Abstract
The ubiquitin-proteasome system plays an essential regulatory role in various cellular processes. Besides its involvement in normal cellular functions, the alteration of proteasomal activity contributes to the pathological states of several clinical disorders, including cancer. Aberrant methylation of the CpG islands has been reported as an alternative way to inactivate gene expression involved in the ubiquitination process and thus protein degradation in tumor tissues. In this study, we aimed to determine the CpG methylation pattern of the UCHL1 promoter, as well as the mutation spectrum and the expression pattern of P53 in sporadic colorectal cancer (CRC) from Tunisian patients. We found that UCHL1 was methylated in 68.57 % and correlated significantly with lymph node metastasis (P = 0.029) and transcriptional silencing in tumor tissues (P = 0.013). Mutation screening of exons 5–9 of P53 showed that 42.85 % of cases harbor somatic mutation and are positively correlated with the methylated pattern of UCHL1 (P = 0.001). Furthermore, cytoplasmic accumulation of P53 was strongly associated with the unmethylated UCHL1 profile (P = 0.006), supporting the relationship between these two proteins in CRC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the second most common cancer with 1.2 million new cases/year worldwide [1]. In Tunisia, the incidence of CRC is 2.5–4.5/100,000 [2]. Over the past decade, the prognosis for CRC has been improved through advances in treatments. However, only 30–40 % of patients are diagnosed at an early stage [3]. In most CRC patients, the progression of normal colonic mucosa to invasive cancer requires several molecular changes [4]. Chromosomal and microsatellite instability pathways constitute the major genetic instability events in CRC [5, 6], and aberrant methylation of cancer-related gene promoters is often responsible for transcriptional silencing of tumor suppressor genes (TSG) in tumor tissues [7–9]. Gene promoter’s methylation has been extensively explored, and reliable biomarkers have been identified in CRC [7, 8]. On the other hand, CpG DNA methylation often occurs at an early stage during CRC carcinogenesis; therefore, the identification of specifically methylated genes in patients compared to controls could be used for early diagnosis of cancerous lesions. Furthermore, high levels of circulating methylated DNA released by tumor cells have been detected in the peripheral blood of CRC patients, which could serve as biomarkers for tumor cell detection in a non-invasive manner contrary to colonoscopy [10, 11]. Hence, it is useful to make efforts for the identification of epigenetic biomarkers in CRC.
Protein ubiquitination system is responsible for the selective degradation of most intracellular proteins. It has emerged not only as one of the most multifaceted post-translational modifications, which plays an essential regulatory role in many critical cellular processes, but also contributes to tumor initiation and progression [12]. Hence, targeting the ubiquitin-proteasome pathway constitutes a novel developing concept in cancer therapy [13]. Ubiquitin C-terminal hydrolase-L1 (UCHL1 or PGP9.5), a member of the UCH class of DUBs, is one of the most well-studied DUBs in view of its association with neurodegenerative pathologies and other malignancies [14]. Normally expressed in neurons, the neuroendocrine system, and gonads, aberrant expression of UCHL1 has been described in non-small cell lung cancer [10, 15], invasive CRC [11], osteosarcoma [16], and esophageal cancer [17]. Overexpression of UCHL1 was associated with tumor size and invasiveness of neoplastic cells [11, 18]. The expression level of UCHL1 is either upregulated or downregulated mainly by methylation of CpG islands, depending on the type of tumor. In fact, hypomethylation of the UCHL1 promoter leads to increased expression in bladder cancer [19]. In contrast, aberrant methylation conducting to transcriptional silencing of the UCHL1 gene has been described in esophageal squamous cell carcinoma and gastric cancer [20, 21].
P53 is among the most commonly affected TSG during the pathogenesis of human cancers, hence the name of universal TSG. P53 acts as a transcription factor regulating the expression of several genes involved in the control of cell cycle, DNA damage, and apoptosis [22, 23].
The P53 gene is mutated in about half of human cancers, and in CRC, somatic mutations are found in 40 to 50 % of samples [24, 25]. Regarding its role as a regulator of gene expression, the P53 levels must be strictly controlled in the cells mainly through its interaction with mdm2 [22]. Recent studies tend to find the link between P53 and UCHL1 in carcinogenesis. Li et al. showed that UCHL1 could deubiquitinate P53 and p14ARF and ubiquitinate mdm2 for P53 stabilization to promote P53 signaling in nasopharyngeal cancer cells [26]. In breast cancer, it was reported that the UCHL1 unmethylated pattern correlated with accumulation of P53 in primary sporadic breast tumors [27].
This study was conducted to elucidate whether the UCHL1 and P53 genes are associated in the pathogenesis of CRC in Tunisian patients in order to identify novel biomarkers of colorectal carcinogenesis, facilitating personalized therapy. To this end, we analyzed the epigenetic alteration of the UCHL1 promoter and the mutational status of the P53 gene in 35 tumors and their association with major clinical parameters. Correlation between P53 expression and UCHL1 methylation was also investigated.
Material and methods
Patient’s characteristics
A total of 35 primary sporadic adenocarcinomas were collected between January 2003 and December 2007 from patients who underwent radical surgical resection at the Department of Digestive Surgery of Habib Bourguiba University Hospital (Sfax, Tunisia). The study was performed in accordance with the ethical standards of the revised Declaration of Helsinki (October 2013), and all patients gave informed consent prior to specimen collection according to institutional guidelines. None of the patients had preoperative or postoperative chemotherapy. At the time of surgery, the age of patients ranged from 35 to 82 years (mean 66.08 years), and the sex ratio was 1:1.05. The histological subtypes were classified according to the World Health Organization criteria. The carcinomas were staged according to the TNM (tumor, lymph node, and metastasis) classification adopted by the American Joint Committee on Cancer.
DNA extraction and methylation-specific PCR
Genomic DNA was isolated from tissue sections by phenol/chloroform procedure as described previously [28], and the quantity was checked by Nanodrop (Thermo Fisher Scientific). DNA samples were stored at −20 °C for further use. For methylation-specific PCR (MSP), 1 μg of DNA was treated with sodium bisulfite which converts the unmethylated cytosine to uracil using the EZ Methylation Kit according to the manufacturer’s recommendations (ZymoResearch). The bisulfite-treated DNA was amplified using specific primers for methylated and unmethylated UCHL1 alleles. The sequences of the primers, annealing temperature, and product size are listed in Table 1. The MSP condition used was described previously [29]. Briefly, after initial denaturation at 95 °C for 5 min, 35 cycles of 30 s at 94 °C, 30 s at optimal annealing temperature, and 30 s at 72 °C were done, followed by a final extension at 72 °C for 10 min. The reactions were performed in a total volume of 25 μl, containing 2 μl of bisulfite-treated DNA, 0.2 μM of each primer, 200 μM dNTP, 1× PCR buffer, and 1 unit of Dream Taq DNA polymerase (Fermentas). The amplified products were analyzed by electrophoresis on 2 % agarose gel, stained with ethidium bromide, and visualized under ultraviolet light.
RNA extraction and RT-PCR
Total RNA was isolated from 35 fresh frozen tumor tissues using TRIzol reagent [30]. First-strand cDNA synthesis was performed on 2 μg of total RNA, treated with DNaseI (Amersham Biosciences), 0.5 μg oligo dT, 2 mM dNTP, 0.5 unit/μl RNase inhibitor (Fermentas), 4 μl of 5× RT buffer, and 200 units of MMLV reverse transcriptase (Fermentas). The reaction mixture was incubated at 37 °C for 1 h, followed by 70 °C for 10 min. The cDNA (2 μl) was used as a template in PCR using specific primers for UCHL1 and GAPDH (Table 1). The PCR products were analyzed on 2 % agarose gel, stained with ethidium bromide, and visualized under UV light.
Mutation analysis
Exons 5–6 and 7–9 of P53 gene were amplified in PCR reactions containing 0.2 μM of each primer (Table 1), 200 μM dNTP, 2 mM MgCl2, 1× PCR buffer, 1 unit of Dream Taq DNA polymerase (Fermentas), and 100 ng of DNA in a total volume of 25 μl for 2 min at 95 °C, 35 cycles of 30 s at 94 °C, 30 s at annealing temperature, 30 s at 72 °C, and then 7 min at 72 °C. PCR products were purified and sequenced in both directions using the BigDye Terminator v3.1 Cycle Sequencing kit on an ABI 3130 Genetic Analyser (Applied Biosystems, CA, USA).
Immunohistochemical staining and scoring
Before immunostaining, two pathologists (LA and AK) reviewed hematoxylin- and eosin-stained slides in each case, and blocks containing adenocarcinoma were selected. Briefly, 4-μm-thick sections were cut from each paraffin block, mounted on poly-l-lysine-coated slides, fixed in acetone for 10 min, and left to dry overnight at 37 °C. Slides were deparaffinized in xylene followed by ethanol and subsequent rehydration in graded ethanol. The sections were then pre-treated with 3 % hydrogen peroxide for 10 min to inactivate endogenous peroxides and washed in phosphate-buffered saline (PBS) solution. Heat-induced antigen retrieval was performed using epitope retrieval solution (DAKO) at 95 °C for 40 min. After heating, slides were allowed to cool down to room temperature, briefly washed in PBS, and then incubated in blocking solution (protein block serum: 0.25 % casein in PBS containing carrier protein and NaN3; DAKO) for 5 min. Immunohistochemical staining was performed using the streptavidin-biotin peroxidase system. Slides were incubated for 30 min at room temperature with anti-P53 (Pab 1801: sc-98; Santa Cruz Biotechnology) antibodies diluted at 1:100, washed with PBS before applying the biotinylated secondary antibody (anti-rabbit, DAKO) for 5 min. Sections were incubated with the streptavidin-biotin complex reagent (Universal Quick Kit, DAKO) for 15 min and developed with 3,3′-diaminobenzidine tetrahydrochloride (DAB) for 30 min. Finally, tissue sections were counterstained by Mayer’s hematoxylin, dehydrated, and mounted (DAKO).
The immunostained slides were scored as described previously [31]. Briefly, the initial scoring was graded according to the extent of immunostaining as follows: 0: no staining or less than 5 %; 1: 5–25 % staining; 2: 26–75 % staining; and 3: 76–100 % staining. In addition, the intensity of staining was also evaluated as follows: 0: negative; 1: weak; 2: moderate; and 3: intense. In regard to the variability in the intensity of staining, each component of the tumor was scored independently. The sum of the intensity and staining extent scores was used as the final immunoreactive score (0–12). The final scores were regarded as negative (0–1 score) and positive (2–12 score).
Statistical analysis
The statistical significance of the association between UCHL1 methylation and P53 expression and mutational status, as well as clinicopathological parameters, was assessed by a two-sided chi-square test. When needed, Fisher’s exact test correction was used in order to validate the chi-square test results. For that statistical analysis, SPSS software version 20 was used.
Results
Methylation profile of the UCHL1 promoter and correlation with clinicopathological parameters
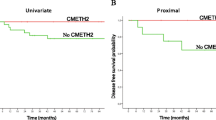
The UCHL1 methylated allele was detected in 68.57 % of cases. A representative example of the MSP results is shown in Fig. 1. Using univariate analysis, we analyzed whether clinicopathological characteristics such as age, gender, tumor stage, grading, or localization of the tumor are associated with the methylation status of UCHL1. Except for one significant association with lymph node metastasis (P = 0.029; t = 0.005), no other associations were observed (Table 2).
Correlation of mRNA and methylation status of UCHL1
In an attempt to validate the effect of aberrant methylation on the expression of UCHL1, we performed semi-quantitative RT-PCR on 35 CRC cases displaying the unmethylated or methylated profiles using the GAPDH as internal control (Fig. 2a). We found that among 24 cases with the methylated pattern, the UCHL1 mRNA was detected in only 5 (20.8 %) cases (P = 0.013; t = 0.022; Fig. 2b). Therefore, we suggest that the CpG methylation is a major event responsible for the silencing of UCHL1 in CRC.
a Representative results of RT-PCR of UCHL1 in CRC cases. GAPDH was used as an endogenous control. H2O negative control for RT-PCR, T1–T5 tumor DNAs, L 100-bp DNA ladder (Fermentas), T7 absence of mRNA, T6, T8–T10 presence of mRNA. b Histogram representing the methylation profile and the mRNA expression of UCHL1 in tumor samples
P53 mutation and expression analysis: association with the UCHL1 methylation pattern
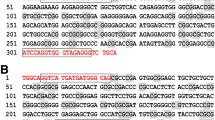
Mutation screening of exons 5–9 of the P53 gene showed that 15 out of 35 cases (42.85 %) were mutated (Table 3). One mutation was novel: the p.D184EfsX61 (c.552_555del4) in exon 5 (Fig. 3a). Interestingly, the p.R196Q (c.587G > A) mutation in exon 6 was identified in 8 out of 15 patients (Fig. 3b). Besides mutation, several polymorphisms were identified and are listed in Table 3. Furthermore, a positive association was seen between the unmethylated profile of the UCHL1 promoter and the mutated P53 gene (P = 0.001; t = 0.001; Table 1). On the other hand, we studied by IHC the expression of P53 in the 35 CRC specimens analyzed by MSPCR. Aberrant cytoplasmic accumulation of P53 was seen in 57.1 % (20 out of 35) of tumors and significantly correlated with the unmethylated UCHL1 promoter (Fig. 4). In fact, among 15 tumor tissues negative for P53 expression, 14 (58.3 %) were methylated for UCHL1 (P = 0.006; t = 0.009), suggesting a relationship between these two proteins in CRC. No association was noted between the P53 immunopositivity and the presence of mutation.
P53 immunohistochemical staining and methylation status of UCHL1. a Histogram representing the cytoplasmic expression of P53 protein depending on the methylation profile of UCHL1 in tumor samples (P = 0.006). b P53 immunoexpression in tumor tissues showing strong cytoplasmic accumulation and unmethylated UCHL1 (left panel) and negative expression and methylated UCHL1 (right panel)
Discussion
Epigenetic modification of the CpG islands in the gene promoter regions has been proposed as an alternative way to inactivate several cancer-related genes in tumor tissues [32]. Recently, many lines of evidence indicated that UCHL1 is involved in tumor progression. However, the UCHL1 roles differ depending on the type of cancer. In fact, it has been shown that in some cancers, UCHL1 acts as an oncogene [18, 33, 34], while in others, it would function as a TSG [26, 35, 36]. In CRC, many lines of evidence indicate that UCHL1 is related to tumorigenesis, but the mechanism is still ambiguous. Zhong et al. provided evidence that UCHL1 functions as an oncogene by regulating the β-catenin/TCF pathway [37]. However, other studies have shown that UCHL1 was more frequently methylated in CRC tissues than in normal colorectal tissues [38], whereas others have indicated that high UCHL1 expression was related to colorectal tumor progression, invasion, lymph node metastasis, and poor clinical outcome [39]. In this study, we showed that UCHL1 is frequently methylated (68.57 %), leading to transcriptional silencing, since a significant correlation was found between the methylated UCHL1 gene promoter and the loss of its corresponding mRNA (P = 0.013; t = 0.022). Our results are in agreement with several studies claiming that methylation of UCHL1 is a common event in colorectal tumors as well as in cell lines of colon cancer [20, 35]. Okochi-Takada et al. showed aberrant methylation of UCHL1 in 47 % of primary colorectal tumors, and a demethylating treatment with 5-azacitidine resulted in the restoration of its expression in the cell lines [35]. In another study, the percentage of methylation was higher (73 %) in primary colorectal tumors and correlated with lymph node metastasis [20]. In our study, CpG methylation of the UCHL1 promoter was significantly more frequent in patients with lymph node metastasis than in N0 patients (P = 0.029; t = 0.05). This result is consistent with the fact that UCHL1 expression is related to lymph node metastases in colorectal patients as previously reported [21, 38]. Regarding its deubiquitinase activity, UCHL1 is involved in different signaling pathways. It was recently shown that in the HCT8 cell line, UCHL1 upregulated the expression of β-catenin by decelerating its degradation [37]. These authors showed that UCHL1 induction increased the accumulation of β-catenin in the cytoplasm and subsequently its translocation into the cell nucleus and activate target genes such as cyclin D1 which is a major regulator of cell proliferation [39]. As a guardian of genome, P53 is strongly regulated, mainly through a feedback loop by MDM2 [40]. The link between UCHL1 and P53 has been reported in breast and nasopharyngeal cancers [26, 27, 41]. It was shown that UCHL1 activates the p14ARF-P53 signaling pathway by deubiquitinating P53 and p14ARF as well as ubiquitinating MDM2 through its two opposing enzyme activities, hydrolase and ligase [41]. We compared the UCHL1 methylation status with P53 expression in tumor tissues. Positive association was seen between cytoplasmic accumulation of P53 and the unmethylated UCHL1 profile. Indeed, among 35 cases, 20 displayed positive immunostaining and 90 % (10 out of 11 cases) of them were unmethylated for the UCHL1 promoter (P = 0.006; t = 0.015). Our result supports previous data on breast and nasopharyngeal carcinoma; nevertheless, we will need to confirm it in a larger number of Tunisian CRC patients.
It was reported that the P53 gene is frequently mutated in CRC cases. The mutations are predominantly of the missense type, located in the DNA binding domain, which leads to the loss of P53 function as a transcription factor [24]. In our series, the P53 gene is mutated in 42.85 % of cases, which is in line with the rates recorded by the majority of the studies [42–44]. According to previous reports, the mutational spectrum of P53 in Tunisian patients is largely variable. In fact, while Chaar et al. found that P53 is mutated in only 17.4 % of patients [45], Aissi et al. showed that P53 mutations are more frequent, reaching 59.6 % [46]. In our study, among the identified mutations, one was novel: the p.D184EfsX61 (c.552_555del4) located in exon 5. The recurrence of the p.R196Q (c.587G > A) mutation in exon 6 was highly interesting since it has been identified in 8 out of 16 patients. This mutation is likely to be frequent in southern areas of Tunisia as it has not been described in patients from north Tunisia [45, 46].
In summary, we found that UCHL1 is frequently methylated in Tunisian patients with sporadic CRC and that aberrant methylation correlated with lymph node metastasis. We also observed positive associations of both P53 expression and mutation in tumor tissues with the unmethylated pattern of the UCHL1 promoter, supporting the evidence that UCHL1 exerts its tumor-suppressive functions through P53 deubiquitination in colon tumorigenesis. It is well established that the half-life of mutant p53 is increased compared to the wild-type form mainly due to translational modifications of specific residues which prevents its interaction with mdm2, thus escaping p53 degradation. However, the question that remains to be resolved is if UCHL1 can deubiquitinate the mutant p53 in order to increase its stability. This hypothesis can be tested on CRC cell lines expressing either wild-type p53 or the mutant form in the presence of unmethylated UCHL1 in order to confirm our data obtained on primary tumor tissues.
Consequently, our results showed that UCHL1 methylation could be useful as a biomarker for tumor invasion, but we believe that a larger study will allow us to confirm our conclusions.
References
Siegel R, Naishadham D, Jemal A. Cancer statistics. CA Cancer J Clin. 2012;62:10–29.
Hsairi M, Ben FR, Abdallah M, Jlidi R, Sellami A, Zheni S, et al. Assessment of cancer in Tunisia. Tunis Med. 2002;80:57–64.
Smith RA, Cokkinides V, Eyre HJ. American Cancer Society guidelines for the early detection of cancer. CA Cancer J Clin. 2006;56:11–25.
Chung DC. The genetic basis of colorectal cancer: insights into critical pathways of tumorigenesis. Gastroenterology. 2000;119:854–65.
Lengauer C, Kinzler KW, Vogelstein B. Genetic instability in colorectal cancers. Nature. 1997;386:623–7.
Fodde R, Smits R, Clevers H. APC, signal transduction and genetic instability in colorectal cancer. Nat Rev Cancer. 2001;1:55–67.
Toyota M, Ahuja N, Ohe-Toyota M, Herman JG, Baylin SB, Issa JP. CpG island methylator phenotype in colorectal cancer. Proc Natl Acad Sci U S A. 1999;96:8681–6.
Kondo Y, Issa JP. Epigenetic changes in colorectal cancer. Cancer Med. 2004;23:29–39.
Baylin SB, Ohm JE. Epigenetic gene silencing in cancer—a mechanism for early oncogenic pathway addiction. Nat Rev Cancer. 2006;6:107–11.
Hibi K, Westra WH, Borges M, Goodman S, Sidransky D, Jen J. PGP9.5 as a candidate tumor marker for non-small-cell lung cancer. Am J Pathol. 1999;155:711–5.
Yamazaki T, Hibi K, Takase T, Tezel E, Nakayama H, Kasai Y, et al. PGP9.5 as a marker for invasive colorectal cancer. Clin Cancer Res. 2002;8:192–5.
Mani A, Gelmann EP. The ubiquitin-proteasome pathway and its role in cancer. J Clin Oncol. 2005;23:4776–89.
Frezza M, Schmitt S, Dou QP. Targeting the ubiquitin-proteasome pathway: an emerging concept in cancer therapy. Curr Top Med Chem. 2011;11(23):2888–905.
Sacco JJ, Coulson JM, Clague MJ, Urbé S. Emerging roles of deubiquitinases in cancer-associated pathways. IUBMB Life. 2010;62(2):140–57.
Hibi K, Liu Q, Beaudry GA, Madden SL, Westra WH, Wehage SL, et al. Serial analysis of gene expression in non-small cell lung cancer. Cancer Res. 1998;58:5690–4.
Liu X, Zeng B, Ma J, Wan C. Comparative proteomic analysis of osteosarcoma cell and human primary cultured osteoblastic cell. Cancer Invest. 2009;27:345–52.
Takase T, Hibi K, Yamazaki T, Nakayama H, Taguchi M, Kasai Y, et al. PGP9.5 overexpression in esophageal squamous cell carcinoma. Hepatogastroenterology. 2003;50:1278–80.
Tezel E, Hibi K, Nagasaka T, Nakao A. PGP9.5 as a prognostic factor in pancreatic cancer. Clin Cancer Res. 2000;6:4764–7.
Lee YM, Lee JY, Kim MJ, Bae HI, Park JY, Kim SG, et al. Hypomethylation of the protein gene product 9.5 promoter region in gallbladder cancer and its relationship with clinicopathological features. Cancer Sci. 2006;97:1205–10.
Sato F, Meltzer SJ. CpG island hypermethylation in progression of esophageal and gastric cancer. Cancer. 2006;106:483–93.
Mandelker DL, Yamashita K, Tokumaru Y, Mimori K, Howard DL, Tanaka Y, et al. PGP9.5 promoter methylation is an independent prognostic factor for esophageal squamous cell carcinoma. Cancer Res. 2005;65:4963–8.
Ko JL, Prives C. p53: puzzle and paradigm. Genes Dev. 1996;10:1054–72.
Levine JA. p53, the cellular gatekeeper for growth and division. Cell. 1997;88:323–31.
Petitjean A, Mathe E, Kato S, Ishioka C, Tavtigian SV, Hainaut P, et al. Impact of mutant p53 functional properties on TP53 mutation patterns and tumor phenotype: lessons from recent developments in the IARC TP53 database. Hum Mutat. 2007;28:622–9.
Iacopetta B. TP53 mutation in colorectal cancer. Hum Mutat. 2003;21:271–6.
Li L, Tao Q, Jin H, van Hasselt A, Poon FF, Wang X, et al. The tumor suppressor UCHL1 forms a complex with p53/MDM2/ARF to promote p53 signaling and is frequently silenced in nasopharyngeal carcinoma. Clin Cancer Res. 2010;16(11):2949–58.
Trifa F, Karray-Chouayekh S, Jmaa ZB, Jmal E, Khabir A, Sellami-Boudawara T, et al. Frequent CpG methylation of ubiquitin carboxyl-terminal hydrolase 1 (UCHL1) in sporadic and hereditary Tunisian breast cancer patients: clinical significance. Med Oncol. 2013;30(1):418.
Sambrook J, Russell DW. Molecular cloning. A laboratory manual. Cold Spring Harbor: Cold Spring Harbor Laboratory Press; 2001. p. 6–4.
Herman JG, Graff JR, Myöhänen S, Nelkin BD, Baylin SB. Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci U S A. 1996;93:9821–6.
Chomczynski P, Sacchi N. Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem. 1987;162:156–9.
Miladi-Abdennadher I, Abdelmaksoud-Damak R, Ayadi L, Khabir A, Amouri A, Frikha F, et al. Expression of p16INK4a, alone or combined with p53, is predictive of better prognosis in colorectal adenocarcinoma in Tunisian patients. Appl Immunohistochem Mol Morphol. 2011;19(6):562–8.
Xu XL, Yu J, Zhang HY, Sun MH, Gu J, Du X, et al. Methylation profile of the promoter CpG islands of 31 genes that may contribute to colorectal carcinogenesis. World J Gastroenterol. 2004;10:3441–54.
Kim HJ, Kim YM, Lim S, Nam YK, Jeong J, Kim HJ, et al. Ubiquitin C-terminal hydrolase-L1 is a key regulator of tumor cell invasion and metastasis. Oncogene. 2009;28:117–27.
Leiblich A, Cross SS, Catto JW, Pesce G, Hamdy FC, Rehman I. Human prostate cancer cells express neuroendocrine cell markers PGP 9.5 and chromogranin A. Prostate. 2007;67:1761–9.
Okochi-Takada E, Nakazawa K, Wakabayashi M, Mori A, Ichimura S, Yasugi T, et al. Silencing of the UCHL1 gene in human colorectal and ovarian cancers. Int J Cancer. 2006;119(6):1338–44.
Yu J, Tao Q, Cheung KF, Jin H, Poon FF, Wang X, et al. Epigenetic identification of ubiquitin carboxyl-terminal hydrolase L1 as a functional tumor suppressor and biomarker for hepatocellular carcinoma and other digestive tumors. Hepatology. 2008;48:508–18.
Zhong J, Zhao M, Ma Y, Luo Q, Liu J, Wang J, et al. UCHL1 acts as a colorectal cancer oncogene via activation of the β-catenin/TCF pathway through its deubiquitinating activity. Int J Mol Med. 2012;30(2):430–6.
Yamazaki T, Hibi K, Takase T, Tezel E, Nakayama H, Kasai Y, et al. PGP9.5 as a marker for invasive colorectal cancer. Clin Cancer Res. 2002;8(1):192–5.
Sherr CJ. Cancer cell cycles. Science. 1996;274:1672–7.
Momand J, Wu HH, Dasgupta G. MDM2—master regulator of the p53 tumor suppressor protein. Gene. 2000;242:15–29.
Xiang T, Li L, Yin X, Yuan C, Tan C, Su X, et al. The ubiquitin peptidase UCHL1 induces G0/G1 cell cycle arrest and apoptosis through stabilizing p53 and is frequently silenced in breast cancer. PLoS One. 2012;7(1), e29783.
Soussi T, Dehouche K, Beroud C. p53 website and analysis of p53 gene mutations in human cancer: forging a link between epidemiology and carcinogenesis. Hum Mutat. 2000;15:105–13.
Soussi T, Beroud C. Significance of TP53 mutations in human cancer: a critical analysis of mutations at CpG dinucleotides. Hum Mutat. 2003;21:192–200.
Tominaga T, Iwahashi M, Takifuji K, Hotta T, Yokoyama S, Matsuda K, et al. Combination of p53 codon 72 polymorphism and inactive p53 mutation predicts chemosensitivity to 5-fluorouracil in colorectal cancer. Int J Cancer. 2010;126:1691–701.
Chaar I, Ounissi D, Boughriba R, Ben Ammar A, Sameh A, Khalfallah T, et al. Implication of K-ras and p53 in colorectal cancer carcinogenesis in Tunisian population cohort. Tumour Biol. 2014;35(7):7163–75.
Aissi S, Buisine MP, Zerimech F, Kourda N, Moussa A, Manai M, et al. TP53 mutations in colorectal cancer from Tunisia: relationships with site of tumor origin, microsatellite instability and KRAS mutations. Mol Biol Rep. 2014;41(3):1807–13.
Acknowledgments
This work was supported by a grant from the Tunisian Ministry of Higher Education and Scientific Research. We thank the technician from the “Department of Analysis-CBS” for DNA sequencing.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdelmaksoud-Dammak, R., Saadallah-Kallel, A., Miladi-Abdennadher, I. et al. CpG methylation of ubiquitin carboxyl-terminal hydrolase 1 (UCHL1) and P53 mutation pattern in sporadic colorectal cancer. Tumor Biol. 37, 1707–1714 (2016). https://doi.org/10.1007/s13277-015-3902-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3902-4