and diplotype frequencies among MM patients and controls in Chinese Jiangsu Han population were found; the frequency of T–G–T haplotype was significantly increased in MM group compared with the control group, which indicated that this haplotype might be associated with the susceptibility to MM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multidrug resistance 1 (MDR1) gene is a member of the adenosine triphosphate (ATP)-binding cassette (ABC) superfamily, and it encodes a 170-kDa membrane transporter named P-glycoprotein (P-gp), which acts as an efflux pump and provides cell protection against various substances, such as drugs and toxins, reducing the intercellular concentrations of different chemotherapeutic agents [1, 2]. It has been demonstrated that single-nucleotide polymorphisms (SNPs) in MDR1 gene, such as C1236T (exon 12, rs1128503), G2677T/A (exon 21, rs2032582), and C3435T (exon 26, rs1045642), affect MDR1 protein expression and function, which might be a protective or a risk factor in the development of many tumors, including hematologic malignant diseases [3–8].
Multiple myeloma (MM) is the second most common hematological malignancy and is characterized by accumulation of clonal plasma B cells in bone marrow, hypercalcemia, renal failure, anemia, and lytic bone lesions. The molecular pathogenesis of MM was still not clear, and lots of studies suggest that genetic component might play an important role in the etiology of MM [9]. As MDR1 polymorphisms might be different in different ethnic and geographic populations for their unique genetic background, the possibility of an association of MDR1 polymorphisms, at the three common loci C1236T (exon 12, rs1128503), G2677T/A (exon 21, rs2032582), and C3435T (exon 26, rs1045642), was assessed in a total of 115 MM patients residing in Jiangsu Province, People’s Republic of China.
Materials and methods
Subjects
In total, 115 cases of patients, Han ethnic, diagnosed with MM [10] were enrolled for MDR1 association study. They consisted of 70 (60.9 %) males and 45 (39.1 %) females, with the median age of 68 years (range = 35–82 years). These patients were selected from Jiangsu population, and the details of their clinical characteristics are summarized in Table 1. DNA samples were also collected from 153 healthy volunteers as a control group from the same ethnic and geographical background in Jiangsu province. The informed written consents were obtained from each patient and control before blood collection, and this study was strictly adhered to the principles of the Helsinki Declaration.
Genotyping
Three interested SNPs in MDR1 gene, including C1236T (rs1128503), G2677T/A (rs2032582), and C3435T (rs1045642), were genotyped by polymerase chain reaction–allele-specific primer (PCR-ASP) method and DNA direct sequencing for both patients and controls. Genomic DNA was isolated from peripheral blood in the light of the protocol provided by the manufacturer using salting-out method (Lot# N3113, Tiangen Company, Beijing, China) and then was stored at −70 °C before touchdown PCR-ASP program was initiated. PCR reactions were performed in the volume of 20-μl PCR mixture, composed of 10 μl PCR Master Mix reaction buffer (Lot# KT201-02, Tiangen Company, Beijing, China), 1 μl of each specific PCR primer, 1 μl Taq DNA polymerase, 1 μl genomic DNA template, and 7 μl ddH2O. After the amplification was completed, PCR products were subjected to undergo electrophoresis on agarose gel with ethidium bromide (EB). MDR1 genotypes in loci of C1236T (rs1128503) and C3435T (rs1045642) were identified by photographed picture of the EB-stained gel. PCR primers and reaction conditions were referenced in our previous literature [11]. Due to the genotype complexity of locus G2677T/A (rs2032582), DNA direct sequencing technique was employed to make out the genotype.
Statistical analysis
Frequencies of allele, genotype, and diplotype were calculated directly, and the maximum likelihood haplotype frequencies were computed by the expectation–maximization (EM) algorithm using Arlequin software 3.01 [12], as well as the Hardy–Weinberg equilibrium test. Chi-squared test was employed to examine the statistical significance in the distributions of allele, genotype, diplotype, and haplotype between MM patients and controls, evaluated by odds ratios (ORs) with 95 % confidence interval (CI). Fisher’s exact test was also used to evaluate the differences in MDR1 SNPs when cells having expected count less than 1 were existed. Bonferroni inequality method [13] was employed to correct the original P value (Pc) to overcome the error when one of the alleles, genotypes, diplotypes, or haplotypes could have deviated significantly by chance. All statistical tests were two sided, and a p value of <0.05 was defined as the criterion of statistical significance.
Results
Hardy–Weinberg equilibrium examination
Distributions of the interested MDR1 SNPs, C1236T at rs1128503, G2677T/A at rs2032582, and C3435T at rs1045642, were tested in Hardy–Weinberg formula, and the results indicated that they were in Hardy–Weinberg equilibrium (p > 0.05) (Table 2).
Distributions of alleles and genotypes
The allelic and genotypic frequency distributions of three common SNPs (C1236T, G2677T/A, and C3435T) in MDR1 gene between MM patients and healthy controls were analyzed and are presented in Table 3. The frequencies of each allelic variant did not show any statistical difference between MM group and control group. At locus G2677T/A, the G allele was detected relatively less frequent in MM patient cohorts than in control group (37.0 % in MM group vs. 43.5 % in control group, OR = 0.8, 95 % CI 0.5–1.1, P = 0.13), but the difference was not significant. In genotype analysis, the frequency of GG genotype at locus G2677T/A was decreased in MM group (12.2 % in MM group vs. 19.6 % in control group, OR = 0.6, 95 % CI 0.3–1.1, p = 0.11). There was also no significance in the distributions of three loci genotypes between MM patients and controls.
Diplotype association study
The distribution of diplotypes at the position of C1236T, G2677T/A, and C3435T was compared in MM patients and controls. Some common diplotypes (top seven in the rank of MM group) were demonstrated from all the diplotypes at any two of three loci. The most common diplotype was 2677GT/3435CT with a frequency of 28.7 %, followed by 1236TT/3435CT with a frequency of 23.5 % and 1236TT/2677GT with a frequency of 16.3 % in MM patients, while the most common diplotypes were 2677GT/3435CT (28.1 %), 1236CT/3435CT (22.9 %), and 1236TT/2677GT (21.6 %) in the control group (Table 4). No significance was found in the distribution of these diplotypes between MM patients and controls.
Haplotype association study
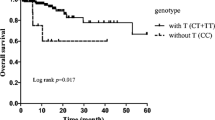
The distribution of all haplotypes computed by the EM algorithm is demonstrated in Table 5. When the three loci haplotype of 1236–2677–3435 were investigated, the most frequently observed haplotype was T–T–T in MM group with a frequency of 36.5 %, followed by T–G–C (28.7 %) and C–G–C (15.2 %). The T–G–C of 1236–2677–3435 showed an increased frequency in MM group compared with the control group, but the difference was not significant (p = 0.058). However, the haplotype of T–G–T was significantly more common than healthy controls (12.6 % in MM group vs. 1.7 % in control group, OR = 8.7, 95 % CI 3.3–22.8, Pc < 0.01). In MM group, the most common haplotype for two loci was T–T with a frequency of 44.9 % in 1236–2677, followed by T–T with a frequency of 39.2 % in 2677–3435, and T–T with a frequency of 37.7 % in 1236–3435. A comparison of two loci haplotype frequencies at 1236–2677, 2677–3435, and 1236–3435 revealed that no significant difference existed between MM patients and controls.
Discussion
Due to the fundamental role of transporting the cells’ endogenous and exogenous harmful compounds outside to protect the cells, increasing evidences have suggested that MDR1 SNPs are associated with cancer development, which might alter the MDR1 expression and protein conformation [14–17]. MDR1 SNPs may also influence the risk of malignant hematologic diseases, such as leukemia, lymphoma, and MM [16–18]. In our previous studies, MDR1 correlations with chronic lymphocytic leukemia (CLL), chronic myeloid leukemia (CML), and diffuse large B cell lymphoma (DLBCL), as well as the prognostic value and drug resistance, have been explored and some risk or protective factors were revealed [7, 8, 19, 20]. Based on the association study of MDR1 SNPs with MM was limited [21, 22] and the genetic background may alter the final associations, we focused on whether potentially functional polymorphisms in MDR1 gene responsible for protection of the organisms against environmental carcinogens have an impact on the susceptibility to MM.
The alleles, genotypes, haplotypes, and diplotypes in MDR1 three common positions, C1236T, G2677T/A, and C3435T, were focused on and compared in MM and control groups in this study. No significant allele or genotype was found in the distribution of three common MDR1 loci between MM patients and controls. Jamroziak et al. [23] have also investigated whether three common MDR1 SNPs (C1236T, G2677T/A, and C3435T) affect predisposition to MM in 111 Caucasians, and they found comparable allele and genotype frequencies among MM patients and controls, which was in accordance with our results. In a CML association study [16], the 1236TT genotype was significantly associated with the susceptibility to CML when compared to the wild-type 1236CC (OR = 2.7, p = 0.04). In non-Hodgkin lymphoma (NHL), 1236CC genotype was associated with a decreased risk for NHL (OR = 0.74, p = 0.04) [6]. We have also focused on the associations of MDR1 SNPs with DLBCL and found that allele G and genotype GT at locus G2677T/A were significantly more common in DLBCL (G: OR = 1.5, p = 0.03; GT: OR = 2.0, p < 0.01), while genotype AT seemed to be protective (OR = 0.3, p = 0.03) at this locus; TT genotype at locus C3435T showed a risk factor in DLBCL (OR = 2.4, p < 0.01) [20]. This discrepancy might be due to various factors, including the different ethnicity of the two populations, different environmental risk factors, different molecular pathogenesis in different tumors, or the difference in the sample size of the studies.
The distribution of diplotypes was similar between MM patients and controls. But, in haplotype association study, haplotype of T–G–T was significantly increased in MM group compared with the control group (12.6 % in MM group vs. 1.7 % in control group, Pc < 0.01). In a similar study, comparable genotype and haplotype frequencies among MM patients and controls were observed in Caucasians [23]. In a CML study, the frequency of T–G–T in CML group was higher than the control group (6.86 % in CML group vs. 2.46 % in control, p = 0.11) [16], indicating a potential trend in CML patients, which was in agreement with our findings.
It is generally accepted that inherited variation in MDR1 involved in the transport and metabolism of environmental toxins in different genetic background and the tumor originations might determine the likelihood of malignant development [24]. A large meta-analysis of 39 independent studies conducted in relation with MDR1 SNPs and cancer risk found an association between the 3435T allele and overall cancer risk (OR = 1.18, 95 % CI 1.04–1-34) [25]. However, MDR1 mechanism associated with cancers or treatment response is surprisingly complex and poorly understood. It has been suggested that impaired MDR1 expression and protein conformation can result in several cancer types or treatment response [6, 26–28]. For instance, Bellusci et al. [26] have reported that the MDR1 C1236T SNP significantly reduces lopinavir plasma concentration affecting the virological response to treatment. Several other reports suggested that these significant associations might be due to linkage disequilibrium with the MDR1 SNPs [29], allele-specific differences in mRNA folding [30], or numerous environmental factors [31].
In conclusion, our results pointed out that there was no significant allele, genotype, and diplotype in the distribution of three common MDR1 loci between MM patients and controls in Chinese Jiangsu Han population. In haplotype analysis, the frequency of T–G–T haplotype was significantly increased in MM group compared with the control group, which indicated that this haplotype might be associated with the predisposition to MM. Further studies should be performed to explore the disease associations and establish the detailed molecular mechanisms, by which the MDR1 SNPs modify the susceptibility to MM.
References
Sauna ZE, Kim IW, Ambudkar SV. Genomics and the mechanism of P-glycoprotein (ABCB1). J Bioenerg Biomembr. 2007;39:481–7.
Bodor M, Kelly EJ, Ho RJ. Characterization of the human MDR1gene. AAPS J. 2005;7(1):E1–5.
Vine J, Cohen SB, Ruchlemer R, Goldschmidt N, Levin M, Libster D, et al. Polymorphisms in the human organic cation transporter and the multidrug resistance gene: correlation with imatinib levels and clinical course in patients with chronic myeloid leukemia. Leuk Lymphoma. 2014;55:2525–31.
Yue Q, Xiong B, Chen L, Chen Y, Bu F, Liu X, et al. MDR1 C3435T polymorphism and childhood acute lymphoblastic leukemia susceptibility: an updated meta-analysis. Biomed Pharmacother. 2015;69:76–81.
Ma L, Liu H, Ruan L, Yang X, Yang H, Feng Y. Multidrug resistance gene 1 C1236T polymorphism and susceptibility to leukemia: a meta-analysis. Biomed Rep. 2015;3:83–7.
Kim HN, Kim NY, Yu L, Kim YK, Lee IK, Yang DH, et al. Polymorphisms in DNA repair genes and MDR1 and the risk for non-Hodgkin lymphoma. Int J Mol Sci. 2014;15:6703–16.
Ni Y, Xiao Z, Yin G, Fan L, Wang L, Zhu H, et al. The single nucleotide polymorphism and haplotype analysis of MDR1 in Chinese diffuse large B cell lymphoma patients. Biomed Pharmacother. 2015;73:24–8.
Dong HJ, Miao KR, Qiao C, Zhuang Y, Shen WY, Hong M, et al. Polymorphisms and haplotypes in multidrug resistance 1 gene are not associated with chronic lymphocytic leukemia susceptibility and prognostic parameters of chronic lymphocytic leukemia in Chinese population. Leuk Lymphoma. 2011;52:1003–9.
Amend SR, Wilson WC, Chu L, Lu L, Liu P, Serie D, et al. Whole genome sequence of multiple myeloma-prone C57BL/KaLwRij mouse strain suggests the origin of disease involves multiple cell types. PLoS One. 2015;10(5):e0127828.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumors of haematopoietic and lymphoid tissues. Lyon: WHO; 2008.
Qiu H, Dong H, Pan S, Miao K. The single nucleotide polymorphism and haplotype analysis of MDR1 in Jiangsu Han population of China. Biomed Pharmacother. 2012;66:459–63.
Excoffier L, Laval G, Schneider S. Arlequin (version 3.0): an integrated software package for population genetics data analysis. Evol Bioinformatics Online. 2005;1:47–50.
Oj D. Multiple comparisons among means. J Am Stat Assoc. 1961;56:52–6.
Gutierrez-Rubio SA, Quintero-Ramos A, Duran-Cardenas A, Franco-Topete RA, Castro-Cervantes JM, Oceguera-Villanueva A, et al. 1236 C/T and 3435 C/T polymorphisms of the ABCB1 gene in Mexican breast cancer patients. Genet Mol Res. 2015;14:1250–9.
Pongstaporn W, Pakakasama S, Chaksangchaichote P, Pongtheerat T, Hongeng S, Permitr S. MDR1 C3435T and C1236T polymorphisms: association with high-risk childhood acute lymphoblastic leukemia. Asian Pac J Cancer Prev. 2015;16:2839–43.
Yaya K, Hind D, Meryem Q, Asma Q, Said B, Sellama N. Single nucleotide polymorphisms of multidrug resistance gene 1 (MDR1) and risk of chronic myeloid leukemia. Tumour Biol. 2014;35:10969–75.
Mhaidat NM, Alshogran OY, Khabour OF, Alzoubi KH. MatalkaII, Haddadin WJ, et al. Multi-drug resistance 1 genetic polymorphism and prediction of chemotherapy response in Hodgkin’s lymphoma. J Exp Clin Cancer Res. 2011;30:68.
Drain S, Catherwood MA, Orr N, Galligan L, Rea IM, Hodkinson C, et al. ABCB1 (MDR1) rs1045642 is associated with increased overall survival in plasma cell myeloma. Leuk Lymphoma. 2009;50:566–70.
Ni Y, Yin G, Xiao Z, Fan L, Wang L, Wu Y, et al. MDR1 polymorphisms have an impact on the prognosis of Chinese diffuse large B cell lymphoma patients. Tumour Biol. 2015 Aug 19.
Ni LN, Li JY, Miao KR, Qiao C, Zhang SJ, Qiu HR, et al. Multidrug resistance gene (MDR1) polymorphisms correlate with imatinib response in chronic myeloid leukemia. Med Oncol. 2011;28(1):265–9.
Buda G, Ricci D, Huang CC, Favis R, Cohen N, Zhuang SH, et al. Polymorphisms in the multiple drug resistance protein 1 and in P-glycoprotein 1 are associated with time to event outcomes in patients with advanced multiple myeloma treated with bortezomib and pegylated liposomal doxorubicin. Ann Hematol. 2010;89(11):1133–40.
Maggini V, Buda G, Martino A, Presciuttini S, Galimberti S, Orciuolo E, et al. MDR1 diplotypes as prognostic markers in multiple myeloma. Pharmacogenet Genomics. 2008;18(5):383–9.
Jamroziak K, Balcerczak E, Calka K, Piaskowski S, Urbanska-Rys H, Salagacka A, et al. Polymorphisms and haplotypes in the multidrug resistance 1 gene (MDR1/ABCB1) and risk of multiple myeloma. Leuk Res. 2009;33(2):332–5.
Lardo M, Castro M, Moiraghi B, Rojas F, Borda N, Rey JA, et al. MDR1/ABCB1 gene polymorphisms in patients with chronic myeloid leukemia. Blood Res. 2015;50(3):154–9.
Sheng X, Zhang L, Tong N, Luo D, Wang M, Xu M, et al. MDR1 C3435T polymorphism and cancer risk: a meta-analysis based on 39 case–control studies. Mol Biol Rep. 2012;39:7237–49.
Bellusci CP, Rocco C, Aulicino P, Mecikovsky D, Curras V, Hegoburu S, et al. Influence of MDR1 C1236T polymorphism on lopinavir plasma concentration and virological response in HIV-1-infected children. Gene. 2013;522(1):96–101.
Wang D, Sadee W. Searching for polymorphisms that affect gene expression and mRNA processing: example ABCB1 (MDR1). AAPS J. 2006;8:E515–20.
Nakamura T, Sakaeda T, Horinouchi M, Tamura T, Aoyama N, Shirakawa T, et al. Effect of the mutation (C3435T) at exon 26 of the MDR1 gene on expression level of MDR1 messenger ribonucleic acid in duodenal enterocytes of healthy Japanese subjects. Clin Pharmacol Ther. 2002;71:297–303.
Tang K, Ngoi SM, Gwee PC, Chua JM, Lee EJ, Chong SS, et al. Distinct haplotype profiles and strong linkage disequilibrium at the MDR1 multidrug transporter gene locus in three ethnic Asian populations. Pharmacogenetics. 2002;12:437–50.
Shen LX, Basilion JP, Stanton Jr VP. Single-nucleotide polymorphisms can cause different structural folds of mRNA. Proc Natl Acad Sci U S A. 1999;96:7871–6.
Perloff MD, von Moltke LL, Störmer E, Shader RI, Greenblatt DJ. Saint John’s wort: an in vitro analysis of P-glycoprotein induction due to extended exposure. Br J Pharmacol. 2001;134:1601–8.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (81470329, 81302040, 81372540), National Public Health Grand Research Foundation (No. 201202017), Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institute (No. JX10231801), Project of National Key Clinical Specialty, National Science & Technology Pillar Program (No. 2014BAI09B12), and Project Funded by Jiangsu Provincial Special Program of Medical Science (No. BL2014086).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Guangli Yin and Zhengrui Xiao contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yin, G., Xiao, Z., Ni, Y. et al. Association of MDR1 single-nucleotide polymorphisms and haplotype variants with multiple myeloma in Chinese Jiangsu Han population. Tumor Biol. 37, 9549–9554 (2016). https://doi.org/10.1007/s13277-015-4574-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4574-9