Abstract
P-glycoprotein (Pgp) is a 170-kDa transmembrane protein that mediates the efflux of anticancer drugs from cells. Pgp overexpression has a distinct role in cells exhibiting multidrug resistance (MDR). We examined reversal of drug resistance in human MDR breast cancer cells by inhibition of protein kinase Cα (PKCα) activity, which is associated with Pgp-mediated efflux of anticancer drugs. PKCα activity was confirmed by measurement of phosphorylation levels of a PKCα-specific peptide substrate (FKKQGSFAKKK-NH2), showing relatively higher basal activity in drug-resistant MCF-7/ADR cells (84 %) than that in drug-sensitive MCF-7 cells (63 %). PKCα activity was effectively suppressed by the PKC inhibitor, Ro-31-7549, and reversal of intracellular accumulation of doxorubicin was observed by inhibition of PKCα activity in MCF-7/ADR cells compared with their intrinsic drug resistance. Importantly, increased accumulation of doxorubicin could enhance the therapeutic efficacy of doxorubicin in MDR cells significantly. These results suggest a potential for overcoming MDR via inhibition of PKCα activity with conventional anticancer drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multidrug resistance (MDR) of cancer cells is a major factor limiting the effectiveness of cancer chemotherapy. A widely studied mechanism of MDR is associated with overexpression of the adenosine triphosphate-binding cassette (ABC) transporter superfamily, which results in increased efflux of chemotherapeutic agents from cells. Among 48 human ABC transporters, a well-characterized P-glycoprotein (Pgp) is highly implicated with reduction of intracellular levels of anticancer drugs below their therapeutic threshold and a consequent decrease in their toxic effects [1–5].
A significant contribution of Pgp to the efflux of endogenous and exogenous molecules, which leads to drug resistance, provides an alternative rationale for the development of targeted therapies against this membrane transporter [6]. Direct inhibitors and modulators of Pgp were identified first in the 1980s, but three generations of Pgp inhibitors have been investigated extensively as a strategy for MDR reversal. However, concerns remain over safety and pharmacokinetic changes of therapeutic drugs in clinical trials [7]. Thus, strategies have been employed to overcome MDR using new chemotherapeutic agents designed as analogs of therapeutic compounds [8, 9], prodrugs [10, 11], Pgp-specific therapeutic antibodies [12], and nanoparticle-based drug delivery systems [13, 14]. These diverse strategies are emerging as promising candidates for the effective treatment of cancer, but the toxicology of long-term exposure to drugs or nanomaterials in humans needs to be studied and evaluated fully [15–17].
Alternatively, Pgp activity can be regulated by protein phosphorylation, particularly if induced by activated protein kinase C (PKC) isoforms; Pgp overexpression has been implicated to have a prominent role in MDR cells in humans [18–20]. Several reports of drug accumulation in human MDR cells have suggested increased activities/levels of PKC isoforms, mainly for PKCα, which phosphorylates the specific serine residues in the linker region of Pgp, thereby activating Pgp to increase ATPase activity and drug efflux [21–24]. It has also been shown that regulation of drug resistance with a PKC inhibitor which inhibits various PKC isoforms non-specifically leads to decreased phosphorylation of Pgp and drug efflux, suggesting the possibility of altered drug resistance in MDR cells [25]. Furthermore, PKCα activity has been proposed to be related to cancer stem cells, which have unique features such as self-renewal, differentiation, and chemoresistance to conventional therapeutic agents. In particular, recent studies have demonstrated that an intrinsic mechanism of resistance of cancer stem cells to chemotherapeutic drugs is acquired through high expression of ABC transporters [26–28]. Therefore, targeting ABC transporters such as Pgp through regulation of PKCα activity could help to reverse MDR, resulting in better anticancer strategies.
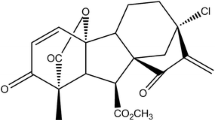
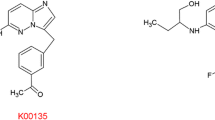
Here, we investigated if Pgp-mediated drug resistance was modulated by inhibition of PKCα activity in human MDR breast cancer cells, in which a PKC inhibitor was used in combination with an anticancer drug to overcome MDR. To assess levels of PKCα activity, a PKCα-specific peptide substrate (Alphatomega; FKKQGSFAKKK-NH2), which we have shown previously to have high specificity towards PKCα [29, 30], was used to compare phosphorylation levels in drug-sensitive MCF-7 cells with those in drug-resistant MCF-7/ADR cells. PKCα activity was modulated by the PKC inhibitor Ro-31-7549, which has highly specific inhibitory effects towards PKCα [30–32]. Inhibition of PKCα activity resulted in increased accumulation of anticancer drug and enhancement of its toxicity in resistant cells (Fig. 1). These observations provided evidence that Pgp phosphorylation induced by activated PKCα has a prominent role in the regulation of drug efflux.
Materials and methods
Cell culture
MCF-7 cells were cultured in modified Eagle medium containing 0.1 mM non-essential amino acids, 1 mM sodium pyruvate, and 10 μg/mL insulin. MCF-7/ADR cells were kindly provided by Dr. Ick Chan Kwon (Center for Theragnosis, Korea Institute of Science and Technology, Seoul, Korea) and cultured in RPMI 1640 medium. All medium contained 10 % fetal bovine serum (FBS), 100 U/mL penicillin, 100 μg/mL streptomycin, and 0.25 μg/mL amphotericin B (all from Gibco Invitrogen, Grand Island, NY, USA). Cells were harvested in a humidified atmosphere of 5 % CO2 and 95 % air at 37 °C.
Cytotoxicity of doxorubicin (Dox) and PKC inhibitor (Ro-31-7549)
Cells (2 × 103) were seeded into 96-well plates and cultured for 24 h at 37 °C in a 5 % CO2. The medium in each well was replaced with 100 μL of fresh medium containing a different concentration of doxorubicin hydrochloride (0–100 nM; Wako Pure Chemicals, Osaka, Japan) and the PKC inhibitor Ro-31-7549 (0–50 μM; Merck Millipore, Billerica, MA, USA). After incubation for 24 or 72 h, the medium was replaced with 100 μL of fresh medium. Then, 10 μL of 4-[3-(2-methoxy-4-nitrophenyl)-2-(4-nitrophenyl)-2H-5-tetrazolio]-1,3-benzene disulfonate sodium salt (WST-8; Dojindo Laboratories, Kumamoto, Japan) was added to each well. Cells were incubated for a further 2 h. Cell viability (%) was calculated by comparing the absorbance of treated cells to that of untreated control cells at 440 nm. This assay was conducted in triplicate.
Phosphorylation assay of the PKCα-responsive peptide substrate
MCF-7 and MCF-7/ADR cells were plated at 1 × 106 in 100-mm dishes or 2 × 105 in six-well plates at 37 °C in 2 mL medium containing 10 % FBS. At ∼70–80 % confluence, cells were stimulated with doxorubicin (0.01–10 nM) and Ro-31-7549 (0.05–100 μM) for 6 h, and then scraped in 1 mL buffer [10 mM HEPES, 10 % sucrose, Complete™ protease inhibitor cocktail (EDTA-free; Roche, Basel, Switzerland)]. Samples were centrifuged at 5000×g for 10 min at 4 °C and the supernatant was removed. Then, 0.1 mL of buffer was added to the precipitate and sonicated twice in ice for 15 s. Samples were centrifuged again at 5000×g for 15 min at 4 °C, and the resulting supernatant used for phosphorylation of the PKCα-specific peptide substrate (prepared by standard Fmoc-chemistry) [30]. Total protein concentration of cell lysates was measured using Protein Assay Dye reagent (Bio-Rad, Hercules, CA, USA) with bovine serum albumin as the standard. Phosphorylation of the peptide substrate responding to PKCα in MCF-7 and MCF-7/ADR cell lines was carried out in 100 μL buffer [10 mM HEPES, 10 mM MgCl2, 0.5 mM CaCl2, 2.0 μg/mL diacylglycerol, 2.5 μg/mL phosphatidylserine, and 200 μM adenosine triphosphate] containing 30 μM peptide substrate and cell lysates at protein concentrations of 100 or 200 μg/mL. Phosphorylation was allowed to proceed for 1 h at 37 °C. Resulting solutions were analyzed by matrix-assisted laser desorption/ionization–time of flight–mass spectrometry (MALDI-TOF-MS). Half-maximal inhibitory concentration (IC50) values were obtained using Prism (GraphPad, Avenida, CA, USA).
Confocal laser scanning microscopy
MCF-7 and MCF-7/ADR cells were plated at 1 × 105 in 35-mm glass-bottom dishes (Matsunami, Osaka, Japan) at 37 °C in 1 mL medium containing 10 % FBS for 24 h. Dishes were washed with phosphate-buffered saline (PBS) and incubated with or without 5 μM Ro-31-7549 for 30 min; cells incubated further with 100 μM doxorubicin for 2 h. Intracellular localization and accumulation of doxorubicin were observed by confocal laser scanning microscopy (CLSM, LSM 700; Carl Zeiss, Oberlochen, Germany) equipped with an EC Plan-Neofluar ×20/0.50 M27 objective lens.
Cellular accumulation of doxorubicin
MCF-7 and MCF-7/ADR cells were plated at 5 × 104 in 24-well plates at 37 °C in medium containing 10 % FBS for 24 h. The medium in each well was washed with PBS and replaced with Opti-MEM (Gibco), and then incubated with or without 50 μM Ro-31-7549 and doxorubicin, (0, 0.1, 1, or 10 nM) for 6 h. Estimation of cellular uptake was conducted by a Tali™ Image-based Cytometer (Invitrogen, Carlsbad, CA, USA).
Statistical analysis
Results are the mean ± S.D. from at least three independent experiments. Differences were determined with the Student’s t test. P < 0.05 was considered significant.
Results and discussion
Resistance to doxorubicin in human breast cancer cells
To investigate resistance to the therapeutic drug doxorubicin in drug-sensitive MCF-7 and resistant MCF-7/ADR cells (which are well-characterized human breast cancer cell lines for multidrug resistance [33, 34]), we first compared cell viability using the WST-8 assay in the presence of various concentrations of doxorubicin (Fig. 2a). Both cell types were exposed to increasing concentrations of doxorubicin (0.01–100 nM) for 72 h. As expected, MCF-7 cells had high sensitivity to doxorubicin (IC50 < 0.1 nM), whereas MCF-7/ADR cells showed ∼100-times higher resistance to doxorubicin than MCF-7 cells (IC50 > 10 nM). Then we examined the toxicity of the PKCα inhibitor Ro-31-7549 on both cell lines. Toxicity of Ro-31-7549 on these cell lines was weak and almost identical (Fig. 2b).
Effect of a PKCα inhibitor on drug-sensitive and drug-resistant cell lines
PKCα activity was estimated from phosphorylation levels of a PKCα-specific peptide substrate (FKKQGSFAKKK-NH2) with MCF-7 and MCF-7/ADR cell lysates at a protein concentration of 200 μg/mL. We have established this method to be a simple and rapid quantification method with MALDI-TOF-MS analyses [29]. Basal activity of PKCα in MCF-7/ADR was higher than MCF-7 (Ro-31-7549 = 0 μM, Fig. 3), a finding that was in accordance with previous reports [35, 36]. Addition of Ro-31-7549 led to a gradual decrease in the phosphorylation level of MCF-7 and MCF-7/ADR cells. IC50 values of Ro-31-7549 were 0.76 μM for MCF-7 and 15 μM for MCF-7/ADR cells, respectively. The higher IC50 value in MCF-7/ADR cells reflected (again) the higher activity of PKCα in this cell line.
Inhibition of PKCα activity by addition of an inhibitor of protein kinase (Ro-31-7549). After 6 h incubation with Ro-31-7549, cells were scraped and sonicated at 4 °C. Samples were then centrifuged and the supernatant used as cell lysates. Phosphorylation of the PKCα-specific peptide substrate with cell lysates at a protein concentration of 200 μg/mL was undertaken at 37 °C for 1 h and analyzed by MALDI-TOF-MS (n = 3)
Effects of doxorubicin on PKCα activity and its inhibition by Ro-31-7549
To investigate the effect of doxorubicin on PKCα activity, a phosphorylation assay was carried out in MCF-7 and MCF-7/ADR cells after exposure to different concentrations of doxorubicin for a short period (6 h), in which the toxicity in both cell lines is negligible. MCF-7 cells showed no change in phosphorylation irrespective of doxorubicin concentration (Fig. 4a). In contrast, MCF-7/ADR cells showed a gradual increase in phosphorylation with increasing doxorubicin concentration. This increase in PKCα activity in response to doxorubicin treatment may correlate with an increase in Pgp-mediated drug efflux in MCF-7/ADR cells.
Effects of doxorubicin and Ro-31-7549 on phosphorylation of the PKCα-specific peptide substrate. After 6 h incubation with doxorubicin alone (a) and with both doxorubicin and Ro-31-7549 (b), cells were scrapped and sonicated at 4 °C. Samples were then centrifuged and the supernatant used as cell lysates. Phosphorylation of the PKCα-specific peptide substrate with cell lysates at a protein concentration of 100 μg/mL was carried out at 37 °C for 1 h and analyzed by MALDI-TOF-MS (n = 3). Data are the mean ± S.D., n.s., not significant, *P < 0.05, ***P < 0.005
Then, we examined the effect of a combination of Ro-31-7549 with doxorubicin. Ro-31-7549 inhibited phosphorylation reactions in MCF-7 (23.6 to 3.6 %) and MCF-7/ADR (41.8 to 0.5 %) cells, irrespective of the presence of doxorubicin (Fig. 4b).
Reversal of resistance to doxorubicin by Ro-31-7549 in drug-resistant cells
To ascertain if inhibition of PKCα activity leads to suppression of Pgp-mediated drug efflux in MDR cells, cellular accumulation of doxorubicin was monitored by CLSM in MCF-7 and MCF-7/ADR cells. In the absence of Ro-31-7549, significant accumulation of doxorubicin was observed in drug-sensitive MCF-7 cells, whereas their accumulation was suppressed substantially in drug-resistant MCF-7/ADR cells (Fig. 5). This lower accumulation of doxorubicin in MCF-7/ADR cells showed marked efflux of doxorubicin by highly expressed Pgp in resistant cells [34]. However, in the presence of Ro-31-7549, cellular uptake of doxorubicin was enhanced extensively in MCF-7/ADR cells, suggesting significant suppression of Pgp-mediated doxorubicin efflux due to inhibition of PKCα activity. Results demonstrated that doxorubicin efflux was inhibited by Ro-31-7549. This is the first report focusing on MDR reversal by a PKCα-specific inhibitor.
Intracellular distribution of doxorubicin in MCF-7 (a) and MCF-7/ADR (b) cells. Cellular accumulation and distribution of doxorubicin (100 nM) was observed by confocal laser scanning microscopy by using doxorubicin’s fluorescence. After treatment with doxorubicin for 2 h with/without pre-incubation of 5 μM Ro-31-7549 for 30 min, images were obtained. Scale bar = 50 μm
Cellular accumulation of doxorubicin was evaluated quantitatively by an image-based cytometer (Fig. 6a, b) and the obtained results summarized in Fig. 6c, d. MCF-7 cells showed increasing cellular accumulation of doxorubicin in a dose-dependent manner in the presence and absence of Ro-31-7549 (Fig. 6a). Median fluorescence intensity is summarized in Fig. 6c. Effect of Ro-31-7549 on enhancement of doxorubicin accumulation was small. In MCF-7/ADR cells, cellular accumulation of doxorubicin was much improved in the presence of Ro-31-7549 (Fig. 6b). Median fluorescence intensity of Ro-31-7549-treated cells was much higher than that of non-treated cells and increased gradually, suggesting dose-dependent accumulation of doxorubicin (Fig. 6d). Such MDR reversal in MCF-7/ADR suggested that Ro-31-7549 suppressed the Pgp-mediated drug efflux via PKCα inhibition.
Effects of Ro-31-7549 (50 μM) on accumulation of doxorubicin in MCF-7 (a) and MCF-7/ADR (b) cells. Median of cellular doxorubicin fluorescence is normalized to cellular doxorubicin fluorescence in doxorubicin (0.1 nM) alone as control (c, d). Data are the mean ± S.D., n.s., not significant, **P < 0.001, ***P < 0.005, significant difference in the presence and absence of Ro-31-7549
Finally, enhancement of the anticancer activity of doxorubicin by PKCα inhibition was investigated after treatment of cells with a combination of the two drugs for 24 h. In MCF-7 cells (Fig. 7a), the presence of Ro-31-7549 weakly enhanced the toxicity of doxorubicin, and this enhancement disappeared at the high concentration of doxorubicin (10 nM). In MCF-7/ADR cells (Fig. 7b), Ro-31-7549 enhanced the toxicity of doxorubicin significantly at all the doxorubicin concentrations examined. Interestingly, doxorubicin toxicity against resistant cells reached almost the same level with doxorubicin-sensitive MCF-7 cells at 10 nM of doxorubicin (∼45 % in both cases). Taken together, these results demonstrated that the anticancer activity of doxorubicin can be improved synergistically by inhibition of PKCα activity, which leads to enhanced cellular accumulation of doxorubicin via suppression of Pgp-mediated drug efflux in drug-resistant MCF-7/ADR cells.
Effects of co-administration with doxorubicin and Ro-31-7549 on viability in MCF-7 (a) and MCF-7/ADR (b) cells. After 24 h incubation with different concentrations of doxorubicin and 5 μM Ro-31-7549, viability was evaluated in sensitive and resistant cell lines (n = 3). Data are the mean ± S.D., **P < 0.001, ***P < 0.005, significant difference in the presence and absence of Ro-31-7549
Conclusions
Inhibition of PKCα activity enhanced the accumulation of doxorubicin in MCF-7/ADR cells. Use of the PKCα-specific inhibitor Ro-31-7549 could lead to a decrease of phosphorylation reactions and consequently induce increased drug accumulation through suppression of Pgp-mediated drug efflux in drug-resistant MCF-7/ADR cells. This observation may suggest that Pgp overexpression in MDR cancer cells is linked to PKCα activities, induces phosphorylation reactions in the linker region of Pgp, and provides evidence of reversal of intrinsic anticancer drug resistance. Moreover, reversal of intracellular accumulation of a drug could induce increase drug efficacy in drug-resistant human breast cancer cells. Hence, regulation of PKCα activity and reversal of drug efflux via Ro-31-7549 combined with doxorubicin is a possible alternative to current approaches with many other therapeutic anticancer drugs for combating MDR.
References
Zgurskaya HI, Nikaido H. Multidrug resistance mechanisms: drug efflux across two membranes. Mol Microbiol. 2000;37:219–25.
Gottesman MM, Fojo T, Bates SE. Multidrug resistance in cancer: role of ATP-dependent transporters. Nat Rev Cancer. 2002;2:48–58.
Thomas H, Coley HM. Overcoming multidrug resistance in cancer: an update on the clinical strategy of inhibiting P-glycoprotein. Cancer Control. 2003;10:159–65.
Jones PM, George AM. The ABC transporter structure and mechanism: perspectives on recent research. Cell Mol Life Sci. 2004;61:682–99.
Deeley RG, Westlake C, Cole SPC. Transmembrane transport of endo- and xenobiotics by mammalian ATP-binding cassette multidrug resistance proteins. Physiol Rev. 2006;86:849–99.
Fletcher JI, Haber M, Henderson MJ, Norris MD. ABC transporters in cancer: more than just drug efflux pumps. Nat Rev Cancer. 2010;10:147–56.
Yu M, Ocana A, Tannock IF. Reversal of ATP-binding cassette drug transporter activity to modulate chemoresistance: why has it failed to provide clinical benefit? Cancer Metast Rev. 2013;32:211–27.
Allen JD, van Loevezijn A, Lakhai JM, van der Valk M, van Tellingen O, Reid G, et al. Potent and specific inhibition of the breast cancer resistance protein multidrug transporter in vitro and in mouse intestine by a novel analogue of fumitremorgin C. Mol Cancer Ther. 2002;1:417–25.
Doyle LA, Ross DD. Multidrug resistance mediated by the breast cancer resistance protein BCRP (ABCG2). Oncogene. 2003;22:7340–58.
Dubikovskaya EA, Thorne SH, Pillow TH, Contag CH, Wender PA. Overcoming multidrug resistance of small-molecule therapeutics through conjugation with releasable octaarginine transporters. Proc Natl Acad Sci U S A. 2008;105:12128–33.
Abu Ajaj K, Graeser R, Kratz F. Zosuquidar and an albumin-binding prodrug of zosuquidar reverse multidrug resistance in breast cancer cells of doxorubicin and an albumin-binding prodrug of doxorubicin. Breast Cancer Res Treat. 2012;134:117–29.
Goda K, Fenyvesi F, Bacso Z, Nagy H, Marian T, Megyeri A, et al. Complete inhibition of P-glycoprotein by simultaneous treatment with a distinct class of modulators and the UIC2 monoclonal antibody. J Pharmacol Exp Ther. 2007;320:81–8.
Patel NR, Rathi A, Mongayt D, Torchilin VP. Reversal of multidrug resistance by co-delivery of tariquidar (XR9576) and paclitaxel using long-circulating liposomes. Int J Pharmaceut. 2011;416:296–9.
Li XR, Li PZ, Zhang YH, Zhou YX, Chen XW, Huang YQ, et al. Novel mixed polymeric micelles for enhancing delivery of anticancer drug and overcoming multidrug resistance in tumor cell lines simultaneously. Pharm Res-Dordr. 2010;27:1498–511.
Gottesman MM. Mechanisms of cancer drug resistance. Annu Rev Med. 2002;53:615–27.
Malam Y, Loizidou M, Seifalian AM. Liposomes and nanoparticles: nanosized vehicles for drug delivery in cancer. Trends Pharmacol Sci. 2009;30:592–9.
Hu CMJ, Zhang LF. Therapeutic nanoparticles to combat cancer drug resistance. Curr Drug Metab. 2009;10:836–41.
Chambers TC, Mcavoy EM, Jacobs JW, Eilon G. Protein kinase C phosphorylates P-glycoprotein in multidrug resistant human KB carcinoma cells. J Biol Chem. 1990;265:7679–86.
Budworth J, Gant TW, Gescher A. Co-ordinate loss of protein kinase C and multidrug resistance gene expression in revertant MCF-7/Adr breast carcinoma cells. Br J Cancer. 1997;75:1330–5.
Idriss H, Urquidi V, Basavappa S. Selective modulation of P-glycoprotein’s ATPase and anion efflux regulation activities with PKC α and PKC ε in Sf9 cells. Cancer Chemother Pharmacol. 2000;46:287–92.
Bates SE, Lee JS, Dickstein B, Spolyar M, Fojo AT. Differential modulation of P-glycoprotein transport by protein kinase inhibition. Biochemistry. 1993;32:9156–64.
Chambers TC, Pohl J, Glass DB, Kuo JF. Phosphorylation by protein kinase C and cyclic AMP-dependent protein kinase of synthetic peptides derived from the linker region of human P-glycoprotein. Biochem J. 1994;299:309–15.
Ahmad S, Safa AR, Glazer RI. Modulation of P-glycoprotein by protein kinase C α in a baculovirus expression system. Biochemistry. 1994;33:10313–8.
Idriss HT, Hannun YA, Boulpaep E, Basavappa S. Regulation of volume-activated chloride channels by P-glycoprotein: phosphorylation has the final say! J Physiol. 2000;524:629–36.
Fine RL, Chambers TC, Sachs CW. P-glycoprotein, multidrug resistance and protein kinase C. Oncologist. 1996;1:261–8.
Dean M, Fojo T, Bates S. Tumour stem cells and drug resistance. Nat Rev Cancer. 2005;5:275–84.
Dean M. ABC transporters, drug resistance, and cancer stem cells. J Mammary Gland Biol. 2009;14:3–9.
Tam WL, Lu HH, Buikhuisen J, Soh BS, Lim E, Reinhardt F, et al. Protein kinase C α is a central signaling node and therapeutic target for breast cancer stem cells. Cancer Cell. 2013;24:347–64.
Kang JH, Asai D, Toita R, Kitazaki H, Katayama Y. Plasma protein kinase C (PKC)α as a biomarker for the diagnosis of cancers. Carcinogenesis. 2009;30:1921–31.
Kang JH, Asai D, Yamada S, Toita R, Oishi J, Mori T, et al. A short peptide is a protein kinase C (PKC) α-specific substrate. Proteomics. 2008;8:2006–11.
Wilkinson SE, Parker PJ, Nixon JS. Isoenzyme specificity of bisindolylmaleimides, selective inhibitors of protein kinase C. Biochem J. 1993;294:335–7.
Murphy CT, Westwick J. Selective inhibition of protein kinase C. Effect on platelet-activating-factor-induced platelet functional responses. Biochem J. 1992;283:159–64.
Scambia G, Ranelletti FO, Panici PB, Devincenzo R, Bonanno G, Ferrandina G, et al. Quercetin potentiates the effect of adriamycin in a multidrug-resistant MCF-7 human breast-cancer cell line: P-glycoprotein as a possible target. Cancer Chemother Pharmacol. 1994;34:459–64.
Doyle LA, Yang WD, Abruzzo LV, Krogmann T, Gao YM, Rishi AK, et al. A multidrug resistance transporter from human MCF-7 breast cancer cells. Proc Natl Acad Sci U S A. 1998;95:15665–70.
Yu G, Ahmad S, Aquino A, Fairchild CR, Trepel JB, Ohno S, et al. Transfection with protein kinase C alpha confers increased multidrug resistance to MCF-7 cells expressing P-glycoprotein. Cancer Commun. 1991;3:181–9.
Blobe GC, Sachs CW, Khan WA, Fabbro D, Stabel S, Wetsel WC, et al. Selective regulation of expression of protein kinase C (PKC) isoenzymes in multidrug-resistant MCF-7 cells: functional significance of enhanced expression of PKC α. J Biol Chem. 1993;268:658–64.
Acknowledgments
We thank Professor Masahiro Goto (Kyushu University) for assistance in CLSM studies and Dr. Ick Chan Kwon for the kind gift of the MCF-7/ADR cell line. We also thank Ms. Sigemi Terakubo and Ms. Ninyo Okamura (St. Marianna University School of Medicine) for technical assistance. This work was supported by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan, and a grant from the KRIBB Research Initiative Program (Korean Biomedical Scientist Fellowship Program), Korea Research Institute of Bioscience and Biotechnology, Republic of Korea (C.W.K.).
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding authors
Additional information
Chan Woo Kim and Daisuke Asai contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 118 kb)
Rights and permissions
About this article
Cite this article
Kim, C.W., Asai, D., Kang, JH. et al. Reversal of efflux of an anticancer drug in human drug-resistant breast cancer cells by inhibition of protein kinase Cα (PKCα) activity. Tumor Biol. 37, 1901–1908 (2016). https://doi.org/10.1007/s13277-015-3963-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3963-4